Association of COVID-19 Infection with Sociodemographic, Anthropometric and Lifestyle Factors: A Cross-Sectional Study in an Older Adults’ Population Aged over 65 Years Old
et al., Diseases, doi:10.3390/diseases11040165, Nov 2023
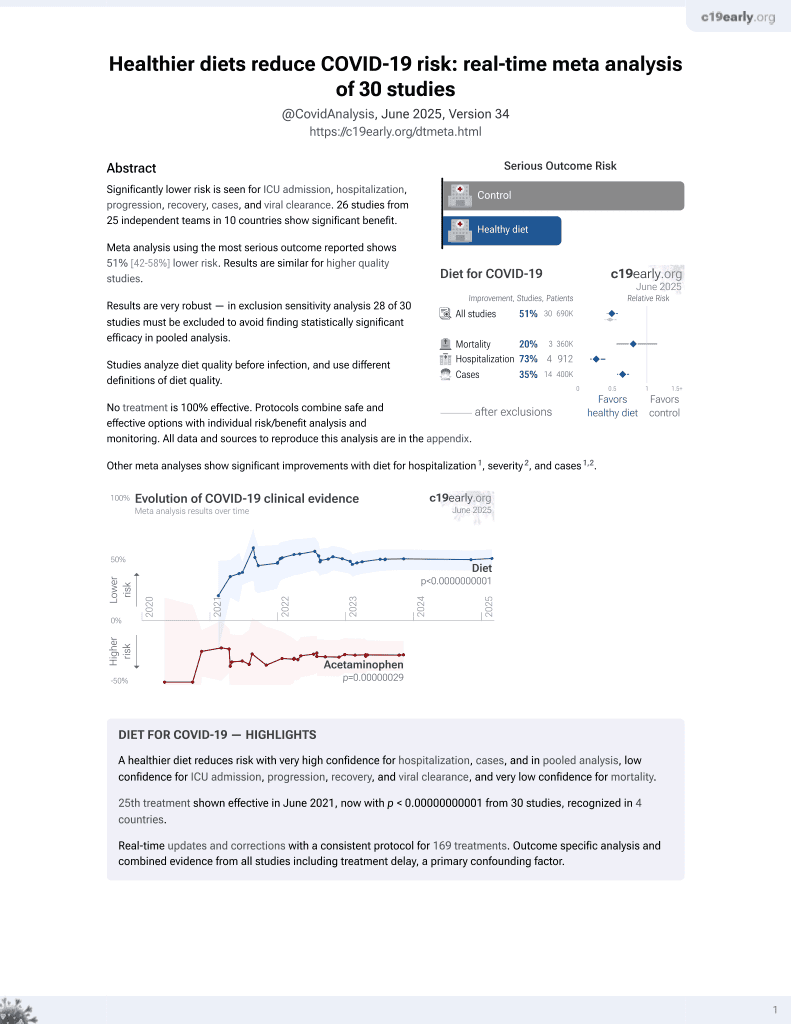
Diet for COVID-19
26th treatment shown to reduce risk in
June 2021, now with p < 0.00000000001 from 30 studies, recognized in 4 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 5,197 Greek adults over 65. After adjustment for confounders, COVID-19 infection was independently associated with poor sleep, low physical activity, low Mediterranean diet adherence, living in urban areas, smoking, obesity, depression, anxiety, stress, and poor health-related quality of life.
|
risk of case, 55.0% lower, OR 0.45, p < 0.001, higher quality diet 2,609, lower quality diet 2,588, adjusted per study, inverted to make OR<1 favor higher quality diet, moderate/high vs. very low/low Mediterranean diet adherence, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Pavlidou et al., 9 Nov 2023, retrospective, Greece, peer-reviewed, 14 authors.
Contact: souzpapa@gmail.com (corresponding author), elen.p.pavl@gmail.com, g.antasouras@gmail.com, rd.olga.alexatou@gmail.com, xeniaggelakou@hotmail.com, fnsd21013@fns.aegean.gr, cgiaginis@aegean.gr, tvorvola@med.duth.gr, gtsourouflis@med.uoa.gr, aserdari@yahoo.com, mgrammat@uth.gr, kvadikol@med.duth.gr, antonios.dakanalis@unimib.it, dlefa@yahoo.gr.
Association of COVID-19 Infection with Sociodemographic, Anthropometric and Lifestyle Factors: A Cross-Sectional Study in an Older Adults’ Population Aged over 65 Years Old
Diseases, doi:10.3390/diseases11040165
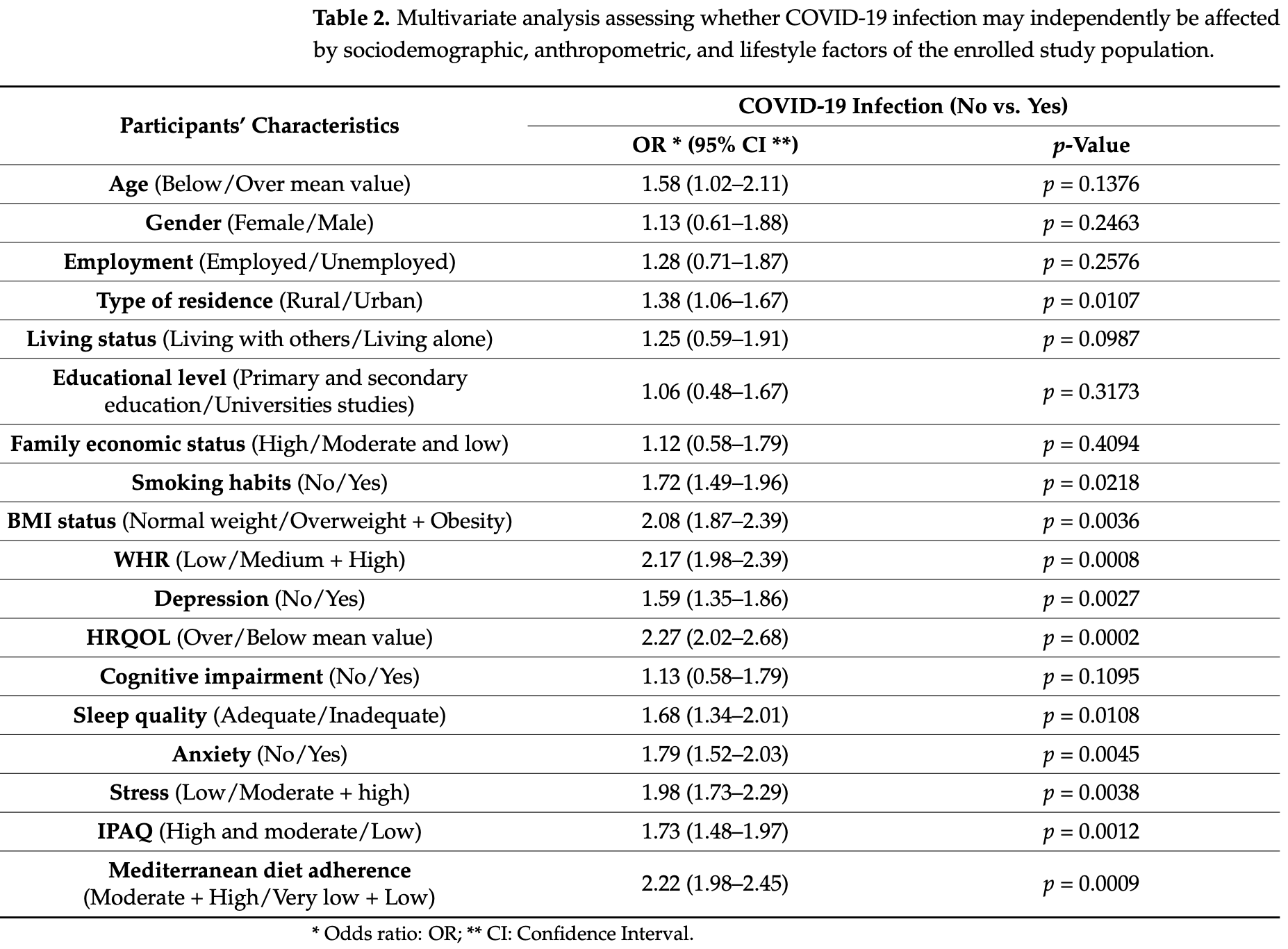
Background: The COVID-19 pandemic has led to unfavorable disruptions to daily living routines by exerting deleterious effects on several aspects of human mental and physical health and quality of life worldwide. The purpose of the current survey is to explore the potential association of COVID-19 infection with multiple sociodemographic, anthropometric, and lifestyle factors of community-dwelling older adults. Methods: This is a cross-sectional survey including 5197 older adults aged over 65 years old from 10 geographically diverse regions of Greece. Relevant questionnaires were used to record study the population sociodemographic factor, while anthropometric parameters were also measured. Validated questionnaires were also applied to assess several lifestyle factors such as depression, anxiety, stress, cognitive status, sleep quality, health-related quality of life, physical activity levels, and Mediterranean diet (MD) adherence. Results: In multivariate regression analysis, COVID-19 infection was significantly, independently related with urban residence (p = 0.0107), regular smoking (p = 0.0218), overweight status and obesity (p = 0.0036), as well as abdominal obesity (p = 0.0008), higher risk of depression (p = 0.0027), anxiety (p = 0.0045), stress (p = 0.0038), inadequate sleep quality (p = 0.0108), lower physical activity levels (p = 0.0012), reduced MD compliance (p = 0.0009), and poor health-related quality of life (p = 0.0002). In univariate analysis, older adults' age (p = 0.0001), male gender (p = 0.0015), living alone (p = 0.0023), lower educational and economic level (p = 0.0175 and p = 0.0294, respectively), and cognition decline (p = 0.0032) were also related with the presence of COVID-19 infection; however, these associations were considerably attenuated at a non-significant level by adjustment for several confounders in multivariate analysis. Conclusions: This is one of the few available studies supporting evidence that COVID-19 infection
Conflicts of Interest: The authors declare no conflict of interest.
References
Ahmad, Rathore, Neurological manifestations and complications of COVID-19: A literature review, J. Clin. Neurosci, doi:10.1016/j.jocn.2020.05.017
Almanan, Raynor, Ogunsulire, Malyshkina, Mukherjee et al., IL-10-producing Tfh cells accumulate with age and link inflammation with age-related immune suppression, Sci. Adv, doi:10.1126/sciadv.abb0806
Andreo-López, Contreras-Bolívar, Muñoz-Torres, García-Fontana, García-Fontana, Influence of the Mediterranean Diet on Healthy Aging, Int. J. Mol. Sci, doi:10.3390/ijms24054491
Andreou, Alexopoulos, Lionis, Varvogli, Gnardellis et al., Perceived Stress Scale: Reliability and validity study in Greece, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph8083287
Angelidi, Kokkinos, Katechaki, Ros, Mantzoros, Mediterranean diet as a nutritional approach for COVID-19, Metabolism, doi:10.1016/j.metabol.2020.154407
Arevalo-Rodriguez, Smailagic, Roqué-Figuls, Ciapponi, Sanchez-Perez et al., Mini-Mental State Examination (MMSE) for the early detection of dementia in people with mild cognitive impairment (MCI), Cochrane Database Syst. Rev, doi:10.1002/14651858
Armitage, Nellums, COVID-19 and the consequences of isolating the elderly, Lancet Public Health, doi:10.1016/S2468-2667(20)30061-X
Arvaniti, Panagiotakos, Healthy indexes in public health practice and research: A review, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408390701326268
Asadi-Pooya, Simani, Central nervous system manifestations of COVID-19: A systematic review, J. Neurol. Sci, doi:10.1016/j.jns.2020.116832
Badenoch, Rengasamy, Watson, Jansen, Chakraborty et al., Persistent neuropsychiatric symptoms after COVID-19: A systematic review and meta-analysis, Brain Commun, doi:10.1093/braincomms/fcab297
Banerjee, Pantea Stoian, Silva-Nunes, Sonmez, Rizvi et al., The role of GLP-1 receptor agonists during COVID-19 pandemia: A hypothetical molecular mechanism, Expert Opin. Drug Saf
Barile, Horner-Johnson, Krahn, Zack, Miranda et al., Measurement characteristics for two health-related quality of life measures in older adults: The SF-36 and the CDC Healthy Days items, Disabil. Health J, doi:10.1016/j.dhjo.2016.04.008
Bergman, Cohen-Fridel, Shrira, Bodner, Palgi, COVID-19 health worries and anxiety symptoms among older adults: The moderating role of ageism, Int. Psychogeriatr, doi:10.1017/S1041610220001258
Bidzan-Bluma, Bidzan, Jurek, Bidzan, Knietzsch et al., A Polish and German Population Study of Quality of Life, Well-Being, and Life Satisfaction in Older Adults During the COVID-19 Pandemic, Front. Psychiatry, doi:10.3389/fpsyt.2020.585813
Boutari, Mantzoros, update on the epidemiology of obesity and a call to action: As its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on, Metabolism, doi:10.1016/j.metabol.2022.155217
Bouças, Rheinheimer, Lagopoulos, Why severe COVID-19 patients are at greater risk of developing depression: A molecular perspective, Neuroscientist, doi:10.1177/1073858420967892
Brooks, Webster, Smith, Woodland, Wessely et al., The psychological impact of quarantine and how to reduce it: Rapid review of the evidence, Lancet, doi:10.1016/S0140-6736(20)30460-8
Cacioppo, Hawkley, Thisted, Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study, Psychol. Aging, doi:10.1037/a0017216
Carriedo, Cecchini, Fernandez-Rio, Méndez-Giménez, Psychological Well-being and Physical Activity Levels in Older Adults During the Nationwide Lockdown in Spain, Am. J. Geriatr. Psychiatry, doi:10.1016/j.jagp.2020.08.007
Chen, Zhou, Min, Mitochondria, Oxidative Stress and Innate Immunity, Front. Physiol, doi:10.3389/fphys.2018.01487
Choi, Oh, Jun, COVID-19 Obesity: Differences in Infection Risk Perception, Obesity Stress, Depression, and Intention to Participate in Leisure Sports Based on Weight Change, Healthcare, doi:10.3390/healthcare11040526
Cohen, Kamarck, Mermelstein, A global measure of perceived stress, J. Health Soc. Behav, doi:10.2307/2136404
Craig, Marshall, Sjöström, Bauman, Booth et al., International physical activity questionnaire: 12-country reliability and validity, Med. Sci. Sports Exerc, doi:10.1249/01.MSS.0000078924.61453.FB
De Pue, Gillebert, Dierckx, Vanderhasselt, De Raedt et al., The impact of the COVID-19 pandemic on wellbeing and cognitive functioning of older adults, Sci. Rep, doi:10.1038/s41598-021-84127-7
Delinasios, Fragkou, Gkirmpa, Tsangaris, Hoffman et al., The Experience of Greece as a Model to Contain COVID-19 Infection Spread, Vivo, doi:10.21873/invivo.12380
Deng, Zhou, Hou, Silver, Wong et al., The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: A meta-analysis, Ann. N. Y. Acad. Sci
Desai, Patel, Stopping the spread of COVID-19, J. Am. Med. Assoc, doi:10.1001/jama.2020.4269
El Khoury, Julien, Inverse Association Between the Mediterranean Diet and COVID-19 Risk in Lebanon: A Case-Control Study, Front. Nutr, doi:10.3389/fnut.2021.707359
Filatov, Sharma, Hindi, Espinosa, Neurological Complications of Coronavirus Disease (COVID-19): Encephalopathy, Cureus, doi:10.7759/cureus.7352
Finicelli, Di Salle, Galderisi, Peluso, The Mediterranean Diet: An Update of the Clinical Trials, Nutrients, doi:10.3390/nu14142956
Fountoulakis, Tsolaki, Chantzi, Kazis, Mini Mental State Examination (MMSE): A validation study in Greece, Am. J. Alzheimer's Dis. Other Dement, doi:10.1177/153331750001500604
Fu, Wang, Yuan, Chen, Ao et al., Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis, J. Infect, doi:10.1016/j.jinf.2020.03.041
Gantenbein, Kanaka-Gantenbein, Mediterranean Diet as an Antioxidant: The Impact on Metabolic Health and Overall Wellbeing, Nutrients, doi:10.3390/nu13061951
Georgieva, Ananiev, Yovchev, Arabadzhiev, Abrashev et al., COVID-19 Complications: Oxidative Stress, Inflammation, and Mitochondrial and Endothelial Dysfunction, Int. J. Mol. Sci, doi:10.3390/ijms241914876
Grossman, Hoffman, Palgi, Shrira, COVID-19 related loneliness and sleep problems in older adults: Worries and resilience as potential moderators, Pers. Individ. Dif, doi:10.1016/j.paid.2020.110371
Holaday, Oladele, Miller, Dueñas, Roy et al., Loneliness, sadness, and feelings of social disconnection in older adults during the COVID-19 pandemic, J. Am. Geriatr. Soc, doi:10.1111/jgs.17599
Hossain, Sultana, Purohit, Mental health outcomes of quarantine and isolation for infection prevention: A systematic umbrella review of the global evidence, Epidemiol. Health, doi:10.4178/epih.e2020038
Huang, Lu, Huang, Wang, Ling et al., Obesity in patients with COVID-19: A systematic review and meta-analysis, Metabolism, doi:10.1016/j.metabol.2020.154378
Jee, WHO International Health Regulations Emergency Committee for the COVID-19 outbreak, Epidemiol. Health, doi:10.4178/epih.e2020013
Kaim, Saban, Dynamic Trends in Sociodemographic Disparities and COVID-19 Morbidity and Mortality-A Nationwide Study during Two Years of a Pandemic, Healthcare, doi:10.3390/healthcare11070933
Khan, Sultana, Hossain, Hasan, Ahmed et al., The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study, J. Affect. Disord, doi:10.1016/j.jad.2020.07.135
Khaskheli, Wang, Hussain, Butt, Yan et al., Global law, policy, and governance for effective prevention and control of COVID-19: A comparative analysis of the law and policy of Pakistan, China, and Russia, Front. Public Health, doi:10.3389/fpubh.2022.1035536
Kim, Rebholz, Hegde, Lafiura, Raghavan et al., Plant-based diets, pescatarian diets and COVID-19 severity: A population-based case-control study in six countries, BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2021-000272
Klok, Boon, Barco, Endres, Geelhoed et al., The Post-COVID-19 Functional Status scale: A tool to measure functional status over time after COVID-19, Eur. Respir. J, doi:10.1183/13993003.01494-2020
Knuutila, Rautiainen, Lehti, Karppinen, Kautiainen et al., Impact of the COVID-19 Pandemic on Older People's Loneliness: Findings from a Longitudinal Study between 2019 and 2021 among Older Home-Dwellers in Finland, J. Nutr. Health Aging, doi:10.1007/s12603-023-1949-2
Kotwal, Cenzer, Waite, Covinsky, Perissinotto et al., The epidemiology of social isolation and loneliness among older adults during the last years of life, J. Am. Geriatr. Soc, doi:10.1111/jgs.17366
Krishnamoorthy, Rajaa, Rehman, Diagnostic accuracy of various forms of geriatric depression scale for screening of depression among older adults: Systematic review and meta-analysis, Arch. Gerontol. Geriatr, doi:10.1016/j.archger.2019.104002
Köverová, Ráczová, Kováčová Holevová, Predictors of Anxiety, Stress, and Concern of COVID-19 Infection in Older Adults During the First and the Second Waves of the COVID-19 Pandemic in Slovakia, Gerontol. Geriatr. Med, doi:10.1177/23337214211047642
Leeming, Johnson, Spector, Le Roy, Effect of Diet on the Gut Microbiota: Rethinking Intervention Duration, Nutrients, doi:10.3390/nu11122862
Liu, Chen, Lin, Han, Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients, J. Infect, doi:10.1016/j.jinf.2020.03.005
Lordan, Rando, Greene, Dietary Supplements and Nutraceuticals under Investigation for COVID-19 Prevention and Treatment, mSystems, doi:10.1128/mSystems.00122-21
Maiorino, Bellastella, Longo, Caruso, Esposito, Mediterranean Diet and COVID-19: Hypothesizing Potential Benefits in People with Diabetes, Front. Endocrinol, doi:10.3389/fendo.2020.574315
Mamelund, A socially neutral disease? Individual social class, household wealth and mortality from Spanish influenza in two socially contrasting parishes in Kristiania 1918-19, Soc. Sci. Med, doi:10.1016/j.socscimed.2005.06.051
Maracy, Rahimi, Shahraki, A survey of knowledge, attitude and practice of the older people about COVID-19 pandemic in Isfahan, Iran, J. Gerontol. Geriatr, doi:10.36150/2499-6564-253
Martins, Ferreira, Fernandes, Vieira, Fontes et al., Depressive and Anxiety Symptoms in Severe COVID-19 Survivors: A Prospective Cohort Study, Psychiatr. Q, doi:10.1007/s11126-022-09998-z
Mazza, Ricci, Biondi, Colasanti, Ferracuti et al., A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph17093165
Merino, Joshi, Nguyen, Leeming, Mazidi et al., Diet quality and risk and severity of COVID-19: A prospective cohort study, Gut, doi:10.1136/gutjnl-2021-325353
Minihan, Orben, Songco, Fox, Ladouceur et al., Social determinants of mental health during a year of the COVID-19 pandemic, Dev. Psychopathol, doi:10.1017/S0954579422000396
Mohammadkhanizadeh, Nikbakht, Investigating the potential mechanisms of depression induced-by COVID-19 infection in patients, J. Clin. Neurosci, doi:10.1016/j.jocn.2021.07.023
Morrow-Howell, Galucia, Swinford, Recovering from the COVID-19 Pandemic: A Focus on Older Adults, J. Aging Soc. Policy, doi:10.1080/08959420.2020.1759758
Mortaz, Bezemer, Alipoor, Varahram, Mumby et al., Nutritional Impact and Its Potential Consequences on Covid-19 Severity, Front. Nutr, doi:10.3389/fnut.2021.698617
Mrityunjaya, Pavithra, Neelam, Janhavi, Halami et al., Immune-Boosting, Antioxidant and Anti-Inflammatory Food Supplements Targeting Pathogenesis of COVID-19, Front. Immunol, doi:10.3389/fimmu.2020.570122
Naser Abed, Kassab, Al-Zamali, Mahdi Muslim, The epidemiological profile associated with lifestyle risk factors and nutritional status for COVID-19 patients in the Iraqi population, J. Public Health Afr, doi:10.4081/jphia.2023.2323
Olgun Yıldızeli, Kocakaya, Saylan, Tastekin, Yıldız et al., Depression, and Sleep Disorders after COVID-19 Infection, Cureus, doi:10.7759/cureus.42637
Paces, Strizova, Smrz, Cerny, COVID-19 and the Immune System, Physiol. Res, doi:10.33549/physiolres.934492
Panagiotakos, Pitsavos, Stefanadis, Dietary patterns: A Mediterranean diet score and its relation to clinical and bio-logical markers of cardiovascular disease risk, Nutr. Metab. Cardiovasc. Dis, doi:10.1016/j.numecd.2005.08.006
Parker, Shalev, Hsu, Shenoy, Cheung et al., Anxiety, and Acute Stress Disorder among Patients Hospitalized with COVID-19: A Prospective Cohort Study, J. Acad. Consult. Liaison Psychiatry, doi:10.1016/j.psym.2020.10.001
Perez-Araluce, Martinez-Gonzalez, Fernández-Lázaro, Bes-Rastrollo, Gea et al., Mediterranean diet and the risk of COVID-19 in the 'Seguimiento Universidad de Navarra' cohort, Clin. Nutr, doi:10.1016/j.clnu.2021.04.001
Perez-Araluce, Martínez-González, Gea, Carlos, Components of the Mediterranean Diet and Risk of COVID-19, Front. Nutr, doi:10.3389/fnut.2021.805533
Perracini, De Amorim, Lima, Da Silva, Trombini-Souza et al., Impact of COVID-19 Pandemic on Life-Space Mobility of Older Adults Living in Brazil: REMOBILIZE Study, Front. Public Health, doi:10.3389/fpubh.2021.643640
Ponzo, Pellegrini, D'eusebio, Bioletto, Goitre et al., Mediterranean Diet and SARS-COV-2 Infection: Is There Any Association? A Proof-of-Concept Study, Nutrients, doi:10.3390/nu13051721
Ramezani, Simani, Karimialavijeh, Rezaei, Hajiesmaeili et al., The Role of Anxiety and Cortisol in Outcomes of Patients with COVID-19, Basic Clin. Neurosci, doi:10.32598/bcn.11.covid19.1168.2
Rashid, Syed Mohamad, Tajjudin, Roslan, Jaffar et al., COVID-19 Pandemic Fatigue and Its Sociodemographic, Mental Health Status, and Perceived Causes: A Cross-Sectional Study Nearing the Transition to an Endemic Phase in Malaysia, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph20054476
Restrepo, Obesity Prevalence Among, Adults During the COVID-19 Pandemic, Am. J. Prev. Med, doi:10.1016/j.amepre.2022.01.012
Rieder, Wyse, Regulation of Inflammation by IRAK-M Pathway Can Be Associated with nAchRalpha7 Activation and COVID-19, Mol. Neurobiol, doi:10.1007/s12035-023-03567-6
Rishi, Thakur, Vij, Rishi, Singh et al., Gut Microbiota and COVID-19, Indian J. Microbiol, doi:10.1007/s12088-020-00908-0
Robb, De Jager, Ahmadi-Abhari, Giannakopoulou, Udeh-Momoh et al., Associations of Social Isolation with Anxiety and Depression During the Early COVID-19 Pandemic: A Survey of Older Adults in London, UK, Front. Psychiatry, doi:10.3389/fpsyt.2020.591120
Rogers, Chesney, Oliver, Pollak, Mcguire et al., Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic, Lancet Psychiatry, doi:10.1016/S2215-0366(20)30203-0
Rutter, Mytton, Mak, Donaldson, Socio-economic disparities in mortality due to pandemic influenza in England, Int. J. Public Health, doi:10.1007/s00038-012-0337-1
Salahuddin, Maru, Kumalo, Pandi-Perumal, Bahammam et al., Validation of the Pittsburgh sleep quality index in community dwelling Ethiopian adults, Health Qual. Life Outcomes, doi:10.1186/s12955-017-0637-5
Sharma, Di Castelnuovo, Costanzo, Persichillo, Panzera et al., Habitual adherence to a traditional Mediterranean diet and risk of SARS-CoV-2 infection and Coronavirus disease 2019 (COVID-19): A longitudinal analysis, Int. J. Food Sci. Nutr, doi:10.1080/09637486.2023.2212879
Sideli, Lo Coco, Bonfanti, Borsarini, Fortunato et al., Effects of COVID-19 lockdown on eating disorders and obesity: A systematic review and meta-analysis, Eur. Eat. Disord. Rev, doi:10.1002/erv.2861
Sidor, Rzymski, Dietary choices and habits during COVID-19 lockdown: Experience from Poland, Nutrients, doi:10.3390/nu12061657
Sousa Moreira, Barbosa, Vieira, Chaves, Felix et al., The psychiatric and neuropsychiatric repercussions associated with severe infections of COVID-19 and other coronaviruses, Prog. Neuropsychopharmacol. Biol. Psychiatry, doi:10.1016/j.pnpbp.2020.110159
Syed Elias, Rohinmi, Knowledge, attitudes, and sociodemographic factors related to COVID-19 among older people living in the community in Malaysia, J. Educ. Health Promot, doi:10.4103/jehp.jehp_1637_21
Tan, Chin, Sathapan, Dewi, Amini et al., Mental Health and the COVID-19 Pandemic: Observational Evidence from Malaysia, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph20054046
Tee, Tee, Anlacan, Aligam, Reyes et al., Psychological impact of COVID-19 pandemic in the Philippines, J. Affect. Disord, doi:10.1016/j.jad.2020.08.043
Tluczek, Henriques, Brown, Support for the reliability and validity of a six-item state anxiety scale derived from the State-Trait Anxiety Inventory, J. Nurs. Meas, doi:10.1891/1061-3749.17.1.19
Tosato, Ciciarello, Zazzara, Janiri, Pais et al., Lifestyle Changes and Psychological Well-Being in Older Adults During COVID-19 Pandemic, Clin. Geriatr. Med, doi:10.1016/j.cger.2022.05.002
Tsigalou, Konstantinidis, Paraschaki, Stavropoulou, Voidarou et al., Mediterranean Diet as a Tool to Combat Inflammation and Chronic Diseases. An Overview, Biomedicine, doi:10.3390/biomedicines8070201
Uzunova, Pallanti, Hollander, Presentation and management of anxiety in individuals with acute symptomatic or asymptomatic COVID-19 infection, and in the post-COVID-19 recovery phase, Int. J. Psychiatry Clin. Pract, doi:10.1080/13651501.2021.1887264
Valtorta, Kanaan, Gilbody, Ronzi, Hanratty, Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies, Heart, doi:10.1136/heartjnl-2015-308790
Vassilopoulou, Bumbacea, Pappa, Papadopoulos, Bumbacea, Obesity and Infection: What Have We Learned from the COVID-19 Pandemic, Front. Nutr, doi:10.3389/fnut.2022.931313
Velayudhan, Aarsland, Ballard, Psychiatric and neuropsychiatric syndromes and COVID-19, Lancet Psychiatry, doi:10.1016/S2215-0366(20)30291-1
Vindegaard, Benros, COVID-19 pandemic and mental health consequences: Systematic review of the current evidence, Brain Behav. Immun, doi:10.1016/j.bbi.2020.05.048
Wang, Di, Ye, Wei, Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China, Psychol. Health Med, doi:10.1080/13548506.2020.1746817
Wang, Zhang, Luan, Social isolation, depression, nutritional status and quality of life during COVID-19 among Chinese community-dwelling older adults: A cross-sectional study, BMJ Open, doi:10.1136/bmjopen-2023-072305
Who Expert Consultation, Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies, Lancet, doi:10.1016/S0140-6736(03)15268-3
Wilson, Krueger, Arnold, Schneider, Kelly et al., Loneliness and risk of Alzheimer disease, Arch. Gen. Psychiatry, doi:10.1001/archpsyc.64.2.234
Wu, Mcgoogan, Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72,314 Cases from the Chinese Center for Disease Control and Prevention, JAMA, doi:10.1001/jama.2020.2648
Xie, Charness, Fingerman, Kaye, Kim et al., When Going Digital Becomes a Necessity: Ensuring Older Adults' Needs for Information, Services, and Social Inclusion During COVID-19, J. Aging Soc. Policy, doi:10.1080/08959420.2020.1771237
Xu, Wu, Jiang, Xu, Ying et al., Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-CoV-2) outside of Wuhan, China: Retrospective case series, BMJ, doi:10.1136/bmj.m606
Yan, Unprecedented pandemic, unprecedented shift, and unprecedented opportunity, Hum. Behav. Emerg. Technol, doi:10.1002/hbe2.192
Yang, Wang, Liu, Fu, Zhou et al., Obesity or increased body mass index and the risk of severe outcomes in patients with COVID-19: A protocol for systematic review and meta-analysis, Medicine, doi:10.1097/MD.0000000000028499
Zhu, Di Gessa, Zaninotto, Changes in health behaviours during the COVID-19 pandemic and effect on weight and obesity among older people in England, Sci. Rep, doi:10.1038/s41598-023-41391-z
Zhuang, Cai, Lu, Xu, Lin et al., Exploring Factors and Associate Responses for Anxiety in the Coronavirus Disease 2019 Pandemic: A Web-Based Survey in Japan, Front. Psychol, doi:10.3389/fpsyg.2021.795219
DOI record:
{
"DOI": "10.3390/diseases11040165",
"ISSN": [
"2079-9721"
],
"URL": "http://dx.doi.org/10.3390/diseases11040165",
"abstract": "<jats:p>Background: The COVID-19 pandemic has led to unfavorable disruptions to daily living routines by exerting deleterious effects on several aspects of human mental and physical health and quality of life worldwide. The purpose of the current survey is to explore the potential association of COVID-19 infection with multiple sociodemographic, anthropometric, and lifestyle factors of community-dwelling older adults. Methods: This is a cross-sectional survey including 5197 older adults aged over 65 years old from 10 geographically diverse regions of Greece. Relevant questionnaires were used to record study the population sociodemographic factor, while anthropometric parameters were also measured. Validated questionnaires were also applied to assess several lifestyle factors such as depression, anxiety, stress, cognitive status, sleep quality, health-related quality of life, physical activity levels, and Mediterranean diet (MD) adherence. Results: In multivariate regression analysis, COVID-19 infection was significantly, independently related with urban residence (p = 0.0107), regular smoking (p = 0.0218), overweight status and obesity (p = 0.0036), as well as abdominal obesity (p = 0.0008), higher risk of depression (p = 0.0027), anxiety (p = 0.0045), stress (p = 0.0038), inadequate sleep quality (p = 0.0108), lower physical activity levels (p = 0.0012), reduced MD compliance (p = 0.0009), and poor health-related quality of life (p = 0.0002). In univariate analysis, older adults’ age (p = 0.0001), male gender (p = 0.0015), living alone (p = 0.0023), lower educational and economic level (p = 0.0175 and p = 0.0294, respectively), and cognition decline (p = 0.0032) were also related with the presence of COVID-19 infection; however, these associations were considerably attenuated at a non-significant level by adjustment for several confounders in multivariate analysis. Conclusions: This is one of the few available studies supporting evidence that COVID-19 infection may be associated with diverse sociodemographic, anthropometric, and lifestyle factors in an older adults’ population in Greece. This study highlights the strong demand to provide psychological and nutritional counselling and support to older adults diagnosed with COVID-19 infection in order to ameliorate disease symptoms and severity, emphasizing the adaptation of healthy dietary and lifestyle habits as preventing and supplementary therapeutic factors against COVID-19.</jats:p>",
"alternative-id": [
"diseases11040165"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-7764-3544",
"affiliation": [
{
"name": "Department of Food Science and Nutrition, School of Environment, University of Aegean, 81400 Myrina, Greece"
}
],
"authenticated-orcid": false,
"family": "Pavlidou",
"given": "Eleni",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-6408-6128",
"affiliation": [
{
"name": "Department of Nutritional Sciences and Dietetics, School of Health Sciences, International Hellenic University, 57400 Thessaloniki, Greece"
}
],
"authenticated-orcid": false,
"family": "Papadopoulou",
"given": "Sousana K.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Food Science and Nutrition, School of Environment, University of Aegean, 81400 Myrina, Greece"
}
],
"family": "Antasouras",
"given": "Georgios",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Geriatric Psychiatry, University Hospital of Alexandroupolis, Democritus University of Thrace, 68100 Alexandoupoli, Greece"
}
],
"family": "Vorvolakos",
"given": "Theofanis",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Food Science and Nutrition, School of Environment, University of Aegean, 81400 Myrina, Greece"
}
],
"family": "Alexatou",
"given": "Olga",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Second Department of Propedeutic Surgery, Medical School, National and Kapodistrian University of Athens, 11527 Athens, Greece"
}
],
"family": "Tsourouflis",
"given": "Gerasimos",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Food Science and Nutrition, School of Environment, University of Aegean, 81400 Myrina, Greece"
}
],
"family": "Angelakou",
"given": "Exakousti-Petroula",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Psychiatry and Child Psychiatry, University Hospital of Alexandroupolis, Democritus University of Thrace, 68100 Alexandroupoli, Greece"
}
],
"family": "Serdari",
"given": "Aspasia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4167-6595",
"affiliation": [
{
"name": "Unit of Immunonutrition and Clinical Nutrition, Department of Rheumatology and Clinical Immunology, School of Health Sciences, Faculty of Medicine, University of Thessaly, 41110 Larissa, Greece"
}
],
"authenticated-orcid": false,
"family": "Grammatikopoulou",
"given": "Maria G.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Food Science and Nutrition, School of Environment, University of Aegean, 81400 Myrina, Greece"
}
],
"family": "Psara",
"given": "Evmorfia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Neurology, School of Medicine, Democritus University of Thrace, 68100 Alexandroupoli, Greece"
}
],
"family": "Vadikolias",
"given": "Konstantinos",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2328-3862",
"affiliation": [
{
"name": "Department of Mental Health and Addiction, Fondazione IRCCS San Gerardo dei Tintori, 20900 Monza, Italy"
},
{
"name": "Department of Medicine and Surgery, University of Milan Bicocca, Via Cadore 38, 20900 Monza, Italy"
}
],
"authenticated-orcid": false,
"family": "Dakanalis",
"given": "Antonios",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Oral and Maxillofacial Surgery, Medical School, Attikon Hospital, National and Kapodistrian University of Athens, Chaidari, 12462 Athens, Greece"
}
],
"family": "Lefantzis",
"given": "Nikolaos",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2878-4831",
"affiliation": [
{
"name": "Department of Food Science and Nutrition, School of Environment, University of Aegean, 81400 Myrina, Greece"
}
],
"authenticated-orcid": false,
"family": "Giaginis",
"given": "Constantinos",
"sequence": "additional"
}
],
"container-title": "Diseases",
"container-title-short": "Diseases",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
11,
9
]
],
"date-time": "2023-11-09T13:08:58Z",
"timestamp": 1699535338000
},
"deposited": {
"date-parts": [
[
2023,
11,
9
]
],
"date-time": "2023-11-09T15:08:07Z",
"timestamp": 1699542487000
},
"indexed": {
"date-parts": [
[
2023,
11,
10
]
],
"date-time": "2023-11-10T00:34:44Z",
"timestamp": 1699576484253
},
"is-referenced-by-count": 0,
"issue": "4",
"issued": {
"date-parts": [
[
2023,
11,
9
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2023,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
11,
9
]
],
"date-time": "2023-11-09T00:00:00Z",
"timestamp": 1699488000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2079-9721/11/4/165/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "165",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
11,
9
]
]
},
"published-online": {
"date-parts": [
[
2023,
11,
9
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref_1",
"unstructured": "World Health Organization (2023, March 14). WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020."
},
{
"key": "ref_2",
"unstructured": "World Health Organization (2023, March 22). WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int."
},
{
"DOI": "10.1002/hbe2.192",
"article-title": "Unprecedented pandemic, unprecedented shift, and unprecedented opportunity",
"author": "Yan",
"doi-asserted-by": "crossref",
"first-page": "110",
"journal-title": "Hum. Behav. Emerg. Technol.",
"key": "ref_3",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30460-8",
"article-title": "The psychological impact of quarantine and how to reduce it: Rapid review of the evidence",
"author": "Brooks",
"doi-asserted-by": "crossref",
"first-page": "912",
"journal-title": "Lancet",
"key": "ref_4",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1002/erv.2861",
"article-title": "Effects of COVID-19 lockdown on eating disorders and obesity: A systematic review and meta-analysis",
"author": "Sideli",
"doi-asserted-by": "crossref",
"first-page": "826",
"journal-title": "Eur. Eat. Disord. Rev.",
"key": "ref_5",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1080/13548506.2020.1746817",
"article-title": "Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "13",
"journal-title": "Psychol. Health Med.",
"key": "ref_6",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.31234/osf.io/64v7x",
"doi-asserted-by": "crossref",
"key": "ref_7",
"unstructured": "Minihan, S., Orben, A., Songco, A., Fox, E., Ladouceur, C.D., Mewton, L., Moulds, M., Pfeifer, J.H., Van Harmelen, A.L., and Schweizer, S. (Dev. Psychopathol., 2022). Social determinants of mental health during a year of the COVID-19 pandemic, Dev. Psychopathol., online ahead of print."
},
{
"DOI": "10.1001/jama.2020.4269",
"article-title": "Stopping the spread of COVID-19",
"author": "Desai",
"doi-asserted-by": "crossref",
"first-page": "1516",
"journal-title": "J. Am. Med. Assoc.",
"key": "ref_8",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2022.1035536",
"article-title": "Global law, policy, and governance for effective prevention and control of COVID-19: A comparative analysis of the law and policy of Pakistan, China, and Russia",
"author": "Khaskheli",
"doi-asserted-by": "crossref",
"first-page": "1035536",
"journal-title": "Front. Public Health",
"key": "ref_9",
"volume": "10",
"year": "2022"
},
{
"article-title": "The epidemiological profile associated with lifestyle risk factors and nutritional status for COVID-19 patients in the Iraqi population",
"first-page": "2323",
"journal-title": "J. Public Health Afr.",
"key": "ref_10",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.3390/healthcare11070933",
"doi-asserted-by": "crossref",
"key": "ref_11",
"unstructured": "Kaim, A., and Saban, M. (2023). Dynamic Trends in Sociodemographic Disparities and COVID-19 Morbidity and Mortality—A Nationwide Study during Two Years of a Pandemic. Healthcare, 11."
},
{
"DOI": "10.1016/j.socscimed.2005.06.051",
"article-title": "A socially neutral disease? Individual social class, household wealth and mortality from Spanish influenza in two socially contrasting parishes in Kristiania 1918–19",
"author": "Mamelund",
"doi-asserted-by": "crossref",
"first-page": "923",
"journal-title": "Soc. Sci. Med.",
"key": "ref_12",
"volume": "62",
"year": "2006"
},
{
"DOI": "10.1007/s00038-012-0337-1",
"article-title": "Socio-economic disparities in mortality due to pandemic influenza in England",
"author": "Rutter",
"doi-asserted-by": "crossref",
"first-page": "745",
"journal-title": "Int. J. Public Health",
"key": "ref_13",
"volume": "57",
"year": "2012"
},
{
"DOI": "10.1111/jgs.17599",
"article-title": "Loneliness, sadness, and feelings of social disconnection in older adults during the COVID-19 pandemic",
"author": "Holaday",
"doi-asserted-by": "crossref",
"first-page": "329",
"journal-title": "J. Am. Geriatr. Soc.",
"key": "ref_14",
"volume": "70",
"year": "2022"
},
{
"DOI": "10.1016/S2468-2667(20)30061-X",
"article-title": "COVID-19 and the consequences of isolating the elderly",
"author": "Armitage",
"doi-asserted-by": "crossref",
"first-page": "e256",
"journal-title": "Lancet Public Health",
"key": "ref_15",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1136/heartjnl-2015-308790",
"article-title": "Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies",
"author": "Valtorta",
"doi-asserted-by": "crossref",
"first-page": "1009",
"journal-title": "Heart",
"key": "ref_16",
"volume": "102",
"year": "2016"
},
{
"DOI": "10.1037/a0017216",
"article-title": "Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study",
"author": "Cacioppo",
"doi-asserted-by": "crossref",
"first-page": "453",
"journal-title": "Psychol. Aging",
"key": "ref_17",
"volume": "25",
"year": "2010"
},
{
"DOI": "10.1001/archpsyc.64.2.234",
"article-title": "Loneliness and risk of Alzheimer disease",
"author": "Wilson",
"doi-asserted-by": "crossref",
"first-page": "234",
"journal-title": "Arch. Gen. Psychiatry",
"key": "ref_18",
"volume": "64",
"year": "2007"
},
{
"DOI": "10.1111/jgs.17366",
"article-title": "The epidemiology of social isolation and loneliness among older adults during the last years of life",
"author": "Kotwal",
"doi-asserted-by": "crossref",
"first-page": "3081",
"journal-title": "J. Am. Geriatr. Soc.",
"key": "ref_19",
"volume": "69",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.2648",
"article-title": "Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72,314 Cases from the Chinese Center for Disease Control and Prevention",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "1239",
"journal-title": "JAMA",
"key": "ref_20",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m606",
"article-title": "Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-CoV-2) outside of Wuhan, China: Retrospective case series",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "m606",
"journal-title": "BMJ",
"key": "ref_21",
"volume": "368",
"year": "2020"
},
{
"DOI": "10.4178/epih.e2020013",
"article-title": "WHO International Health Regulations Emergency Committee for the COVID-19 outbreak",
"author": "Jee",
"doi-asserted-by": "crossref",
"first-page": "e2020013",
"journal-title": "Epidemiol. Health",
"key": "ref_22",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.03.041",
"article-title": "Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis",
"author": "Fu",
"doi-asserted-by": "crossref",
"first-page": "656",
"journal-title": "J. Infect.",
"key": "ref_23",
"volume": "80",
"year": "2020"
},
{
"article-title": "Neurological Complications of Coronavirus Disease (COVID-19): Encephalopathy",
"author": "Filatov",
"first-page": "e7352",
"journal-title": "Cureus",
"key": "ref_24",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.jns.2020.116832",
"article-title": "Central nervous system manifestations of COVID-19: A systematic review",
"author": "Simani",
"doi-asserted-by": "crossref",
"first-page": "116832",
"journal-title": "J. Neurol. Sci.",
"key": "ref_25",
"volume": "413",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.03.005",
"article-title": "Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "e14",
"journal-title": "J. Infect.",
"key": "ref_26",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2020.05.048",
"article-title": "COVID-19 pandemic and mental health consequences: Systematic review of the current evidence",
"author": "Vindegaard",
"doi-asserted-by": "crossref",
"first-page": "531",
"journal-title": "Brain Behav. Immun.",
"key": "ref_27",
"volume": "89",
"year": "2020"
},
{
"DOI": "10.3390/ijerph17093165",
"doi-asserted-by": "crossref",
"key": "ref_28",
"unstructured": "Mazza, C., Ricci, E., Biondi, S., Colasanti, M., Ferracuti, S., Napoli, C., and Roma, P. (2020). A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health, 17."
},
{
"DOI": "10.3390/ijerph20054476",
"doi-asserted-by": "crossref",
"key": "ref_29",
"unstructured": "Abdul Rashid, M.R., Syed Mohamad, S.N., Tajjudin, A.I.A., Roslan, N., Jaffar, A., Mohideen, F.B.S., Addnan, F.H., Baharom, N., and Ithnin, M. (2023). COVID-19 Pandemic Fatigue and Its Sociodemographic, Mental Health Status, and Perceived Causes: A Cross-Sectional Study Nearing the Transition to an Endemic Phase in Malaysia. Int. J. Environ. Res. Public Health, 20."
},
{
"DOI": "10.3390/ijerph20054046",
"doi-asserted-by": "crossref",
"key": "ref_30",
"unstructured": "Tan, E.S.S., Chin, S.A.F.X., Sathapan, M.S.P., Dewi, A.D., Amini, F., Bustami, N.A., Tan, P.Y., Ho, Y.B., and Tan, C.K. (2023). Mental Health and the COVID-19 Pandemic: Observational Evidence from Malaysia. Int. J. Environ. Res. Public Health, 20."
},
{
"DOI": "10.1016/j.jad.2020.08.043",
"article-title": "Psychological impact of COVID-19 pandemic in the Philippines",
"author": "Tee",
"doi-asserted-by": "crossref",
"first-page": "379",
"journal-title": "J. Affect. Disord.",
"key": "ref_31",
"volume": "277",
"year": "2020"
},
{
"DOI": "10.1016/j.jad.2020.07.135",
"article-title": "The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study",
"author": "Khan",
"doi-asserted-by": "crossref",
"first-page": "121",
"journal-title": "J. Affect. Disord.",
"key": "ref_32",
"volume": "277",
"year": "2020"
},
{
"DOI": "10.1183/13993003.01494-2020",
"article-title": "The Post-COVID-19 Functional Status scale: A tool to measure functional status over time after COVID-19",
"author": "Klok",
"doi-asserted-by": "crossref",
"first-page": "2001494",
"journal-title": "Eur. Respir. J.",
"key": "ref_33",
"volume": "56",
"year": "2020"
},
{
"DOI": "10.4103/jehp.jehp_1637_21",
"article-title": "Knowledge, attitudes, and sociodemographic factors related to COVID-19 among older people living in the community in Malaysia",
"author": "Rohinmi",
"doi-asserted-by": "crossref",
"first-page": "298",
"journal-title": "J. Educ. Health Promot.",
"key": "ref_34",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.36150/2499-6564-253",
"article-title": "A survey of knowledge, attitude and practice of the older people about COVID-19 pandemic in Isfahan, Iran",
"author": "Maracy",
"doi-asserted-by": "crossref",
"first-page": "204",
"journal-title": "J. Gerontol. Geriatr.",
"key": "ref_35",
"volume": "68",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-84127-7",
"article-title": "The impact of the COVID-19 pandemic on wellbeing and cognitive functioning of older adults",
"author": "Gillebert",
"doi-asserted-by": "crossref",
"first-page": "4636",
"journal-title": "Sci. Rep.",
"key": "ref_36",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1080/08959420.2020.1771237",
"article-title": "When Going Digital Becomes a Necessity: Ensuring Older Adults’ Needs for Information, Services, and Social Inclusion During COVID-19",
"author": "Xie",
"doi-asserted-by": "crossref",
"first-page": "460",
"journal-title": "J. Aging Soc. Policy",
"key": "ref_37",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1080/08959420.2020.1759758",
"article-title": "Recovering from the COVID-19 Pandemic: A Focus on Older Adults",
"author": "Galucia",
"doi-asserted-by": "crossref",
"first-page": "526",
"journal-title": "J. Aging Soc. Policy",
"key": "ref_38",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1136/bmjopen-2023-072305",
"article-title": "Social isolation, depression, nutritional status and quality of life during COVID-19 among Chinese community-dwelling older adults: A cross-sectional study",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "e072305",
"journal-title": "BMJ Open",
"key": "ref_39",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1007/s12603-023-1949-2",
"article-title": "Impact of the COVID-19 Pandemic on Older People’s Loneliness: Findings from a Longitudinal Study between 2019 and 2021 among Older Home-Dwellers in Finland",
"author": "Knuutila",
"doi-asserted-by": "crossref",
"first-page": "619",
"journal-title": "J. Nutr. Health Aging",
"key": "ref_40",
"volume": "27",
"year": "2023"
},
{
"DOI": "10.1016/j.cger.2022.05.002",
"article-title": "Lifestyle Changes and Psychological Well-Being in Older Adults During COVID-19 Pandemic",
"author": "Tosato",
"doi-asserted-by": "crossref",
"first-page": "449",
"journal-title": "Clin. Geriatr. Med.",
"key": "ref_41",
"volume": "38",
"year": "2022"
},
{
"DOI": "10.3389/fpubh.2021.643640",
"article-title": "Impact of COVID-19 Pandemic on Life-Space Mobility of Older Adults Living in Brazil: REMOBILIZE Study",
"author": "Perracini",
"doi-asserted-by": "crossref",
"first-page": "643640",
"journal-title": "Front. Public Health",
"key": "ref_42",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.21873/invivo.12380",
"article-title": "The Experience of Greece as a Model to Contain COVID-19 Infection Spread",
"author": "Delinasios",
"doi-asserted-by": "crossref",
"first-page": "1285",
"journal-title": "In Vivo",
"key": "ref_43",
"volume": "35",
"year": "2021"
},
{
"key": "ref_44",
"unstructured": "(2023, February 12). National Organism of Public Health, Available online: https://eody.gov.gr/."
},
{
"DOI": "10.1016/S0140-6736(03)15268-3",
"doi-asserted-by": "crossref",
"key": "ref_45",
"unstructured": "WHO Expert Consultation (2004). Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet, 363, 157–163."
},
{
"key": "ref_46",
"unstructured": "World Health Organization (2023, March 11). Waist Circumference and Waist-Hip Ratio. Report of a WHO Expert Consultation. World Health Organization, Geneva. Available online: https://apps.who.int/iris/bitstream/handle/10665/44583/9789241501491_eng.pdf."
},
{
"DOI": "10.1016/j.archger.2019.104002",
"article-title": "Diagnostic accuracy of various forms of geriatric depression scale for screening of depression among older adults: Systematic review and meta-analysis",
"author": "Krishnamoorthy",
"doi-asserted-by": "crossref",
"first-page": "104002",
"journal-title": "Arch. Gerontol. Geriatr.",
"key": "ref_47",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.1016/j.dhjo.2016.04.008",
"article-title": "Measurement characteristics for two health-related quality of life measures in older adults: The SF-36 and the CDC Healthy Days items",
"author": "Barile",
"doi-asserted-by": "crossref",
"first-page": "567",
"journal-title": "Disabil. Health J.",
"key": "ref_48",
"volume": "9",
"year": "2016"
},
{
"DOI": "10.1177/153331750001500604",
"article-title": "Mini Mental State Examination (MMSE): A validation study in Greece",
"author": "Fountoulakis",
"doi-asserted-by": "crossref",
"first-page": "342",
"journal-title": "Am. J. Alzheimer’s Dis. Other Dement.",
"key": "ref_49",
"volume": "15",
"year": "2000"
},
{
"article-title": "Mini-Mental State Examination (MMSE) for the early detection of dementia in people with mild cognitive impairment (MCI)",
"author": "Smailagic",
"first-page": "CD010783",
"journal-title": "Cochrane Database Syst. Rev.",
"key": "ref_50",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1891/1061-3749.17.1.19",
"article-title": "Support for the reliability and validity of a six-item state anxiety scale derived from the State-Trait Anxiety Inventory",
"author": "Tluczek",
"doi-asserted-by": "crossref",
"first-page": "19",
"journal-title": "J. Nurs. Meas.",
"key": "ref_51",
"volume": "17",
"year": "2009"
},
{
"DOI": "10.3389/fpsyg.2021.795219",
"article-title": "Exploring Factors and Associate Responses for Anxiety in the Coronavirus Disease 2019 Pandemic: A Web-Based Survey in Japan",
"author": "Zhuang",
"doi-asserted-by": "crossref",
"first-page": "795219",
"journal-title": "Front. Psychol.",
"key": "ref_52",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.3390/ijerph8083287",
"article-title": "Perceived Stress Scale: Reliability and validity study in Greece",
"author": "Andreou",
"doi-asserted-by": "crossref",
"first-page": "3287",
"journal-title": "Int. J. Environ. Res. Public Health",
"key": "ref_53",
"volume": "8",
"year": "2011"
},
{
"DOI": "10.2307/2136404",
"article-title": "A global measure of perceived stress",
"author": "Cohen",
"doi-asserted-by": "crossref",
"first-page": "385",
"journal-title": "J. Health Soc. Behav.",
"key": "ref_54",
"volume": "24",
"year": "1983"
},
{
"DOI": "10.1186/s12955-017-0637-5",
"article-title": "Validation of the Pittsburgh sleep quality index in community dwelling Ethiopian adults",
"author": "Salahuddin",
"doi-asserted-by": "crossref",
"first-page": "58",
"journal-title": "Health Qual. Life Outcomes",
"key": "ref_55",
"volume": "15",
"year": "2017"
},
{
"DOI": "10.1249/01.MSS.0000078924.61453.FB",
"article-title": "International physical activity questionnaire: 12-country reliability and validity",
"author": "Craig",
"doi-asserted-by": "crossref",
"first-page": "1381",
"journal-title": "Med. Sci. Sports Exerc.",
"key": "ref_56",
"volume": "35",
"year": "2003"
},
{
"DOI": "10.1016/j.numecd.2005.08.006",
"article-title": "Dietary patterns: A Mediterranean diet score and its relation to clinical and bio-logical markers of cardiovascular disease risk",
"author": "Panagiotakos",
"doi-asserted-by": "crossref",
"first-page": "559",
"journal-title": "Nutr. Metab. Cardiovasc. Dis.",
"key": "ref_57",
"volume": "16",
"year": "2006"
},
{
"DOI": "10.1080/10408390701326268",
"article-title": "Healthy indexes in public health practice and research: A review",
"author": "Arvaniti",
"doi-asserted-by": "crossref",
"first-page": "317",
"journal-title": "Crit. Rev. Food Sci. Nutr.",
"key": "ref_58",
"volume": "48",
"year": "2008"
},
{
"DOI": "10.1016/j.jocn.2021.07.023",
"article-title": "Investigating the potential mechanisms of depression induced-by COVID-19 infection in patients",
"author": "Mohammadkhanizadeh",
"doi-asserted-by": "crossref",
"first-page": "283",
"journal-title": "J. Clin. Neurosci.",
"key": "ref_59",
"volume": "91",
"year": "2021"
},
{
"DOI": "10.1016/S2215-0366(20)30203-0",
"article-title": "Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic",
"author": "Rogers",
"doi-asserted-by": "crossref",
"first-page": "611",
"journal-title": "Lancet Psychiatry",
"key": "ref_60",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.jocn.2020.05.017",
"article-title": "Neurological manifestations and complications of COVID-19: A literature review",
"author": "Ahmad",
"doi-asserted-by": "crossref",
"first-page": "8",
"journal-title": "J. Clin. Neurosci.",
"key": "ref_61",
"volume": "77",
"year": "2020"
},
{
"DOI": "10.1016/j.psym.2020.10.001",
"article-title": "Depression, Anxiety, and Acute Stress Disorder among Patients Hospitalized with COVID-19: A Prospective Cohort Study",
"author": "Parker",
"doi-asserted-by": "crossref",
"first-page": "211",
"journal-title": "J. Acad. Consult. Liaison Psychiatry",
"key": "ref_62",
"volume": "62",
"year": "2021"
},
{
"DOI": "10.1177/1073858420967892",
"article-title": "Why severe COVID-19 patients are at greater risk of developing depression: A molecular perspective",
"author": "Rheinheimer",
"doi-asserted-by": "crossref",
"first-page": "11",
"journal-title": "Neuroscientist",
"key": "ref_63",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.32598/bcn.11.covid19.1168.2",
"article-title": "The Role of Anxiety and Cortisol in Outcomes of Patients with COVID-19",
"author": "Ramezani",
"doi-asserted-by": "crossref",
"first-page": "179",
"journal-title": "Basic Clin. Neurosci.",
"key": "ref_64",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1111/nyas.14506",
"article-title": "The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: A meta-analysis",
"author": "Deng",
"doi-asserted-by": "crossref",
"first-page": "90",
"journal-title": "Ann. N. Y. Acad. Sci.",
"key": "ref_65",
"volume": "1486",
"year": "2021"
},
{
"DOI": "10.1080/13651501.2021.1887264",
"article-title": "Presentation and management of anxiety in individuals with acute symptomatic or asymptomatic COVID-19 infection, and in the post-COVID-19 recovery phase",
"author": "Uzunova",
"doi-asserted-by": "crossref",
"first-page": "115",
"journal-title": "Int. J. Psychiatry Clin. Pract.",
"key": "ref_66",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1016/j.pnpbp.2020.110159",
"doi-asserted-by": "crossref",
"key": "ref_67",
"unstructured": "De Sousa Moreira, J.L., Barbosa, S.M.B., Vieira, J.G., Chaves, N.C.B., Felix, E.B.G., Feitosa, P.W.G., da Cruz, I.S., da Silva, C.G.L., and Neto, M.L.R. (2021). The psychiatric and neuropsychiatric repercussions associated with severe infections of COVID-19 and other coronaviruses. Prog. Neuropsychopharmacol. Biol. Psychiatry., 106."
},
{
"DOI": "10.1016/S2215-0366(20)30291-1",
"article-title": "Psychiatric and neuropsychiatric syndromes and COVID-19",
"author": "Velayudhan",
"doi-asserted-by": "crossref",
"first-page": "663",
"journal-title": "Lancet Psychiatry",
"key": "ref_68",
"volume": "7",
"year": "2020"
},
{
"article-title": "Predictors of Anxiety, Stress, and Concern of COVID-19 Infection in Older Adults During the First and the Second Waves of the COVID-19 Pandemic in Slovakia",
"first-page": "23337214211047642",
"journal-title": "Gerontol. Geriatr. Med.",
"key": "ref_69",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1017/S1041610220001258",
"article-title": "COVID-19 health worries and anxiety symptoms among older adults: The moderating role of ageism",
"author": "Bergman",
"doi-asserted-by": "crossref",
"first-page": "1371",
"journal-title": "Int. Psychogeriatr.",
"key": "ref_70",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1016/j.jagp.2020.08.007",
"article-title": "COVID-19, Psychological Well-being and Physical Activity Levels in Older Adults During the Nationwide Lockdown in Spain",
"author": "Carriedo",
"doi-asserted-by": "crossref",
"first-page": "1146",
"journal-title": "Am. J. Geriatr. Psychiatry",
"key": "ref_71",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.3389/fpsyt.2020.591120",
"article-title": "Associations of Social Isolation with Anxiety and Depression During the Early COVID-19 Pandemic: A Survey of Older Adults in London, UK",
"author": "Robb",
"doi-asserted-by": "crossref",
"first-page": "591120",
"journal-title": "Front. Psychiatry",
"key": "ref_72",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3389/fpsyt.2020.585813",
"article-title": "A Polish and German Population Study of Quality of Life, Well-Being, and Life Satisfaction in Older Adults During the COVID-19 Pandemic",
"author": "Bidzan",
"doi-asserted-by": "crossref",
"first-page": "585813",
"journal-title": "Front. Psychiatry",
"key": "ref_73",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.paid.2020.110371",
"article-title": "COVID-19 related loneliness and sleep problems in older adults: Worries and resilience as potential moderators",
"author": "Grossman",
"doi-asserted-by": "crossref",
"first-page": "110371",
"journal-title": "Pers. Individ. Dif.",
"key": "ref_74",
"volume": "168",
"year": "2021"
},
{
"article-title": "Anxiety, Depression, and Sleep Disorders after COVID-19 Infection",
"author": "Kocakaya",
"first-page": "e42637",
"journal-title": "Cureus",
"key": "ref_75",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1093/braincomms/fcab297",
"article-title": "Persistent neuropsychiatric symptoms after COVID-19: A systematic review and meta-analysis",
"author": "Badenoch",
"doi-asserted-by": "crossref",
"first-page": "fcab297",
"journal-title": "Brain Commun.",
"key": "ref_76",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1007/s11126-022-09998-z",
"article-title": "Depressive and Anxiety Symptoms in Severe COVID-19 Survivors: A Prospective Cohort Study",
"author": "Martins",
"doi-asserted-by": "crossref",
"first-page": "891",
"journal-title": "Psychiatr. Q.",
"key": "ref_77",
"volume": "93",
"year": "2022"
},
{
"DOI": "10.4178/epih.e2020038",
"article-title": "Mental health outcomes of quarantine and isolation for infection prevention: A systematic umbrella review of the global evidence",
"author": "Hossain",
"doi-asserted-by": "crossref",
"first-page": "e2020038",
"journal-title": "Epidemiol. Health",
"key": "ref_78",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.3390/healthcare11040526",
"doi-asserted-by": "crossref",
"key": "ref_79",
"unstructured": "Choi, C., Oh, K.R., and Jun, M.G. (2023). COVID-19 Obesity: Differences in Infection Risk Perception, Obesity Stress, Depression, and Intention to Participate in Leisure Sports Based on Weight Change. Healthcare, 11."
},
{
"key": "ref_80",
"unstructured": "Korea Health Promotion Institute (2023, March 26). Changes in Life after COVID-19. Available online: https://www.khealth.or.kr/board/view?linkId=1001442&menuId=MENU00907."
},
{
"key": "ref_81",
"unstructured": "World Health Organization (2023, March 13). Considerations for Sports Federations/Sports Event Organizers When Planning Mass Gatherings in the Context of COVID-19: Interim Guidance. Available online: https://www.who.int/publications/i/item/considerations-for-sports-federations-sports-event-organizers-when-planning-mass-gatherings-in-the-context-of-covid-19-interim-guidance."
},
{
"DOI": "10.3390/nu12061657",
"doi-asserted-by": "crossref",
"key": "ref_82",
"unstructured": "Sidor, A., and Rzymski, P. (2020). Dietary choices and habits during COVID-19 lockdown: Experience from Poland. Nutrients, 12."
},
{
"DOI": "10.1038/s41598-023-41391-z",
"article-title": "Changes in health behaviours during the COVID-19 pandemic and effect on weight and obesity among older people in England",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "14661",
"journal-title": "Sci. Rep.",
"key": "ref_83",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1016/j.amepre.2022.01.012",
"article-title": "Obesity Prevalence among U.S. Adults During the COVID-19 Pandemic",
"author": "Restrepo",
"doi-asserted-by": "crossref",
"first-page": "102",
"journal-title": "Am. J. Prev. Med.",
"key": "ref_84",
"volume": "63",
"year": "2022"
},
{
"DOI": "10.1016/j.metabol.2022.155217",
"article-title": "A 2022 update on the epidemiology of obesity and a call to action: As its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on",
"author": "Boutari",
"doi-asserted-by": "crossref",
"first-page": "155217",
"journal-title": "Metabolism",
"key": "ref_85",
"volume": "133",
"year": "2022"
},
{
"DOI": "10.3389/fnut.2022.931313",
"article-title": "Obesity and Infection: What Have We Learned from the COVID-19 Pandemic",
"author": "Vassilopoulou",
"doi-asserted-by": "crossref",
"first-page": "931313",
"journal-title": "Front. Nutr.",
"key": "ref_86",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1016/j.metabol.2020.154378",
"article-title": "Obesity in patients with COVID-19: A systematic review and meta-analysis",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "154378",
"journal-title": "Metabolism",
"key": "ref_87",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.1097/MD.0000000000028499",
"article-title": "Obesity or increased body mass index and the risk of severe outcomes in patients with COVID-19: A protocol for systematic review and meta-analysis",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "e28499",
"journal-title": "Medicine",
"key": "ref_88",
"volume": "101",
"year": "2022"
},
{
"DOI": "10.3389/fimmu.2020.570122",
"article-title": "Immune-Boosting, Antioxidant and Anti-Inflammatory Food Supplements Targeting Pathogenesis of COVID-19",
"author": "Mrityunjaya",
"doi-asserted-by": "crossref",
"first-page": "570122",
"journal-title": "Front. Immunol.",
"key": "ref_89",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1128/mSystems.00122-21",
"article-title": "Dietary Supplements and Nutraceuticals under Investigation for COVID-19 Prevention and Treatment",
"author": "Lordan",
"doi-asserted-by": "crossref",
"first-page": "e00122-21",
"journal-title": "mSystems",
"key": "ref_90",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.3389/fphys.2018.01487",
"article-title": "Mitochondria, Oxidative Stress and Innate Immunity",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "1487",
"journal-title": "Front. Physiol.",
"key": "ref_91",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1126/sciadv.abb0806",
"article-title": "IL-10-producing Tfh cells accumulate with age and link inflammation with age-related immune suppression",
"author": "Almanan",
"doi-asserted-by": "crossref",
"first-page": "eabb0806",
"journal-title": "Sci. Adv.",
"key": "ref_92",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.3389/fnut.2021.698617",
"article-title": "Nutritional Impact and Its Potential Consequences on Covid-19 Severity",
"author": "Mortaz",
"doi-asserted-by": "crossref",
"first-page": "698617",
"journal-title": "Front. Nutr.",
"key": "ref_93",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.33549/physiolres.934492",
"article-title": "COVID-19 and the Immune System",
"author": "Paces",
"doi-asserted-by": "crossref",
"first-page": "379",
"journal-title": "Physiol. Res.",
"key": "ref_94",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.3390/nu11122862",
"doi-asserted-by": "crossref",
"key": "ref_95",
"unstructured": "Leeming, E.R., Johnson, A.J., Spector, T.D., and Le Roy, C.I. (2019). Effect of Diet on the Gut Microbiota: Rethinking Intervention Duration. Nutrients, 11."
},
{
"DOI": "10.1007/s12088-020-00908-0",
"article-title": "Diet, Gut Microbiota and COVID-19",
"author": "Rishi",
"doi-asserted-by": "crossref",
"first-page": "420",
"journal-title": "Indian J. Microbiol.",
"key": "ref_96",
"volume": "60",
"year": "2020"
},
{
"DOI": "10.1080/09637486.2023.2212879",
"article-title": "Habitual adherence to a traditional Mediterranean diet and risk of SARS-CoV-2 infection and Coronavirus disease 2019 (COVID-19): A longitudinal analysis",
"author": "Sharma",
"doi-asserted-by": "crossref",
"first-page": "382",
"journal-title": "Int. J. Food Sci. Nutr.",
"key": "ref_97",
"volume": "74",
"year": "2023"
},
{
"DOI": "10.3389/fnut.2021.707359",
"article-title": "Inverse Association Between the Mediterranean Diet and COVID-19 Risk in Lebanon: A Case-Control Study",
"author": "Julien",
"doi-asserted-by": "crossref",
"first-page": "707359",
"journal-title": "Front. Nutr.",
"key": "ref_98",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.3389/fnut.2021.805533",
"article-title": "Components of the Mediterranean Diet and Risk of COVID-19",
"author": "Gea",
"doi-asserted-by": "crossref",
"first-page": "805533",
"journal-title": "Front. Nutr.",
"key": "ref_99",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1016/j.clnu.2021.04.001",
"article-title": "Mediterranean diet and the risk of COVID-19 in the ‘Seguimiento Universidad de Navarra’ cohort",
"author": "Gea",
"doi-asserted-by": "crossref",
"first-page": "3061",
"journal-title": "Clin. Nutr.",
"key": "ref_100",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.3390/nu13051721",
"doi-asserted-by": "crossref",
"key": "ref_101",
"unstructured": "Ponzo, V., Pellegrini, M., D’Eusebio, C., Bioletto, F., Goitre, I., Buscemi, S., Frea, S., Ghigo, E., and Simona Bo, S. (2021). Mediterranean Diet and SARS-COV-2 Infection: Is There Any Association? A Proof-of-Concept Study. Nutrients, 13."
},
{
"DOI": "10.1016/j.metabol.2020.154407",
"article-title": "Mediterranean diet as a nutritional approach for COVID-19",
"author": "Angelidi",
"doi-asserted-by": "crossref",
"first-page": "154407",
"journal-title": "Metabolism",
"key": "ref_102",
"volume": "114",
"year": "2021"
},
{
"DOI": "10.3389/fendo.2020.574315",
"article-title": "Mediterranean Diet and COVID-19: Hypothesizing Potential Benefits in People with Diabetes",
"author": "Maiorino",
"doi-asserted-by": "crossref",
"first-page": "574315",
"journal-title": "Front. Endocrinol.",
"key": "ref_103",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1136/gutjnl-2021-325353",
"article-title": "Diet quality and risk and severity of COVID-19: A prospective cohort study",
"author": "Merino",
"doi-asserted-by": "crossref",
"first-page": "2096",
"journal-title": "Gut",
"key": "ref_104",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1136/bmjnph-2021-000272",
"article-title": "Plant-based diets, pescatarian diets and COVID-19 severity: A population-based case-control study in six countries",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "257",
"journal-title": "BMJ Nutr. Prev. Health",
"key": "ref_105",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.3390/ijms24054491",
"doi-asserted-by": "crossref",
"key": "ref_106",
"unstructured": "Andreo-López, M.C., Contreras-Bolívar, V., Muñoz-Torres, M., García-Fontana, B., and García-Fontana, C. (2023). Influence of the Mediterranean Diet on Healthy Aging. Int. J. Mol. Sci., 24."
},
{
"DOI": "10.3390/biomedicines8070201",
"doi-asserted-by": "crossref",
"key": "ref_107",
"unstructured": "Tsigalou, C., Konstantinidis, T., Paraschaki, A., Stavropoulou, E., Voidarou, C., and Bezirtzoglou, E. (2020). Mediterranean Diet as a Tool to Combat Inflammation and Chronic Diseases. An Overview. Biomedicine, 8."
},
{
"DOI": "10.3390/nu14142956",
"doi-asserted-by": "crossref",
"key": "ref_108",
"unstructured": "Finicelli, M., Di Salle, A., Galderisi, U., and Peluso, G. (2022). The Mediterranean Diet: An Update of the Clinical Trials. Nutrients, 14."
},
{
"DOI": "10.3390/nu13061951",
"doi-asserted-by": "crossref",
"key": "ref_109",
"unstructured": "Gantenbein, K.V., and Kanaka-Gantenbein, C. (2021). Mediterranean Diet as an Antioxidant: The Impact on Metabolic Health and Overall Wellbeing. Nutrients, 13."
},
{
"DOI": "10.3390/ijms241914876",
"doi-asserted-by": "crossref",
"key": "ref_110",
"unstructured": "Georgieva, E., Ananiev, J., Yovchev, Y., Arabadzhiev, G., Abrashev, H., Abrasheva, D., Atanasov, V., Kostandieva, R., Mitev, M., and Petkova-Parlapanska, K. (2023). COVID-19 Complications: Oxidative Stress, Inflammation, and Mitochondrial and Endothelial Dysfunction. Int. J. Mol. Sci., 24."
},
{
"DOI": "10.1007/s12035-023-03567-6",
"doi-asserted-by": "crossref",
"key": "ref_111",
"unstructured": "Rieder, A.S., and Wyse, A.T.S. (Mol. Neurobiol., 2023). Regulation of Inflammation by IRAK-M Pathway Can Be Associated with nAchRalpha7 Activation and COVID-19, Mol. Neurobiol., in press."
},
{
"DOI": "10.1080/14740338.2021.1970744",
"article-title": "The role of GLP-1 receptor agonists during COVID-19 pandemia: A hypothetical molecular mechanism",
"author": "Banerjee",
"doi-asserted-by": "crossref",
"first-page": "1309",
"journal-title": "Expert Opin. Drug Saf.",
"key": "ref_112",
"volume": "20",
"year": "2021"
}
],
"reference-count": 112,
"references-count": 112,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2079-9721/11/4/165"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Association of COVID-19 Infection with Sociodemographic, Anthropometric and Lifestyle Factors: A Cross-Sectional Study in an Older Adults’ Population Aged over 65 Years Old",
"type": "journal-article",
"volume": "11"
}
pavlidou