Early Antiandrogen Therapy With Dutasteride Reduces Viral Shedding, Inflammatory Responses, and Time-to-Remission in Males With COVID-19: A Randomized, Double-Blind, Placebo-Controlled Interventional Trial (EAT-DUTA AndroCoV Trial – Biochemical)
et al., Cureus, doi:10.7759/cureus.13047, Feb 2021
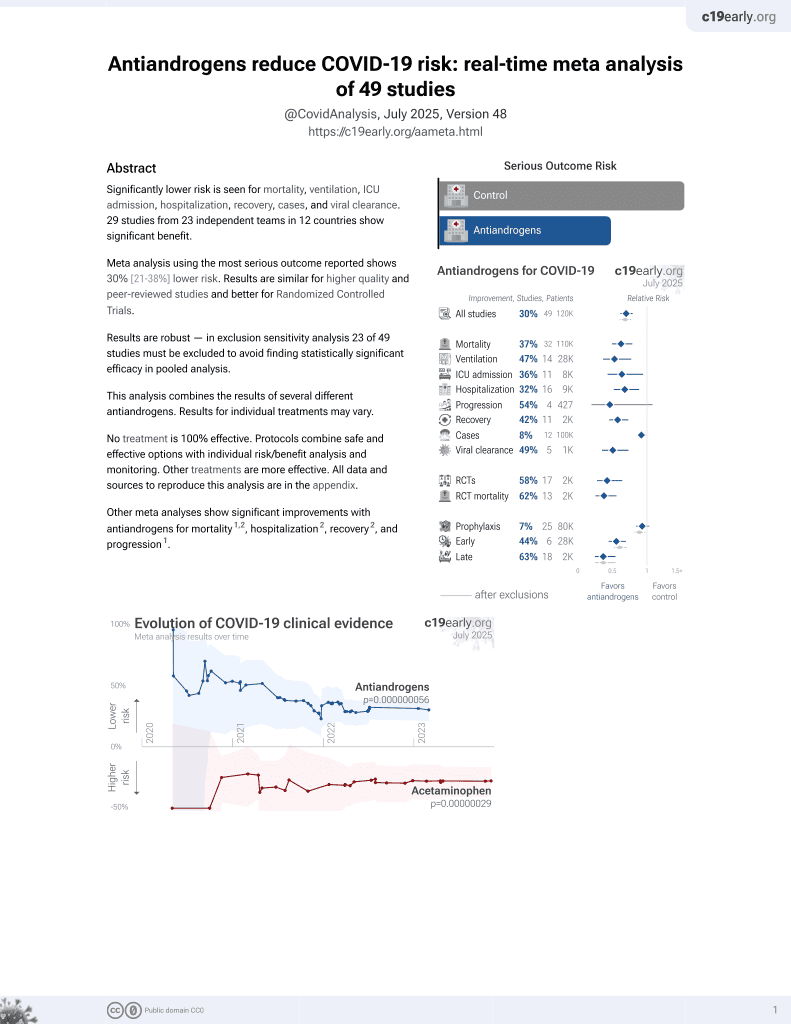
7th treatment shown to reduce risk in
September 2020, now with p = 0.000000056 from 49 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
RCT 130 outpatients in Brazil, 54 treated with dutasteride, showing faster recovery with treatment. All patients received nitazoxanide. There were no hospitalizations, mechanical ventilation, or deaths. Some percentages for viral clearance in Table 3 do not match the group sizes, and a third-party analysis suggests possible randomization failure. 34110420.2.0000.0008.
This study is excluded in the after exclusion results of meta-analysis:
potential randomization failure.
|
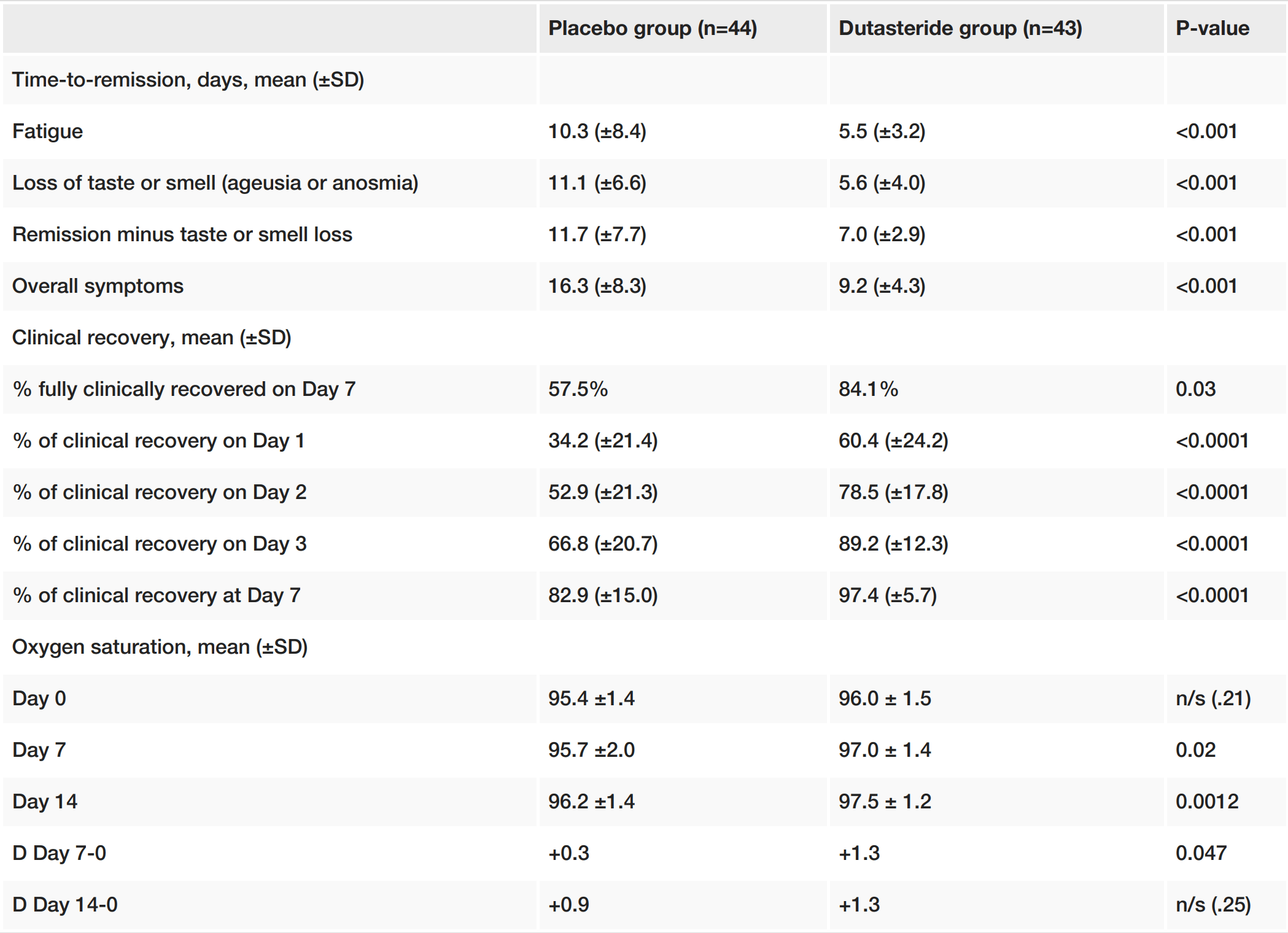
risk of no recovery, 62.0% lower, RR 0.38, p = 0.009, treatment 7 of 44 (15.9%), control 18 of 43 (41.9%), NNT 3.9.
|
|
recovery time, 43.6% lower, relative time 0.56, p < 0.001, treatment 44, control 43, all symptoms.
|
|
recovery time, 40.2% lower, relative time 0.60, p < 0.001, treatment 44, control 43, all symptoms except loss of smell or taste.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Cadegiani et al., 1 Feb 2021, Double Blind Randomized Controlled Trial, Brazil, peer-reviewed, 4 authors.
Early Antiandrogen Therapy With Dutasteride Reduces Viral Shedding, Inflammatory Responses, and Time-to-Remission in Males With COVID-19: A Randomized, Double-Blind, Placebo-Controlled Interventional Trial (EAT-DUTA AndroCoV Trial – Biochemical)
Cureus, doi:10.7759/cureus.13047
Background and objective Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) cell entry and subsequent infectivity are mediated by androgens and the androgen receptors through the regulation of transmembrane protease, serine 2 (TMPRSS2). Androgenetic alopecia (AGA) predisposes males to severe coronavirus disease 2019 (COVID-19) disease, while the use of 5-alpha-reductase inhibitors (5ARis) and androgen receptor antagonists reduce COVID-19 disease severity. In this study, we aimed to determine the potential benefit of dutasteride, a commonly used broad and potent 5ARi, as a treatment for COVID-19.
Design, setting, and participants The study was conducted at outpatient clinics. Subjects presented to the clinics with a positive reverse transcription-polymerase chain reaction (RT-PCR) test taken within 24 hours of recruitment. All subjects presented with mild to moderate symptoms.
Interventions Subjects were given either dutasteride 0.5 mg/day or placebo for 30 days or until full COVID-19 remission. All subjects received standard therapy with nitazoxanide 500 mg twice a day for six days and azithromycin 500 mg/day for five days.
Main outcome(s) and measure(s) The main outcome(s) and measure(s) were as follows: time to remission, oxygen saturation (%), positivity rates of RT-PCR-SARS-CoV-2, and biochemical analysis [ultrasensitive C-reactive protein (usCRP), D-dimer, lactate, lactate dehydrogenase (LDH), erythrocyte sedimentation rate (ESR), ultrasensitive troponin, and ferritin].
Results Subjects taking dutasteride (n=43) demonstrated reduced fatigue, anosmia, and overall disease duration compared to subjects taking a placebo (n=44) (p<.0001 for all). Compared to the placebo group, on Day seven, subjects taking dutasteride had a higher virologic remission rate (64.3% versus 11.8%; p=.0094), higher clinical recovery rate (84.7% versus 57.5%; p=.03), higher mean [standard deviation: SD] oxygen saturation (97.0% [1.4%] versus 95.7% [2.0%]; p=.02), lower median [Interquartile range: IQR] usCRP (0.34 mg/L [0.23 mg/L-0.66 mg/L] versus 1.47 mg/L [0.70 mg/L-3.37 mg/L]; p<.0001), lower median [IQR] lactate (2.01 mmol/L [1.12 mmol/L-2.43 mmol/L] versus 2.66 mmol/L [2.05 mmol/L-3.55 mmol/L]; p=.0049), lower median [IQR] ESR (5.0 mm/1h [3.0 mm/1h-11.0 mm/1h] versus 14.0 mm/1h [7.25 mm/1h-18.5 mm/1h]; p=.
Additional Information Disclosures
References
Cadegiani, Can spironolactone be used to prevent COVID-19-induced acute respiratory distress syndrome in patients with hypertension?, Am J Physiol Endocrinol Metab, doi:10.1152/ajpendo.00136.2020?utm_medium=email&utm_source=transaction
Cadegiani, Goren, Wambier, Mccoy, males with mild-to-moderate COVID-19 (The Pre-AndroCoV Male Trial), doi:10.21203/rs.3.rs-88952/v1?utm_medium=email&utm_source=transaction
Cadegiani, Goren, Wambier, Spironolactone may provide protection from SARS-CoV-2: targeting androgens, angiotensin converting enzyme 2 (ACE2), and renin-angiotensin-aldosterone system (RAAS), Med Hypotheses, doi:10.1016/j.mehy.2020.110112?utm_medium=email&utm_source=transaction
Cadegiani, Lim, Goren, Clinical symptoms of hyperandrogenic women diagnosed with COVID-19 (Epub ahead of print), J Eur Acad Dermatol Venereol, doi:10.1111/jdv.17004?utm_medium=email&utm_source=transaction
Cadegiani, Repurposing existing drugs for COVID-19: an endocrinology perspective, BMC Endocr Disord, doi:10.1186/s12902-020-00626-0?utm_medium=email&utm_source=transaction
Cadegiani, Wambier, Goren, Spironolactone: an anti-androgenic and anti-hypertensive drug that may provide protection against the novel coronavirus (SARS-CoV-2) induced acute respiratory distress syndrome (ARDS) in COVID-19, Front Med, doi:10.3389/fmed.2020.00453?utm_medium=email&utm_source=transaction
Gebhard, Regitz-Zagrosek, Neuhauser, Morgan, Klein, Impact of sex and gender on COVID-19 outcomes in Europe, Biol Sex Differ, doi:10.1186/s13293-020-00304-9?utm_medium=email&utm_source=transaction
Goren, Vaño-Galván, Wambier, A preliminary observation: male pattern hair loss among hospitalized COVID-19 patients in Spain -A potential clue to the role of androgens in COVID-19 severity, J Cosmet Dermatol, doi:10.1111/jocd.13443?utm_medium=email&utm_source=transaction
Goren, Wambier, Herrera, Anti-androgens may protect against severe COVID-19 outcomes: results from a prospective cohort study of 77 hospitalized men (Epub ahead of print), J Eur Acad Dermatol Venereol, doi:10.1111/jdv.16953?utm_medium=email&utm_source=transaction
Guan, Ni, Hu, Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med, doi:10.1056/NEJMoa2002032?utm_medium=email&utm_source=transaction
Hoffmann, Kleine-Weber, Schroeder, SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor, Cell, doi:10.1016/j.cell.2020.02.052?utm_medium=email&utm_source=transaction
Kyrou, Karteris, Robbins, Chatha, Drenos et al., Polycystic ovary syndrome (PCOS) and COVID-19: an overlooked female patient population at potentially higher risk during the COVID-19 pandemic, BMC Med, doi:10.1186/s12916-020-01697-5?utm_medium=email&utm_source=transaction
Lucas, Heinlein, Kim, The androgen-regulated protease TMPRSS2 activates a proteolytic cascade involving components of the tumor microenvironment and promotes prostate cancer metastasis, Cancer Discov, doi:10.1158/2159-8290.CD-13-1010?utm_medium=email&utm_source=transaction
Mcconnell, Wilson, George, Geller, Pappas et al., Finasteride, an inhibitor of 5 alphareductase, suppresses prostatic dihydrotestosterone in men with benign prostatic hyperplasia, J Clin Endocrinol Metab, doi:10.1210/jcem.74.3.1371291?utm_medium=email&utm_source=transaction
Mccoy, Cadegiani, Wambier, 5-alpha-reductase inhibitors are associated with reduced frequency of COVID-19 symptoms in males with androgenetic alopecia (Epub ahead of print), J Eur Acad Dermatol Venereol, doi:10.1111/jdv.17021?utm_medium=email&utm_source=transaction
Mccoy, Wambier, Herrera, Androgen receptor genetic variant predicts COVID-19 disease severity: a prospective longitudinal study of hospitalized COVID-19 male patients (Epub ahead of print), J Eur Acad Dermatol Venereol, doi:10.1111/jdv.16956?utm_medium=email&utm_source=transaction
Mccoy, Wambier, Vano-Galvan, Racial variations in COVID-19 deaths may be due to androgen receptor genetic variants associated with prostate cancer and androgenetic alopecia. Are anti-androgens a potential treatment for COVID-19?, J Cosmet Dermatol, doi:10.1111/jocd.13455?utm_medium=email&utm_source=transaction
Montopoli, Zumerle, Vettor, Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532), Ann Oncol, doi:10.1016/j.annonc.2020.04.479?utm_medium=email&utm_source=transaction
Vermeulen, Giagulli, Schepper, Buntinx, Hormonal effects of a 5 alpha-reductase inhibitor (finasteride) on hormonal levels in normal men and in patients with benign prostatic hyperplasia, Eur Urol, doi:10.1159/000471752?utm_medium=email&utm_source=transaction
Wambier, Vaño-Galván, Mccoy, Androgenetic alopecia present in the majority of patients hospitalized with COVID-19: the "Gabrin sign, J Am Acad Dermatol, doi:10.1016/j.jaad.2020.05.079?utm_medium=email&utm_source=transaction
Wambier, Vaño-Galván, Mccoy, Pai, Dhurat et al., Androgenetic alopecia in COVID-19: Compared to age-matched epidemiologic studies and hospital outcomes with or without the Gabrin sign, J Am Acad Dermatol, doi:10.1016/j.jaad.2020.07.099?utm_medium=email&utm_source=transaction
DOI record:
{
"DOI": "10.7759/cureus.13047",
"ISSN": [
"2168-8184"
],
"URL": "http://dx.doi.org/10.7759/cureus.13047",
"author": [
{
"affiliation": [],
"family": "Cadegiani",
"given": "Flavio A",
"sequence": "first"
},
{
"affiliation": [],
"family": "McCoy",
"given": "John",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gustavo Wambier",
"given": "Carlos",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Goren",
"given": "Andy",
"sequence": "additional"
}
],
"container-title": "Cureus",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
2,
1
]
],
"date-time": "2021-02-01T09:25:50Z",
"timestamp": 1612171550000
},
"deposited": {
"date-parts": [
[
2024,
2,
9
]
],
"date-time": "2024-02-09T19:29:14Z",
"timestamp": 1707506954000
},
"indexed": {
"date-parts": [
[
2024,
4,
3
]
],
"date-time": "2024-04-03T14:34:00Z",
"timestamp": 1712154840565
},
"is-referenced-by-count": 29,
"issued": {
"date-parts": [
[
2021,
2,
1
]
]
},
"language": "en",
"link": [
{
"URL": "https://www.cureus.com/articles/50511-early-antiandrogen-therapy-with-dutasteride-reduces-viral-shedding-inflammatory-responses-and-time-to-remission-in-males-with-covid-19-a-randomized-double-blind-placebo-controlled-interventional-trial-eat-duta-androcov-trial---biochemical",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.7759",
"published": {
"date-parts": [
[
2021,
2,
1
]
]
},
"published-print": {
"date-parts": [
[
2021,
2,
1
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical characteristics of coronavirus disease 2019 in China",
"author": "Guan WJ",
"doi-asserted-by": "publisher",
"journal-title": "N Engl J Med",
"key": "ref1",
"unstructured": "Guan WJ, Ni ZY, Hu Y, et al.. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020, 382:1708-1720. 10.1056/NEJMoa2002032",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1186/s13293-020-00304-9",
"article-title": "Impact of sex and gender on COVID-19 outcomes in Europe",
"author": "Gebhard C",
"doi-asserted-by": "publisher",
"journal-title": "Biol Sex Differ",
"key": "ref2",
"unstructured": "Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R, Klein SL. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ. 2020, 11:29. 10.1186/s13293-020-00304-9",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.jaad.2020.05.079",
"article-title": "Androgenetic alopecia present in the majority of patients hospitalized with COVID-19: the \"Gabrin sign\"",
"author": "Wambier CG",
"doi-asserted-by": "publisher",
"journal-title": "J Am Acad Dermatol",
"key": "ref3",
"unstructured": "Wambier CG, Vaño-Galván S, McCoy J, et al.. Androgenetic alopecia present in the majority of patients hospitalized with COVID-19: the \"Gabrin sign\". J Am Acad Dermatol. 2020, 83:680-682. 10.1016/j.jaad.2020.05.079",
"volume": "83",
"year": "2020"
},
{
"DOI": "10.1111/jocd.13443",
"article-title": "A preliminary observation: male pattern hair loss among hospitalized COVID-19 patients in Spain - A potential clue to the role of androgens in COVID-19 severity",
"author": "Goren A",
"doi-asserted-by": "publisher",
"journal-title": "J Cosmet Dermatol",
"key": "ref4",
"unstructured": "Goren A, Vaño-Galván S, Wambier CG, et al.. A preliminary observation: male pattern hair loss among hospitalized COVID-19 patients in Spain - A potential clue to the role of androgens in COVID-19 severity. J Cosmet Dermatol. 2020, 19:1545-1547. 10.1111/jocd.13443",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1016/j.jaad.2020.07.099",
"article-title": "Androgenetic alopecia in COVID-19: Compared to age-matched epidemiologic studies and hospital outcomes with or without the Gabrin sign",
"author": "Wambier CG",
"doi-asserted-by": "publisher",
"journal-title": "J Am Acad Dermatol",
"key": "ref5",
"unstructured": "Wambier CG, Vaño-Galván S, McCoy J, Pai S, Dhurat R, Goren A. Androgenetic alopecia in COVID-19: Compared to age-matched epidemiologic studies and hospital outcomes with or without the Gabrin sign. J Am Acad Dermatol. 2020, 83:e453-e454. 10.1016/j.jaad.2020.07.099",
"volume": "83",
"year": "2020"
},
{
"DOI": "10.1111/jdv.16953",
"article-title": "Anti-androgens may protect against severe COVID-19 outcomes: results from a prospective cohort study of 77 hospitalized men (Epub ahead of print)",
"author": "Goren A",
"doi-asserted-by": "publisher",
"journal-title": "J Eur Acad Dermatol Venereol",
"key": "ref6",
"unstructured": "Goren A, Wambier CG, Herrera S, et al.. Anti-androgens may protect against severe COVID-19 outcomes: results from a prospective cohort study of 77 hospitalized men (Epub ahead of print). J Eur Acad Dermatol Venereol. 2020, 10.1111/jdv.16953",
"year": "2020"
},
{
"DOI": "10.1111/jdv.17021",
"article-title": "5-alpha-reductase inhibitors are associated with reduced frequency of COVID-19 symptoms in males with androgenetic alopecia (Epub ahead of print)",
"author": "McCoy J",
"doi-asserted-by": "publisher",
"journal-title": "J Eur Acad Dermatol Venereol",
"key": "ref7",
"unstructured": "McCoy J, Cadegiani FA, Wambier CG, et al.. 5-alpha-reductase inhibitors are associated with reduced frequency of COVID-19 symptoms in males with androgenetic alopecia (Epub ahead of print). J Eur Acad Dermatol Venereol. 2020, 10.1111/jdv.17021",
"year": "2020"
},
{
"DOI": "10.1016/j.annonc.2020.04.479",
"article-title": "Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532)",
"author": "Montopoli M",
"doi-asserted-by": "publisher",
"journal-title": "Ann Oncol",
"key": "ref8",
"unstructured": "Montopoli M, Zumerle S, Vettor R, et al.. Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532). Ann Oncol. 2020, 31:1040-1045. 10.1016/j.annonc.2020.04.479",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor",
"author": "Hoffmann M",
"doi-asserted-by": "publisher",
"journal-title": "Cell",
"key": "ref9",
"unstructured": "Hoffmann M, Kleine-Weber H, Schroeder S, et al.. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020, 181:271-280. 10.1016/j.cell.2020.02.052",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1158/2159-8290.CD-13-1010",
"article-title": "The androgen-regulated protease TMPRSS2 activates a proteolytic cascade involving components of the tumor microenvironment and promotes prostate cancer metastasis",
"author": "Lucas JM",
"doi-asserted-by": "publisher",
"journal-title": "Cancer Discov",
"key": "ref10",
"unstructured": "Lucas JM, Heinlein C, Kim T, et al.. The androgen-regulated protease TMPRSS2 activates a proteolytic cascade involving components of the tumor microenvironment and promotes prostate cancer metastasis. Cancer Discov. 2014, 4:1310-1325. 10.1158/2159-8290.CD-13-1010",
"volume": "4",
"year": "2014"
},
{
"DOI": "10.1186/s12916-020-01697-5",
"article-title": "Polycystic ovary syndrome (PCOS) and COVID-19: an overlooked female patient population at potentially higher risk during the COVID-19 pandemic",
"author": "Kyrou I",
"doi-asserted-by": "publisher",
"journal-title": "BMC Med",
"key": "ref11",
"unstructured": "Kyrou I, Karteris E, Robbins T, Chatha K, Drenos F, Randeva HS. Polycystic ovary syndrome (PCOS) and COVID-19: an overlooked female patient population at potentially higher risk during the COVID-19 pandemic. BMC Med. 2020, 18:220. 10.1186/s12916-020-01697-5",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1111/jdv.17004",
"article-title": "Clinical symptoms of hyperandrogenic women diagnosed with COVID-19 (Epub ahead of print)",
"author": "Cadegiani FA",
"doi-asserted-by": "publisher",
"journal-title": "J Eur Acad Dermatol Venereol",
"key": "ref12",
"unstructured": "Cadegiani FA, Lim RK, Goren A, et al.. Clinical symptoms of hyperandrogenic women diagnosed with COVID-19 (Epub ahead of print). J Eur Acad Dermatol Venereol. 2020, 10.1111/jdv.17004",
"year": "2020"
},
{
"DOI": "10.1111/jocd.13455",
"article-title": "Racial variations in COVID-19 deaths may be due to androgen receptor genetic variants associated with prostate cancer and androgenetic alopecia. Are anti-androgens a potential treatment for COVID-19?",
"author": "McCoy J",
"doi-asserted-by": "publisher",
"journal-title": "J Cosmet Dermatol",
"key": "ref13",
"unstructured": "McCoy J, Wambier CG, Vano-Galvan S, et al.. Racial variations in COVID-19 deaths may be due to androgen receptor genetic variants associated with prostate cancer and androgenetic alopecia. Are anti-androgens a potential treatment for COVID-19?. J Cosmet Dermatol. 2020, 19:1542-1543. 10.1111/jocd.13455",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1186/s12902-020-00626-0",
"article-title": "Repurposing existing drugs for COVID-19: an endocrinology perspective",
"author": "Cadegiani FA",
"doi-asserted-by": "publisher",
"journal-title": "BMC Endocr Disord",
"key": "ref14",
"unstructured": "Cadegiani FA. Repurposing existing drugs for COVID-19: an endocrinology perspective. BMC Endocr Disord. 2020, 20:149. 10.1186/s12902-020-00626-0",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.3389/fmed.2020.00453",
"article-title": "Spironolactone: an anti-androgenic and anti-hypertensive drug that may provide protection against the novel coronavirus (SARS-CoV-2) induced acute respiratory distress syndrome (ARDS) in COVID-19",
"author": "Cadegiani FA",
"doi-asserted-by": "publisher",
"journal-title": "Front Med (Lausanne)",
"key": "ref15",
"unstructured": "Cadegiani FA, Wambier CG, Goren A. Spironolactone: an anti-androgenic and anti-hypertensive drug that may provide protection against the novel coronavirus (SARS-CoV-2) induced acute respiratory distress syndrome (ARDS) in COVID-19. Front Med (Lausanne). 2020, 7:453. 10.3389/fmed.2020.00453",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.mehy.2020.110112",
"article-title": "Spironolactone may provide protection from SARS-CoV-2: targeting androgens, angiotensin converting enzyme 2 (ACE2), and renin-angiotensin-aldosterone system (RAAS)",
"author": "Cadegiani FA",
"doi-asserted-by": "publisher",
"journal-title": "Med Hypotheses",
"key": "ref16",
"unstructured": "Cadegiani FA, Goren A, Wambier CG. Spironolactone may provide protection from SARS-CoV-2: targeting androgens, angiotensin converting enzyme 2 (ACE2), and renin-angiotensin-aldosterone system (RAAS). Med Hypotheses. 2020, 143:110112. 10.1016/j.mehy.2020.110112",
"volume": "143",
"year": "2020"
},
{
"DOI": "10.1152/ajpendo.00136.2020",
"article-title": "Can spironolactone be used to prevent COVID-19-induced acute respiratory distress syndrome in patients with hypertension?",
"author": "Cadegiani FA",
"doi-asserted-by": "publisher",
"journal-title": "Am J Physiol Endocrinol Metab",
"key": "ref17",
"unstructured": "Cadegiani FA. Can spironolactone be used to prevent COVID-19-induced acute respiratory distress syndrome in patients with hypertension?. Am J Physiol Endocrinol Metab. 2020, 318:E587-E588. 10.1152/ajpendo.00136.2020",
"volume": "318",
"year": "2020"
},
{
"DOI": "10.1111/jdv.16956",
"article-title": "Androgen receptor genetic variant predicts COVID-19 disease severity: a prospective longitudinal study of hospitalized COVID-19 male patients (Epub ahead of print)",
"author": "McCoy J",
"doi-asserted-by": "publisher",
"journal-title": "J Eur Acad Dermatol Venereol",
"key": "ref18",
"unstructured": "McCoy J, Wambier CG, Herrera S, et al.. Androgen receptor genetic variant predicts COVID-19 disease severity: a prospective longitudinal study of hospitalized COVID-19 male patients (Epub ahead of print). J Eur Acad Dermatol Venereol. 2020, 10.1111/jdv.16956",
"year": "2020"
},
{
"DOI": "10.1159/000471752",
"article-title": "Hormonal effects of a 5 alpha-reductase inhibitor (finasteride) on hormonal levels in normal men and in patients with benign prostatic hyperplasia",
"author": "Vermeulen A",
"doi-asserted-by": "publisher",
"journal-title": "Eur Urol",
"key": "ref19",
"unstructured": "Vermeulen A, Giagulli VA, De Schepper P, Buntinx A. Hormonal effects of a 5 alpha-reductase inhibitor (finasteride) on hormonal levels in normal men and in patients with benign prostatic hyperplasia. Eur Urol. 1991, 20:82-86. 10.1159/000471752",
"volume": "20",
"year": "1991"
},
{
"DOI": "10.1210/jcem.74.3.1371291",
"article-title": "Finasteride, an inhibitor of 5 alpha-reductase, suppresses prostatic dihydrotestosterone in men with benign prostatic hyperplasia",
"author": "McConnell JD",
"doi-asserted-by": "publisher",
"journal-title": "J Clin Endocrinol Metab",
"key": "ref20",
"unstructured": "McConnell JD, Wilson JD, George FW, Geller J, Pappas F, Stoner E. Finasteride, an inhibitor of 5 alpha-reductase, suppresses prostatic dihydrotestosterone in men with benign prostatic hyperplasia. J Clin Endocrinol Metab. 1992, 74:505-508. 10.1210/jcem.74.3.1371291",
"volume": "74",
"year": "1992"
},
{
"DOI": "10.21203/rs.3.rs-88952/v1",
"article-title": "Azithromycin with nitazoxanide, hydroxychloroquine or ivermectin, with or without dutasteride, for early stage COVID-19: an open-label prospective observational study in males with mild-to-moderate COVID-19 (The Pre-AndroCoV Male Trial) [PREPRINT]",
"author": "Cadegiani FA",
"doi-asserted-by": "publisher",
"journal-title": "Res Sq",
"key": "ref21",
"unstructured": "Cadegiani FA, Goren A, Wambier CG, McCoy J. Azithromycin with nitazoxanide, hydroxychloroquine or ivermectin, with or without dutasteride, for early stage COVID-19: an open-label prospective observational study in males with mild-to-moderate COVID-19 (The Pre-AndroCoV Male Trial) [PREPRINT]. Res Sq. 2020, 10.21203/rs.3.rs-88952/v1",
"year": "2020"
}
],
"reference-count": 21,
"references-count": 21,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.cureus.com/articles/50511-early-antiandrogen-therapy-with-dutasteride-reduces-viral-shedding-inflammatory-responses-and-time-to-remission-in-males-with-covid-19-a-randomized-double-blind-placebo-controlled-interventional-trial-eat-duta-androcov-trial---biochemical"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Aerospace Engineering"
],
"subtitle": [],
"title": "Early Antiandrogen Therapy With Dutasteride Reduces Viral Shedding, Inflammatory Responses, and Time-to-Remission in Males With COVID-19: A Randomized, Double-Blind, Placebo-Controlled Interventional Trial (EAT-DUTA AndroCoV Trial – Biochemical)",
"type": "journal-article"
}