Androgen Drives the Expression of SARS-CoV-2 Entry Proteins in Sinonasal Tissue
et al., Journal of Clinical and Translational Pathology, doi:10.14218/jctp.2022.00031, May 2023
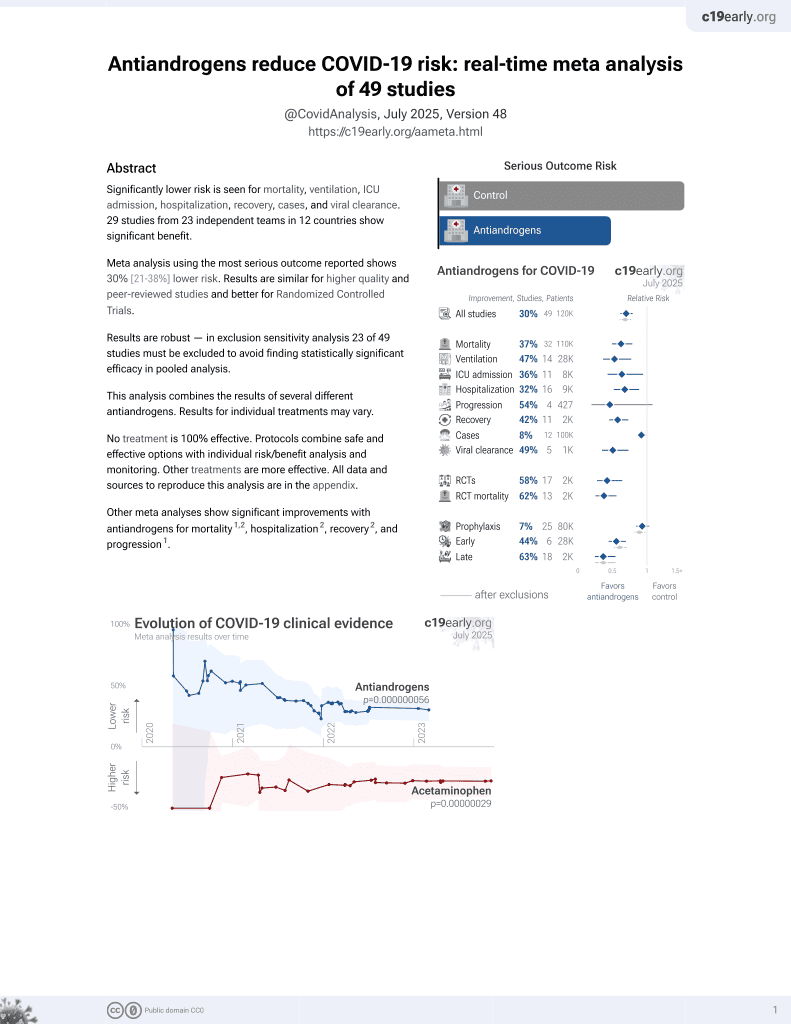
7th treatment shown to reduce risk in
September 2020, now with p = 0.000000056 from 49 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
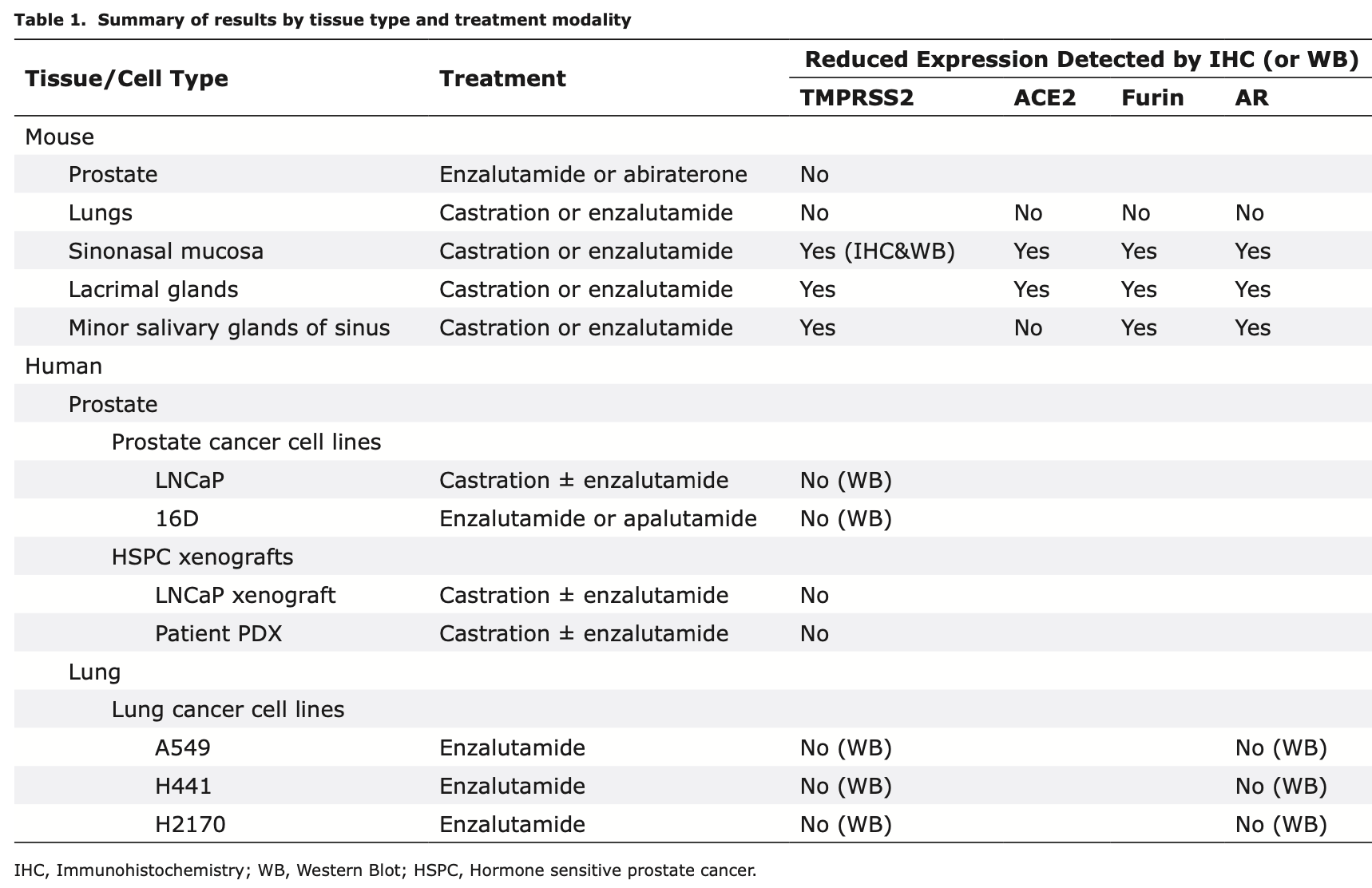
Mouse study showing that androgen deprivation therapy (ADT) reduced expression of SARS-CoV-2 viral entry proteins TMPRSS2, ACE2, and furin in sinonasal tissue and adjacent glands, but not in lungs. Authors found that surgical castration or treatment with antiandrogens enzalutamide or bicalutamide decreased expression of these proteins in nasal epithelium, lacrimal glands, and minor salivary glands of mice. No changes were seen in mouse lungs. Analysis of human tissue also suggested a potential role for ADT in sinonasal tissue but not in the lung.
4 preclinical studies support the efficacy of antiandrogens for COVID-19:
1.
Saih et al., In-Silico Molecular Docking, Validation, Drug-Likeness, and ADMET Studies of Antiandrogens to Use in the Fight against SARS-CoV-2, Physical Chemistry Research, doi:10.22036/pcr.2022.324549.2016.
2.
Majidipur et al., Apalutamide Prevents SARS-CoV-2 Infection in Lung Epithelial Cells and in Human Nasal Epithelial Cells, International Journal of Molecular Sciences, doi:10.3390/ijms24043288.
Huang et al., 1 May 2023, peer-reviewed, 12 authors.
Contact: rhuang@mednet.ucla.edu, huihui.ye@cshs.org.
Androgen Drives the Expression of SARS-CoV-2 Entry Proteins in Sinonasal Tissue
Journal of Clinical and Translational Pathology, doi:10.14218/jctp.2022.00031
Background and objectives: Men have higher morbidity and mortality from COVID-19 than women, possibly due to androgen receptor-regulated viral entry protein expression. This led to a clinical trial of androgen deprivation therapy (ADT), which has not shown a significant benefit in the outcomes among hospitalized male COVID-19 patients. The aim of this study was to explore biological explanations for the failure of ADT to mitigate clinical outcomes in men with severe COVID-19 by assessing the role of androgen in regulating viral entry protein expression in the upper and lower respiratory tract. Methods: Immunohistochemistry was used to assess the expression of transmembrane serine protease 2 (TMPRSS2) and angiotensin-converting enzyme 2 (ACE2) and how it correlated to androgen receptor expression in the sinonasal epithelium, minor salivary glands of the sinus, lacrimal glands, and lungs from mice pretreated with and without castration and ADT as well as the sinonasal epithelium obtained from healthy human donors and hospitalized COVID-19 patients. Results: In murine models, castration and ADT treatment downregulated the expression of TMPRSS2 and ACE2 in the sinonasal epithelium, minor salivary glands of the sinus, and lacrimal glands, but not in the lungs. Correlative analyses using human tissue also showed a potential role of ADT in men during the early sinonasal phase but not in the later lung phase of SARS-CoV-2 infection. Conclusions: Our study suggests a potential benefit of ADT in male patients with early COVID-19 when the virus enters the nasopharynx, but not in those with advanced disease. The downregulation of viral entry proteins in the upper respiratory system following androgen blockade may be a key mechanism for this effect.
Funding The authors gratefully acknowledge research support from the UCLA David Geffen School of Medicine
Conflict of interest The authors have no conflicts of interest related to this publication.
Author contributions Study design, performance of experiments, analysis and interpretation of data, critical revision (RRH); performance of experiments, analysis and interpretation of data, statistical analysis (JMG, TH); study design, analysis and interpretation of data, critical funding, administration, technical and material support (LYZ); performance of experiments (WBY); technical support, administration (JYR); performance of experiments, analysis and interpretation of data (JWR); technical and material support (SPB); technical and material support, administration (NGN); study design, analysis and interpretation of data, critical revision, administration, material support (MBR); Study design, analysis and interpretation of data, technical and material support (AG); study design, analysis and interpretation of data, manuscript writing, critical revision, administration, technical and material support (HY). All authors have made a significant contribution to this study and have approved the final manuscript.
Ethical statement This study was carried out in accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. The protocol was approved by the Animal Research Committee on the Ethics of Animal..
References
Ahn, Kim, Hong, Choi, Yang et al., Nasal ciliated cells are primary targets for SARS-CoV-2 replication in the early stage of COVID-19, J Clin Invest, doi:10.1172/JCI148517
Baig, Ahmad, Khaleeq, Rafique, Rajput et al., Ocular COVID-19: Eyes as a Reservoir to Conceal and Spread SARSCoV-2, Infect Disord Drug Targets, doi:10.2174/1871526520999200729182242
Baratchian, Mcmanus, Berk, Nakamura, Mukhopadhyay et al., Androgen regulation of pulmonary AR, TMPRSS2 and ACE2 with implications for sex-discordant COVID-19 outcomes, Sci Rep, doi:10.1038/s41598-021-90491-1
Bestle, Heindl, Limburg, Lam Van T, Pilgram et al., TMPRSS2 and furin are both essential for proteolytic activation of SARS-CoV-2 in human airway cells, Life Sci Alliance, doi:10.26508/lsa.202000786
Cadegiani, Mccoy, Wambier, Goren, Early Antiandrogen Therapy With Dutasteride Reduces Viral Shedding, Inflammatory Responses, and Time-to-Remission in Males With COVID-19: A Randomized, Double-Blind, Placebo-Controlled Interventional Trial (EAT-DUTA AndroCoV Trial -Biochemical), Cureus, doi:10.7759/cureus.13047
Cadegiani, Mccoy, Wambier, Vaño-Galván, Shapiro et al., Proxalutamide Significantly Accelerates Viral Clearance and Reduces Time to Clinical Remission in Patients with Mild to Moderate COVID-19: Results from a Randomized, Double-Blinded, Placebo-Controlled Trial, Cureus, doi:10.7759/cureus.13492
Cadegiani, Zimerman, Fonseca, Correia, Muller et al., Final Results of a Randomized, Placebo-Controlled, Two-Arm, Parallel Clinical Trial of Proxalutamide for Hospitalized COVID-19 Patients: A Multiregional, Joint Analysis of the Proxa-Rescue AndroCoV Trial, Cureus, doi:10.7759/cureus.20691
Cevik, Kuppalli, Kindrachuk, Peiris, Virology, transmission, and pathogenesis of SARS-CoV-2, BMJ, doi:10.1136/bmj.m3862
Chakravarty, Nair, Hammouda, Ratnani, Gharib et al., Sex differences in SARS-CoV-2 infection rates and the potential link to prostate cancer, Commun Biol, doi:10.1038/s42003-020-1088-9
Deng, Rasool, Russell, Natesan, Asangani, Targeting androgen regulation of TMPRSS2 and ACE2 as a therapeutic strategy to combat COVID-19, iScience, doi:10.1016/j.isci.2021.102254
Dong, Hawker, Mcwilliam, Bangah, Burger et al., Circulating immunoreactive inhibin and testosterone levels in men with critical illness, Clin Endocrinol (Oxf), doi:10.1111/j.1365-2265.1992.tb01466.x
Foster, Taylor, Hill, Bentley, Bishop et al., Mapping the Steroid Response to Major Trauma From Injury to Recovery: A Prospective Cohort Study, J Clin Endocrinol Metab, doi:10.1210/clinem/dgz302
Guo, Porter, Crozier, Coates, Jha et al., Topical TMPRSS2 inhibition prevents SARS-CoV-2 infection in differentiated human airway cultures, Life Sci Alliance, doi:10.26508/lsa.202101116
Ho, Low, Tong, Gupta, Veeraraghavan et al., COVID-19 and the Ocular Surface: A Review of Transmission and Manifestations, Ocul Immunol Inflamm, doi:10.1080/09273948.2020.1772313
Iwasaki, Fujisawa, Nakakubo, Kamada, Yamashita et al., Comparison of SARS-CoV-2 detection in nasopharyngeal swab and saliva, J Infect, doi:10.1016/j.jinf.2020.05.071
Li, Han, Dai, Xu, He et al., Distinct mechanisms for TM-PRSS2 expression explain organ-specific inhibition of SARS-CoV-2 infection by enzalutamide, Nat Commun, doi:10.1038/s41467-021-21171-x
Martin, Wolf, Lapp, Agostini, Schlunck et al., Viral S protein histochemistry reveals few potential SARS-CoV-2 entry sites in human ocular tissues, Sci Rep, doi:10.1038/s41598-021-98709-y
Martines, Ritter, Matkovic, Gary, Bollweg et al., Pathology and Pathogenesis of SARS-CoV-2 Associated with Fatal Coronavirus Disease, United States, Emerg Infect Dis, doi:10.3201/eid2609.202095
Matuck, Dolhnikoff, Duarte-Neto, Maia, Gomes et al., Salivary glands are a target for SARS-CoV-2: a source for saliva contamination, J Pathol, doi:10.1002/path.5679
Mccoy, Goren, Cadegiani, Vaño-Galván, Kovacevic et al., Proxalutamide Reduces the Rate of Hospitalization for COVID-19 Male Outpatients: A Randomized Double-Blinded Placebo-Controlled Trial, Front Med, doi:10.3389/fmed.2021.668698
Montopoli, Zumerle, Vettor, Rugge, Zorzi et al., Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532), Ann Oncol, doi:10.1016/j.annonc.2020.04.479
Nickols, Dematt, Biswas, Clise, Huggins, Effect of Androgen Suppression on Clinical Outcomes in Hospitalized Men With COVID-19: The HITCH Randomized Clinical Trial, JAMA Netw Open, doi:10.1001/jamanetworkopen.2022.7852
Pascolo, Zupin, Melato, Tricarico, Crovella, TMPRSS2 and ACE2 Coexpression in SARS-CoV-2 Salivary Glands Infection, J Dent Res, doi:10.1177/0022034520933589
Qiao, Wang, Mannan, Pitchiaya, Zhang et al., Targeting transcriptional regulation of SARS-CoV-2 entry factors ACE2 and TMPRSS2, Proc Natl Acad Sci U S A, doi:10.1073/pnas.2021450118
Sungnak, Huang, Bécavin, Berg, Queen et al., SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes, Nat Med, doi:10.1038/s41591-020-0868-6
Tanaka, Senpuku, Ogawa, Yasuhara, Ohnuma et al., Human induced pluripotent stem cell-derived salivary gland organoids model SARS-CoV-2 infection and replication, Nat Cell Biol, doi:10.1038/s41556-022-01007-6
Wasyluk, Wasyluk, Zwolak, Sepsis as a Pan-Endocrine Illness-Endocrine Disorders in Septic Patients, J Clin Med, doi:10.3390/jcm10102075
Welén, Rosendal, Gisslén, Lenman, Freyhult et al., A Phase 2 Trial of the Effect of Antiandrogen Therapy on COVID-19 Outcome: No Evidence of Benefit, Supported by Epidemiology and In Vitro Data, Eur Urol, doi:10.1016/j.eururo.2021.12.013
Xu, Li, Gan, Du, Yao, Salivary Glands: Potential Reservoirs for COVID-19 Asymptomatic Infection, J Dent Res, doi:10.1177/0022034520918518
DOI record:
{
"DOI": "10.14218/jctp.2022.00031",
"ISSN": [
"2771-165X"
],
"URL": "http://dx.doi.org/10.14218/jctp.2022.00031",
"alternative-id": [
"10.14218/JCTP.2022.00031"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5308-8024",
"affiliation": [],
"authenticated-orcid": false,
"family": "Huang",
"given": "Rong Rong",
"sequence": "first"
},
{
"affiliation": [],
"family": "Giafaglione",
"given": "Jenna M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hashimoto",
"given": "Takao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Liying",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yu",
"given": "Weibo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rao",
"given": "Jianyu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Russo",
"given": "Joshua W.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Balk",
"given": "Steven P.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nickols",
"given": "Nicholas G.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rettig",
"given": "Mathew B.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Goldstein",
"given": "Andrew",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8307-9492",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ye",
"given": "Huihui",
"sequence": "additional"
}
],
"container-title": "Journal of Clinical and Translational Pathology",
"container-title-short": "J Clin Transl Pathol",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.xiahepublishing.com"
]
},
"created": {
"date-parts": [
[
2023,
5,
1
]
],
"date-time": "2023-05-01T04:32:02Z",
"timestamp": 1682915522000
},
"deposited": {
"date-parts": [
[
2023,
5,
1
]
],
"date-time": "2023-05-01T04:32:02Z",
"timestamp": 1682915522000
},
"indexed": {
"date-parts": [
[
2023,
5,
1
]
],
"date-time": "2023-05-01T05:11:21Z",
"timestamp": 1682917881214
},
"is-referenced-by-count": 0,
"issue": "000",
"issued": {
"date-parts": [
[
2023,
5,
1
]
]
},
"journal-issue": {
"issue": "000",
"published-online": {
"date-parts": [
[
2023,
5,
1
]
]
},
"published-print": {
"date-parts": [
[
2023,
5,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
1
]
],
"date-time": "2023-05-01T00:00:00Z",
"timestamp": 1682899200000
}
}
],
"link": [
{
"URL": "https://www.xiahepublishing.com/2771-165X/JCTP-2022-00031",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "5334",
"original-title": [],
"page": "000-000",
"prefix": "10.14218",
"published": {
"date-parts": [
[
2023,
5,
1
]
]
},
"published-online": {
"date-parts": [
[
2023,
5,
1
]
]
},
"published-print": {
"date-parts": [
[
2023,
5,
1
]
]
},
"publisher": "Xia & He Publishing",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.xiahepublishing.com/2771-165X/JCTP-2022-00031"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Androgen Drives the Expression of SARS-CoV-2 Entry Proteins in Sinonasal Tissue",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.14218/crossmark_policy",
"volume": "000"
}