Apalutamide Prevents SARS-CoV-2 Infection in Lung Epithelial Cells and in Human Nasal Epithelial Cells
et al., International Journal of Molecular Sciences, doi:10.3390/ijms24043288, Feb 2023
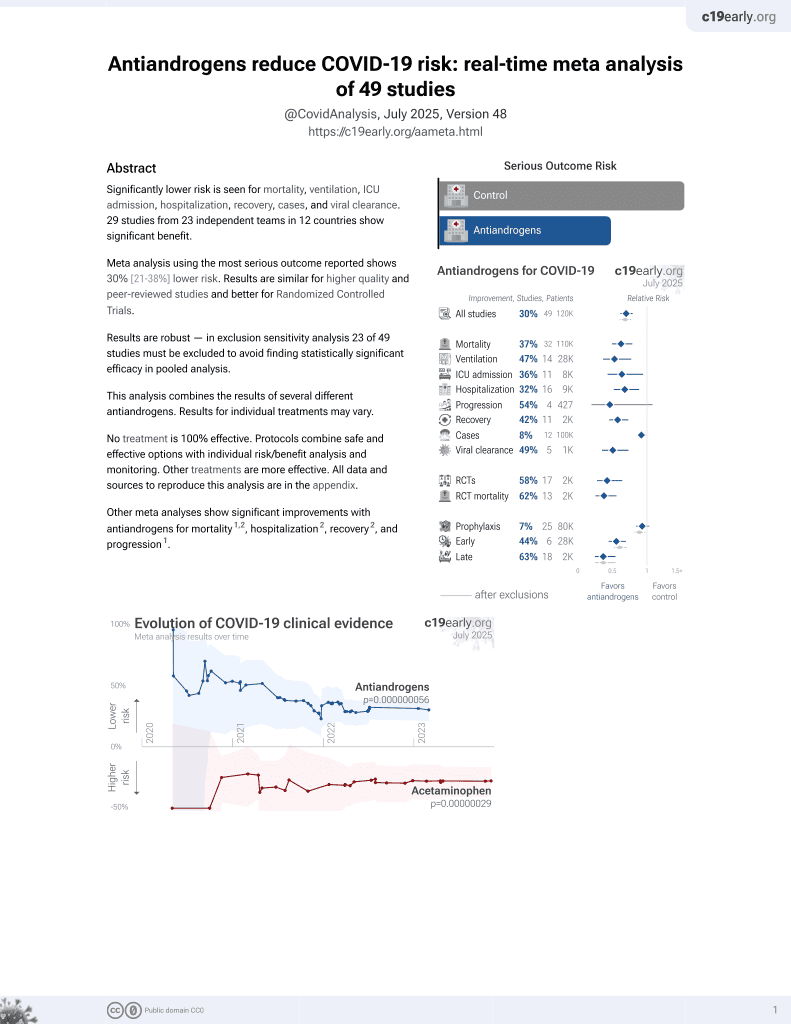
7th treatment shown to reduce risk in
September 2020, now with p = 0.000000056 from 49 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
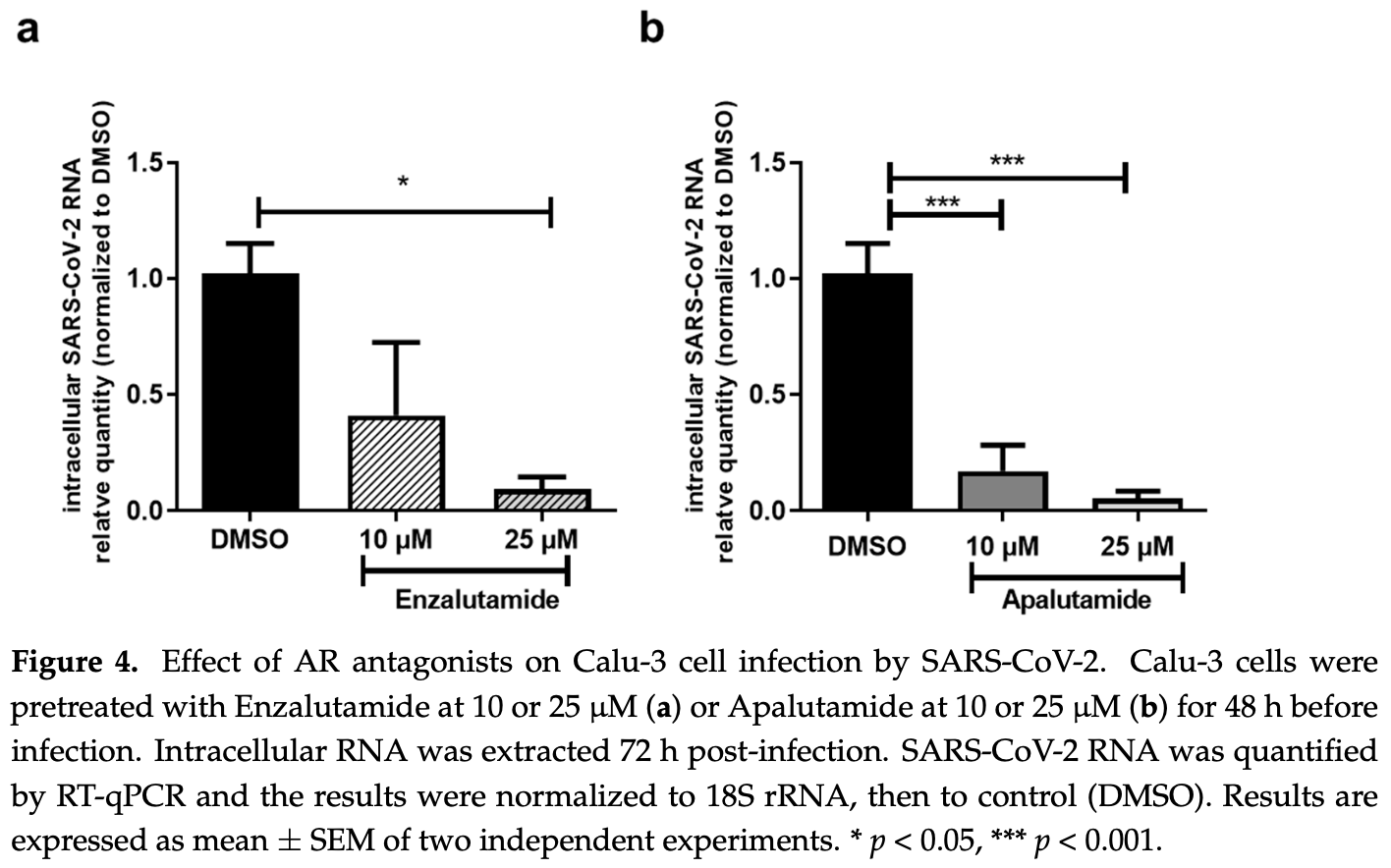
In vitro study showing that TMPRSS2 expression is regulated by androgens in Calu-3 cells, and treatment with anti-androgen drugs such as apalutamide significantly reduced SARS-CoV-2 entry and infection in both Calu-3 lung cells and primary human nasal epithelial cells.
Majidipur et al., 7 Feb 2023, France, peer-reviewed, 20 authors.
Contact: virginie.firlej@u-pec.fr (corresponding author).
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Apalutamide Prevents SARS-CoV-2 Infection in Lung Epithelial Cells and in Human Nasal Epithelial Cells
International Journal of Molecular Sciences, doi:10.3390/ijms24043288
In early 2020, the novel pathogenic severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in Wuhan, China, and rapidly propagated worldwide causing a global health emergency. SARS-CoV-2 binds to the angiotensin-converting enzyme 2 (ACE2) protein for cell entry, followed by proteolytic cleavage of the Spike (S) protein by the transmembrane serine protease 2 (TMPRSS2), allowing fusion of the viral and cellular membranes. Interestingly, TMPRSS2 is a key regulator in prostate cancer (PCa) progression which is regulated by androgen receptor (AR) signaling. Our hypothesis is that the AR signaling may regulate the expression of TMPRSS2 in human respiratory cells and thus influence the membrane fusion entry pathway of SARS-CoV-2. We show here that TMPRSS2 and AR are expressed in Calu-3 lung cells. In this cell line, TMPRSS2 expression is regulated by androgens. Finally, pre-treatment with anti-androgen drugs such as apalutamide significantly reduced SARS-CoV-2 entry and infection in Calu-3 lung cells but also in primary human nasal epithelial cells. Altogether, these data provide strong evidence to support the use of apalutamide as a treatment option for the PCa population vulnerable to severe COVID-19.
Supplementary Materials: The following supporting information can be downloaded at https:// www.mdpi.com/article/10.3390/ijms24043288/s1, Figure S1 : Effect of AR antagonists on TMPRSS2 expression in lung and prostate cells,
Conflicts of Interest: The sponsors had no role in the design, execution, interpretation, or writing of the study.
References
Afar, Vivanco, Hubert, Kuo, Chen et al., Catalytic Cleavage of the Androgen-Regulated TMPRSS2 Protease Results in Its Secretion by Prostate and Prostate Cancer Epithelia, Cancer Res
Al-Jarallah, Rajan, Dashti, Al Saber, Brady et al., In-Hospital Mortality in SARS-CoV-2 Stratified by Sex Diffrences: A Retrospective Cross-Sectional Cohort Study, Ann. Med. Surg, doi:10.1016/j.amsu.2022.104026
Baczenas, Andersen, Rashid, Yarmosh, Puthuveetil et al., Propagation of SARS-CoV-2 in Calu-3 Cells to Eliminate Mutations in the Furin Cleavage Site of Spike, Viruses, doi:10.3390/v13122434
Baratchian, Mcmanus, Berk, Nakamura, Mukhopadhyay et al., Androgen Regulation of Pulmonary AR, TMPRSS2 and ACE2 with Implications for Sex-Discordant COVID-19 Outcomes, Sci. Rep, doi:10.1038/s41598-021-90491-1
Bequignon, Dhommée, Angely, Thomas, Bottier et al., FcRn-Dependent Transcytosis of Monoclonal Antibody in Human Nasal Epithelial Cells In Vitro: A Prerequisite for a New Delivery Route for Therapy?, Int. J. Mol. Sci, doi:10.3390/ijms20061379
Bestle, Heindl, Limburg, Van Lam, Pilgram et al., TMPRSS2 and Furin Are Both Essential for Proteolytic Activation of SARS-CoV-2 in Human Airway Cells, Life Sci. Alliance, doi:10.26508/lsa.202000786
Chakravarty, Nair, Hammouda, Ratnani, Gharib et al., Sex Differences in SARS-CoV-2 Infection Rates and the Potential Link to Prostate Cancer, Commun. Biol
Chen, Chughtai, Dyda, Macintyre, Comparative Epidemiology of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) in Saudi Arabia and South Korea, Emerg. Microbes Infect, doi:10.1038/emi.2017.40
Coste, Brugel, Maître, Boussat, Papon et al., Inflammatory Cells as Well as Epithelial Cells in Nasal Polyps Express Vascular Endothelial Growth Factor, Eur. Respir. J, doi:10.1034/j.1399-3003.2000.15b24.x
Deng, Rasool, Russell, Natesan, Asangani, Targeting Androgen Regulation of TMPRSS2 and ACE2 as a Therapeutic Strategy to Combat COVID-19, iScience, doi:10.1016/j.isci.2021.102254
Gedeborg, Loeb, Styrke, Kiiski-Berggren, Garmo et al., Susceptibility to SARS-Cov-2 Infection and Risk for Severe COVID-19 in Patients with Prostate Cancer on Androgen Deprivation Therapy, Int. J. Cancer
Guo, Porter, Crozier, Coates, Jha et al., Topical TMPRSS2 Inhibition Prevents SARS-CoV-2 Infection in Differentiated Human Airway Cultures, Life Sci. Alliance, doi:10.26508/lsa.202101116
Haitao, Vermunt, Abeykoon, Ghamrawi, Gunaratne et al., COVID-19 and Sex Differences, Mayo. Clin. Proc, doi:10.1016/j.mayocp.2020.07.024
Hoffmann, Kleine-Weber, Schroeder, Krüger, Herrler et al., SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Huang, Wang, Li, Ren, Zhao et al., Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Karimi, Nowroozi, Alilou, Amini, Effects of Androgen Deprivation Therapy on COVID-19 in Patients with Prostate Cancer: A Systematic Review and Meta-Analysis, Urol. J, doi:10.22037/uj.v18i.6691
Karlberg, Chong, Lai, Do Men Have a Higher Case Fatality Rate of Severe Acute Respiratory Syndrome than Women Do?, Am. J. Epidemiol, doi:10.1093/aje/kwh056
Klein, Li, Milinovich, Schold, Sharifi et al., Androgen Deprivation Therapy in Men with Prostate Cancer Does Not Affect Risk of Infection with SARS-CoV-2, J. Urol, doi:10.1097/JU.0000000000001338
Koch, Uckeley, Doldan, Stanifer, Boulant et al., TMPRSS2 Expression Dictates the Entry Route Used by SARS-CoV-2 to Infect Host Cells, EMBO J, doi:10.15252/embj.2021107821
Koskinen, Carpen, Honkanen, Seppänen, Miettinen et al., Androgen Deprivation and SARS-CoV-2 in Men with Prostate Cancer, Ann. Oncol, doi:10.1016/j.annonc.2020.06.015
Leach, Mohr, Giotis, Cil, Isac et al., The Antiandrogen Enzalutamide Downregulates TMPRSS2 and Reduces Cellular Entry of SARS-CoV-2 in Human Lung Cells, Nat. Commun, doi:10.1038/s41467-021-24342-y
Li, Han, Dai, Xu, He et al., Distinct Mechanisms for TMPRSS2 Expression Explain Organ-Specific Inhibition of SARS-CoV-2 Infection by Enzalutamide, Nat. Commun, doi:10.1038/s41467-021-21171-x
Lin, Ferguson, White, Wang, Vessella et al., Prostate-Localized and Androgen-Regulated Expression of the Membrane-Bound Serine Protease TMPRSS2, Cancer Res
Lucas, Heinlein, Kim, Hernandez, Malik et al., The Androgen-Regulated Protease TMPRSS2 Activates a Proteolytic Cascade Involving Components of the Tumor Microenvironment and Promotes Prostate Cancer Metastasis, Cancer Discov, doi:10.1158/2159-8290.CD-13-1010
Lucas, True, Hawley, Matsumura, Morrissey et al., The Androgen-Regulated Type II Serine Protease TMPRSS2 Is Differentially Expressed and Mislocalized in Prostate Adenocarcinoma, J. Pathol
Matsuyama, Nagata, Shirato, Kawase, Takeda et al., Efficient Activation of the Severe Acute Respiratory Syndrome Coronavirus Spike Protein by the Transmembrane Protease TMPRSS2, J. Virol, doi:10.1128/JVI.01542-10
Matsuyama, Ujike, Morikawa, Tashiro, Taguchi, Protease-Mediated Enhancement of Severe Acute Respiratory Syndrome Coronavirus Infection, doi:10.1073/pnas.0503203102
Mikkonen, Pihlajamaa, Sahu, Zhang, Jänne, Androgen Receptor and Androgen-Dependent Gene Expression in Lung, Mol. Cell. Endocrinol, doi:10.1016/j.mce.2009.12.022
Montopoli, Zumerle, Vettor, Rugge, Zorzi et al., Androgen-Deprivation Therapies for Prostate Cancer and Risk of Infection by SARS-CoV-2: A Population-Based Study (N=4532), Ann. Oncol, doi:10.1016/j.annonc.2020.04.479
Mori, Mostafaei, Pradere, Motlagh, Quhal et al., Enzalutamide, and Darolutamide for Non-Metastatic Castration-Resistant Prostate Cancer: A Systematic Review and Network Meta-Analysis, Int. J. Clin. Oncol, doi:10.1007/s10147-020-01777-9
Mousavizadeh, Ghasemi, Genotype and Phenotype of COVID-19: Their Roles in Pathogenesis, J. Microbiol. Immunol. Infect, doi:10.1016/j.jmii.2020.03.022
Müller, Brighton, Carson, Fischer, Jaspers, Culturing of Human Nasal Epithelial Cells at the Air Liquid Interface, J. Vis. Exp, doi:10.3791/50646
Papon, Coste, Gendron, Cordonnier, Wingerstmann et al., HLA-DR and ICAM-1 Expression and Modulation in Epithelial Cells from Nasal Polyps, Laryngoscope, doi:10.1097/00005537-200211000-00030
Patel, Zhong, Liaw, Tremblay, Tsao et al., Does Androgen Deprivation Therapy Protect against Severe Complications from COVID-19?, Ann. Oncol, doi:10.1016/j.annonc.2020.06.023
Peckham, De Gruijter, Raine, Radziszewska, Ciurtin et al., Male Sex Identified by Global COVID-19 Meta-Analysis as a Risk Factor for Death and ITU Admission, Nat. Commun, doi:10.1038/s41467-020-19741-6
Qiao, Wang, Mannan, Pitchiaya, Zhang et al., Targeting Transcriptional Regulation of SARS-CoV-2 Entry Factors ACE2 and TMPRSS2, doi:10.1073/pnas.2021450118
Recchia, Musti, Lanzino, Panno, Turano et al., A Cross-Talk between the Androgen Receptor and the Epidermal Growth Factor Receptor Leads to P38MAPK-Dependent Activation of MTOR and CyclinD1 Expression in Prostate and Lung Cancer Cells, Int. J. Biochem. Cell Biol, doi:10.1016/j.biocel.2008.07.004
Samuel, Majd, Richter, Ghazizadeh, Zekavat et al., Androgen Signaling Regulates SARS-CoV-2 Receptor Levels and Is Associated with Severe COVID-19 Symptoms in Men, Cell Stem Cell, doi:10.1016/j.stem.2020.11.009
Schmidt, Tucker, Bakouny, Labaki, Hsu et al., Association Between Androgen Deprivation Therapy and Mortality Among Patients With Prostate Cancer and COVID-19, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2021.34330
Scully, Haverfield, Ursin, Tannenbaum, Klein, Considering How Biological Sex Impacts Immune Responses and COVID-19 Outcomes, Nat. Rev. Immunol, doi:10.1038/s41577-020-0348-8
Shah, Patel, Zhong, Pina, Hawley et al., The Impact of Androgen Deprivation Therapy on COVID-19 Illness in Men With Prostate Cancer, JNCI Cancer Spectr
Shang, Wan, Luo, Ye, Geng et al., Cell Entry Mechanisms of SARS-CoV-2, doi:10.1073/pnas.2003138117
Treppiedi, Marra, Di Muro, Catalano, Mangili et al., TMPRSS2 Expression and Activity Modulation by Sex-Related Hormones in Lung Calu-3 Cells: Impact on Gender-Specific SARS-CoV-2 Infection, Front. Endocrinol, doi:10.3389/fendo.2022.862789
Vahidy, Pan, Ahnstedt, Munshi, Choi et al., Sex Differences in Susceptibility, Severity, and Outcomes of Coronavirus Disease 2019: Cross-Sectional Analysis from a Diverse US Metropolitan Area, PLoS ONE, doi:10.1371/journal.pone.0245556
Welén, Rosendal, Gisslén, Lenman, Freyhult et al., A Phase 2 Trial of the Effect of Antiandrogen Therapy on COVID-19 Outcome: No Evidence of Benefit, Supported by Epidemiology and In Vitro Data, Eur. Urol, doi:10.1016/j.eururo.2021.12.013
Wu, Mcgoogan, Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention, JAMA, doi:10.1001/jama.2020.2648
Zhu, Feng, Hu, Wang, Yu et al., A Genome-Wide CRISPR Screen Identifies Host Factors That Regulate SARS-CoV-2 Entry, Nat. Commun, doi:10.1038/s41467-021-21213-4
Zhu, Zhang, Wang, Li, Yang et al., A Novel Coronavirus from Patients with Pneumonia in China, N. Engl. J. Med, doi:10.1056/NEJMoa2001017
DOI record:
{
"DOI": "10.3390/ijms24043288",
"ISSN": [
"1422-0067"
],
"URL": "http://dx.doi.org/10.3390/ijms24043288",
"abstract": "<jats:p>In early 2020, the novel pathogenic severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in Wuhan, China, and rapidly propagated worldwide causing a global health emergency. SARS-CoV-2 binds to the angiotensin-converting enzyme 2 (ACE2) protein for cell entry, followed by proteolytic cleavage of the Spike (S) protein by the transmembrane serine protease 2 (TMPRSS2), allowing fusion of the viral and cellular membranes. Interestingly, TMPRSS2 is a key regulator in prostate cancer (PCa) progression which is regulated by androgen receptor (AR) signaling. Our hypothesis is that the AR signaling may regulate the expression of TMPRSS2 in human respiratory cells and thus influence the membrane fusion entry pathway of SARS-CoV-2. We show here that TMPRSS2 and AR are expressed in Calu-3 lung cells. In this cell line, TMPRSS2 expression is regulated by androgens. Finally, pre-treatment with anti-androgen drugs such as apalutamide significantly reduced SARS-CoV-2 entry and infection in Calu-3 lung cells but also in primary human nasal epithelial cells. Altogether, these data provide strong evidence to support the use of apalutamide as a treatment option for the PCa population vulnerable to severe COVID-19.</jats:p>",
"alternative-id": [
"ijms24043288"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-0925-5563",
"affiliation": [
{
"name": "TRePCa, Université Paris Est Créteil, F-94010 Créteil, France"
}
],
"authenticated-orcid": false,
"family": "Majidipur",
"given": "Amene",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Team “Viruses, Hepatology, Cancer“, Institut Mondor de Recherche Biomédicale, Université Paris Est Créteil, INSERM U955, F-94010 Créteil, France"
}
],
"family": "Morin-Dewaele",
"given": "Margot",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "TRePCa, Université Paris Est Créteil, F-94010 Créteil, France"
}
],
"family": "Gaspar Lopes",
"given": "Jeanne",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Team “Viruses, Hepatology, Cancer“, Institut Mondor de Recherche Biomédicale, Université Paris Est Créteil, INSERM U955, F-94010 Créteil, France"
}
],
"family": "Berry",
"given": "Francois",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "TRePCa, Université Paris Est Créteil, F-94010 Créteil, France"
}
],
"family": "Fouchet",
"given": "Julien",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of ENT and Head and Neck Surgery, Centre Hospitalier Intercommunal de Créteil, F-94010 Créteil, France"
},
{
"name": "AP-HP, Department of ENT and Head and Neck Surgery, Centre Hospitalier Universitaire Henri Mondor, F-94010 Créteil, France"
},
{
"name": "Team “Biomechanics and Respiratory System”, Institut Mondor de Recherche Biomédicale, Université Paris Est Créteil, INSERM U955, CNRS EMR 7000, F-94010 Créteil, France"
}
],
"family": "Bartier",
"given": "Sophie",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "TRePCa, Université Paris Est Créteil, F-94010 Créteil, France"
}
],
"family": "Dufros Duval",
"given": "Anais",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "TRePCa, Université Paris Est Créteil, F-94010 Créteil, France"
}
],
"family": "Soyeux",
"given": "Pascale",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5541-5954",
"affiliation": [
{
"name": "TRePCa, Université Paris Est Créteil, F-94010 Créteil, France"
}
],
"authenticated-orcid": false,
"family": "Huet",
"given": "Eric",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Team “Biomechanics and Respiratory System”, Institut Mondor de Recherche Biomédicale, Université Paris Est Créteil, INSERM U955, CNRS EMR 7000, F-94010 Créteil, France"
}
],
"family": "Louis",
"given": "Bruno",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of ENT and Head and Neck Surgery, Centre Hospitalier Intercommunal de Créteil, F-94010 Créteil, France"
},
{
"name": "AP-HP, Department of ENT and Head and Neck Surgery, Centre Hospitalier Universitaire Henri Mondor, F-94010 Créteil, France"
},
{
"name": "Team “Biomechanics and Respiratory System”, Institut Mondor de Recherche Biomédicale, Université Paris Est Créteil, INSERM U955, CNRS EMR 7000, F-94010 Créteil, France"
}
],
"family": "Coste",
"given": "André",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5193-5776",
"affiliation": [
{
"name": "Department of ENT and Head and Neck Surgery, Centre Hospitalier Intercommunal de Créteil, F-94010 Créteil, France"
},
{
"name": "AP-HP, Department of ENT and Head and Neck Surgery, Centre Hospitalier Universitaire Henri Mondor, F-94010 Créteil, France"
},
{
"name": "Team “Biomechanics and Respiratory System”, Institut Mondor de Recherche Biomédicale, Université Paris Est Créteil, INSERM U955, CNRS EMR 7000, F-94010 Créteil, France"
}
],
"authenticated-orcid": false,
"family": "Béquignon",
"given": "Émilie",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "TRePCa, Université Paris Est Créteil, F-94010 Créteil, France"
},
{
"name": "AP-HP, Department of Oncology, Centre Hospitalier Universitaire Henri Mondor, F-94010 Créteil, France"
}
],
"family": "Saldana",
"given": "Carolina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "INSERM, AP-HP, Clinical Investigation Center 1430, Henri Mondor University Hospital, F-94000 Créteil, France"
}
],
"family": "Le Corvoisier",
"given": "Philippe",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4959-2580",
"affiliation": [
{
"name": "TRePCa, Université Paris Est Créteil, F-94010 Créteil, France"
}
],
"authenticated-orcid": false,
"family": "Destouches",
"given": "Damien",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Team “Viruses, Hepatology, Cancer“, Institut Mondor de Recherche Biomédicale, Université Paris Est Créteil, INSERM U955, F-94010 Créteil, France"
},
{
"name": "AP-HP, Department of Virology, Centre Hospitalier Universitaire Henri Mondor, F-94010 Créteil, France"
}
],
"family": "Pawlotsky",
"given": "Jean-Michel",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "TRePCa, Université Paris Est Créteil, F-94010 Créteil, France"
},
{
"name": "AP-HP, Department of Oncology, Centre Hospitalier Universitaire Henri Mondor, F-94010 Créteil, France"
},
{
"name": "AP-HP, Department of Urology, Centre Hospitalier Universitaire Henri Mondor, F-94010 Créteil, France"
}
],
"family": "de la Taille",
"given": "Alexandre",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "TRePCa, Université Paris Est Créteil, F-94010 Créteil, France"
}
],
"family": "Vacherot",
"given": "Francis",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0719-0826",
"affiliation": [
{
"name": "Team “Viruses, Hepatology, Cancer“, Institut Mondor de Recherche Biomédicale, Université Paris Est Créteil, INSERM U955, F-94010 Créteil, France"
}
],
"authenticated-orcid": false,
"family": "Bruscella",
"given": "Patrice",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4132-0695",
"affiliation": [
{
"name": "TRePCa, Université Paris Est Créteil, F-94010 Créteil, France"
}
],
"authenticated-orcid": false,
"family": "Firlej",
"given": "Virginie",
"sequence": "additional"
}
],
"container-title": "International Journal of Molecular Sciences",
"container-title-short": "IJMS",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
2,
8
]
],
"date-time": "2023-02-08T08:01:45Z",
"timestamp": 1675843305000
},
"deposited": {
"date-parts": [
[
2023,
2,
8
]
],
"date-time": "2023-02-08T08:49:10Z",
"timestamp": 1675846150000
},
"funder": [
{
"name": "UFR Santé-UPEC"
},
{
"name": "Ligue contre le Cancer 94/Val-de-Marne"
},
{
"name": "Astellas Pharma"
},
{
"name": "Janssen-Cilag"
}
],
"indexed": {
"date-parts": [
[
2023,
2,
9
]
],
"date-time": "2023-02-09T05:33:04Z",
"timestamp": 1675920784400
},
"is-referenced-by-count": 0,
"issue": "4",
"issued": {
"date-parts": [
[
2023,
2,
7
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2023,
2
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
2,
7
]
],
"date-time": "2023-02-07T00:00:00Z",
"timestamp": 1675728000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1422-0067/24/4/3288/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "3288",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
2,
7
]
]
},
"published-online": {
"date-parts": [
[
2023,
2,
7
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "ref_1",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2001017",
"article-title": "A Novel Coronavirus from Patients with Pneumonia in China, 2019",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "727",
"journal-title": "N. Engl. J. Med.",
"key": "ref_2",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.2648",
"article-title": "Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "1239",
"journal-title": "JAMA",
"key": "ref_3",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/j.amsu.2022.104026",
"article-title": "In-Hospital Mortality in SARS-CoV-2 Stratified by Sex Diffrences: A Retrospective Cross-Sectional Cohort Study",
"author": "Rajan",
"doi-asserted-by": "crossref",
"first-page": "104026",
"journal-title": "Ann. Med. Surg.",
"key": "ref_4",
"volume": "79",
"year": "2022"
},
{
"DOI": "10.1016/j.mayocp.2020.07.024",
"article-title": "COVID-19 and Sex Differences",
"author": "Haitao",
"doi-asserted-by": "crossref",
"first-page": "2189",
"journal-title": "Mayo. Clin. Proc.",
"key": "ref_5",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.1038/s41577-020-0348-8",
"article-title": "Considering How Biological Sex Impacts Immune Responses and COVID-19 Outcomes",
"author": "Scully",
"doi-asserted-by": "crossref",
"first-page": "442",
"journal-title": "Nat. Rev. Immunol.",
"key": "ref_6",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0245556",
"doi-asserted-by": "crossref",
"key": "ref_7",
"unstructured": "Vahidy, F.S., Pan, A.P., Ahnstedt, H., Munshi, Y., Choi, H.A., Tiruneh, Y., Nasir, K., Kash, B.A., Andrieni, J.D., and McCullough, L.D. (2021). Sex Differences in Susceptibility, Severity, and Outcomes of Coronavirus Disease 2019: Cross-Sectional Analysis from a Diverse US Metropolitan Area. PLoS ONE, 16."
},
{
"DOI": "10.1093/aje/kwh056",
"article-title": "Do Men Have a Higher Case Fatality Rate of Severe Acute Respiratory Syndrome than Women Do?",
"author": "Karlberg",
"doi-asserted-by": "crossref",
"first-page": "229",
"journal-title": "Am. J. Epidemiol.",
"key": "ref_8",
"volume": "159",
"year": "2004"
},
{
"DOI": "10.1038/emi.2017.40",
"article-title": "Comparative Epidemiology of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) in Saudi Arabia and South Korea",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "e51",
"journal-title": "Emerg. Microbes Infect.",
"key": "ref_9",
"volume": "6",
"year": "2017"
},
{
"DOI": "10.1016/j.jmii.2020.03.022",
"article-title": "Genotype and Phenotype of COVID-19: Their Roles in Pathogenesis",
"author": "Mousavizadeh",
"doi-asserted-by": "crossref",
"first-page": "159",
"journal-title": "J. Microbiol. Immunol. Infect.",
"key": "ref_10",
"volume": "54",
"year": "2020"
},
{
"DOI": "10.1073/pnas.2003138117",
"article-title": "Cell Entry Mechanisms of SARS-CoV-2",
"author": "Shang",
"doi-asserted-by": "crossref",
"first-page": "11727",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_11",
"volume": "117",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor",
"author": "Hoffmann",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Cell",
"key": "ref_12",
"volume": "181",
"year": "2020"
},
{
"article-title": "Prostate-Localized and Androgen-Regulated Expression of the Membrane-Bound Serine Protease TMPRSS2",
"author": "Lin",
"first-page": "4180",
"journal-title": "Cancer Res.",
"key": "ref_13",
"volume": "59",
"year": "1999"
},
{
"article-title": "Catalytic Cleavage of the Androgen-Regulated TMPRSS2 Protease Results in Its Secretion by Prostate and Prostate Cancer Epithelia",
"author": "Afar",
"first-page": "1686",
"journal-title": "Cancer Res.",
"key": "ref_14",
"volume": "61",
"year": "2001"
},
{
"DOI": "10.1002/path.2330",
"article-title": "The Androgen-Regulated Type II Serine Protease TMPRSS2 Is Differentially Expressed and Mislocalized in Prostate Adenocarcinoma",
"author": "Lucas",
"doi-asserted-by": "crossref",
"first-page": "118",
"journal-title": "J. Pathol.",
"key": "ref_15",
"volume": "215",
"year": "2008"
},
{
"DOI": "10.1158/2159-8290.CD-13-1010",
"article-title": "The Androgen-Regulated Protease TMPRSS2 Activates a Proteolytic Cascade Involving Components of the Tumor Microenvironment and Promotes Prostate Cancer Metastasis",
"author": "Lucas",
"doi-asserted-by": "crossref",
"first-page": "1310",
"journal-title": "Cancer Discov.",
"key": "ref_16",
"volume": "4",
"year": "2014"
},
{
"DOI": "10.1016/j.isci.2021.102254",
"article-title": "Targeting Androgen Regulation of TMPRSS2 and ACE2 as a Therapeutic Strategy to Combat COVID-19",
"author": "Deng",
"doi-asserted-by": "crossref",
"first-page": "102254",
"journal-title": "iScience",
"key": "ref_17",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1073/pnas.2021450118",
"article-title": "Targeting Transcriptional Regulation of SARS-CoV-2 Entry Factors ACE2 and TMPRSS2",
"author": "Qiao",
"doi-asserted-by": "crossref",
"first-page": "e2021450118",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_18",
"volume": "118",
"year": "2021"
},
{
"DOI": "10.1038/s41467-021-24342-y",
"article-title": "The Antiandrogen Enzalutamide Downregulates TMPRSS2 and Reduces Cellular Entry of SARS-CoV-2 in Human Lung Cells",
"author": "Leach",
"doi-asserted-by": "crossref",
"first-page": "4068",
"journal-title": "Nat. Commun.",
"key": "ref_19",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.26508/lsa.202101116",
"article-title": "Topical TMPRSS2 Inhibition Prevents SARS-CoV-2 Infection in Differentiated Human Airway Cultures",
"author": "Guo",
"doi-asserted-by": "crossref",
"first-page": "e202101116",
"journal-title": "Life Sci. Alliance",
"key": "ref_20",
"volume": "5",
"year": "2022"
},
{
"DOI": "10.1038/s41598-021-90491-1",
"article-title": "Androgen Regulation of Pulmonary AR, TMPRSS2 and ACE2 with Implications for Sex-Discordant COVID-19 Outcomes",
"author": "Baratchian",
"doi-asserted-by": "crossref",
"first-page": "11130",
"journal-title": "Sci. Rep.",
"key": "ref_21",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1038/s41467-021-21171-x",
"article-title": "Distinct Mechanisms for TMPRSS2 Expression Explain Organ-Specific Inhibition of SARS-CoV-2 Infection by Enzalutamide",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "866",
"journal-title": "Nat. Commun.",
"key": "ref_22",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/s41467-021-21213-4",
"article-title": "A Genome-Wide CRISPR Screen Identifies Host Factors That Regulate SARS-CoV-2 Entry",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "961",
"journal-title": "Nat. Commun.",
"key": "ref_23",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.15252/embj.2021107821",
"article-title": "TMPRSS2 Expression Dictates the Entry Route Used by SARS-CoV-2 to Infect Host Cells",
"author": "Koch",
"doi-asserted-by": "crossref",
"first-page": "e107821",
"journal-title": "EMBO J.",
"key": "ref_24",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.1007/s10147-020-01777-9",
"article-title": "Apalutamide, Enzalutamide, and Darolutamide for Non-Metastatic Castration-Resistant Prostate Cancer: A Systematic Review and Network Meta-Analysis",
"author": "Mori",
"doi-asserted-by": "crossref",
"first-page": "1892",
"journal-title": "Int. J. Clin. Oncol.",
"key": "ref_25",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1034/j.1399-3003.2000.15b24.x",
"article-title": "Inflammatory Cells as Well as Epithelial Cells in Nasal Polyps Express Vascular Endothelial Growth Factor",
"author": "Coste",
"doi-asserted-by": "crossref",
"first-page": "367",
"journal-title": "Eur. Respir. J.",
"key": "ref_26",
"volume": "15",
"year": "2000"
},
{
"DOI": "10.1097/00005537-200211000-00030",
"article-title": "HLA-DR and ICAM-1 Expression and Modulation in Epithelial Cells from Nasal Polyps",
"author": "Papon",
"doi-asserted-by": "crossref",
"first-page": "2067",
"journal-title": "Laryngoscope",
"key": "ref_27",
"volume": "112",
"year": "2002"
},
{
"DOI": "10.3390/ijms20061379",
"doi-asserted-by": "crossref",
"key": "ref_28",
"unstructured": "Bequignon, E., Dhommée, C., Angely, C., Thomas, L., Bottier, M., Escudier, E., Isabey, D., Coste, A., Louis, B., and Papon, J.-F. (2019). FcRn-Dependent Transcytosis of Monoclonal Antibody in Human Nasal Epithelial Cells In Vitro: A Prerequisite for a New Delivery Route for Therapy?. Int. J. Mol. Sci., 20."
},
{
"article-title": "Culturing of Human Nasal Epithelial Cells at the Air Liquid Interface",
"author": "Brighton",
"first-page": "e50646",
"journal-title": "J. Vis. Exp.",
"key": "ref_29",
"volume": "80",
"year": "2013"
},
{
"DOI": "10.3389/fendo.2022.862789",
"article-title": "TMPRSS2 Expression and Activity Modulation by Sex-Related Hormones in Lung Calu-3 Cells: Impact on Gender-Specific SARS-CoV-2 Infection",
"author": "Treppiedi",
"doi-asserted-by": "crossref",
"first-page": "862789",
"journal-title": "Front. Endocrinol.",
"key": "ref_30",
"volume": "13",
"year": "2022"
},
{
"key": "ref_31",
"unstructured": "(2022, November 08). Global Health 50/50. The COVID-19 Sex-Disaggregated Data Tracker. Available online: https://globalhealth5050.org/the-sex-gender-and-covid-19-project/the-data-tracker/."
},
{
"DOI": "10.1038/s41467-020-19741-6",
"article-title": "Male Sex Identified by Global COVID-19 Meta-Analysis as a Risk Factor for Death and ITU Admission",
"author": "Peckham",
"doi-asserted-by": "crossref",
"first-page": "6317",
"journal-title": "Nat. Commun.",
"key": "ref_32",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.mce.2009.12.022",
"article-title": "Androgen Receptor and Androgen-Dependent Gene Expression in Lung",
"author": "Mikkonen",
"doi-asserted-by": "crossref",
"first-page": "14",
"journal-title": "Mol. Cell. Endocrinol.",
"key": "ref_33",
"volume": "317",
"year": "2010"
},
{
"DOI": "10.3390/v13122434",
"doi-asserted-by": "crossref",
"key": "ref_34",
"unstructured": "Baczenas, J.J., Andersen, H., Rashid, S., Yarmosh, D., Puthuveetil, N., Parker, M., Bradford, R., Florence, C., Stemple, K.J., and Lewis, M.G. (2021). Propagation of SARS-CoV-2 in Calu-3 Cells to Eliminate Mutations in the Furin Cleavage Site of Spike. Viruses, 13."
},
{
"DOI": "10.1016/j.biocel.2008.07.004",
"article-title": "A Cross-Talk between the Androgen Receptor and the Epidermal Growth Factor Receptor Leads to P38MAPK-Dependent Activation of MTOR and CyclinD1 Expression in Prostate and Lung Cancer Cells",
"author": "Recchia",
"doi-asserted-by": "crossref",
"first-page": "603",
"journal-title": "Int. J. Biochem. Cell Biol.",
"key": "ref_35",
"volume": "41",
"year": "2009"
},
{
"DOI": "10.1073/pnas.0503203102",
"article-title": "Protease-Mediated Enhancement of Severe Acute Respiratory Syndrome Coronavirus Infection",
"author": "Matsuyama",
"doi-asserted-by": "crossref",
"first-page": "12543",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_36",
"volume": "102",
"year": "2005"
},
{
"DOI": "10.1128/JVI.01542-10",
"article-title": "Efficient Activation of the Severe Acute Respiratory Syndrome Coronavirus Spike Protein by the Transmembrane Protease TMPRSS2",
"author": "Matsuyama",
"doi-asserted-by": "crossref",
"first-page": "12658",
"journal-title": "J. Virol.",
"key": "ref_37",
"volume": "84",
"year": "2010"
},
{
"DOI": "10.26508/lsa.202000786",
"article-title": "TMPRSS2 and Furin Are Both Essential for Proteolytic Activation of SARS-CoV-2 in Human Airway Cells",
"author": "Bestle",
"doi-asserted-by": "crossref",
"first-page": "e202000786",
"journal-title": "Life Sci. Alliance",
"key": "ref_38",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1016/j.annonc.2020.04.479",
"article-title": "Androgen-Deprivation Therapies for Prostate Cancer and Risk of Infection by SARS-CoV-2: A Population-Based Study (N=4532)",
"author": "Montopoli",
"doi-asserted-by": "crossref",
"first-page": "1040",
"journal-title": "Ann. Oncol.",
"key": "ref_39",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1016/j.annonc.2020.06.023",
"article-title": "Does Androgen Deprivation Therapy Protect against Severe Complications from COVID-19?",
"author": "Patel",
"doi-asserted-by": "crossref",
"first-page": "1419",
"journal-title": "Ann. Oncol.",
"key": "ref_40",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1038/s42003-020-1088-9",
"article-title": "Sex Differences in SARS-CoV-2 Infection Rates and the Potential Link to Prostate Cancer",
"author": "Chakravarty",
"doi-asserted-by": "crossref",
"first-page": "374",
"journal-title": "Commun. Biol.",
"key": "ref_41",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1016/j.annonc.2020.06.015",
"article-title": "Androgen Deprivation and SARS-CoV-2 in Men with Prostate Cancer",
"author": "Koskinen",
"doi-asserted-by": "crossref",
"first-page": "1417",
"journal-title": "Ann. Oncol.",
"key": "ref_42",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2021.34330",
"article-title": "Association Between Androgen Deprivation Therapy and Mortality Among Patients With Prostate Cancer and COVID-19",
"author": "Schmidt",
"doi-asserted-by": "crossref",
"first-page": "e2134330",
"journal-title": "JAMA Netw. Open",
"key": "ref_43",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1002/ijc.34204",
"article-title": "Susceptibility to SARS-Cov-2 Infection and Risk for Severe COVID-19 in Patients with Prostate Cancer on Androgen Deprivation Therapy",
"author": "Gedeborg",
"doi-asserted-by": "crossref",
"first-page": "1925",
"journal-title": "Int. J. Cancer",
"key": "ref_44",
"volume": "151",
"year": "2022"
},
{
"DOI": "10.1097/JU.0000000000001338",
"article-title": "Androgen Deprivation Therapy in Men with Prostate Cancer Does Not Affect Risk of Infection with SARS-CoV-2",
"author": "Klein",
"doi-asserted-by": "crossref",
"first-page": "441",
"journal-title": "J. Urol.",
"key": "ref_45",
"volume": "205",
"year": "2021"
},
{
"article-title": "Effects of Androgen Deprivation Therapy on COVID-19 in Patients with Prostate Cancer: A Systematic Review and Meta-Analysis",
"author": "Karimi",
"first-page": "577",
"journal-title": "Urol. J.",
"key": "ref_46",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1093/jncics/pkac035",
"article-title": "The Impact of Androgen Deprivation Therapy on COVID-19 Illness in Men With Prostate Cancer",
"author": "Shah",
"doi-asserted-by": "crossref",
"first-page": "pkac035",
"journal-title": "JNCI Cancer Spectr.",
"key": "ref_47",
"volume": "6",
"year": "2022"
},
{
"DOI": "10.1016/j.stem.2020.11.009",
"article-title": "Androgen Signaling Regulates SARS-CoV-2 Receptor Levels and Is Associated with Severe COVID-19 Symptoms in Men",
"author": "Samuel",
"doi-asserted-by": "crossref",
"first-page": "876",
"journal-title": "Cell Stem Cell",
"key": "ref_48",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1016/j.eururo.2021.12.013",
"article-title": "A Phase 2 Trial of the Effect of Antiandrogen Therapy on COVID-19 Outcome: No Evidence of Benefit, Supported by Epidemiology and In Vitro Data",
"author": "Rosendal",
"doi-asserted-by": "crossref",
"first-page": "285",
"journal-title": "Eur. Urol.",
"key": "ref_49",
"volume": "81",
"year": "2022"
}
],
"reference-count": 49,
"references-count": 49,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1422-0067/24/4/3288"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Inorganic Chemistry",
"Organic Chemistry",
"Physical and Theoretical Chemistry",
"Computer Science Applications",
"Spectroscopy",
"Molecular Biology",
"General Medicine",
"Catalysis"
],
"subtitle": [],
"title": "Apalutamide Prevents SARS-CoV-2 Infection in Lung Epithelial Cells and in Human Nasal Epithelial Cells",
"type": "journal-article",
"volume": "24"
}