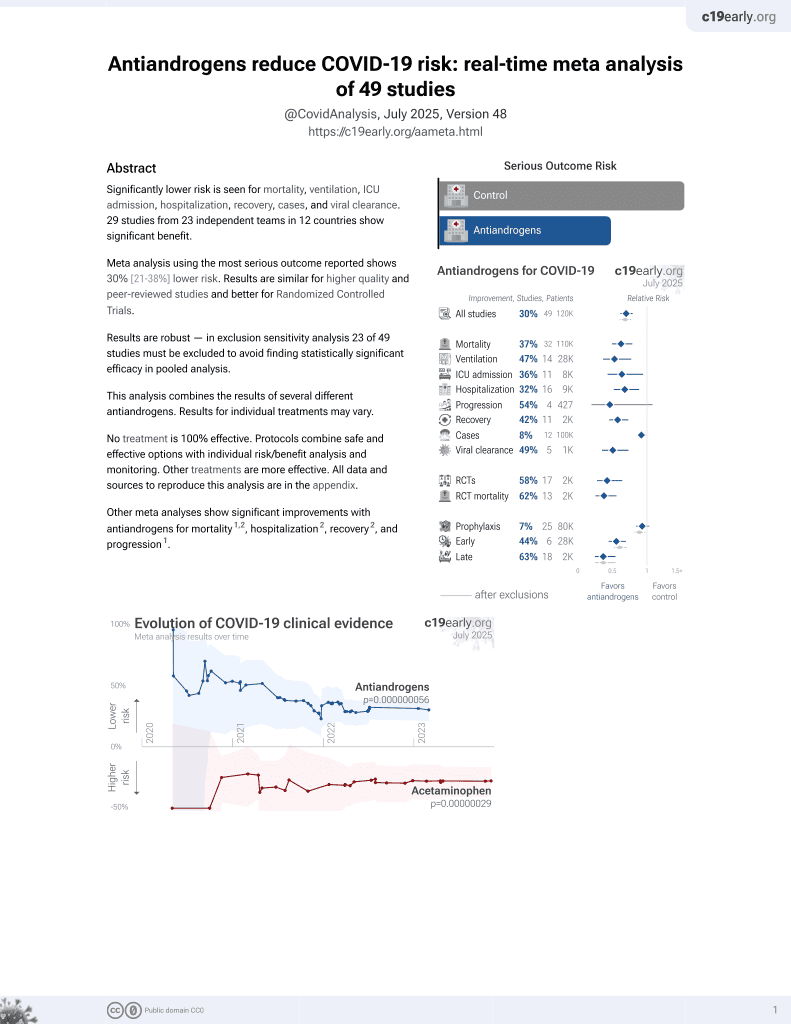
A population-level analysis of the protective effects of androgen deprivation therapy against COVID-19 disease incidence and severity
et al., Frontiers in Medicine, doi:10.3389/fmed.2022.774773, Mar 2022
7th treatment shown to reduce risk in
September 2020, now with p = 0.000000056 from 49 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 3,057 androgen deprivation therapy patients in the USA, and 36,096 control patients with cancer, showing lower risk of cases and severity with ADT.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
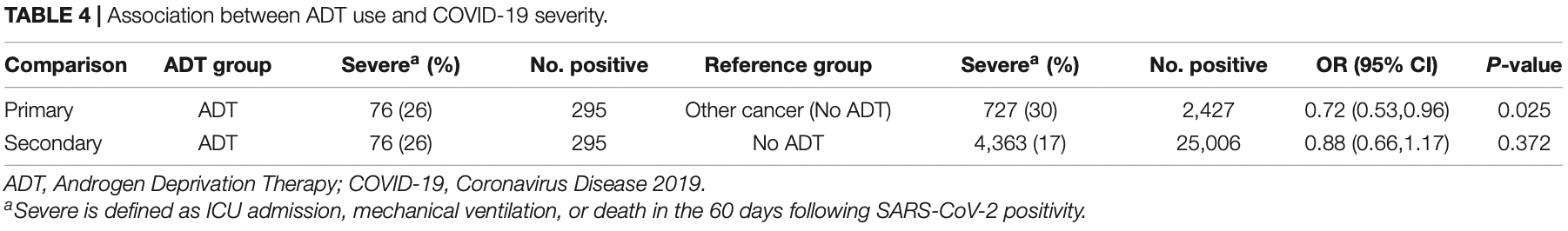
risk of severe case, 21.4% lower, RR 0.79, p = 0.03, treatment 76 of 295 (25.8%), control 727 of 2,427 (30.0%), NNT 24, adjusted per study, odds ratio converted to relative risk, propensity score weighting, multivariable.
|
|
risk of case, 11.3% lower, RR 0.89, p < 0.001, treatment 295 of 3,057 (9.6%), control 2,427 of 36,096 (6.7%), adjusted per study, odds ratio converted to relative risk, propensity score weighting, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Lee et al., 7 Mar 2022, retrospective, USA, peer-reviewed, 14 authors, study period 15 February, 2020 - 15 July, 2020.
Contact: rhauger@health.ucsd.edu, mrettig@mednet.ucla.edu.
A Population-Level Analysis of the Protective Effects of Androgen Deprivation Therapy Against COVID-19 Disease Incidence and Severity
Frontiers in Medicine, doi:10.3389/fmed.2022.774773
Background: The incidence and severity of coronavirus disease 19 (COVID-19) is substantially higher in men. Sex hormones may be a potential mechanism for differences in COVID-19 outcome in men and women. We hypothesized that men treated with androgen deprivation therapy (ADT) have lower incidence and severity of COVID-19.
Methods: We conducted an observational study of male Veterans treated in the Veterans Health Administration from February 15th to July 15th, 2020. We developed a propensity score model to predict the likelihood to undergo Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) testing. We performed multivariable logistic regression modeling adjusted with inverse probability weighting to examine the relationship between ADT and COVID-19 incidence. We conducted logistic regression analysis among COVID-19 patients to test the association between ADT and COVID-19 severity. Results: We identified a large cohort of 246,087 VA male patients who had been tested for SARS-CoV-2, of whom 3,057 men were exposed to ADT, and 36,096 men with cancer without ADT. Of these, 295 ADT patients and 2,427 cancer patients not on ADT had severe COVID-19 illness. In the primary, propensity-weighted comparison of ADT patients to cancer patients not on ADT, ADT was associated with decreased likelihood of testing positive for SARS-CoV-2 (adjusted OR, 0.88 [95% CI, 0.81-0.95]; p = 0.001).
Rules of Behavior for Access and Use of Data from VHA Vital Status File. The data are not publicly available. Further inquiries can be directed to the corresponding author.
ETHICS STATEMENT The studies involving human participants were reviewed and approved by the VA Central Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
AUTHOR CONTRIBUTIONS
SUPPLEMENTARY MATERIAL The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.
2022.774773/full#supplementary-material Author Disclaimer: The views expressed are those of the authors and do not necessarily represent the views or policy of the Department of Veterans Affairs or the United States Government. Conflict of Interest: SL reports equity in Gilead Sciences, Inc. SD reports research grants from the following for-profit organizations outside this submitted work: Alnylam Pharmaceuticals Inc., AbbVie Inc., Astellas Pharma Inc., AstraZeneca Pharmaceuticals LP, Biodesix, Inc., Boehringer Ingelheim International GmbH, Celgene Corporation, Eli Lilly and Company, Genentech Inc., Gilead Sciences Inc., GlaxoSmithKline PLC, Innocrin Pharmaceuticals Inc., Janssen Pharmaceuticals, Inc., Kantar Health, Myriad Genetic Laboratories, Inc., Novartis International AG, and Parexel International Corporation through the University of Utah or Western..
References
Baldassarri, Picchiotti, Fava, Fallerini, Benetti et al., Shorter androgen receptor polyQ alleles protect against life-threatening COVID-19 disease in European males, EBioMedicine, doi:10.1016/j.ebiom.2021.103246
Benigni, Cassis, Remuzzi, Angiotensin II revisited: new roles in inflammation, immunology and aging, EMBO Mol Med, doi:10.1002/emmm.201000080
Biesheuvel, Vergouwe, Oudega, Hoes, Grobbee et al., Advantages of the nested case-control design in diagnostic research, BMC Med Res Methodol, doi:10.1186/1471-2288-8-48
Brown, Su, An inconvenient variable: sex hormones and their impact on T cell responses, J Immunol, doi:10.4049/jimmunol.1801403
Bupp, Jorgensen, Androgen-induced immunosuppression, Front Immunol, doi:10.3389/fimmu.2018.00794
Cheng, Zhou, To, Chu, Li et al., Identification of TMPRSS2 as a susceptibility gene for severe 2009 pandemic A(H1N1) influenza and A(H7N9) influenza, J Infect Dis, doi:10.1093/infdis/jiv246
Desai, Franklin, Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: a primer for practitioners, BMJ-BRITISH Med J, doi:10.1136/bmj.l5657
Dhindsa, Zhang, Mcphaul, Wu, Ghoshal et al., Association of circulating sex hormones with inflammation and disease severity in patients with COVID-19, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.11398
Forrester, Booz, Sigmund, Coffman, Kawai et al., Angiotensin II signal transduction: an update on mechanisms of physiology and pathophysiology, Physiol Rev, doi:10.1152/physrev.00038.2017
Gebhard, Regitz-Zagrosek, Neuhauser, Morgan, Klein, Impact of sex and gender on COVID-19 outcomes in Europe, Biol Sex Differ, doi:10.1186/s13293-020-00304-9
Gersh, Keefe, Lavie, Henry, The renin-angiotensinaldosterone system in postmenopausal women: the promise of hormone therapy, Mayo Clin Proc, doi:10.1016/j.mayocp.2021.08.009
Griffith, Morris, Tudball, Herbert, Mancano et al., Collider bias undermines our understanding of COVID-19 disease risk and severity, Nat Commun, doi:10.1038/s41467-020-19478-2
Heurich, Hofmann-Winkler, Gierer, Liepold, Jahn et al., TMPRSS2 and ADAM17 cleave ACE2 differentially and only proteolysis by TMPRSS2 augments entry driven by the severe acute respiratory syndrome coronavirus spike protein, J Virol, doi:10.1128/JVI.02202-13
Hoffmann, Kleine-Weber, Schroeder, Krüger, Herrler et al., SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Hussain, Mahawar, Xia, Yang, El-Hasani, Obesity and mortality of COVID-19. Meta-analysis, Obes Res Clin Pract, doi:10.1016/j.orcp.2020.07.002
Irham, Chou, Calkins, Adikusuma, Hsieh et al., Genetic variants that influence SARS-CoV-2 receptor TMPRSS2 expression among population cohorts from multiple continents, Biochem Biophys Res Commun, doi:10.1016/j.bbrc.2020.05.179
Kissick, Sanda, Dunn, Pellegrini, On et al., Androgens alter T-cell immunity by inhibiting T-helper 1 differentiation, Proc Natl Acad Sci U S A, doi:10.1073/pnas.1402468111
Klein, Li, Milinovich, Schold, Sharifi et al., Androgen deprivation therapy in men with prostate cancer does not affect risk of infection with SARS-CoV-2, J Urol, doi:10.1097/JU.0000000000001338
Kopel, Perisetti, Roghani, Aziz, Gajendran et al., Racial and gender-based differences in COVID-19, Front Public Heal, doi:10.3389/fpubh.2020.00418
Koskinen, Carpen, Honkanen, Seppänen, Miettinen et al., Androgen deprivation and SARS-CoV-2 in men with prostate cancer, Ann Oncol Off J Eur Soc Med Oncol, doi:10.1016/j.annonc.2020.06.015
Kwon, Vashisht, Borno, Aggarwal, Small et al., Androgen-deprivation therapy and SARS-CoV-2 in men with prostate cancer: findings from the University of California Health System registry, Ann Oncol Off J Eur Soc Med Oncol, doi:10.1016/j.annonc.2021.01.067
Lucas, Wong, Klein, Castro, Silva et al., Longitudinal analyses reveal immunological misfiring in severe COVID-19, Nature, doi:10.1038/s41586-020-2588-y
Majoros, Platanitis, Kernbauer-Hölzl, Rosebrock, Müller et al., Canonical and non-canonical aspects of JAK-STAT signaling: lessons from interferons for cytokine responses, Front Immunol, doi:10.3389/fimmu.2017.00029
Mccoy, Wambier, Herrera, Vaño-Galván, Gioia et al., Androgen receptor genetic variant predicts COVID-19 disease severity: a prospective longitudinal study of hospitalized COVID-19 male patients, J Eur Acad Dermatol Venereol, doi:10.1111/jdv.16956
Montopoli, Zumerle, Vettor, Rugge, Zorzi et al., Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532), Ann Oncol, doi:10.1016/j.annonc.2020.04.479
Pagadala, Jasuja, Palnati, Lynch, Anglin et al., Discovery of novel trans-ancestry and ancestry-specific gene loci for total testosterone in a multi-ancestral analysis of men in the million veteran program, medRxiv, doi:10.1101/2022.02.16.21265846
Patel, Zhong, Liaw, Tremblay, Tsao et al., Does androgen deprivation therapy protect against severe complications from COVID-19?, Ann Oncol, doi:10.1016/j.annonc.2020.06.023
Quan, Sundararajan, Halfon, Fong, Burnand et al., Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data, Med Care, doi:10.1097/01.mlr.0000182534.19832.83
Richardson, Hirsch, Narasimhan, Crawford, Mcginn et al., Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area, JAMA, doi:10.1001/jama.2020.6775
Salciccia, Giudice, Eisenberg, Mastroianni, Berardinis et al., Testosterone target therapy: focus on immune response, controversies and clinical implications in patients with COVID-19 infection, Ther Adv Endocrinol Metab, doi:10.1177/20420188211010105
Seaman, White, Review of inverse probability weighting for dealing with missing data, Stat Methods Med Res, doi:10.1177/0962280210395740
Sharma, Stevens, Obukhov, Grant, Oudit et al., ACE2 (Angiotensin-Converting Enzyme 2) in cardiopulmonary diseases: ramifications for the control of SARS-CoV-2, Hypertension, doi:10.1161/HYPERTENSIONAHA.120.15595
Stopsack, Mucci, Antonarakis, Nelson, Kantoff, TMPRSS2 and COVID-19: serendipity or opportunity for intervention?, Cancer Discov, doi:10.1158/2159-8290.CD-20-0451
Sullivan, Sex and the renin-angiotensin system: inequality between the sexes in response to RAS stimulation and inhibition, Am J Physiol Integr Comp Physiol, doi:10.1152/ajpregu.00864.2007
Thunders, Delahunt, Gene of the month: TMPRSS2 (transmembrane serine protease 2), J Clin Pathol, doi:10.1136/jclinpath-2020-206987
Trigunaite, Dimo, Jørgensen, Suppressive effects of androgens on the immune system, Cell Immunol, doi:10.1016/j.cellimm.2015.02.004
Vaduganathan, Vardeny, Michel, Mcmurray, Pfeffer et al., Renin-Angiotensin-aldosterone system inhibitors in patients with Covid-19, N Engl J Med, doi:10.1056/NEJMsr2005760
Verma, Tsao, Thomann, Ho, Iyengar et al., A Phenome-Wide Association Study of genes associated with COVID-19 severity reveals shared genetics with complex diseases in the Million Veteran Program, doi:10.1101/2021.05.18.21257396
Viveiros, Rasmuson, Vu, Mulvagh, Yip et al., Sex differences in COVID-19: candidate pathways, genetics of ACE2, and sex hormones, Am J Physiol Circ Physiol, doi:10.1152/ajpheart.00755.2020
Wenham, Smith, Morgan, COVID-19: the gendered impacts of the outbreak, Lancet, doi:10.1016/S0140-6736(20)30526-2
Wiersinga, Rhodes, Cheng, Peacock, Prescott, Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review, JAMA, doi:10.1001/jama.2020.12839
Wu, Maric, Roesch, Zheng, Verbalis et al., Estrogen regulates adrenal angiotensin AT1 receptors by modulating AT1 receptor translation, Endocrinology, doi:10.1210/en.2003-0015
DOI record:
{
"DOI": "10.3389/fmed.2022.774773",
"ISSN": [
"2296-858X"
],
"URL": "http://dx.doi.org/10.3389/fmed.2022.774773",
"abstract": "<jats:sec><jats:title>Background</jats:title><jats:p>The incidence and severity of coronavirus disease 19 (COVID-19) is substantially higher in men. Sex hormones may be a potential mechanism for differences in COVID-19 outcome in men and women. We hypothesized that men treated with androgen deprivation therapy (ADT) have lower incidence and severity of COVID-19.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>We conducted an observational study of male Veterans treated in the Veterans Health Administration from February 15th to July 15th, 2020. We developed a propensity score model to predict the likelihood to undergo Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) testing. We performed multivariable logistic regression modeling adjusted with inverse probability weighting to examine the relationship between ADT and COVID-19 incidence. We conducted logistic regression analysis among COVID-19 patients to test the association between ADT and COVID-19 severity.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>We identified a large cohort of 246,087 VA male patients who had been tested for SARS-CoV-2, of whom 3,057 men were exposed to ADT, and 36,096 men with cancer without ADT. Of these, 295 ADT patients and 2,427 cancer patients not on ADT had severe COVID-19 illness. In the primary, propensity-weighted comparison of ADT patients to cancer patients not on ADT, ADT was associated with decreased likelihood of testing positive for SARS-CoV-2 (adjusted OR, 0.88 [95% CI, 0.81–0.95]; <jats:italic>p</jats:italic> = 0.001). Furthermore, ADT was associated with fewer severe COVID-19 outcomes (OR 0.72 [95% CI 0.53–0.96]; <jats:italic>p</jats:italic> = 0.03).</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>ADT is associated with reduced incidence and severity of COVID-19 amongst male Veterans. Testosterone and androgen receptor signaling may confer increased risk for SARS-CoV-2 infection and contribute to severe COVID-19 pathophysiology in men.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fmed.2022.774773"
],
"author": [
{
"affiliation": [],
"family": "Lee",
"given": "Kyung Min",
"sequence": "first"
},
{
"affiliation": [],
"family": "Heberer",
"given": "Kent",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gao",
"given": "Anthony",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Becker",
"given": "Daniel J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Loeb",
"given": "Stacy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Makarov",
"given": "Danil V.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gulanski",
"given": "Barbara",
"sequence": "additional"
},
{
"affiliation": [],
"family": "DuVall",
"given": "Scott L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aslan",
"given": "Mihaela",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lee",
"given": "Jennifer",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shih",
"given": "Mei-Chiung",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lynch",
"given": "Julie A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hauger",
"given": "Richard L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rettig",
"given": "Matthew",
"sequence": "additional"
}
],
"container-title": "Frontiers in Medicine",
"container-title-short": "Front. Med.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2022,
5,
4
]
],
"date-time": "2022-05-04T07:53:58Z",
"timestamp": 1651650838000
},
"deposited": {
"date-parts": [
[
2022,
5,
4
]
],
"date-time": "2022-05-04T07:54:02Z",
"timestamp": 1651650842000
},
"funder": [
{
"DOI": "10.13039/100000738",
"award": [
"825-MS-DI-33848"
],
"doi-asserted-by": "publisher",
"name": "U.S. Department of Veterans Affairs"
}
],
"indexed": {
"date-parts": [
[
2022,
5,
4
]
],
"date-time": "2022-05-04T08:15:03Z",
"timestamp": 1651652103881
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
5,
4
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
5,
4
]
],
"date-time": "2022-05-04T00:00:00Z",
"timestamp": 1651622400000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2022.774773/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2022,
5,
4
]
]
},
"published-online": {
"date-parts": [
[
2022,
5,
4
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"journal-title": "WHO Coronavirus Disease (COVID-19) Dashboard.",
"key": "B1",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.6775",
"article-title": "Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area.",
"author": "Richardson",
"doi-asserted-by": "publisher",
"first-page": "2052",
"journal-title": "JAMA.",
"key": "B2",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2020.00418",
"article-title": "Racial and gender-based differences in COVID-19.",
"author": "Kopel",
"doi-asserted-by": "publisher",
"first-page": "418",
"journal-title": "Front Public Heal.",
"key": "B3",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.orcp.2020.07.002",
"article-title": "Obesity and mortality of COVID-19. Meta-analysis.",
"author": "Hussain",
"doi-asserted-by": "publisher",
"first-page": "295",
"journal-title": "Obes Res Clin Pract.",
"key": "B4",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30526-2",
"article-title": "COVID-19: the gendered impacts of the outbreak.",
"author": "Wenham",
"doi-asserted-by": "publisher",
"first-page": "846",
"journal-title": "Lancet.",
"key": "B5",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1186/s13293-020-00304-9",
"article-title": "Impact of sex and gender on COVID-19 outcomes in Europe.",
"author": "Gebhard",
"doi-asserted-by": "publisher",
"first-page": "29",
"journal-title": "Biol Sex Differ.",
"key": "B6",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2018.00794",
"article-title": "Androgen-induced immunosuppression.",
"author": "Gubbels Bupp",
"doi-asserted-by": "publisher",
"first-page": "794",
"journal-title": "Front Immunol.",
"key": "B7",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1016/j.cellimm.2015.02.004",
"article-title": "Suppressive effects of androgens on the immune system.",
"author": "Trigunaite",
"doi-asserted-by": "publisher",
"first-page": "87",
"journal-title": "Cell Immunol.",
"key": "B8",
"volume": "294",
"year": "2015"
},
{
"DOI": "10.1001/jama.2020.12839",
"article-title": "Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review.",
"author": "Wiersinga",
"doi-asserted-by": "publisher",
"first-page": "782",
"journal-title": "JAMA.",
"key": "B9",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1056/NEJMsr2005760",
"article-title": "Renin-Angiotensin-aldosterone system inhibitors in patients with Covid-19.",
"author": "Vaduganathan",
"doi-asserted-by": "publisher",
"first-page": "1653",
"journal-title": "N Engl J Med.",
"key": "B10",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1128/JVI.02202-13",
"article-title": "TMPRSS2 and ADAM17 cleave ACE2 differentially and only proteolysis by TMPRSS2 augments entry driven by the severe acute respiratory syndrome coronavirus spike protein.",
"author": "Heurich",
"doi-asserted-by": "publisher",
"first-page": "1293",
"journal-title": "J Virol.",
"key": "B11",
"volume": "88",
"year": "2014"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor.",
"author": "Hoffmann",
"doi-asserted-by": "publisher",
"first-page": "271",
"journal-title": "Cell.",
"key": "B12",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1158/2159-8290.CD-20-0451",
"article-title": "TMPRSS2 and COVID-19: serendipity or opportunity for intervention?",
"author": "Stopsack",
"doi-asserted-by": "publisher",
"first-page": "779",
"journal-title": "Cancer Discov.",
"key": "B13",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1016/j.bbrc.2020.05.179",
"article-title": "Genetic variants that influence SARS-CoV-2 receptor TMPRSS2 expression among population cohorts from multiple continents.",
"author": "Irham",
"doi-asserted-by": "publisher",
"first-page": "263",
"journal-title": "Biochem Biophys Res Commun.",
"key": "B14",
"volume": "529",
"year": "2020"
},
{
"DOI": "10.1136/jclinpath-2020-206987",
"article-title": "Gene of the month: TMPRSS2 (transmembrane serine protease 2).",
"author": "Thunders",
"doi-asserted-by": "publisher",
"first-page": "773",
"journal-title": "J Clin Pathol.",
"key": "B15",
"volume": "73",
"year": "2020"
},
{
"DOI": "10.1093/infdis/jiv246",
"article-title": "Identification of TMPRSS2 as a susceptibility gene for severe 2009 pandemic A(H1N1) influenza and A(H7N9) influenza.",
"author": "Cheng",
"doi-asserted-by": "publisher",
"first-page": "1214",
"journal-title": "J Infect Dis.",
"key": "B16",
"volume": "212",
"year": "2015"
},
{
"DOI": "10.1016/j.annonc.2020.04.479",
"article-title": "Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532).",
"author": "Montopoli",
"doi-asserted-by": "publisher",
"first-page": "1040",
"journal-title": "Ann Oncol.",
"key": "B17",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1097/JU.0000000000001338",
"article-title": "Androgen deprivation therapy in men with prostate cancer does not affect risk of infection with SARS-CoV-2.",
"author": "Klein",
"doi-asserted-by": "publisher",
"first-page": "441",
"journal-title": "J Urol.",
"key": "B18",
"volume": "205",
"year": "2020"
},
{
"DOI": "10.1016/j.annonc.2020.06.023",
"article-title": "Does androgen deprivation therapy protect against severe complications from COVID-19?",
"author": "Patel",
"doi-asserted-by": "publisher",
"first-page": "1419",
"journal-title": "Ann Oncol.",
"key": "B19",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1016/j.annonc.2020.06.015",
"article-title": "Androgen deprivation and SARS-CoV-2 in men with prostate cancer.",
"author": "Koskinen",
"doi-asserted-by": "publisher",
"first-page": "1417",
"journal-title": "Ann Oncol Off J Eur Soc Med Oncol.",
"key": "B20",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1016/j.annonc.2021.01.067",
"article-title": "Androgen-deprivation therapy and SARS-CoV-2 in men with prostate cancer: findings from the University of California Health System registry.",
"author": "Kwon",
"doi-asserted-by": "publisher",
"first-page": "678",
"journal-title": "Ann Oncol Off J Eur Soc Med Oncol.",
"key": "B21",
"volume": "32",
"year": "2021"
},
{
"journal-title": "VA COVID-19: Shared Data Resource.",
"key": "B22",
"year": "2020"
},
{
"DOI": "10.1097/01.mlr.0000182534.19832.83",
"article-title": "Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data.",
"author": "Quan",
"doi-asserted-by": "publisher",
"first-page": "1130",
"journal-title": "Med Care.",
"key": "B23",
"volume": "43",
"year": "2005"
},
{
"DOI": "10.1038/s41467-020-19478-2",
"article-title": "Collider bias undermines our understanding of COVID-19 disease risk and severity.",
"author": "Griffith",
"doi-asserted-by": "publisher",
"first-page": "5749",
"journal-title": "Nat Commun.",
"key": "B24",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1177/0962280210395740",
"article-title": "Review of inverse probability weighting for dealing with missing data.",
"author": "Seaman",
"doi-asserted-by": "publisher",
"first-page": "278",
"journal-title": "Stat Methods Med Res.",
"key": "B25",
"volume": "22",
"year": "2013"
},
{
"DOI": "10.1136/bmj.l5657",
"article-title": "Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: a primer for practitioners.",
"author": "Desai",
"doi-asserted-by": "publisher",
"first-page": "l5657",
"journal-title": "BMJ-BRITISH Med J.",
"key": "B26",
"volume": "367",
"year": "2019"
},
{
"DOI": "10.1186/1471-2288-8-48",
"article-title": "Advantages of the nested case-control design in diagnostic research.",
"author": "Biesheuvel",
"doi-asserted-by": "publisher",
"first-page": "48",
"journal-title": "BMC Med Res Methodol.",
"key": "B27",
"volume": "8",
"year": "2008"
},
{
"DOI": "10.4049/jimmunol.1801403",
"article-title": "An inconvenient variable: sex hormones and their impact on T cell responses.",
"author": "Brown",
"doi-asserted-by": "publisher",
"first-page": "1927",
"journal-title": "J Immunol.",
"key": "B28",
"volume": "202",
"year": "2019"
},
{
"DOI": "10.1038/s41586-020-2588-y",
"article-title": "Longitudinal analyses reveal immunological misfiring in severe COVID-19.",
"author": "Lucas",
"doi-asserted-by": "publisher",
"first-page": "463",
"journal-title": "Nature.",
"key": "B29",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2017.00029",
"article-title": "Canonical and non-canonical aspects of JAK-STAT signaling: lessons from interferons for cytokine responses.",
"author": "Majoros",
"doi-asserted-by": "publisher",
"first-page": "29",
"journal-title": "Front Immunol.",
"key": "B30",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.1073/pnas.1402468111",
"article-title": "Androgens alter T-cell immunity by inhibiting T-helper 1 differentiation.",
"author": "Kissick",
"doi-asserted-by": "publisher",
"first-page": "9887",
"journal-title": "Proc Natl Acad Sci U S A.",
"key": "B31",
"volume": "111",
"year": "2014"
},
{
"DOI": "10.1101/2021.05.18.21257396",
"article-title": "A Phenome-Wide Association Study of genes associated with COVID-19 severity reveals shared genetics with complex diseases in the Million Veteran Program.",
"author": "Verma",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv[Preprint].",
"key": "B32",
"year": "2021"
},
{
"DOI": "10.1002/emmm.201000080",
"article-title": "Angiotensin II revisited: new roles in inflammation, immunology and aging.",
"author": "Benigni",
"doi-asserted-by": "publisher",
"first-page": "247",
"journal-title": "EMBO Mol Med.",
"key": "B33",
"volume": "2",
"year": "2010"
},
{
"DOI": "10.1152/physrev.00038.2017",
"article-title": "Angiotensin II signal transduction: an update on mechanisms of physiology and pathophysiology.",
"author": "Forrester",
"doi-asserted-by": "publisher",
"first-page": "1627",
"journal-title": "Physiol Rev.",
"key": "B34",
"volume": "98",
"year": "2018"
},
{
"DOI": "10.1161/HYPERTENSIONAHA.120.15595",
"article-title": "ACE2 (Angiotensin-Converting Enzyme 2) in cardiopulmonary diseases: ramifications for the control of SARS-CoV-2.",
"author": "Sharma",
"doi-asserted-by": "publisher",
"first-page": "651",
"journal-title": "Hypertension.",
"key": "B35",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1152/ajpregu.00864.2007",
"article-title": "Sex and the renin-angiotensin system: inequality between the sexes in response to RAS stimulation and inhibition.",
"author": "Sullivan",
"doi-asserted-by": "publisher",
"first-page": "R1220",
"journal-title": "Am J Physiol Integr Comp Physiol.",
"key": "B36",
"volume": "294",
"year": "2008"
},
{
"DOI": "10.1152/ajpheart.00755.2020",
"article-title": "Sex differences in COVID-19: candidate pathways, genetics of ACE2, and sex hormones.",
"author": "Viveiros",
"doi-asserted-by": "publisher",
"first-page": "H296",
"journal-title": "Am J Physiol Circ Physiol.",
"key": "B37",
"volume": "320",
"year": "2021"
},
{
"DOI": "10.1016/j.mayocp.2021.08.009",
"article-title": "The renin-angiotensin-aldosterone system in postmenopausal women: the promise of hormone therapy.",
"author": "Gersh",
"doi-asserted-by": "publisher",
"first-page": "3130",
"journal-title": "Mayo Clin Proc.",
"key": "B38",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1210/en.2003-0015",
"article-title": "Estrogen regulates adrenal angiotensin AT1 receptors by modulating AT1 receptor translation.",
"author": "Wu",
"doi-asserted-by": "publisher",
"first-page": "3251",
"journal-title": "Endocrinology.",
"key": "B39",
"volume": "144",
"year": "2003"
},
{
"DOI": "10.1210/endocr/bqab114",
"article-title": "Do Anti-androgens have potential as therapeutics for COVID-19?",
"author": "Mauvais-Jarvis",
"doi-asserted-by": "publisher",
"first-page": "bqab114",
"journal-title": "Endocrinology.",
"key": "B40",
"volume": "162",
"year": "2021"
},
{
"DOI": "10.1177/20420188211010105",
"article-title": "Testosterone target therapy: focus on immune response, controversies and clinical implications in patients with COVID-19 infection.",
"author": "Salciccia",
"doi-asserted-by": "publisher",
"first-page": "20420188211010104",
"journal-title": "Ther Adv Endocrinol Metab.",
"key": "B41",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.11398",
"article-title": "Association of circulating sex hormones with inflammation and disease severity in patients with COVID-19.",
"author": "Dhindsa",
"doi-asserted-by": "publisher",
"first-page": "e2111398",
"journal-title": "JAMA Netw Open.",
"key": "B42",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1016/j.ebiom.2021.103246",
"article-title": "Shorter androgen receptor polyQ alleles protect against life-threatening COVID-19 disease in European males.",
"author": "Baldassarri",
"doi-asserted-by": "publisher",
"first-page": "103246",
"journal-title": "EBioMedicine.",
"key": "B43",
"volume": "65",
"year": "2021"
},
{
"DOI": "10.1111/jdv.16956",
"article-title": "Androgen receptor genetic variant predicts COVID-19 disease severity: a prospective longitudinal study of hospitalized COVID-19 male patients.",
"author": "McCoy",
"doi-asserted-by": "publisher",
"first-page": "e15",
"journal-title": "J Eur Acad Dermatol Venereol.",
"key": "B44",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1101/2022.02.16.21265846",
"article-title": "Discovery of novel trans-ancestry and ancestry-specific gene loci for total testosterone in a multi-ancestral analysis of men in the million veteran program.",
"author": "Pagadala",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv[Preprint].",
"key": "B45",
"year": "2022"
}
],
"reference-count": 45,
"references-count": 45,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2022.774773/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "A Population-Level Analysis of the Protective Effects of Androgen Deprivation Therapy Against COVID-19 Disease Incidence and Severity",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "9"
}