The Association of Weight Reduction and Other Variables after Bariatric Surgery with the Likelihood of SARS-CoV-2 Infection
et al., Journal of Clinical Medicine, doi:10.3390/jcm12124054, Jun 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
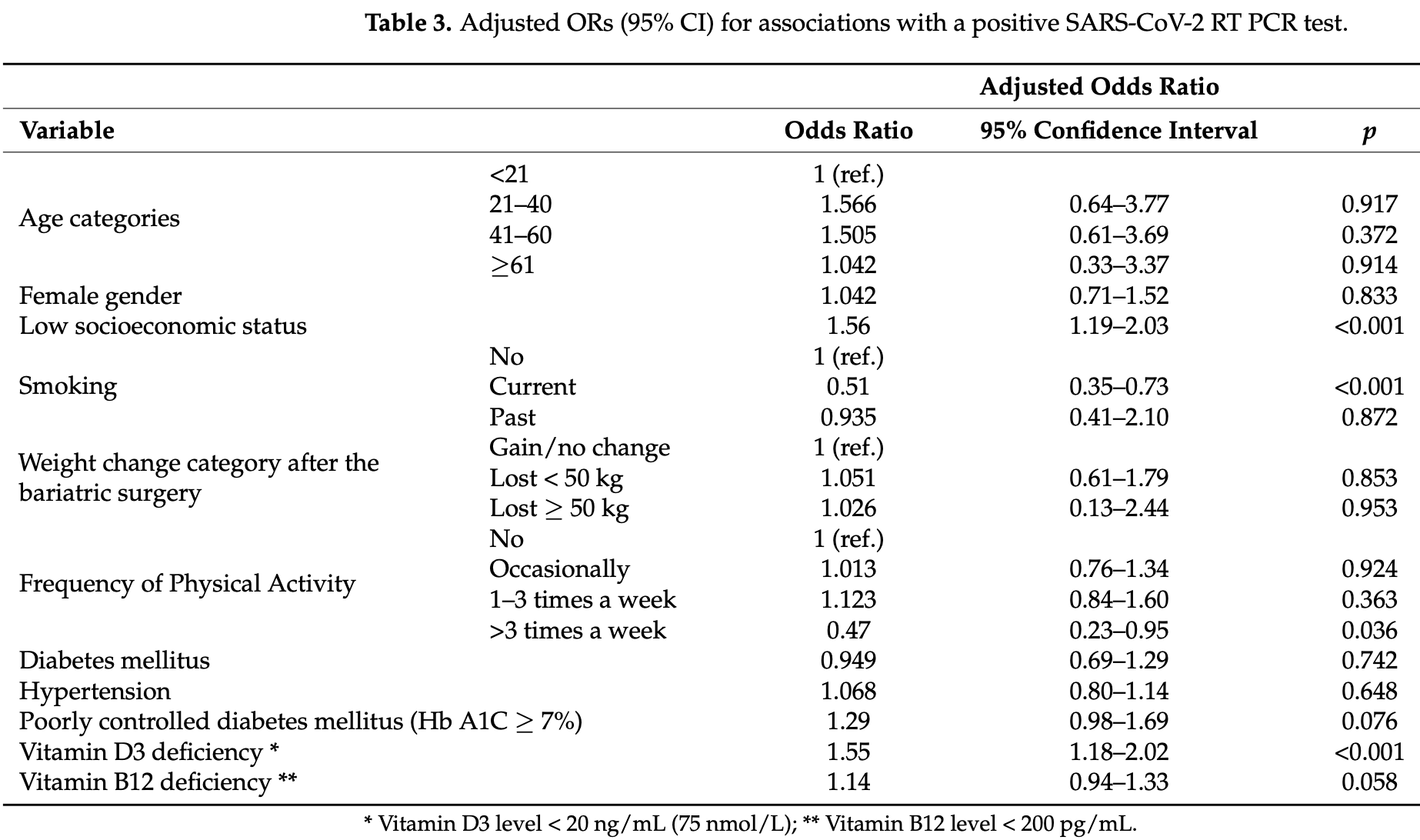
Retrospective 3,038 bariatric surgery patients in Israel, showing higher risk of SARS-CoV-2 infection with vitamin D deficiency, and lower risk with physical activity.
This is the 183rd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Study covers exercise and vitamin D.
|
risk of case, 35.5% lower, OR 0.65, p = 0.001, cutoff 20ng/mL, adjusted per study, inverted to make OR<1 favor high D levels (≥20ng/mL), multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Frish et al., 15 Jun 2023, retrospective, Israel, peer-reviewed, 7 authors, study period 1 February, 2020 - 31 December, 2020.
Contact: emarzon@leumit.co.il (corresponding author), noamfrish12@gmail.com, shaias@ariel.ac.il, aisrael@leumit.co.il, svinker@leumit.co.il, igreen@leumit.co.il, agolanchoen@leumit.co.il.
The Association of Weight Reduction and Other Variables after Bariatric Surgery with the Likelihood of SARS-CoV-2 Infection
Journal of Clinical Medicine, doi:10.3390/jcm12124054
Background and aims: Although obesity has been confirmed as a risk factor for SARS-CoV-2 infection and its severity, the role of post-bariatric surgery (BS) variables and the infection is unclear. We, therefore, aimed to study comprehensively the relationship between the extent of weight reduction after surgery and other demographic, clinical, and laboratory variables with the rates of SARS-CoV-2 infection. Methods: A population-based cross-sectional study was performed, utilizing advanced tracking methodologies on the computerized database of a nation-wide health maintenance organization (HMO). The study population included all HMO members aged ≥18 years that had been tested at least once for SARS-CoV-2 during the study period and underwent BS at least one year before their testing. Results: Of the total 3038 individuals who underwent BS, 2697 (88.78%) were positive for SARS-CoV-2 infection and 341 (11.22%) were negative. Multivariate regression analysis demonstrated that the body mass index and the amount of weight reduction after the BS were not related to the likelihood of SARS-CoV-2 infection. Post-operative low socioeconomic status (SES) and vitamin D3 deficiency were associated with significant and independent increased rates of SARS-CoV-2 infection (odds ratio [OR] 1.56, 95% confidence interval [CI], 1.19-2.03, p < 0.001; and OR 1.55, 95% CI, 1.18-2.02, p < 0.001; respectively). Post-operative physical activity > 3 times/week was associated with a significant and independent reduced rate of SARS-CoV-2 infection (OR 0.51, 95% CI, 0.35-0.73, p < 0.001). Conclusion: Post-BS vitamin D3 deficiency, SES, and physical activity, but not the amount of weight reduction, were significantly associated with the rates of SARS-CoV-2 infection. Healthcare workers should be aware of these associations after BS and intervene accordingly.
Conflicts of Interest: The authors declare no conflict of interest.
References
Adams, Katz, Grandpre, Population-Based Estimates of Chronic Conditions Affecting Risk for Complications from Coronavirus Disease, United States. Emerg, doi:10.3201/eid2608.200679
Annamaria, Domenico, Anna, Santina, Carmela et al., Contribution of vitamin D3 and thiols status to the outcome of COVID-19 disease in Italian pediatric and adult patients, Sci, doi:10.1038/s41598-023-29519-7
Birkmeyer, Barnato, Birkmeyer, Bessler, Skinner, The Impact of The COVID-19 Pandemic On Hospital Admissions In The United States. Health Aff, doi:10.1377/hlthaff.2020.00980
Blanchard, Perennec, Smati, Tramunt, Guyomarch et al., History of bariatric surgery and COVID-19 outcomes in patients with type 2 diabetes: Results from the CORONADO study, Obesity, doi:10.1002/oby.23314
Briguglio, Pregliasco, Lombardi, Perazzo, Banfi, The Malnutritional Status of the Host as a Virulence Factor for New Coronavirus SARS-CoV-2, doi:10.3389/fmed.2020.00146
Caci, Albini, Malerba, Noonan, Pochetti et al., COVID-19 and Obesity: Dangerous Liaisons, J. Clin. Med, doi:10.3390/jcm9082511
Chakhtoura, Rahme, El-Hajj Fuleihan, Vitamin D Metabolism in Bariatric Surgery, Endocrinol. Metab. Clin. N. Am, doi:10.1016/j.ecl.2017.07.006
Chang, Stoll, Song, Varela, Eagon et al., The effectiveness and risks of bariatric surgery: An updated systematic review and meta-analysis, JAMA Surg, doi:10.1001/jamasurg.2013.3654
Colombi, Bodini, Petrini, Maffi, Morelli et al., Well-aerated lung on admitting chest CT to predict adverse outcome in COVID-19 Pneumonia, Radiology, doi:10.1148/radiol.2020201433
Ellulu, Khaza'ai, Rahmat, Patimah, Abed, Obesity can predict and promote systemic inflammation in healthy adults, Int. J. Cardiol, doi:10.1016/j.ijcard.2016.04.089
Ellulu, Patimah, Khaza'ai, Rahmat, Abed, Obesity and inflammation: The linking mechanism and the complications, Arch. Med. Sci, doi:10.5114/aoms.2016.58928
Eroume, Egom, Shiwani, Nouthe, From acute SARS-CoV-2 infection to pulmonary hypertension, Front. Physiol, doi:10.3389/fphys.2022.1023758
Gonzalez-Rubio, Navarro-Lopez, Lopez-Najera, Lopez-Najera, Jimenez-Diaz et al., Cytokine release syndrome (CRS) and nicotine in COVID-19 patients: Trying to calm the storm, Front. Immunol, doi:10.3389/fimmu.2020.01359
Green, Merzon, Vinker, Golan-Cohen, Israel et al., A higher frequency of physical activity is associated with reduced rates of SARS-CoV-2 infection, Eur. J. Gen, doi:10.1080/13814788.2022.2138855
Green, Merzon, Vinker, Golan-Cohen, Magen, COVID-19 Susceptibility in Bronchial Asthma, J. Allergy Clin. Immunol. Pract, doi:10.1016/j.jaip.2020.11.020
Gregory, Slaughter, Duffus, Smith, Lestourgeon et al., COVID-19 Severity Is Tripled in the Diabetes Community: A Prospective Analysis of the Pandemic's Impact in Type 1 and Type 2 Diabetes, Diabetes Care, doi:10.2337/dc20-2260
Huang, Lu, Huang, Wang, Ling et al., Obesity in Patients with COVID-19: A Systematic Review and Meta-Analysis, Metabolism, doi:10.1016/j.metabol.2020.154378
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, Lancet, doi:10.1016/S0140-6736(20)30183-5
Hussain, Mahawar, Xia, Yang, El-Hasani, Obesity and mortality of COVID-19. Meta-analysis, Obes. Res. Clin. Pract, doi:10.1016/j.orcp.2020.07.002
Israel, Cicurel, Feldhamer, Stern, Dror et al., Vitamin D deficiency is associated with higher risks for SARS-CoV-2 infection and COVID-19 severity: A retrospective case-control study, Intern. Emerg. Med, doi:10.1007/s11739-021-02902-w
Israel, Felhamer, Lahad, Levin-Zamit, Lavie, Smoking and the risk of COVID-19 in a large observational population study, MedRxiv, doi:10.1101/2020.06.01.20118877
Jackson, Brown, Shahab, Steptoe, Fancourt, COVID-19, Smoking and Inequalities: A Study of 53 002 Adults in the UK. Tobacco Control, doi:10.1136/tobaccocontrol-2020-055933
Jammah, Endocrine and metabolic complications after bariatric surgery, Saudi J. Gastroenterol, doi:10.4103/1319-3767.164183
Lespessailles, Toumi, Vitamin D alteration associated with obesity and bariatric surgery, Exp. Biol. Med, doi:10.1177/1535370216688567
Liu, Cao, Du, Zhi, Prevalence of Comorbid Asthma and Related Outcomes in COVID-19: A Systematic Review and Meta-Analysis, J. Allergy Clin. Immunol. Pract, doi:10.1016/j.jaip.2020.11.054
Lopez-Picazo, Vidal-Abarca, Beteta, López-Ibáñez, García-Vázquez, Impact of the COVID-19 Pandemic on the Hospital: Inpatient's Perceived Quality in Spain, J. Patient Exp, doi:10.1177/2374373521998625
Ludvigsson, Systematic Review of COVID-19 in Children Shows Milder Cases and a Better Prognosis than Adults, Acta Paediatr, doi:10.1111/apa.15270
Marchesi, Valente, Riccò, Rottoli, Baldini et al., Effects of Bariatric Surgery on COVID-19: A Multicentric Study from a High Incidence Area, Obes. Surg
Mcgrath, Mcdonald, Macdonald, Transdermal nictoine for induction of remission in ulcerative colitis, Cochrane Database Syst. Rev
Merzon, Green, Shpigelman, Vinker, Raz et al., Haemoglobin A1c is a predictor of COVID-19 severity in patients with diabetes, Diabetes Metab. Res. Rev, doi:10.1002/dmrr.3398
Merzon, Tworowski, Gorohovski, Vinker, Golan Cohen et al., Low Plasma 25(OH) Vitamin D Level Is Associated with Increased Risk of COVID-19 Infection: An Israeli Population-Based Study, FEBS J, doi:10.1111/febs.15495
Merzon, Weiss, Cortese, Rotem, Schneider et al., The Association between ADHD and the Severity of COVID-19 Infection, J. Atten. Disord, doi:10.1177/10870547211003659
Merzon, Weiss, Krone, Cohen, Ilani et al., Clinical and Socio-Demographic Variables Associated with the Diagnosis of Long COVID Syndrome in Youth: A Population-Based Study, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19105993
Montini, Nozzolillo, Rancoita, Zanetta, Moiola et al., Modifiable risk factors of COVID-19 in patients with multiple sclerosis: A single-centre case-control study, J. Neurol, doi:10.1007/s00415-023-11618-0
Moradpour, Amini, Moeinvaziri, Hosseini, Rajabi et al., Bariatric Surgery and COVID-19: What We Have Learned from the Pandemic in Iran: A Retrospective Study, Obes. Surg
Msemburi, Karlinsky, Knutson, Aleshin-Guendel, Chatterji et al., The WHO Estimates of excess mortality associated with the COVID-19 pandemic, Nature, doi:10.1038/s41586-022-05522-2
Mukherjee, Gorohovski, Merzon, Levy, Mukherjee et al., Seasonal UV exposure and vitamin D: Association with the dynamics of COVID-19 transmission in Europe, FEBS Open Bio, doi:10.1002/2211-5463.13309
Nakeshbandi, Maini, Daniel, Rosengarten, Parmar et al., The impact of obesity on COVID-19 complications: A retrospective cohort study, Int. J. Obes
Núñez-Cortés, López-Bueno, Torres-Castro, Soto-Carmona, Ortega-Palavecinos et al., Risk Factors for One-Year Mortality in Hospitalized Adults with Severe COVID-19, Aging Dis, doi:10.14336/AD.2022.0424
Palaiodimos, Kokkinidis, Li, Karamanis, Ognibene et al., Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, Metabolism, doi:10.1016/j.metabol.2020.154262
Pescariu, Tudoran, Pop, Pescariu, Timar et al., Impact of COVID-19 Pandemic on the Implantation of Intra-Cardiac Devices in Diabetic and Non-Diabetic Patients in the Western of Romania, Medicina, doi:10.3390/medicina57050441
Sagie, Na'amnih, Frej, Cohen, Alpert et al., Correlates of Hospitalizations in Internal Medicine Divisions among Israeli Adults of Different Ethnic Groups with Hypertension, Diabetes and Cardiovascular Diseases, PLoS ONE, doi:10.1371/journal.pone.0215639
Sallis, Young, Tartof, Sallis, Sall et al., Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients, Br. J. Sports Med, doi:10.1136/bjsports-2021-104080
Santa-Cruz, Siqueira, Coutinho, Leão, Almeida et al., Is COVID-19 Severity Impacted by Bariatric Surgery in the Early Postoperative Period?, Obes. Surg, doi:10.1007/s11695-022-05915-2
Seligman, Ferranna, Bloom, Social Determinants of Mortality from COVID-19: A Simulation Study Using NHANES, PLoS Med, doi:10.1371/journal.pmed.1003490
Shapiro, Yavne, Shepshelovich, Predicting Which Patients Are at Risk for Clinical Deterioration in COVID-19: A Review of the Current Models in Use, Isr. Med. Assoc. J. (IMAJ)
Tajlil, Ghaffari, Pourafkari, Mashayekhi, Roshanravan, Nicotine and smoking in the COVID-19 era, J. Cardiovasc. Thorac. Res, doi:10.34172/jcvtr.2020.22
Thomas, Rhodes, Ingram, Mechanism of disease: Nicotine-a review of its actions in the context of gastrointestinal disease, Nat. Clin. Pract, doi:10.1038/ncpgasthep0316
Treskova-Schwarzbach, Haas, Reda, Pilic, Borodova et al., Pre-Existing Health Conditions and Severe COVID-19 Outcomes: An Umbrella Review Approach and Meta-Analysis of Global Evidence, BMC Med, doi:10.1186/s12916-021-02058-6
Tripathi, Mishra, A review article on neuroprotective, immunomodulatory, and anti-inflammatory role of vitamin-D3 in elderly COVID-19 patients, Egypt J. Neurol. Psychiatr. Neurosurg, doi:10.1186/s41983-023-00611-z
Tudoran, Tudoran, Lazureanu, Marinescu, Cut et al., Factors Influencing the Evolution of Pulmonary Hypertension in Previously Healthy Subjects Recovering from a SARS-CoV-2 Infection, J. Clin. Med, doi:10.3390/jcm10225272
Tudoran, Tudoran, Lazureanu, Marinescu, Pop et al., Evidence of Pulmonary Hypertension after SARS-CoV-2 Infection in Subjects without Previous Significant Cardiovascular Pathology, J. Clin. Med, doi:10.3390/jcm10020199
Verity, Okell, Dorigatti, Winskill, Whittaker et al., Estimates of the severity of Coronavirus Disease 2019: A model-based analysis, Lancet Infect. Dis
Wolfe, Kvach, Eckel, Treatment of Obesity: Weight Loss and Bariatric Surgery, Circ. Res, doi:10.1161/CIRCRESAHA.116.307591
Young, Sallis, Baecker, Cohen, Nau et al., Associations of Physical Inactivity and COVID-19 Outcomes Among Subgroups, Am. J. Prev. Med, doi:10.1016/j.amepre.2022.10.007
DOI record:
{
"DOI": "10.3390/jcm12124054",
"ISSN": [
"2077-0383"
],
"URL": "http://dx.doi.org/10.3390/jcm12124054",
"abstract": "<jats:p>Background and aims: Although obesity has been confirmed as a risk factor for SARS-CoV-2 infection and its severity, the role of post-bariatric surgery (BS) variables and the infection is unclear. We, therefore, aimed to study comprehensively the relationship between the extent of weight reduction after surgery and other demographic, clinical, and laboratory variables with the rates of SARS-CoV-2 infection. Methods: A population-based cross-sectional study was performed, utilizing advanced tracking methodologies on the computerized database of a nation-wide health maintenance organization (HMO). The study population included all HMO members aged ≥18 years that had been tested at least once for SARS-CoV-2 during the study period and underwent BS at least one year before their testing. Results: Of the total 3038 individuals who underwent BS, 2697 (88.78%) were positive for SARS-CoV-2 infection and 341 (11.22%) were negative. Multivariate regression analysis demonstrated that the body mass index and the amount of weight reduction after the BS were not related to the likelihood of SARS-CoV-2 infection. Post-operative low socioeconomic status (SES) and vitamin D3 deficiency were associated with significant and independent increased rates of SARS-CoV-2 infection (odds ratio [OR] 1.56, 95% confidence interval [CI], 1.19–2.03, p < 0.001; and OR 1.55, 95% CI, 1.18–2.02, p < 0.001; respectively). Post-operative physical activity > 3 times/week was associated with a significant and independent reduced rate of SARS-CoV-2 infection (OR 0.51, 95% CI, 0.35–0.73, p < 0.001). Conclusion: Post-BS vitamin D3 deficiency, SES, and physical activity, but not the amount of weight reduction, were significantly associated with the rates of SARS-CoV-2 infection. Healthcare workers should be aware of these associations after BS and intervene accordingly.</jats:p>",
"alternative-id": [
"jcm12124054"
],
"author": [
{
"affiliation": [
{
"name": "Adelson School of Medicine, Ariel University, Ariel 40700, Israel"
}
],
"family": "Frish",
"given": "Noam",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-4389-8896",
"affiliation": [
{
"name": "Leumit Health Services, Tel Aviv 64738, Israel"
},
{
"name": "Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv 69978, Israel"
}
],
"authenticated-orcid": false,
"family": "Israel",
"given": "Ariel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7244-0679",
"affiliation": [
{
"name": "Adelson School of Medicine, Ariel University, Ariel 40700, Israel"
}
],
"authenticated-orcid": false,
"family": "Ashkenazi",
"given": "Shai",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Leumit Health Services, Tel Aviv 64738, Israel"
},
{
"name": "Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv 69978, Israel"
}
],
"family": "Vinker",
"given": "Shlomo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9435-7152",
"affiliation": [
{
"name": "Leumit Health Services, Tel Aviv 64738, Israel"
},
{
"name": "Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv 69978, Israel"
}
],
"authenticated-orcid": false,
"family": "Green",
"given": "Ilan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Leumit Health Services, Tel Aviv 64738, Israel"
},
{
"name": "Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv 69978, Israel"
}
],
"family": "Golan-Cohen",
"given": "Avivit",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5469-0236",
"affiliation": [
{
"name": "Adelson School of Medicine, Ariel University, Ariel 40700, Israel"
},
{
"name": "Leumit Health Services, Tel Aviv 64738, Israel"
}
],
"authenticated-orcid": false,
"family": "Merzon",
"given": "Eugene",
"sequence": "additional"
}
],
"container-title": "Journal of Clinical Medicine",
"container-title-short": "JCM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
6,
15
]
],
"date-time": "2023-06-15T06:03:19Z",
"timestamp": 1686808999000
},
"deposited": {
"date-parts": [
[
2023,
6,
15
]
],
"date-time": "2023-06-15T08:02:42Z",
"timestamp": 1686816162000
},
"indexed": {
"date-parts": [
[
2023,
6,
16
]
],
"date-time": "2023-06-16T04:12:57Z",
"timestamp": 1686888777651
},
"is-referenced-by-count": 0,
"issue": "12",
"issued": {
"date-parts": [
[
2023,
6,
15
]
]
},
"journal-issue": {
"issue": "12",
"published-online": {
"date-parts": [
[
2023,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
6,
15
]
],
"date-time": "2023-06-15T00:00:00Z",
"timestamp": 1686787200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2077-0383/12/12/4054/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "4054",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
6,
15
]
]
},
"published-online": {
"date-parts": [
[
2023,
6,
15
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref_1",
"unstructured": "World Health Organization (2023, March 03). WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/."
},
{
"DOI": "10.1038/s41586-022-05522-2",
"article-title": "The WHO Estimates of excess mortality associated with the COVID-19 pandemic",
"author": "Msemburi",
"doi-asserted-by": "crossref",
"first-page": "130",
"journal-title": "Nature",
"key": "ref_2",
"volume": "613",
"year": "2023"
},
{
"DOI": "10.1111/apa.15270",
"article-title": "Systematic Review of COVID-19 in Children Shows Milder Cases and a Better Prognosis than Adults",
"author": "Ludvigsson",
"doi-asserted-by": "crossref",
"first-page": "1088",
"journal-title": "Acta Paediatr.",
"key": "ref_3",
"volume": "109",
"year": "2020"
},
{
"DOI": "10.1016/S1473-3099(20)30243-7",
"article-title": "Estimates of the severity of Coronavirus Disease 2019: A model-based analysis",
"author": "Verity",
"doi-asserted-by": "crossref",
"first-page": "669",
"journal-title": "Lancet Infect. Dis.",
"key": "ref_4",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.3390/medicina57050441",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "Pescariu, S.A., Tudoran, C., Pop, G.N., Pescariu, S., Timar, R.Z., and Tudoran, M. (2021). Impact of COVID-19 Pandemic on the Implantation of Intra-Cardiac Devices in Diabetic and Non-Diabetic Patients in the Western of Romania. Medicina, 57."
},
{
"article-title": "Impact of the COVID-19 Pandemic on the Hospital: Inpatient’s Perceived Quality in Spain",
"author": "Beteta",
"first-page": "2374373521998625",
"journal-title": "J. Patient Exp.",
"key": "ref_6",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1377/hlthaff.2020.00980",
"article-title": "The Impact of The COVID-19 Pandemic On Hospital Admissions In The United States",
"author": "Birkmeyer",
"doi-asserted-by": "crossref",
"first-page": "2010",
"journal-title": "Health Aff.",
"key": "ref_7",
"volume": "39",
"year": "2020"
},
{
"article-title": "Predicting Which Patients Are at Risk for Clinical Deterioration in COVID-19: A Review of the Current Models in Use",
"author": "Shapiro",
"first-page": "699",
"journal-title": "Isr. Med. Assoc. J. (IMAJ)",
"key": "ref_8",
"volume": "24",
"year": "2022"
},
{
"DOI": "10.3390/ijerph19105993",
"doi-asserted-by": "crossref",
"key": "ref_9",
"unstructured": "Merzon, E., Weiss, M., Krone, B., Cohen, S., Ilani, G., Vinker, S., Cohen-Golan, A., Green, I., Israel, A., and Schneider, T. (2022). Clinical and Socio-Demographic Variables Associated with the Diagnosis of Long COVID Syndrome in Youth: A Population-Based Study. Int. J. Environ. Res. Public Health, 19."
},
{
"DOI": "10.1371/journal.pmed.1003888",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Seligman, B., Ferranna, M., and Bloom, D.E. (2021). Social Determinants of Mortality from COVID-19: A Simulation Study Using NHANES. PLoS Med., 18."
},
{
"DOI": "10.1016/j.metabol.2020.154378",
"article-title": "Obesity in Patients with COVID-19: A Systematic Review and Meta-Analysis",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "154378",
"journal-title": "Metabolism",
"key": "ref_11",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.1136/tobaccocontrol-2020-055933",
"article-title": "COVID-19, Smoking and Inequalities: A Study of 53 002 Adults in the UK",
"author": "Jackson",
"doi-asserted-by": "crossref",
"first-page": "e111",
"journal-title": "Tobacco Control",
"key": "ref_12",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1111/febs.15495",
"article-title": "Low Plasma 25(OH) Vitamin D Level Is Associated with Increased Risk of COVID-19 Infection: An Israeli Population—Based Study",
"author": "Merzon",
"doi-asserted-by": "crossref",
"first-page": "3693",
"journal-title": "FEBS J.",
"key": "ref_13",
"volume": "287",
"year": "2020"
},
{
"DOI": "10.1186/s12916-021-02058-6",
"doi-asserted-by": "crossref",
"key": "ref_14",
"unstructured": "Treskova-Schwarzbach, M., Haas, L., Reda, S., Pilic, A., Borodova, A., Karimi, K., Koch, J., Nygren, T., Scholz, S., and Schönfeld, V. (2021). Pre-Existing Health Conditions and Severe COVID-19 Outcomes: An Umbrella Review Approach and Meta-Analysis of Global Evidence. BMC Med., 19."
},
{
"DOI": "10.1016/j.jaip.2020.11.054",
"article-title": "Prevalence of Comorbid Asthma and Related Outcomes in COVID-19: A Systematic Review and Meta-Analysis",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "693",
"journal-title": "J. Allergy Clin. Immunol. Pract.",
"key": "ref_15",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.2337/dc20-2260",
"article-title": "COVID-19 Severity Is Tripled in the Diabetes Community: A Prospective Analysis of the Pandemic’s Impact in Type 1 and Type 2 Diabetes",
"author": "Gregory",
"doi-asserted-by": "crossref",
"first-page": "526",
"journal-title": "Diabetes Care",
"key": "ref_16",
"volume": "44",
"year": "2020"
},
{
"DOI": "10.3201/eid2608.200679",
"article-title": "Population-Based Estimates of Chronic Conditions Affecting Risk for Complications from Coronavirus Disease, United States",
"author": "Adams",
"doi-asserted-by": "crossref",
"first-page": "1831",
"journal-title": "Emerg. Infect. Dis.",
"key": "ref_17",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1177/10870547211003659",
"article-title": "The Association between ADHD and the Severity of COVID-19 Infection",
"author": "Merzon",
"doi-asserted-by": "crossref",
"first-page": "491",
"journal-title": "J. Atten. Disord.",
"key": "ref_18",
"volume": "26",
"year": "2022"
},
{
"DOI": "10.3390/jcm10020199",
"doi-asserted-by": "crossref",
"key": "ref_19",
"unstructured": "Tudoran, C., Tudoran, M., Lazureanu, V.E., Marinescu, A.R., Pop, G.N., Pescariu, A.S., Enache, A., and Cut, T.G. (2021). Evidence of Pulmonary Hypertension after SARS-CoV-2 Infection in Subjects without Previous Significant Cardiovascular Pathology. J. Clin. Med., 10."
},
{
"DOI": "10.3389/fphys.2022.1023758",
"article-title": "From acute SARS-CoV-2 infection to pulmonary hypertension",
"author": "Eroume",
"doi-asserted-by": "crossref",
"first-page": "1023758",
"journal-title": "Front. Physiol.",
"key": "ref_20",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.37247/PAMED4ED.4.22.4",
"doi-asserted-by": "crossref",
"key": "ref_21",
"unstructured": "Tudoran, C., Tudoran, M., Lazureanu, V.E., Marinescu, A.R., Cut, T.G., Oancea, C., Pescariu, S.A., and Pop, G.N. (2021). Factors Influencing the Evolution of Pulmonary Hypertension in Previously Healthy Subjects Recovering from a SARS-CoV-2 Infection. J. Clin. Med., 10."
},
{
"DOI": "10.3390/jcm9082511",
"doi-asserted-by": "crossref",
"key": "ref_22",
"unstructured": "Caci, G., Albini, A., Malerba, M., Noonan, D.M., Pochetti, P., and Polosa, R. (2020). COVID-19 and Obesity: Dangerous Liaisons. J. Clin. Med., 9."
},
{
"DOI": "10.1038/s41366-020-0648-x",
"article-title": "The impact of obesity on COVID-19 complications: A retrospective cohort study",
"author": "Nakeshbandi",
"doi-asserted-by": "crossref",
"first-page": "1832",
"journal-title": "Int. J. Obes.",
"key": "ref_23",
"volume": "44",
"year": "2020"
},
{
"DOI": "10.1016/j.orcp.2020.07.002",
"article-title": "Obesity and mortality of COVID-19. Meta-analysis",
"author": "Hussain",
"doi-asserted-by": "crossref",
"first-page": "295",
"journal-title": "Obes. Res. Clin. Pract.",
"key": "ref_24",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.metabol.2020.154262",
"article-title": "Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York",
"author": "Palaiodimos",
"doi-asserted-by": "crossref",
"first-page": "154262",
"journal-title": "Metabolism",
"key": "ref_25",
"volume": "108",
"year": "2020"
},
{
"DOI": "10.5114/aoms.2016.58928",
"article-title": "Obesity and inflammation: The linking mechanism and the complications",
"author": "Ellulu",
"doi-asserted-by": "crossref",
"first-page": "851",
"journal-title": "Arch. Med. Sci.",
"key": "ref_26",
"volume": "13",
"year": "2017"
},
{
"DOI": "10.1016/j.ijcard.2016.04.089",
"article-title": "Obesity can predict and promote systemic inflammation in healthy adults",
"author": "Ellulu",
"doi-asserted-by": "crossref",
"first-page": "318",
"journal-title": "Int. J. Cardiol.",
"key": "ref_27",
"volume": "215",
"year": "2016"
},
{
"DOI": "10.1161/CIRCRESAHA.116.307591",
"article-title": "Treatment of Obesity: Weight Loss and Bariatric Surgery",
"author": "Wolfe",
"doi-asserted-by": "crossref",
"first-page": "1844",
"journal-title": "Circ. Res.",
"key": "ref_28",
"volume": "118",
"year": "2016"
},
{
"DOI": "10.1001/jamasurg.2013.3654",
"article-title": "The effectiveness and risks of bariatric surgery: An updated systematic review and meta-analysis",
"author": "Chang",
"doi-asserted-by": "crossref",
"first-page": "275",
"journal-title": "JAMA Surg.",
"key": "ref_29",
"volume": "149",
"year": "2014"
},
{
"DOI": "10.1177/1535370216688567",
"article-title": "Vitamin D alteration associated with obesity and bariatric surgery",
"author": "Lespessailles",
"doi-asserted-by": "crossref",
"first-page": "1086",
"journal-title": "Exp. Biol. Med.",
"key": "ref_30",
"volume": "242",
"year": "2017"
},
{
"DOI": "10.4103/1319-3767.164183",
"article-title": "Endocrine and metabolic complications after bariatric surgery",
"author": "Jammah",
"doi-asserted-by": "crossref",
"first-page": "269",
"journal-title": "Saudi J. Gastroenterol.",
"key": "ref_31",
"volume": "21",
"year": "2015"
},
{
"DOI": "10.1007/s11695-021-05761-8",
"article-title": "Bariatric Surgery and COVID-19: What We Have Learned from the Pandemic in Iran: A Retrospective Study",
"author": "Moradpour",
"doi-asserted-by": "crossref",
"first-page": "18",
"journal-title": "Obes. Surg.",
"key": "ref_32",
"volume": "32",
"year": "2022"
},
{
"DOI": "10.1002/dmrr.3398",
"article-title": "Haemoglobin A1c is a predictor of COVID-19 severity in patients with diabetes",
"author": "Merzon",
"doi-asserted-by": "crossref",
"first-page": "e3398",
"journal-title": "Diabetes Metab. Res. Rev.",
"key": "ref_33",
"volume": "37",
"year": "2021"
},
{
"DOI": "10.1007/s11695-022-05915-2",
"article-title": "Is COVID-19 Severity Impacted by Bariatric Surgery in the Early Postoperative Period?",
"author": "Siqueira",
"doi-asserted-by": "crossref",
"first-page": "1178",
"journal-title": "Obes. Surg.",
"key": "ref_34",
"volume": "32",
"year": "2022"
},
{
"DOI": "10.1007/s11695-020-05193-w",
"article-title": "Effects of Bariatric Surgery on COVID-19: A Multicentric Study from a High Incidence Area",
"author": "Marchesi",
"doi-asserted-by": "crossref",
"first-page": "2477",
"journal-title": "Obes. Surg.",
"key": "ref_35",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.1002/oby.23314",
"article-title": "History of bariatric surgery and COVID-19 outcomes in patients with type 2 diabetes: Results from the CORONADO study",
"author": "Blanchard",
"doi-asserted-by": "crossref",
"first-page": "599",
"journal-title": "Obesity",
"key": "ref_36",
"volume": "30",
"year": "2022"
},
{
"DOI": "10.1371/journal.pone.0215639",
"doi-asserted-by": "crossref",
"key": "ref_37",
"unstructured": "Sagie, S., Na’amnih, W., Frej, J., Cohen, D., Alpert, G., and Muhsen, K. (2019). Correlates of Hospitalizations in Internal Medicine Divisions among Israeli Adults of Different Ethnic Groups with Hypertension, Diabetes and Cardiovascular Diseases. PLoS ONE, 14."
},
{
"DOI": "10.3389/fmed.2020.00146",
"article-title": "The Malnutritional Status of the Host as a Virulence Factor for New Coronavirus SARS-CoV-2",
"author": "Briguglio",
"doi-asserted-by": "crossref",
"first-page": "146",
"journal-title": "Front. Med.",
"key": "ref_38",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.ecl.2017.07.006",
"article-title": "Vitamin D Metabolism in Bariatric Surgery",
"author": "Chakhtoura",
"doi-asserted-by": "crossref",
"first-page": "947",
"journal-title": "Endocrinol. Metab. Clin. N. Am.",
"key": "ref_39",
"volume": "46",
"year": "2017"
},
{
"DOI": "10.1002/2211-5463.13309",
"article-title": "Seasonal UV exposure and vitamin D: Association with the dynamics of COVID-19 transmission in Europe",
"author": "Mukherjee",
"doi-asserted-by": "crossref",
"first-page": "106",
"journal-title": "FEBS Open Bio",
"key": "ref_40",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1007/s11739-021-02902-w",
"article-title": "Vitamin D deficiency is associated with higher risks for SARS-CoV-2 infection and COVID-19 severity: A retrospective case-control study",
"author": "Israel",
"doi-asserted-by": "crossref",
"first-page": "1053",
"journal-title": "Intern. Emerg. Med.",
"key": "ref_41",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1038/s41598-023-29519-7",
"article-title": "Contribution of vitamin D3 and thiols status to the outcome of COVID-19 disease in Italian pediatric and adult patients",
"author": "Annamaria",
"doi-asserted-by": "crossref",
"first-page": "2504",
"journal-title": "Sci. Rep.",
"key": "ref_42",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1186/s41983-023-00611-z",
"article-title": "A review article on neuroprotective, immunomodulatory, and anti-inflammatory role of vitamin-D3 in elderly COVID-19 patients",
"author": "Tripathi",
"doi-asserted-by": "crossref",
"first-page": "18",
"journal-title": "Egypt J. Neurol. Psychiatr. Neurosurg.",
"key": "ref_43",
"volume": "59",
"year": "2023"
},
{
"DOI": "10.14336/AD.2022.0424",
"article-title": "Risk Factors for One-Year Mortality in Hospitalized Adults with Severe COVID-19",
"author": "Calatayud",
"doi-asserted-by": "crossref",
"first-page": "14",
"journal-title": "Aging Dis.",
"key": "ref_44",
"volume": "14",
"year": "2023"
},
{
"article-title": "A higher frequency of physical activity is associated with reduced rates of SARS-CoV-2 infection",
"author": "Green",
"first-page": "2138855",
"journal-title": "Eur. J. Gen. Pract.",
"key": "ref_45",
"volume": "7",
"year": "2022"
},
{
"DOI": "10.1136/bjsports-2021-104080",
"article-title": "Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients",
"author": "Sallis",
"doi-asserted-by": "crossref",
"first-page": "1099",
"journal-title": "Br. J. Sports Med.",
"key": "ref_46",
"volume": "55",
"year": "2021"
},
{
"article-title": "Associations of Physical Inactivity and COVID-19 Outcomes Among Subgroups",
"author": "Young",
"first-page": "492",
"journal-title": "Am. J. Prev. Med.",
"key": "ref_47",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1016/j.jaip.2020.11.020",
"article-title": "COVID-19 Susceptibility in Bronchial Asthma",
"author": "Green",
"doi-asserted-by": "crossref",
"first-page": "684",
"journal-title": "J. Allergy Clin. Immunol. Pract.",
"key": "ref_48",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1101/2020.06.01.20118877",
"doi-asserted-by": "crossref",
"key": "ref_49",
"unstructured": "Israel, A., Felhamer, E., Lahad, A., Levin-Zamit, L., and Lavie, G. (MedRxiv, 2020). Smoking and the risk of COVID-19 in a large observational population study, MedRxiv, preprint."
},
{
"DOI": "10.1007/s00415-023-11618-0",
"article-title": "Modifiable risk factors of COVID-19 in patients with multiple sclerosis: A single-centre case-control study",
"author": "Montini",
"doi-asserted-by": "crossref",
"first-page": "1835",
"journal-title": "J. Neurol.",
"key": "ref_50",
"volume": "270",
"year": "2023"
},
{
"DOI": "10.1148/radiol.2020201433",
"article-title": "Well-aerated lung on admitting chest CT to predict adverse outcome in COVID-19 Pneumonia",
"author": "Colombi",
"doi-asserted-by": "crossref",
"first-page": "E86",
"journal-title": "Radiology",
"key": "ref_51",
"volume": "296",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "ref_52",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2020.01359",
"article-title": "Cytokine release syndrome (CRS) and nicotine in COVID-19 patients: Trying to calm the storm",
"author": "Najera",
"doi-asserted-by": "crossref",
"first-page": "1359",
"journal-title": "Front. Immunol.",
"key": "ref_53",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.34172/jcvtr.2020.22",
"article-title": "Nicotine and smoking in the COVID-19 era",
"author": "Tajlil",
"doi-asserted-by": "crossref",
"first-page": "136",
"journal-title": "J. Cardiovasc. Thorac. Res.",
"key": "ref_54",
"volume": "12",
"year": "2020"
},
{
"article-title": "Transdermal nictoine for induction of remission in ulcerative colitis",
"author": "McGrath",
"first-page": "CD004722",
"journal-title": "Cochrane Database Syst. Rev.",
"key": "ref_55",
"volume": "18",
"year": "2004"
},
{
"article-title": "Mechanism of disease: Nicotine- a review of its actions in the context of gastrointestinal disease",
"author": "Thomas",
"first-page": "536",
"journal-title": "Nat. Clin. Pract.",
"key": "ref_56",
"volume": "2",
"year": "2005"
}
],
"reference-count": 56,
"references-count": 56,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2077-0383/12/12/4054"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "The Association of Weight Reduction and Other Variables after Bariatric Surgery with the Likelihood of SARS-CoV-2 Infection",
"type": "journal-article",
"volume": "12"
}
