Meta-analysis of the Effect of Colchicine on Mortality and Mechanical Ventilation in COVID-19
et al., The American Journal of Cardiology, doi:10.1016/j.amjcard.2021.02.005, Apr 2021
Colchicine for COVID-19
5th treatment shown to reduce risk in
September 2020, now with p = 0.0000049 from 54 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
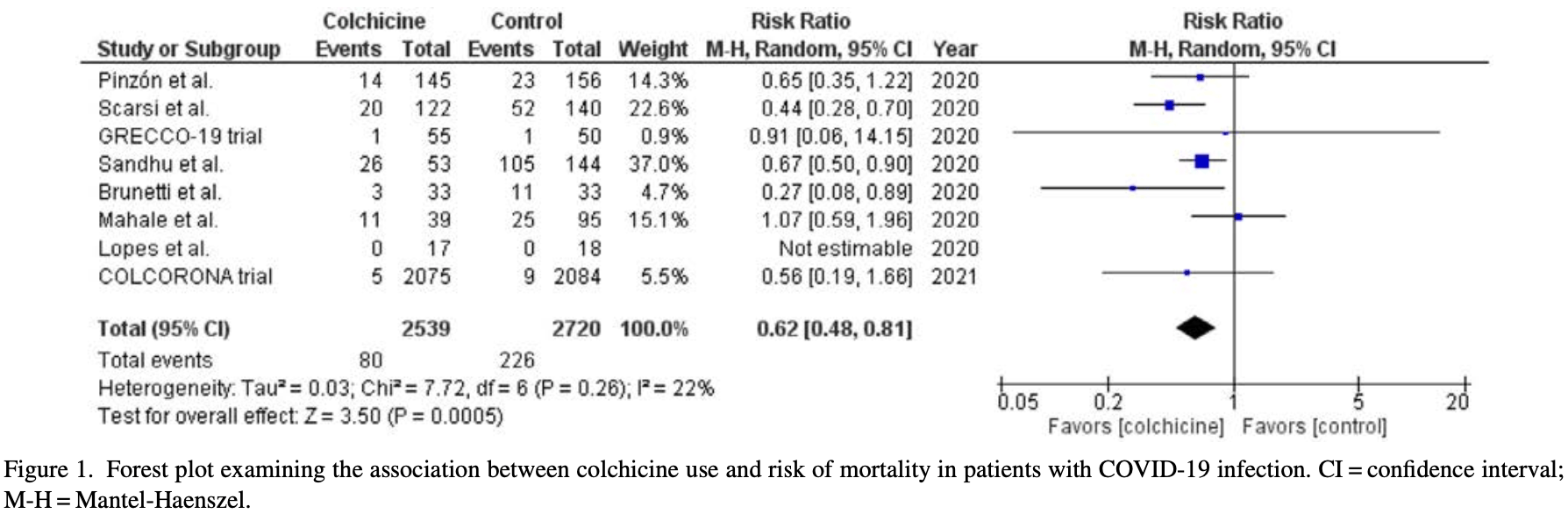
Meta analysis of 8 studies, showing significantly lower COVID-19 mortality with colchicine.
10 meta-analyses show significant improvements with colchicine for mortality1-8,
oxygen therapy8,
hospitalization9, and
severity10.
Currently there are 54 colchicine for COVID-19 studies, showing 22% lower mortality [12‑31%], 29% lower ventilation [-15‑56%], 34% lower ICU admission [8‑52%], 17% lower hospitalization [9‑25%], and 9% more cases [-8‑29%].
|
risk of death, 38.0% lower, RR 0.62, p < 0.001.
|
|
risk of mechanical ventilation, 25.0% lower, RR 0.75, p = 0.27.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Zein et al., Effect of colchicine on mortality in patients with COVID-19 – A systematic review and meta-analysis, Diabetes & Metabolic Syndrome: Clinical Research & Reviews, doi:10.1016/j.dsx.2022.102395.
2.
Rai et al., The Potential Role of Colchicine in Reducing Mortality and Mechanical Ventilation Rates in COVID-19 Infection: A Meta-analysis, Journal of Advances in Medicine and Medical Research, doi:10.9734/jammr/2022/v34i2031503.
3.
Elshafei et al., Colchicine use might be associated with lower mortality in COVID‐19 patients: A meta‐analysis, European Journal of Clinical Investigation, doi:10.1111/eci.13645.
4.
Lien et al., Repurposing Colchicine in Treating Patients with COVID-19: A Systematic Review and Meta-Analysis, Life, doi:10.3390/life11080864.
5.
Danjuma et al., Does Colchicine Reduce Mortality in Patients with Covid-19 Clinical Syndrome? An Umbrella Review of Published Meta-Analyses, Elsevier BV, doi:10.2139/ssrn.4447127.
6.
Salah et al., Meta-analysis of the Effect of Colchicine on Mortality and Mechanical Ventilation in COVID-19, The American Journal of Cardiology, doi:10.1016/j.amjcard.2021.02.005.
7.
Golpour et al., The effectiveness of Colchicine as an anti-inflammatory drug in the treatment of coronavirus disease 2019: Meta-analysis, International Journal of Immunopathology and Pharmacology, doi:10.1177/20587384211031763.
8.
Elshiwy et al., The role of colchicine in the management of COVID-19: a meta-analysis, BMC Pulmonary Medicine, doi:10.1186/s12890-024-03001-0.
Salah et al., 30 Apr 2021, peer-reviewed, 2 authors.
Abstract: 170
The American Journal of Cardiology (www.ajconline.org)
time frame analysis showed a significant
drop in hospitalization rates just after PC
encounters, and continued to decrease
over time (Panel A). The annual trends
for 90-day all-cause hospitalization
rates before PC encounters showed a
significant reduction over time
(59.7% in 2010 to 53.3% in 2018, p
<0.001), but hospitalization rates
after PC remained stable over the
study period (Panel B).
In this observational nationwide
analysis of over 25,000 acute on
chronic HF admissions, PC encounters
were associated with a significant
reduction in all-cause, HF-specific, and
non-HF 90-day hospitalization rates.
This reduction was noted immediately
after discharge from the index admission with a PC encounter. Hospitalization rates before PC utilization
decreased over the study period perhaps
due to the early recognition of value of
PC among these sick patients.
This study is limited by the nature of
this administrative database which carries a risk of mis- or under-coding.
Additionally, we could not identify
patients who died after hospital discharge. Some of the reduction in readmission may be due to this factor.
However, it is unlikely that death would
account for the entire decrease
in admission rates after a hospital PC
consultation, since not all patients seen
by PC physicians are appropriate for
hospice or accept a palliative approach
to care, and the previously reported
post-HF discharge 30-day mortality
rate »7% (1). Moreover, the philosophical change of care to a palliative
approach encourages a decrease in
low-value health care utilization such
as repeat hospital admissions at the
end of life. In summary, we found that
patients who received a PC encounter
during a hospitalization had a reduction in subsequent readmission rates.
Further studies should assess the competing risk of death in this population.
Disclosure: The authors have nothing
to disclose, and no relationship with
industry.
Funding: Self-funded
Ahmed Elkaryoni, MDa,*
Brett W. Sperry, MDb
Anna Royce, MDc
Kevin Walsh, MDd
Elizabeth Bruno, MDd
Subir Shah, DOa,d
Amir Darki, MD MSca,d
Islam Y. Elgendy, MDe
a
Division of Cardiovascular Disease, Loyola
University Medical Center, Loyola Stritch School of
Medicine, Maywood, Illinois
b
Division of Cardiovascular Disease, Mid America
Heart Institute, University of Missouri-Kansas City,
Kansas City, Missouri
c
Department of Internal Medicine, University of
Oklahoma, Oklahoma
d
Department of Internal Medicine, Loyola
University Medical Center, Loyola Stritch School of
Medicine, Maywood, Illinois
e
Divison of Cardiology, Weill Cornell MedicineQatar, Doha, Qatar
27 January 2021
1. Virani SS, Alonso A, Benjamin EJ, Bittencourt
MS, Callaway CW, Carson AP, Chamberlain
AM, Chang AR, Cheng S, Delling FN, Djousse
L, Elkind MSV, Ferguson JF, Fornage M, Khan
SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker
CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM,
Rosamond WD, Roth GA, Sampson UKA,
Satou GM, Schroeder EB, Shah SH, Shay CM,
Spartano NL, Stokes A, Tirschwell DL, VanWagner LB, Tsao CW, American Heart Association Council on Epidemiology and Prevention
Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics2020 update: a report from the American Heart
Association. Circulation 2020;141:e139–e596.
2. Diop MS, Bowen GS, Jiang L, Wu WC, Cornell
PY, Gozalo P, Rudolph JL...
DOI record:
{
"DOI": "10.1016/j.amjcard.2021.02.005",
"ISSN": [
"0002-9149"
],
"URL": "http://dx.doi.org/10.1016/j.amjcard.2021.02.005",
"alternative-id": [
"S0002914921001429"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Meta-analysis of the Effect of Colchicine on Mortality and Mechanical Ventilation in COVID-19"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "The American Journal of Cardiology"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.amjcard.2021.02.005"
},
{
"label": "Content Type",
"name": "content_type",
"value": "simple-article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "Published by Elsevier Inc."
}
],
"author": [
{
"affiliation": [],
"family": "Salah",
"given": "Husam M.",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-0384-2097",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mehta",
"given": "Jawahar L.",
"sequence": "additional"
}
],
"container-title": "The American Journal of Cardiology",
"container-title-short": "The American Journal of Cardiology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.jp",
"clinicalkey.com",
"ajconline.org",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.fr",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
2,
19
]
],
"date-time": "2021-02-19T20:30:37Z",
"timestamp": 1613766637000
},
"deposited": {
"date-parts": [
[
2021,
3,
23
]
],
"date-time": "2021-03-23T10:19:48Z",
"timestamp": 1616494788000
},
"indexed": {
"date-parts": [
[
2023,
5,
15
]
],
"date-time": "2023-05-15T09:12:35Z",
"timestamp": 1684141955158
},
"is-referenced-by-count": 19,
"issued": {
"date-parts": [
[
2021,
4
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
4,
1
]
],
"date-time": "2021-04-01T00:00:00Z",
"timestamp": 1617235200000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0002914921001429?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0002914921001429?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "170-172",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
4
]
]
},
"published-print": {
"date-parts": [
[
2021,
4
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1007/s40495-020-00225-6",
"article-title": "Colchicine in COVID-19: an old drug, new use",
"author": "Schlesinger",
"doi-asserted-by": "crossref",
"first-page": "137",
"journal-title": "Curr Pharmacol Rep",
"key": "10.1016/j.amjcard.2021.02.005_bib0001",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1016/j.yexcr.2009.08.020",
"article-title": "Microtubule-mediated NF-kappaB activation in the TNF-alpha signaling pathway",
"author": "Jackman",
"doi-asserted-by": "crossref",
"first-page": "3242",
"journal-title": "Exp Cell Res",
"key": "10.1016/j.amjcard.2021.02.005_bib0002",
"volume": "315",
"year": "2009"
},
{
"DOI": "10.1002/cmdc.201800641",
"article-title": "Synthesis, biological evaluation, and molecular docking of combretastatin and colchicine derivatives and their hCE1-activated prodrugs as antiviral agents",
"author": "Richter",
"doi-asserted-by": "crossref",
"first-page": "469",
"journal-title": "ChemMedChem",
"key": "10.1016/j.amjcard.2021.02.005_bib0003",
"volume": "14",
"year": "2019"
},
{
"DOI": "10.1001/jamanetworkopen.2020.13136",
"article-title": "Effect of colchicine vs standard care on cardiac and inflammatory biomarkers and clinical outcomes in patients hospitalized with coronavirus disease 2019: the GRECCO-19 randomized clinical trial",
"author": "Deftereos",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw Open",
"key": "10.1016/j.amjcard.2021.02.005_bib0004",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1016/j.hjc.2020.11.012",
"article-title": "Impact of colchicine on mortality in patients with COVID-19. A meta-analysis",
"author": "Vrachatis",
"doi-asserted-by": "crossref",
"journal-title": "Hellenic J Cardiol",
"key": "10.1016/j.amjcard.2021.02.005_bib0005",
"year": "2021"
},
{
"DOI": "10.1136/annrheumdis-2020-217712",
"article-title": "Association between treatment with colchicine and improved survival in a single-centre cohort of adult hospitalised patients with COVID-19 pneumonia and acute respiratory distress syndrome",
"author": "Scarsi",
"doi-asserted-by": "crossref",
"first-page": "1286",
"journal-title": "Ann Rheum Dis",
"key": "10.1016/j.amjcard.2021.02.005_bib0006",
"volume": "79",
"year": "2020"
},
{
"DOI": "10.1155/2020/8865954",
"article-title": "A case control study to evaluate the impact of colchicine on patients admitted to the hospital with moderate to severe COVID-19 infection",
"author": "Sandhu",
"doi-asserted-by": "crossref",
"journal-title": "Can J Infect Dis Med Microbiol",
"key": "10.1016/j.amjcard.2021.02.005_bib0007",
"volume": "2020",
"year": "2020"
},
{
"article-title": "Beneficial effects of colchicine for moderate to severe COVID-19: an interim analysis of a randomized, double-blinded, placebo controlled clinical trial",
"author": "Lopes",
"journal-title": "medRxiv",
"key": "10.1016/j.amjcard.2021.02.005_bib0008",
"year": "2020"
},
{
"DOI": "10.5005/jp-journals-10071-23599",
"article-title": "A retrospective observational study of hypoxic COVID-19 patients treated with immunomodulatory drugs in a Tertiary Care Hospital",
"author": "Mahale",
"doi-asserted-by": "crossref",
"first-page": "1020",
"journal-title": "Indian J Crit Care Med",
"key": "10.1016/j.amjcard.2021.02.005_bib0009",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.3390/jcm9092961",
"article-title": "Colchicine to weather the cytokine storm in hospitalized patients with COVID-19",
"author": "Brunetti",
"doi-asserted-by": "crossref",
"first-page": "2961",
"journal-title": "J Clin Med",
"key": "10.1016/j.amjcard.2021.02.005_bib0010",
"volume": "9",
"year": "2020"
},
{
"article-title": "Efficacy of colchicine in non-hospitalized patients with COVID-19",
"author": "Tardif",
"journal-title": "medRxiv",
"key": "10.1016/j.amjcard.2021.02.005_bib0011",
"year": "2021"
},
{
"article-title": "Clinical outcome of patients with COVID-19 pneumonia treated with corticosteroids and colchicine in Colombia",
"author": "Pinzón MA",
"journal-title": "Res Sqaure",
"key": "10.1016/j.amjcard.2021.02.005_bib0012",
"year": "2020"
}
],
"reference-count": 12,
"references-count": 12,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0002914921001429"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cardiology and Cardiovascular Medicine"
],
"subtitle": [],
"title": "Meta-analysis of the Effect of Colchicine on Mortality and Mechanical Ventilation in COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "145"
}
