Association between ursodeoxycholic acid use and COVID-19 in individuals with chronic liver disease: a nationwide case-control study in South Korea
et al., Virology Journal, doi:10.1186/s12985-024-02464-1, Aug 2024
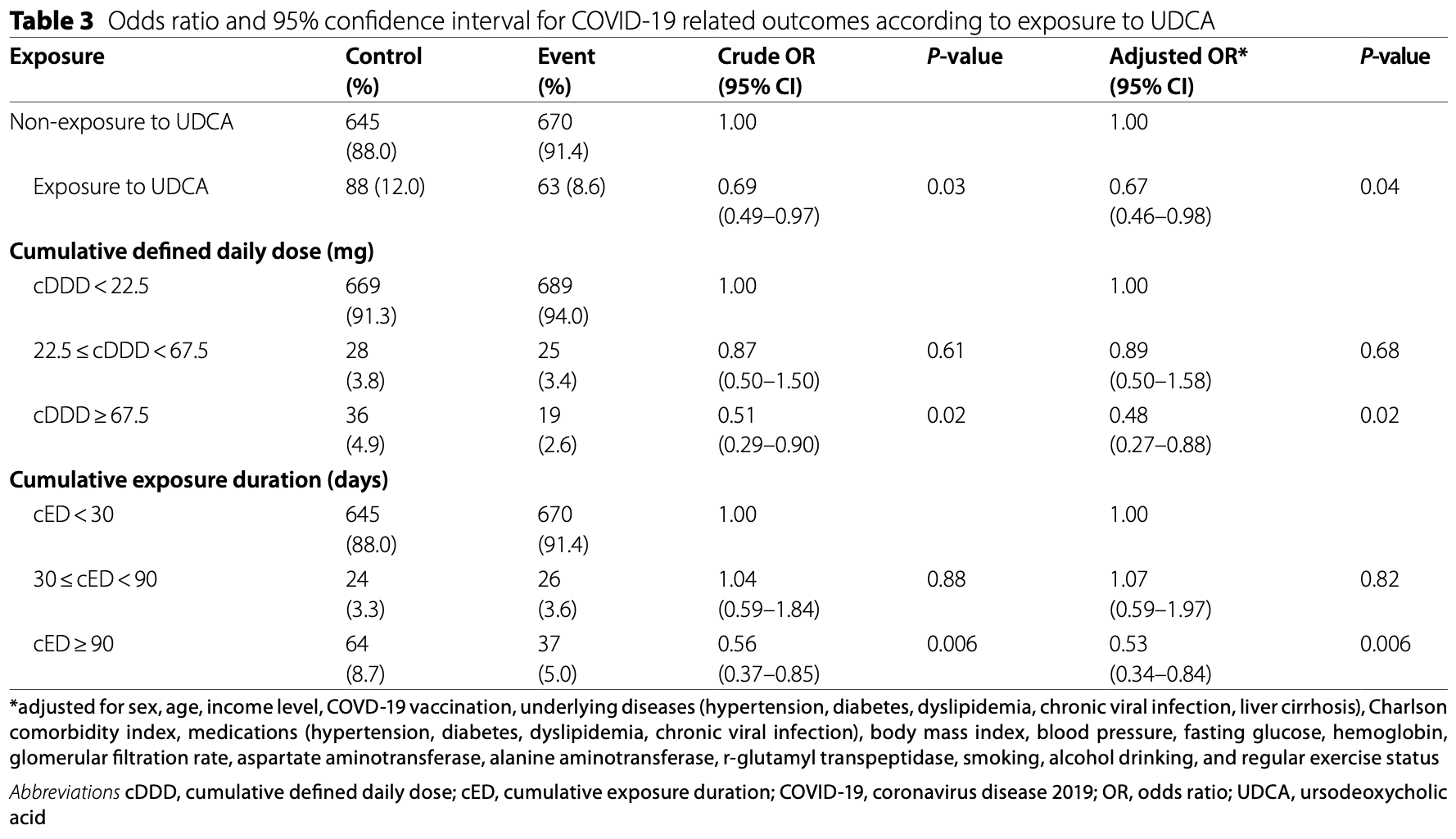
Retrospective 74,074 individuals with chronic liver disease in South Korea, showing lower risk of COVID-19 infection and related severe outcomes with ursodeoxycholic acid (UDCA) use. The risk reduction was dose-dependent, with greater benefits seen with higher UDCA exposure. Authors hypothesize that UDCA may reduce viral entry by downregulating the ACE2 receptor and modulate the cytokine storm implicated in severe COVID-19.
|
risk of severe case, 33.0% lower, OR 0.67, p = 0.04, treatment 63 of 733 (8.6%) cases,
88 of 733 (12.0%) controls, NNT 11, case control OR, propensity score matching.
|
|
risk of case, 20.0% lower, OR 0.80, p < 0.001, treatment 4,082 of 37,037 (11.0%) cases,
4,752 of 37,037 (12.8%) controls, NNT 23, case control OR, propensity score matching.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Moon et al., 27 Aug 2024, retrospective, South Korea, peer-reviewed, 6 authors, study period 1 January, 2021 - 31 December, 2021.
Contact: p100100@dau.ac.kr.
Association between ursodeoxycholic acid use and COVID-19 in individuals with chronic liver disease: a nationwide case-control study in South Korea
Virology Journal, doi:10.1186/s12985-024-02464-1
Background Conflicting evidence exists regarding the effects of ursodeoxycholic acid (UDCA) on coronavirus disease 2019 . This study investigates the association between UDCA administration and COVID-19 infection and its related outcomes in individuals with chronic liver disease (CLD). Methods A customized COVID-19 research database (n = 3,485,376) was created by integrating data from the National Health Insurance Service (NHIS) and the Korea Disease Control and Prevention Agency's COVID-19 databases. The study focused on patients diagnosed with COVID-19 in 2021, using the NHIS data from 365 days before diagnosis. To create comparable groups with and without UDCA administration before COVID-19, we used propensity score matching. The primary endpoint was the first confirmed positive result for severe acute respiratory syndrome coronavirus-2. In addition, we identified severe COVID-19-related outcomes. Subgroup analysis were conducted based on the dose of UDCA exposure.
Results Data from 74,074 individuals with CLD was analyzed. The participants' average age was 57.5 years, and 52.1% (19,277) of those in each group were male. Those with prior UDCA exposure had a significantly lower risk of COVID-19 infection (adjusted OR: 0.80, 95% CI [0.76-0.85]) compared to the non-UDCA group. Additionally, the UDCA group had a lower risk of severe ). Subgroup analyses indicated that there was a decrease in COVID-19 infection and its related outcomes with increasing UDCA exposure dose. Conclusions Our large observational study highlights the potential use of readily available UDCA as an adjunctive therapy for COVID-19 in individuals with CLD.
Supplementary Information The online version contains supplementary material available at https://doi. org/10.1186/s12985-024-02464-1.
Supplementary Material 1
Supplementary Material 2
Author contributions Sang Yi Moon and Minkook Son contributed equally to this work as first authors. Dr. S. Moon, M. Son, and Y. Baek had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: S. Moon, M. SonAcquisition, analysis, or interpretation of data: S. Moon, M. Son. Drafting of the manuscript: S. Moon, M. Son. Critical review of the manuscript for important intellectual content: Y, Kang, Y. Baek. Statistical analysis: M. Son. Administrative, technical, or material support: Y. Baek. Supervision: Y. Baek. All authors reviewed the manuscript.
Declarations Ethics approval and consent to participate The Dong-A University College of Medicine Institutional Review Board exempted this retrospective study from review due to its design (utilizing de-identified, publicly available clinical data for analysis) (DAUHIRB-EXP-23-026).
Consent for publication Not applicable.
Additional information This study used the database of the KDCA and the NHIS for policy and academic research. The research number of this study is KDCA-NHIS-2023-1-567. The KDCA is the Korea Disease Control and Prevention Agency, Republic of Korea. The NHIS is the National Health Insurance Service, Republic of Korea.
..
References
Abdulrab, Al-Maweri, Halboub, Ursodeoxycholic acid as a candidate therapeutic to alleviate and/or prevent COVID-19-associated cytokine storm, Med Hypotheses
Atc/Ddd, None
Baldelli, Marjot, Barnes, Barritt, Webb et al., SARS-CoV-2 infection and liver disease: a review of Pathogenesis and outcomes, Gut Liver
Barouch, Covid-19 vaccines -immunity, variants, boosters, N Engl J Med
Bedford, Enria, Giesecke, Heymann, Ihekweazu et al., COVID-19: towards controlling of a pandemic, Lancet
Beyerstedt, Casaro, Rangel, COVID-19: angiotensin-converting enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection, Eur J Clin Microbiol Infect Dis
Brevini, Maes, Webb, John, Fuchs et al., FXR inhibition may protect from SARS-CoV-2 infection by reducing ACE2, Nature
Burki, WHO ends the COVID-19 public health emergency, Lancet Respir Med
Carino, Moraca, Fiorillo, Marchianò, Sepe et al., Hijacking SARS-CoV-2/ACE2 receptor Interaction by Natural and semi-synthetic Steroidal agents acting on functional pockets on the receptor binding domain, Front Chem
Chang, Kim, Sinn, Cho, Kim et al., Clinical outcomes and validation of Ursodeoxycholic Acid Response scores in patients with Korean primary biliary cholangitis: a Multicenter Cohort Study, Gut Liver
Choi, Park, Lee, Suh, Song et al., Variable effects of underlying diseases on the prognosis of patients with COVID-19, PLoS ONE
Colapietro, Angelotti, Masetti, Shiffer, Pugliese et al., Ursodeoxycholic Acid Does Not Improve COVID-19 Outcome in Hospitalized Patients, Viruses
Contreras, Iftekhar, Priesemann, From emergency response to longterm management: the many faces of the endemic state of COVID-19, Lancet Reg Health Eur
Corpechot, Verdoux, Frank-Soltysiak, Vallée, Grimaldi, Exploring the impact of ursodeoxycholic acid therapy on COVID-19 in a realword setting, J Med Virol
Cromer, Steain, Reynaldi, Schlub, Khan et al., Predicting vaccine effectiveness against severe COVID-19 over time and against variants: a meta-analysis, Nat Commun
Dessie, Zewotir, Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients, BMC Infect Dis
El-Sherbiny, Taye, It, Role of ursodeoxycholic acid in prevention of hepatotoxicity caused by Amoxicillin-clavulanic acid in rats, Ann Hepatol
Fan, Dominitz, Eastment, Locke, Green et al., Risk factors for testing positive for severe Acute Respiratory Syndrome Coronavirus 2 in a National United States Healthcare System, Clin Infect Dis
Fiorillo, Marchianò, Moraca, Sepe, Carino et al., Discovery of bile acid derivatives as potent ACE2 activators by virtual screening and essential dynamics, J Chem Inf Model
Fiorucci, Urbani, Biagioli, Sepe, Distrutti et al., Bile acids and bile acid activated receptors in the treatment of Covid-19, Biochem Pharmacol
Gaziano, Giambartolomei, Pereira, Gaulton, Posner et al., Actionable druggable genome-wide mendelian randomization identifies repurposing opportunities for COVID-19, Nat Med
Ge, Pletcher, Lai, Outcomes of SARS-CoV-2 infection in patients with chronic liver disease and cirrhosis: a National COVID Cohort Collaborative Study, Gastroenterology
Hassine, Covid-19 vaccines and variants of concern: a review, Rev Med Virol
Hu, Zhang, Huang, Shen, Feng et al., transplantation: a multicenter retrospective cohort study
Ioannou, Liang, Locke, Green, Berry et al., Cirrhosis and severe Acute Respiratory Syndrome Coronavirus 2 infection in US veterans: risk of infection, hospitalization, Ventilation, and Mortality, Hepatology
John, Bastaich, Webb, Brevini, Moon et al., Ursodeoxycholic acid is associated with a reduction in SARS-CoV-2 infection and reduced severity of COVID-19 in patients with cirrhosis, J Intern Med
Ko, Lee, Kim, Jo, Kumar et al., Anti-inflammatory effects of ursodeoxycholic acid by lipopolysaccharide-stimulated inflammatory responses in RAW 264.7 macrophages, PLoS ONE
Lee, Lee, Choi, Han, Jung et al., Direct oral anticoagulants in patients with Atrial Fibrillation and Liver Disease, J Am Coll Cardiol
Lee, Sung, Yoon, Lee, Yoo et al., Therapeutic mechanisms and beneficial effects of non-antidiabetic drugs in chronic liver diseases, Clin Mol Hepatol
Li, Zhu, Cui, Lin, Li, Protective effect of ursodeoxycholic acid on COVID-19 in patients with chronic liver disease, Front Cell Infect Microbiol
Lindor, Bowlus, Boyer, Levy, Mayo, Primary biliary cholangitis: 2018 Practice Guidance from the American Association for the study of Liver diseases, Hepatology
Liu, Wang, Ursodeoxycholic acid administration did not reduce susceptibility to SARS-CoV-2 infection in children, Liver Int
Marjot, Webb, Ast, Moon, Stamataki et al., COVID-19 and liver disease: mechanistic and clinical perspectives, Nat Rev Gastroenterol Hepatol
Marrone, Covino, Merra, Piccioni, Amodeo et al., Ursodeoxycholic acid does not affect the clinical outcome of SARS-CoV-2 infection: a retrospective study of propensity score-matched cohorts, Liver Int
Moon, Webb, García-Juárez, Kulkarni, Adali et al., SARS-CoV-2 infections among patients with Liver Disease and Liver Transplantation who received COVID-19 vaccination, Hepatol Commun
Mueller, Castro, Thorell, Marschall, Auer et al., Ursodeoxycholic acid: effects on hepatic unfolded protein response, apoptosis and oxidative stress in morbidly obese patients, Liver Int
Naseer, Khalid, Parveen, Abbass, Song et al., COVID-19 outbreak: impact on global economy, Front Public Health
Oh, Bae, Lee, Shin, Oh et al., Ursodeoxycholic acid decreases age-related adiposity and inflammation in mice, BMB Rep
Okada, Shoda, Taguchi, Maher, Ishizaki et al., Ursodeoxycholic acid stimulates Nrf2-mediated hepatocellular transport, detoxification, and antioxidative stress systems in mice, Am J Physiol Gastrointest Liver Physiol
Omer, Salmon, Orenstein, Dehart, Halsey, Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases, N Engl J Med
Park, Byun, Kim, Ahn, Rhee et al., Regular follow-up visits reduce the risk for asthma exacerbation requiring admission in Korean adults with asthma, Allergy Asthma Clin Immunol
Park, Byun, Kim, Rhee, Kim et al., Frequent outpatient visits prevent exacerbation of Chronic Obstructive Pulmonary Disease, Sci Rep
Peeri, Shrestha, Rahman, Zaki, Tan et al., The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned?, Int J Epidemiol
Poupon, Ursodeoxycholic acid and bile-acid mimetics as therapeutic agents for cholestatic liver diseases: an overview of their mechanisms of action, Clin Res Hepatol Gastroenterol
Prayitno, Bhat, Repurposing UDCA, an FXR inhibitor, to prevent SARS-Cov-2 infection, Gastroenterology
Quan, Li, Couris, Fushimi, Graham et al., Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries, Am J Epidemiol
Roy, Biswas, Islam, Azam, Potential factors influencing COVID-19 vaccine acceptance and hesitancy: a systematic review, PLoS ONE
Sarker, Roknuzzaman, Hossain, Bhuiyan, Islam, The WHO declares COVID-19 is no longer a public health emergency of international concern: benefits, challenges, and necessary precautions to come back to normal life, Int J Surg
Sohan, Hossain, Islam, The SARS-CoV-2 Omicron (B.1.1.529) variant and effectiveness of existing vaccines: what we know so far, J Med Virol
Spearman, Aghemo, Valenti, Sonderup, COVID-19 and the liver: a 2021 update, Liver Int
Takigawa, Miyazaki, Kinoshita, Kawarabayashi, Nishiyama et al., Glucocorticoid receptor-dependent immunomodulatory effect of ursodeoxycholic acid on liver lymphocytes in mice, Am J Physiol Gastrointest Liver Physiol
Wong, Hui, Yip, Lui, Hui et al., Minimal risk of Drug-Induced Liver Injury with Molnupiravir and Ritonavir-Boosted Nirmatrelvir, Gastroenterology
Zampino, Mele, Florio, Bertolino, Andini et al., Liver injury in remdesivir-treated COVID-19 patients, Hepatol Int
DOI record:
{
"DOI": "10.1186/s12985-024-02464-1",
"ISSN": [
"1743-422X"
],
"URL": "http://dx.doi.org/10.1186/s12985-024-02464-1",
"alternative-id": [
"2464"
],
"article-number": "202",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "22 May 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "7 August 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "27 August 2024"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "The Dong-A University College of Medicine Institutional Review Board exempted this retrospective study from review due to its design (utilizing de-identified, publicly available clinical data for analysis) (DAUHIRB-EXP-23-026)."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "Not applicable."
},
{
"group": {
"label": "Additional information",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "This study used the database of the KDCA and the NHIS for policy and academic research. The research number of this study is KDCA-NHIS-2023-1-567. The KDCA is the Korea Disease Control and Prevention Agency, Republic of Korea. The NHIS is the National Health Insurance Service, Republic of Korea."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 5,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Moon",
"given": "Sang Yi",
"sequence": "first"
},
{
"affiliation": [],
"family": "Son",
"given": "Minkook",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kang",
"given": "Yeo Wool",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Koh",
"given": "Myeongseok",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lee",
"given": "Jong Yoon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Baek",
"given": "Yang Hyun",
"sequence": "additional"
}
],
"container-title": "Virology Journal",
"container-title-short": "Virol J",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2024,
8,
27
]
],
"date-time": "2024-08-27T18:03:13Z",
"timestamp": 1724781793000
},
"deposited": {
"date-parts": [
[
2024,
8,
27
]
],
"date-time": "2024-08-27T19:02:23Z",
"timestamp": 1724785343000
},
"funder": [
{
"name": "Dong-A University Research Fund"
}
],
"indexed": {
"date-parts": [
[
2024,
8,
28
]
],
"date-time": "2024-08-28T00:27:28Z",
"timestamp": 1724804848886
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
8,
27
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
8,
27
]
],
"date-time": "2024-08-27T00:00:00Z",
"timestamp": 1724716800000
}
},
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
8,
27
]
],
"date-time": "2024-08-27T00:00:00Z",
"timestamp": 1724716800000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12985-024-02464-1.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1186/s12985-024-02464-1/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12985-024-02464-1.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2024,
8,
27
]
]
},
"published-online": {
"date-parts": [
[
2024,
8,
27
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30673-5",
"author": "J Bedford",
"doi-asserted-by": "publisher",
"first-page": "1015",
"journal-title": "Lancet",
"key": "2464_CR1",
"unstructured": "Bedford J, Enria D, Giesecke J, Heymann DL, Ihekweazu C, Kobinger G, Lane HC, Memish Z, Oh MD, Sall AA, et al. COVID-19: towards controlling of a pandemic. Lancet. 2020;395:1015–8.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2022.1009393",
"author": "S Naseer",
"doi-asserted-by": "publisher",
"first-page": "1009393",
"journal-title": "Front Public Health",
"key": "2464_CR2",
"unstructured": "Naseer S, Khalid S, Parveen S, Abbass K, Song H, Achim MV. COVID-19 outbreak: impact on global economy. Front Public Health. 2022;10:1009393.",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1186/s12879-021-06536-3",
"author": "ZG Dessie",
"doi-asserted-by": "publisher",
"first-page": "855",
"journal-title": "BMC Infect Dis",
"key": "2464_CR3",
"unstructured": "Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021;21:855.",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0254258",
"author": "YJ Choi",
"doi-asserted-by": "publisher",
"first-page": "e0254258",
"journal-title": "PLoS ONE",
"key": "2464_CR4",
"unstructured": "Choi YJ, Park JY, Lee HS, Suh J, Song JY, Byun MK, Cho JH, Kim HJ, Park HJ. Variable effects of underlying diseases on the prognosis of patients with COVID-19. PLoS ONE. 2021;16:e0254258.",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.5009/gnl220327",
"author": "L Baldelli",
"doi-asserted-by": "publisher",
"first-page": "12",
"journal-title": "Gut Liver",
"key": "2464_CR5",
"unstructured": "Baldelli L, Marjot T, Barnes E, Barritt AS, Webb GJ, Moon AM. SARS-CoV-2 infection and liver disease: a review of Pathogenesis and outcomes. Gut Liver. 2023;17:12–23.",
"volume": "17",
"year": "2023"
},
{
"DOI": "10.1002/hep.31649",
"author": "GN Ioannou",
"doi-asserted-by": "publisher",
"first-page": "322",
"journal-title": "Hepatology",
"key": "2464_CR6",
"unstructured": "Ioannou GN, Liang PS, Locke E, Green P, Berry K, O’Hare AM, Shah JA, Crothers K, Eastment MC, Fan VS, Dominitz JA. Cirrhosis and severe Acute Respiratory Syndrome Coronavirus 2 infection in US veterans: risk of infection, hospitalization, Ventilation, and Mortality. Hepatology. 2021;74:322–35.",
"volume": "74",
"year": "2021"
},
{
"DOI": "10.1111/liv.14984",
"author": "CW Spearman",
"doi-asserted-by": "publisher",
"first-page": "1988",
"journal-title": "Liver Int",
"key": "2464_CR7",
"unstructured": "Spearman CW, Aghemo A, Valenti L, Sonderup MW. COVID-19 and the liver: a 2021 update. Liver Int. 2021;41:1988–98.",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1038/s41575-021-00426-4",
"author": "T Marjot",
"doi-asserted-by": "publisher",
"first-page": "348",
"journal-title": "Nat Rev Gastroenterol Hepatol",
"key": "2464_CR8",
"unstructured": "Marjot T, Webb GJ, Barritt ASt, Moon AM, Stamataki Z, Wong VW, Barnes E. COVID-19 and liver disease: mechanistic and clinical perspectives. Nat Rev Gastroenterol Hepatol. 2021;18:348–64.",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1053/j.gastro.2021.07.010",
"author": "J Ge",
"doi-asserted-by": "publisher",
"first-page": "1487",
"journal-title": "Gastroenterology",
"key": "2464_CR9",
"unstructured": "Ge J, Pletcher MJ, Lai JC. Outcomes of SARS-CoV-2 infection in patients with chronic liver disease and cirrhosis: a National COVID Cohort Collaborative Study. Gastroenterology. 2021;161:1487–e15011485.",
"volume": "161",
"year": "2021"
},
{
"DOI": "10.1002/hep4.1853",
"author": "AM Moon",
"doi-asserted-by": "publisher",
"first-page": "889",
"journal-title": "Hepatol Commun",
"key": "2464_CR10",
"unstructured": "Moon AM, Webb GJ, García-Juárez I, Kulkarni AV, Adali G, Wong DK, Lusina B, Dalekos GN, Masson S, Shore BM, et al. SARS-CoV-2 infections among patients with Liver Disease and Liver Transplantation who received COVID-19 vaccination. Hepatol Commun. 2022;6:889–97.",
"volume": "6",
"year": "2022"
},
{
"DOI": "10.1038/s41467-023-37176-7",
"author": "D Cromer",
"doi-asserted-by": "publisher",
"first-page": "1633",
"journal-title": "Nat Commun",
"key": "2464_CR11",
"unstructured": "Cromer D, Steain M, Reynaldi A, Schlub TE, Khan SR, Sasson SC, Kent SJ, Khoury DS, Davenport MP. Predicting vaccine effectiveness against severe COVID-19 over time and against variants: a meta-analysis. Nat Commun. 2023;14:1633.",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1007/s12072-020-10077-3",
"author": "R Zampino",
"doi-asserted-by": "publisher",
"first-page": "881",
"journal-title": "Hepatol Int",
"key": "2464_CR12",
"unstructured": "Zampino R, Mele F, Florio LL, Bertolino L, Andini R, Galdo M, De Rosa R, Corcione A, Durante-Mangoni E. Liver injury in remdesivir-treated COVID-19 patients. Hepatol Int. 2020;14:881–3.",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1053/j.gastro.2022.09.008",
"author": "GL Wong",
"doi-asserted-by": "publisher",
"first-page": "151",
"journal-title": "Gastroenterology",
"key": "2464_CR13",
"unstructured": "Wong GL, Hui VW, Yip TC, Lui GC, Hui DS, Wong VW. Minimal risk of Drug-Induced Liver Injury with Molnupiravir and Ritonavir-Boosted Nirmatrelvir. Gastroenterology. 2023;164:151–3.",
"volume": "164",
"year": "2023"
},
{
"DOI": "10.1038/s41591-021-01310-z",
"author": "L Gaziano",
"doi-asserted-by": "publisher",
"first-page": "668",
"journal-title": "Nat Med",
"key": "2464_CR14",
"unstructured": "Gaziano L, Giambartolomei C, Pereira AC, Gaulton A, Posner DC, Swanson SA, Ho Y-L, Iyengar SK, Kosik NM, Vujkovic M, et al. Actionable druggable genome-wide mendelian randomization identifies repurposing opportunities for COVID-19. Nat Med. 2021;27:668–76.",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1038/s41586-022-05594-0",
"author": "T Brevini",
"doi-asserted-by": "publisher",
"first-page": "134",
"journal-title": "Nature",
"key": "2464_CR15",
"unstructured": "Brevini T, Maes M, Webb GJ, John BV, Fuchs CD, Buescher G, Wang L, Griffiths C, Brown ML, Scott WE, et al. FXR inhibition may protect from SARS-CoV-2 infection by reducing ACE2. Nature. 2023;615:134–42.",
"volume": "615",
"year": "2023"
},
{
"DOI": "10.3389/fcimb.2023.1178590",
"author": "Y Li",
"doi-asserted-by": "publisher",
"first-page": "1178590",
"journal-title": "Front Cell Infect Microbiol",
"key": "2464_CR16",
"unstructured": "Li Y, Zhu N, Cui X, Lin Y, Li X. Protective effect of ursodeoxycholic acid on COVID-19 in patients with chronic liver disease. Front Cell Infect Microbiol. 2023;13:1178590.",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1111/joim.13630",
"author": "BV John",
"doi-asserted-by": "publisher",
"first-page": "636",
"journal-title": "J Intern Med",
"key": "2464_CR17",
"unstructured": "John BV, Bastaich D, Webb G, Brevini T, Moon A, Ferreira RD, Chin AM, Kaplan DE, Taddei TH, Serper M, et al. Ursodeoxycholic acid is associated with a reduction in SARS-CoV-2 infection and reduced severity of COVID-19 in patients with cirrhosis. J Intern Med. 2023;293:636–47.",
"volume": "293",
"year": "2023"
},
{
"DOI": "10.1093/qjmed/hcad254",
"doi-asserted-by": "crossref",
"key": "2464_CR18",
"unstructured": "Hu L, Zhang H, Huang C, Shen T, Feng Z, Mu F, Xu L, Lin Y, Yue C, Guo K, et al. Effect of Ursodeoxycholic Acid on preventing SARS-CoV-2 infection in patients with liver transplantation: a multicenter retrospective cohort study. Qjm; 2023."
},
{
"DOI": "10.3390/v15081738",
"doi-asserted-by": "crossref",
"key": "2464_CR19",
"unstructured": "Colapietro F, Angelotti G, Masetti C, Shiffer D, Pugliese N, De Nicola S, Carella F, Desai A, Ormas M, Calatroni M et al. Ursodeoxycholic Acid Does Not Improve COVID-19 Outcome in Hospitalized Patients. Viruses : 2023, 15."
},
{
"DOI": "10.1111/liv.15660",
"author": "T Liu",
"doi-asserted-by": "publisher",
"first-page": "1950",
"journal-title": "Liver Int",
"key": "2464_CR20",
"unstructured": "Liu T, Wang JS. Ursodeoxycholic acid administration did not reduce susceptibility to SARS-CoV-2 infection in children. Liver Int. 2023;43:1950–4.",
"volume": "43",
"year": "2023"
},
{
"DOI": "10.1111/liv.15736",
"author": "G Marrone",
"doi-asserted-by": "publisher",
"first-page": "83",
"journal-title": "Liver Int",
"key": "2464_CR21",
"unstructured": "Marrone G, Covino M, Merra G, Piccioni A, Amodeo A, Novelli A, Murri R, Pompili M, Gasbarrini A, Franceschi F. Ursodeoxycholic acid does not affect the clinical outcome of SARS-CoV-2 infection: a retrospective study of propensity score-matched cohorts. Liver Int. 2024;44:83–92.",
"volume": "44",
"year": "2024"
},
{
"DOI": "10.1002/jmv.29418",
"author": "C Corpechot",
"doi-asserted-by": "publisher",
"first-page": "e29418",
"journal-title": "J Med Virol",
"key": "2464_CR22",
"unstructured": "Corpechot C, Verdoux M, Frank-Soltysiak M, Duclos-Vallée JC, Grimaldi L. Exploring the impact of ursodeoxycholic acid therapy on COVID-19 in a real-word setting. J Med Virol. 2024;96:e29418.",
"volume": "96",
"year": "2024"
},
{
"key": "2464_CR23",
"unstructured": "Nation Health Insurance Data Sharing Service. 2024. [https://nhiss.nhis.or.kr/bd/ab/bdaba000eng.do]"
},
{
"key": "2464_CR24",
"unstructured": "ATC/DDD, Index. 2024. [https://atcddd.fhi.no/atc_ddd_index/code=A05AA02]"
},
{
"DOI": "10.1093/aje/kwq433",
"author": "H Quan",
"doi-asserted-by": "publisher",
"first-page": "676",
"journal-title": "Am J Epidemiol",
"key": "2464_CR25",
"unstructured": "Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, Januel JM, Sundararajan V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–82.",
"volume": "173",
"year": "2011"
},
{
"DOI": "10.1016/j.jacc.2019.04.052",
"author": "SR Lee",
"doi-asserted-by": "publisher",
"first-page": "3295",
"journal-title": "J Am Coll Cardiol",
"key": "2464_CR26",
"unstructured": "Lee SR, Lee HJ, Choi EK, Han KD, Jung JH, Cha MJ, Oh S, Lip GYH. Direct oral anticoagulants in patients with Atrial Fibrillation and Liver Disease. J Am Coll Cardiol. 2019;73:3295–308.",
"volume": "73",
"year": "2019"
},
{
"DOI": "10.1093/cid/ciaa1624",
"author": "VS Fan",
"doi-asserted-by": "publisher",
"first-page": "e3085",
"journal-title": "Clin Infect Dis",
"key": "2464_CR27",
"unstructured": "Fan VS, Dominitz JA, Eastment MC, Locke ER, Green P, Berry K, O’Hare AM, Shah JA, Crothers K, Ioannou GN. Risk factors for testing positive for severe Acute Respiratory Syndrome Coronavirus 2 in a National United States Healthcare System. Clin Infect Dis. 2021;73:e3085–94.",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.1002/hep.30145",
"author": "KD Lindor",
"doi-asserted-by": "publisher",
"first-page": "394",
"journal-title": "Hepatology",
"key": "2464_CR28",
"unstructured": "Lindor KD, Bowlus CL, Boyer J, Levy C, Mayo M. Primary biliary cholangitis: 2018 Practice Guidance from the American Association for the study of Liver diseases. Hepatology. 2019;69:394–419.",
"volume": "69",
"year": "2019"
},
{
"DOI": "10.3350/cmh.2022.0186",
"author": "HA Lee",
"doi-asserted-by": "publisher",
"first-page": "425",
"journal-title": "Clin Mol Hepatol",
"key": "2464_CR29",
"unstructured": "Lee HA, Chang Y, Sung PS, Yoon EL, Lee HW, Yoo J-J, Lee Y-S, An J, Song DS, Cho YY, et al. Therapeutic mechanisms and beneficial effects of non-antidiabetic drugs in chronic liver diseases. Clin Mol Hepatol. 2022;28:425–72.",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.5009/gnl220420",
"author": "J-I Chang",
"doi-asserted-by": "publisher",
"first-page": "620",
"journal-title": "Gut Liver",
"key": "2464_CR30",
"unstructured": "Chang J-I, Kim JH, Sinn DH, Cho J-Y, Kim KM, Oh JH, Park Y, Sohn W, Goh MJ, Kang W, et al. Clinical outcomes and validation of Ursodeoxycholic Acid Response scores in patients with Korean primary biliary cholangitis: a Multicenter Cohort Study. Gut Liver. 2023;17:620–8.",
"volume": "17",
"year": "2023"
},
{
"DOI": "10.1016/S2210-7401(12)70015-3",
"author": "R Poupon",
"doi-asserted-by": "publisher",
"first-page": "S3",
"issue": "Suppl 1",
"journal-title": "Clin Res Hepatol Gastroenterol",
"key": "2464_CR31",
"unstructured": "Poupon R. Ursodeoxycholic acid and bile-acid mimetics as therapeutic agents for cholestatic liver diseases: an overview of their mechanisms of action. Clin Res Hepatol Gastroenterol. 2012;36(Suppl 1):S3–12.",
"volume": "36",
"year": "2012"
},
{
"DOI": "10.5483/BMBRep.2016.49.2.173",
"author": "AR Oh",
"doi-asserted-by": "publisher",
"first-page": "105",
"journal-title": "BMB Rep",
"key": "2464_CR32",
"unstructured": "Oh AR, Bae JS, Lee J, Shin E, Oh BC, Park SC, Cha JY. Ursodeoxycholic acid decreases age-related adiposity and inflammation in mice. BMB Rep. 2016;49:105–10.",
"volume": "49",
"year": "2016"
},
{
"DOI": "10.1152/ajpgi.00205.2012",
"author": "T Takigawa",
"doi-asserted-by": "publisher",
"first-page": "G427",
"journal-title": "Am J Physiol Gastrointest Liver Physiol",
"key": "2464_CR33",
"unstructured": "Takigawa T, Miyazaki H, Kinoshita M, Kawarabayashi N, Nishiyama K, Hatsuse K, Ono S, Saitoh D, Seki S, Yamamoto J. Glucocorticoid receptor-dependent immunomodulatory effect of ursodeoxycholic acid on liver lymphocytes in mice. Am J Physiol Gastrointest Liver Physiol. 2013;305:G427–438.",
"volume": "305",
"year": "2013"
},
{
"DOI": "10.1152/ajpgi.90321.2008",
"author": "K Okada",
"doi-asserted-by": "publisher",
"first-page": "G735",
"journal-title": "Am J Physiol Gastrointest Liver Physiol",
"key": "2464_CR34",
"unstructured": "Okada K, Shoda J, Taguchi K, Maher JM, Ishizaki K, Inoue Y, Ohtsuki M, Goto N, Takeda K, Utsunomiya H, et al. Ursodeoxycholic acid stimulates Nrf2-mediated hepatocellular transport, detoxification, and antioxidative stress systems in mice. Am J Physiol Gastrointest Liver Physiol. 2008;295:G735–747.",
"volume": "295",
"year": "2008"
},
{
"DOI": "10.1016/S1665-2681(19)31792-2",
"author": "GA El-Sherbiny",
"doi-asserted-by": "publisher",
"first-page": "134",
"journal-title": "Ann Hepatol",
"key": "2464_CR35",
"unstructured": "El-Sherbiny GA, Taye A, Abdel-Raheem IT. Role of ursodeoxycholic acid in prevention of hepatotoxicity caused by Amoxicillin-clavulanic acid in rats. Ann Hepatol. 2009;8:134–40.",
"volume": "8",
"year": "2009"
},
{
"DOI": "10.1111/liv.13562",
"author": "M Mueller",
"doi-asserted-by": "publisher",
"first-page": "523",
"journal-title": "Liver Int",
"key": "2464_CR36",
"unstructured": "Mueller M, Castro RE, Thorell A, Marschall HU, Auer N, Herac M, Rodrigues CMP, Trauner M. Ursodeoxycholic acid: effects on hepatic unfolded protein response, apoptosis and oxidative stress in morbidly obese patients. Liver Int. 2018;38:523–31.",
"volume": "38",
"year": "2018"
},
{
"DOI": "10.1007/s10096-020-04138-6",
"author": "S Beyerstedt",
"doi-asserted-by": "publisher",
"first-page": "905",
"journal-title": "Eur J Clin Microbiol Infect Dis",
"key": "2464_CR37",
"unstructured": "Beyerstedt S, Casaro EB, Rangel ÉB. COVID-19: angiotensin-converting enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection. Eur J Clin Microbiol Infect Dis. 2021;40:905–19.",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.1016/j.bcp.2023.115983",
"doi-asserted-by": "crossref",
"key": "2464_CR38",
"unstructured": "Fiorucci S, Urbani G, Biagioli M, Sepe V, Distrutti E, Zampella A. Bile acids and bile acid activated receptors in the treatment of Covid-19. Biochem Pharmacol 2023:115983."
},
{
"DOI": "10.3389/fchem.2020.572885",
"author": "A Carino",
"doi-asserted-by": "publisher",
"first-page": "572885",
"journal-title": "Front Chem",
"key": "2464_CR39",
"unstructured": "Carino A, Moraca F, Fiorillo B, Marchianò S, Sepe V, Biagioli M, Finamore C, Bozza S, Francisci D, Distrutti E, et al. Hijacking SARS-CoV-2/ACE2 receptor Interaction by Natural and semi-synthetic Steroidal agents acting on functional pockets on the receptor binding domain. Front Chem. 2020;8:572885.",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1021/acs.jcim.1c01126",
"author": "B Fiorillo",
"doi-asserted-by": "publisher",
"first-page": "196",
"journal-title": "J Chem Inf Model",
"key": "2464_CR40",
"unstructured": "Fiorillo B, Marchianò S, Moraca F, Sepe V, Carino A, Rapacciuolo P, Biagioli M, Limongelli V, Zampella A, Catalanotti B, Fiorucci S. Discovery of bile acid derivatives as potent ACE2 activators by virtual screening and essential dynamics. J Chem Inf Model. 2022;62:196–209.",
"volume": "62",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0180673",
"author": "WK Ko",
"doi-asserted-by": "publisher",
"first-page": "e0180673",
"journal-title": "PLoS ONE",
"key": "2464_CR41",
"unstructured": "Ko WK, Lee SH, Kim SJ, Jo MJ, Kumar H, Han IB, Sohn S. Anti-inflammatory effects of ursodeoxycholic acid by lipopolysaccharide-stimulated inflammatory responses in RAW 264.7 macrophages. PLoS ONE. 2017;12:e0180673.",
"volume": "12",
"year": "2017"
},
{
"DOI": "10.1016/j.mehy.2020.109897",
"author": "S Abdulrab",
"doi-asserted-by": "publisher",
"first-page": "109897",
"journal-title": "Med Hypotheses",
"key": "2464_CR42",
"unstructured": "Abdulrab S, Al-Maweri S, Halboub E. Ursodeoxycholic acid as a candidate therapeutic to alleviate and/or prevent COVID-19-associated cytokine storm. Med Hypotheses. 2020;143:109897.",
"volume": "143",
"year": "2020"
},
{
"DOI": "10.1053/j.gastro.2023.01.014",
"author": "K Prayitno",
"doi-asserted-by": "publisher",
"first-page": "1019",
"journal-title": "Gastroenterology",
"key": "2464_CR43",
"unstructured": "Prayitno K, Bhat M. Repurposing UDCA, an FXR inhibitor, to prevent SARS-Cov-2 infection. Gastroenterology. 2023;164:1019–20.",
"volume": "164",
"year": "2023"
},
{
"DOI": "10.1016/j.lanepe.2023.100664",
"author": "S Contreras",
"doi-asserted-by": "publisher",
"first-page": "100664",
"journal-title": "Lancet Reg Health Eur",
"key": "2464_CR44",
"unstructured": "Contreras S, Iftekhar EN, Priesemann V. From emergency response to long-term management: the many faces of the endemic state of COVID-19. Lancet Reg Health Eur. 2023;30:100664.",
"volume": "30",
"year": "2023"
},
{
"DOI": "10.1016/S2213-2600(23)00217-5",
"author": "T Burki",
"doi-asserted-by": "publisher",
"first-page": "588",
"journal-title": "Lancet Respir Med",
"key": "2464_CR45",
"unstructured": "Burki T. WHO ends the COVID-19 public health emergency. Lancet Respir Med. 2023;11:588.",
"volume": "11",
"year": "2023"
},
{
"DOI": "10.1097/JS9.0000000000000513",
"author": "R Sarker",
"doi-asserted-by": "publisher",
"first-page": "2851",
"journal-title": "Int J Surg",
"key": "2464_CR46",
"unstructured": "Sarker R, Roknuzzaman ASM, Hossain MJ, Bhuiyan MA, Islam MR. The WHO declares COVID-19 is no longer a public health emergency of international concern: benefits, challenges, and necessary precautions to come back to normal life. Int J Surg. 2023;109:2851–2.",
"volume": "109",
"year": "2023"
},
{
"DOI": "10.1002/rmv.2313",
"author": "I Hadj Hassine",
"doi-asserted-by": "publisher",
"first-page": "e2313",
"journal-title": "Rev Med Virol",
"key": "2464_CR47",
"unstructured": "Hadj Hassine I. Covid-19 vaccines and variants of concern: a review. Rev Med Virol. 2022;32:e2313.",
"volume": "32",
"year": "2022"
},
{
"DOI": "10.1002/jmv.27574",
"author": "M Sohan",
"doi-asserted-by": "publisher",
"first-page": "1796",
"journal-title": "J Med Virol",
"key": "2464_CR48",
"unstructured": "Sohan M, Hossain MJ, Islam MR. The SARS-CoV-2 Omicron (B.1.1.529) variant and effectiveness of existing vaccines: what we know so far. J Med Virol. 2022;94:1796–8.",
"volume": "94",
"year": "2022"
},
{
"DOI": "10.1056/NEJMra2206573",
"author": "DH Barouch",
"doi-asserted-by": "publisher",
"first-page": "1011",
"journal-title": "N Engl J Med",
"key": "2464_CR49",
"unstructured": "Barouch DH. Covid-19 vaccines - immunity, variants, boosters. N Engl J Med. 2022;387:1011–20.",
"volume": "387",
"year": "2022"
},
{
"DOI": "10.1056/NEJMsa0806477",
"author": "SB Omer",
"doi-asserted-by": "publisher",
"first-page": "1981",
"journal-title": "N Engl J Med",
"key": "2464_CR50",
"unstructured": "Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. 2009;360:1981–8.",
"volume": "360",
"year": "2009"
},
{
"DOI": "10.1371/journal.pone.0265496",
"author": "DN Roy",
"doi-asserted-by": "publisher",
"first-page": "e0265496",
"journal-title": "PLoS ONE",
"key": "2464_CR51",
"unstructured": "Roy DN, Biswas M, Islam E, Azam MS. Potential factors influencing COVID-19 vaccine acceptance and hesitancy: a systematic review. PLoS ONE. 2022;17:e0265496.",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1186/s13223-018-0250-0",
"author": "HJ Park",
"doi-asserted-by": "publisher",
"first-page": "29",
"journal-title": "Allergy Asthma Clin Immunol",
"key": "2464_CR52",
"unstructured": "Park HJ, Byun MK, Kim HJ, Ahn CM, Rhee CK, Kim K, Kim BY, Bae HW, Yoo KH. Regular follow-up visits reduce the risk for asthma exacerbation requiring admission in Korean adults with asthma. Allergy Asthma Clin Immunol. 2018;14:29.",
"volume": "14",
"year": "2018"
},
{
"DOI": "10.1038/s41598-020-63064-x",
"author": "HJ Park",
"doi-asserted-by": "publisher",
"first-page": "6049",
"journal-title": "Sci Rep",
"key": "2464_CR53",
"unstructured": "Park HJ, Byun MK, Kim T, Rhee CK, Kim K, Kim BY, Ahn SI, Jo YU, Yoo KH. Frequent outpatient visits prevent exacerbation of Chronic Obstructive Pulmonary Disease. Sci Rep. 2020;10:6049.",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1093/ije/dyaa033",
"author": "NC Peeri",
"doi-asserted-by": "publisher",
"first-page": "717",
"journal-title": "Int J Epidemiol",
"key": "2464_CR54",
"unstructured": "Peeri NC, Shrestha N, Rahman MS, Zaki R, Tan Z, Bibi S, Baghbanzadeh M, Aghamohammadi N, Zhang W, Haque U. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol. 2020;49:717–26.",
"volume": "49",
"year": "2020"
}
],
"reference-count": 54,
"references-count": 54,
"relation": {},
"resource": {
"primary": {
"URL": "https://virologyj.biomedcentral.com/articles/10.1186/s12985-024-02464-1"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Association between ursodeoxycholic acid use and COVID-19 in individuals with chronic liver disease: a nationwide case-control study in South Korea",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "21"
}