Vitamin D Levels in COVID-19 Outpatients from Western Mexico: Clinical Correlation and Effect of Its Supplementation
, Journal of Clinical Medicine, doi:10.3390/jcm10112378, May 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
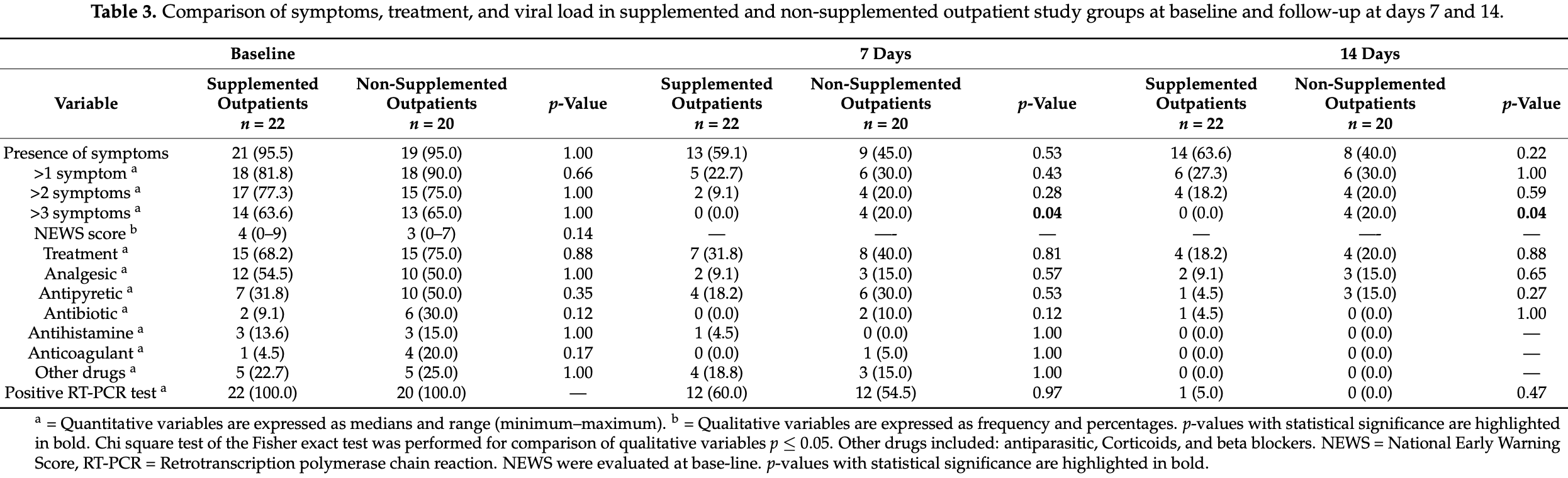
Very small 42 PCR+ outpatient RCT in Mexico, 22 treated with vitamin D. Most patients had insufficient vitamin D levels, there were more symptoms in those with insufficient levels, and there were less cases with fever or with >3 symptoms at day 14 for treatment with vitamin D.
This is the 4th of 40 COVID-19 RCTs for vitamin D, which collectively show efficacy with p=0.0000001.
This is the 38th of 135 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
|
risk of severe case, 89.4% lower, RR 0.11, p = 0.04, treatment 0 of 22 (0.0%), control 4 of 20 (20.0%), NNT 5.0, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), risk of >3 symptoms at day 14.
|
|
risk of no recovery, 80.8% lower, RR 0.19, p = 0.22, treatment 0 of 22 (0.0%), control 2 of 20 (10.0%), NNT 10.0, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), risk of fever at day 14, Table S1.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Sánchez-Zuno et al., 28 May 2021, Randomized Controlled Trial, Mexico, peer-reviewed, 12 authors, dosage 10,000IU days 1-14.
Vitamin D Levels in COVID-19 Outpatients from Western Mexico: Clinical Correlation and Effect of Its Supplementation
Journal of Clinical Medicine, doi:10.3390/jcm10112378
Background: The immunomodulatory effects of vitamin D are known to be beneficial in viral infections; it is also known that its deficiency is associated with a prognosis more critical of Coronavirus Disease 2019. This study aimed to determine baseline vitamin D serum concentrations and the effects of its supplementation in asymptomatic or mildly symptomatic Coronavirus Disease 2019 outpatients. Methods: 42 outpatients were included, 22 of which received a supplement of 10,000 IU of vitamin D3 for 14 days; the remaining 20 outpatients were designated as a control group. Serum levels of transferrin, ferritin, vitamin D, and D-dimer were measured at baseline in both groups. After 14 days, serum levels of total vitamin D were determined in the supplemented group. Results: At baseline, only 19% of infected outpatients had vitamin D levels corresponding to sufficiency. All outpatients with vitamin D insufficiency had at least one symptom associated with the disease, while only 75% of patients with symptoms presented sufficiency. On the seventh and fourteenth day of follow-up, the supplemented group presented fewer symptoms with respect to those non-supplemented. A vitamin D3 dose of 10,000 IU/daily for 14 days was sufficient to raise vitamin D serum concentrations. Conclusions: Immunomodulatory effects of vitamin D appear to be linked to the development of symptoms in positive outpatients. Vitamin D supplementation could have significant benefits in the Western Mexican population.
References
Ajabshir, The Effects of Vitamin D on the Renin-Angiotensin System, Eff. Vitam. Renin. Angiotensin Syst, doi:10.12860/jnp.2014.09
Azrielant, Shoenfeld, Vitamin D and the Immune System, Israel Med. Assoc. J
Baeke, Takiishi, Korf, Gysemans, Mathieu et al., Modulator of the Immune System, Curr. Opin. Pharmacol, doi:10.1016/j.coph.2010.04.001
Bedolla-Barajas, López-Hernández, García-Padilla, Morales-Romero, Velarde-Rivera et al., Prevalencia de insuficiencia y deficiencia de vitamina D en adultos mexicanos con asma alérgica, Rev. Alerg. México, doi:10.29262/ram.v64i2.255
Bolondi, Russo, Gamberini, Circelli, Meca et al., Iron Metabolism and Lymphocyte Characterisation during Covid-19 Infection in ICU Patients: An Observational Cohort Study, World J. Emerg. Surg, doi:10.1186/s13017-020-00323-2
Cheng, Li, Li, Liu, Yan et al., Ferritin in the Coronavirus Disease 2019 (COVID-19): A Systematic Review and Meta-analysis, J. Clin. Lab. Anal, doi:10.1002/jcla.23618
Clark, Vivanco-Muñoz, Piña, Rivas-Ruiz, Huitrón et al., High Prevalence of Hypovitaminosis D in Mexicans Aged 14 Years and Older and Its Correlation with Parathyroid Hormone, Arch. Osteoporos, doi:10.1007/s11657-015-0225-4
Conti, Induction of Pro-Inflammatory Cytokines (IL-1 and IL-6) and Lung Inflammation by COVID-19: Anti-Inflammatory Strategies, J. Biol. Regul. Homeost. Agents, doi:10.23812/CONTI-E
Dai, ABO Blood Group Predisposes to COVID-19 Severity and Cardiovascular Diseases, Eur. J. Prev. Cardiol, doi:10.1177/2047487320922370
Dancer, Parekh, Lax, D'souza, Zheng et al., Vitamin D Deficiency Contributes Directly to the Acute Respiratory Distress Syndrome (ARDS), Thorax, doi:10.1136/thoraxjnl-2014-206680
De Lucena, Da Silva Santos, De Lima, De Albuquerque Borborema, De Azevêdo et al., Mechanism of Inflammatory Response in Associated Comorbidities in COVID, Diabetes Metab. Syndr. Clin. Res. Rev, doi:10.1016/j.dsx.2020.05.025
Ebadi, Montano-Loza, Perspective: Improving Vitamin D Status in the Management of COVID, Eur. J. Clin. Nutr, doi:10.1038/s41430-020-0661-0
Franco, Silva, Barreto, Relationship of Body Mass Index and Waist-to-Hip Ratio with Fibrinolytic Activity Measured as d-Dimer, Obes. Res. Clin. Pract, doi:10.1016/j.orcp.2010.12.003
Fu, Bruce, Wu, Giedroc, The S2 Cu( I ) Site in CupA from Streptococcus Pneumoniae Is Required for Cellular Copper Resistance, Metallomics, doi:10.1039/C5MT00221D
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence That Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Greiller, Martineau, Modulation of the Immune Response to Respiratory Viruses by Vitamin D, Nutrients, doi:10.3390/nu7064240
Hansen, Johnson, An Update on Vitamin D for Clinicians, Curr. Opin. Endocrinol. Diabetes Obes, doi:10.1097/MED.0000000000000288
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of Vitamin D Level among Asymptomatic and Critically Ill COVID-19 Patients and Its Correlation with Inflammatory Markers, Sci. Rep, doi:10.1038/s41598-020-77093-z
Jolliffe, Greenberg, Hooper, Griffiths, Camargo et al., Vitamin D Supplementation to Prevent Asthma Exacerbations: A Systematic Review and Meta-Analysis of Individual Participant Data, Lancet Respir. Med, doi:10.1016/S2213-2600(17)30306-5
Kell, Pretorius, Serum Ferritin Is an Important Inflammatory Disease Marker, as It Is Mainly a Leakage Product from Damaged Cells, Metallomics, doi:10.1039/C3MT00347G
Kuriacose, Olive, Vitamin D Insufficiency/Deficiency Management, South. Med. J, doi:10.1097/SMJ.0000000000000051
Latz, Decarlo, Boitano, Png, Patell et al., Blood Type and Outcomes in Patients with COVID-19, Ann. Hematol, doi:10.1007/s00277-020-04169-1
Lee, Park, Kwon, Ham, Kim et al., Decreased Lung Function Is Associated with Elevated Ferritin but Not Iron or Transferrin Saturation in 42,927 Healthy Korean Men: A Cross-Sectional Study, PLoS ONE, doi:10.1371/journal.pone.0231057
Linkins, Takach Lapner, Review of D-Dimer Testing: Good, Bad, and Ugly, Int. J. Lab. Hematol, doi:10.1111/ijlh.12665
Malaguarnera, Vitamin D3 as Potential Treatment Adjuncts for COVID, Nutrients, doi:10.3390/nu12113512
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D Supplementation to Prevent Acute Respiratory Tract Infections: Systematic Review and Meta-Analysis of Individual Participant Data, BMJ, doi:10.1136/bmj.i6583
Martínez-Zavala, López-Sánchez, Vergara-Lopez, Chávez-Tapia, Uribe et al., Vitamin D Deficiency in Mexicans Have a High Prevalence: A Cross-Sectional Analysis of the Patients from the Centro Médico Nacional 20 de Noviembre, Arch. Osteoporos, doi:10.1007/s11657-020-00765-w
Mccartney, O'shea, Faul, Healy, Byrne et al., Vitamin D and SARS-CoV-2 Infection-Evolution of Evidence Supporting Clinical Practice and Policy Development: A Position Statement from the Covit-D Consortium, Ir. J. Med. Sci, doi:10.1007/s11845-020-02427-9
Meltzer, Best, Zhang, Vokes, Arora et al., Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2020.19722
Mohan, Cherian, Sharma, Exploring Links between Vitamin D Deficiency and COVID, PLoS Pathog, doi:10.1371/journal.ppat.1008874
Nowaczewska, Wici Ński, Osi Ński, Kaźmierczak, The Role of Vitamin D in Primary Headache-from Potential Mechanism to Treatment, Nutrients, doi:10.3390/nu12010243
O'brien, Sandler, Taylor, Weinberg, Serum Vitamin D and Risk of Breast Cancer within Five Years, Environ. Health Perspect, doi:10.1289/EHP943
Pinzon, Angela, None
Pradana, Vitamin D Deficiency among Patients with COVID-19: Case Series and Recent Literature Review, Trop. Med. Health, doi:10.1186/s41182-020-00277-w
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger et al., Vitamin D Deficiency and Outcome of COVID-19 Patients, Nutrients, doi:10.3390/nu12092757
Rastogi, Bhansali, Khare, Suri, Yaddanapudi et al., Short Term, High-Dose Vitamin D Supplementation for COVID-19 Disease: A Randomised, Placebo-Controlled, Study (SHADE Study), Postgrad. Med. J, doi:10.1136/postgradmedj-2020-139065
Sanyaolu, Okorie, Marinkovic, Patidar, Younis et al., Comorbidity and Its Impact on Patients with COVID, SN Compr. Clin. Med, doi:10.1007/s42399-020-00363-4
Shahid, Kalayanamitra, Mcclafferty, Kepko, Ramgobin et al., COVID -19 and Older Adults: What We Know, J. Am. Geriatr. Soc, doi:10.1111/jgs.16472
Shi, Liu, Fu, Xu, Wu et al., Vitamin D/VDR Signaling Attenuates Lipopolysaccharide-Induced Acute Lung Injury by Maintaining the Integrity of the Pulmonary Epithelial Barrier, Mol. Med. Rep, doi:10.3892/mmr.2015.4685
Shitrit, Peled, Shitrit, .-G.; Meidan, Bendayan et al., An Association between Oxygen Desaturation and D-Dimer in Patients with Obstructive Sleep Apnea Syndrome, Thromb. Haemost, doi:10.1160/TH05-02-0103
Smith, Prytherch, Meredith, Schmidt, Featherstone, The Ability of the National Early Warning Score (NEWS) to Discriminate Patients at Risk of Early Cardiac Arrest, Unanticipated Intensive Care Unit Admission, and Death, Resuscitation, doi:10.1016/j.resuscitation.2012.12.016
Taneri, Gómez-Ochoa, Llanaj, Raguindin, Rojas et al., Anemia and Iron Metabolism in COVID-19: A Systematic Review and Meta-Analysis, Eur. J. Epidemiol, doi:10.1007/s10654-020-00678-5
Tay, Poh, Rénia, Macary, Ng, The Trinity of COVID-19: Immunity, Inflammation and Intervention, Nat. Rev. Immunol, doi:10.1038/s41577-020-0311-8
Terpos, Ntanasis-Stathopoulos, Elalamy, Kastritis, Sergentanis et al., Hematological Findings and Complications of COVID, Am. J. Hematol, doi:10.1002/ajh.25829
Turrubiates-Hernández, Sánchez-Zuno, González-Estevez, Hernández-Bello, Macedo-Ojeda et al., Potential Immunomodulatory Effects of Vitamin D in the Prevention of Severe Coronavirus Disease 2019: An Ally for Latin America (Review), Int. J. Mol. Med, doi:10.3892/ijmm.2021.4865
Velavan, Meyer, Mild versus Severe COVID-19: Laboratory Markers, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.04.061
Weitz, Fredenburgh, Eikelboom, A Test in Context: D-Dimer, J. Am. Coll. Cardiol, doi:10.1016/j.jacc.2017.09.024
Whittemore, COVID-19 Fatalities, Latitude, Sunlight, and Vitamin D, Am. J. Infect. Control, doi:10.1016/j.ajic.2020.06.193
Xu, Yang, Chen, Luo, Zhang et al., Vitamin D Alleviates Lipopolysaccharide-Induced Acute Lung Injury via Regulation of the Renin-Angiotensin System, Mol. Med. Rep, doi:10.3892/mmr.2017.7546
Ye, Tang, Liao, Shaw, Deng et al., Does Serum Vitamin D Level Affect COVID-19 Infection and Its Severity?-A Case-Control Study, J. Am. Coll. Nutr, doi:10.1080/07315724.2020.1826005
Yuan, Huang, Ye, Chen, Huang et al., Changes of Hematological and Immunological Parameters in COVID-19 Patients, Int. J. Hematol, doi:10.1007/s12185-020-02930-w
Yılmaz, Şen, Is Vitamin D Deficiency a Risk Factor for COVID-19 in Children?, Pediatr. Pulmonol, doi:10.1002/ppul.25106
DOI record:
{
"DOI": "10.3390/jcm10112378",
"ISSN": [
"2077-0383"
],
"URL": "http://dx.doi.org/10.3390/jcm10112378",
"abstract": "<jats:p>Background: The immunomodulatory effects of vitamin D are known to be beneficial in viral infections; it is also known that its deficiency is associated with a prognosis more critical of Coronavirus Disease 2019. This study aimed to determine baseline vitamin D serum concentrations and the effects of its supplementation in asymptomatic or mildly symptomatic Coronavirus Disease 2019 outpatients. Methods: 42 outpatients were included, 22 of which received a supplement of 10,000 IU of vitamin D3 for 14 days; the remaining 20 outpatients were designated as a control group. Serum levels of transferrin, ferritin, vitamin D, and D-dimer were measured at baseline in both groups. After 14 days, serum levels of total vitamin D were determined in the supplemented group. Results: At baseline, only 19% of infected outpatients had vitamin D levels corresponding to sufficiency. All outpatients with vitamin D insufficiency had at least one symptom associated with the disease, while only 75% of patients with symptoms presented sufficiency. On the seventh and fourteenth day of follow-up, the supplemented group presented fewer symptoms with respect to those non-supplemented. A vitamin D3 dose of 10,000 IU/daily for 14 days was sufficient to raise vitamin D serum concentrations. Conclusions: Immunomodulatory effects of vitamin D appear to be linked to the development of symptoms in positive outpatients. Vitamin D supplementation could have significant benefits in the Western Mexican population.</jats:p>",
"alternative-id": [
"jcm10112378"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-4390-8604",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sánchez-Zuno",
"given": "Gabriela Athziri",
"sequence": "first"
},
{
"affiliation": [],
"family": "González-Estevez",
"given": "Guillermo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Matuz-Flores",
"given": "Mónica Guadalupe",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3815-2160",
"affiliation": [],
"authenticated-orcid": false,
"family": "Macedo-Ojeda",
"given": "Gabriela",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hernández-Bello",
"given": "Jorge",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mora-Mora",
"given": "Jesús Carlos",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0007-1824",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pérez-Guerrero",
"given": "Edsaúl Emilio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "García-Chagollán",
"given": "Mariel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4749-2498",
"affiliation": [],
"authenticated-orcid": false,
"family": "Vega-Magaña",
"given": "Natali",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9637-168X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Turrubiates-Hernández",
"given": "Francisco Javier",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Machado-Sulbaran",
"given": "Andrea Carolina",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2272-9260",
"affiliation": [],
"authenticated-orcid": false,
"family": "Muñoz-Valle",
"given": "José Francisco",
"sequence": "additional"
}
],
"container-title": "Journal of Clinical Medicine",
"container-title-short": "JCM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
5,
28
]
],
"date-time": "2021-05-28T15:33:20Z",
"timestamp": 1622216000000
},
"deposited": {
"date-parts": [
[
2021,
5,
28
]
],
"date-time": "2021-05-28T16:32:11Z",
"timestamp": 1622219531000
},
"funder": [
{
"DOI": "10.13039/501100003141",
"award": [
"A1-S-8774"
],
"doi-asserted-by": "publisher",
"name": "Consejo Nacional de Ciencia y Tecnología"
}
],
"indexed": {
"date-parts": [
[
2024,
2,
22
]
],
"date-time": "2024-02-22T12:47:07Z",
"timestamp": 1708606027409
},
"is-referenced-by-count": 26,
"issue": "11",
"issued": {
"date-parts": [
[
2021,
5,
28
]
]
},
"journal-issue": {
"issue": "11",
"published-online": {
"date-parts": [
[
2021,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
5,
28
]
],
"date-time": "2021-05-28T00:00:00Z",
"timestamp": 1622160000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2077-0383/10/11/2378/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "2378",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
5,
28
]
]
},
"published-online": {
"date-parts": [
[
2021,
5,
28
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1038/s41577-020-0311-8",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"key": "ref2",
"unstructured": "Coronavirus Disease (COVID-19) Situation Reports\n https://covid19.who.int"
},
{
"key": "ref3",
"unstructured": "Mortality Analyses—Johns Hopkins Coronavirus Resource\n https://coronavirus.jhu.edu/data/mortality"
},
{
"DOI": "10.23812/CONTI-E",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1038/s41430-020-0661-0",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1016/j.ijid.2020.04.061",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1186/s13017-020-00323-2",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1177/2047487320922370",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1007/s00277-020-04169-1",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1016/j.dsx.2020.05.025",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1007/s42399-020-00363-4",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1111/jgs.16472",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.3390/nu12113512",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.3892/ijmm.2021.4865",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.3892/mmr.2015.4685",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.3892/mmr.2017.7546",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.3390/nu7064240",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1016/j.coph.2010.04.001",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1002/ppul.25106",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1371/journal.ppat.1008874",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1016/j.ajic.2020.06.193",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1007/s11845-020-02427-9",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1016/j.resuscitation.2012.12.016",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1097/SMJ.0000000000000051",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1002/jcla.23618",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1002/ajh.25829",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1007/s12185-020-02930-w",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1016/j.jacc.2017.09.024",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1111/ijlh.12665",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1007/s10654-020-00678-5",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1039/C3MT00347G",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1039/C5MT00221D",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1371/journal.pone.0231057",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1016/j.orcp.2010.12.003",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1160/TH05-02-0103",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1136/postgradmedj-2020-139065",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1136/bmj.i6583",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1136/thoraxjnl-2014-206680",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1289/EHP943",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.1016/S2213-2600(17)30306-5",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.29262/ram.v64i2.255",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"article-title": "Vitamin D and the Immune System",
"author": "Azrielant",
"first-page": "510",
"journal-title": "Israel Med. Assoc. J.",
"key": "ref45",
"volume": "19",
"year": "2017"
},
{
"DOI": "10.1097/MED.0000000000000288",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.1007/s11657-015-0225-4",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.1186/s41182-020-00277-w",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.3390/nu12010243",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1080/07315724.2020.1826005",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.12860/jnp.2014.09",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.1007/s11657-020-00765-w",
"doi-asserted-by": "publisher",
"key": "ref53"
}
],
"reference-count": 53,
"references-count": 53,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2077-0383/10/11/2378"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Vitamin D Levels in COVID-19 Outpatients from Western Mexico: Clinical Correlation and Effect of Its Supplementation",
"type": "journal-article",
"volume": "10"
}
