Serum 25(OH) Vitamin D Levels in Pregnant Women with Coronavirus Disease 2019 (COVID-19): A Case-Control Study
et al., International Journal of Environmental Research and Public Health, doi:10.3390/ijerph19073965, Mar 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 256 pregnant women, 82 with COVID-19 and 174 controls, showing significantly lower vitamin D levels for COVID-19 patients.
This is the 127th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of ICU admission, 81.8% lower, RR 0.18, p = 1.00, high D levels (≥20ng/mL) 0 of 9 (0.0%), low D levels (<20ng/mL) 4 of 73 (5.5%), NNT 18, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), excluded in exclusion analyses:
unadjusted results with no group details.
|
|
risk of moderate/severe case, 88.7% lower, RR 0.11, p = 1.00, high D levels (≥20ng/mL) 0 of 9 (0.0%), low D levels (<20ng/mL) 7 of 73 (9.6%), NNT 10, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm), excluded in exclusion analyses:
unadjusted results with no group details.
|
|
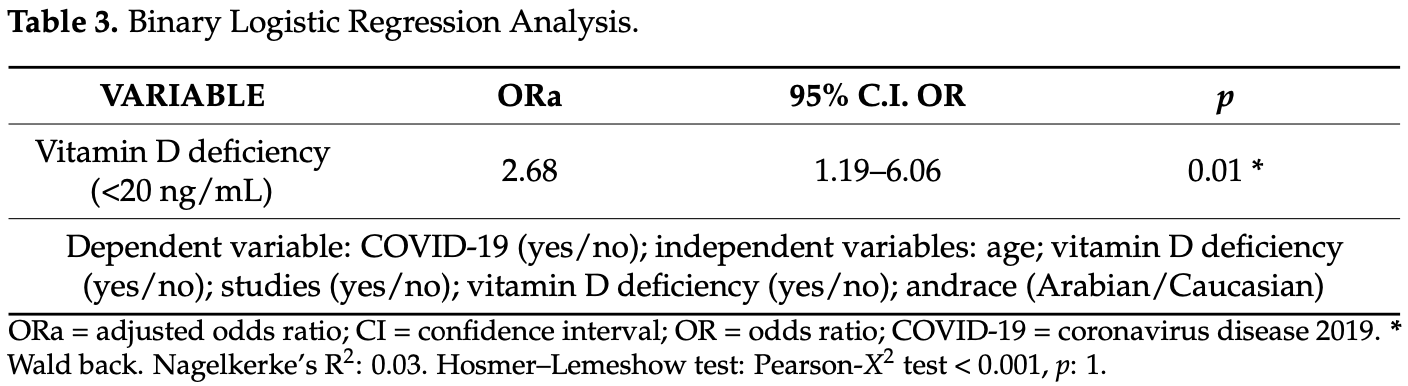
risk of case, 62.7% lower, OR 0.37, p = 0.01, cutoff 20ng/mL, adjusted per study, inverted to make OR<1 favor high D levels (≥20ng/mL), multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ferrer-Sánchez et al., 26 Mar 2022, retrospective, Spain, peer-reviewed, 7 authors.
Serum 25(OH) Vitamin D Levels in Pregnant Women with Coronavirus Disease 2019 (COVID-19): A Case-Control Study
International Journal of Environmental Research and Public Health, doi:10.3390/ijerph19073965
The physiological changes during pregnancy may increase the risk of complications in pregnant women with coronavirus disease 2019 (COVID-19). Vitamin D is a fat-soluble secosteroid hormone and its role in immunity is appears to be of particular importance in this recent pandemic. Nevertheless, there is little research about the role of vitamin D levels regarding COVID-19 in pregnant women to date. This study aimed to establish a relationship between serum 25-hydroxyvitamin D (25(OH)D) levels in pregnant women and COVID-19. A comparative case-control study was performed with a study population of 256 pregnant women (82 pregnant women with infection and 174 women in control group). Serum 25(OH)D levels were significantly lower in pregnant women with COVID-19 infection than in those without infection. In addition, 89% of COVID-19-positive pregnant women had 25(OH)D deficiency, while in the control group the percentage was 75.30%, finding statistically significant differences (ORa = 2.68; 95% CI 1.19-6.06; p = 0.01). Our results find a relationship between vitamin D deficiency in pregnant women and COVID-19 infection. This finding could be relevant for actual clinical practice. Thus, more research is needed in this field.
Institutional Review Board Statement: The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of the Torrecardenas University Hospital (protocol code 2607-143/2020 and date of approval: 27 January 2021). Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
References
Angelidi, Belanger, Lorinsky, Karamanis, Chamorro-Pareja et al., Vitamin D status is associated with in-hospital mortality and mechanical ventilation: A cohort of COVID-19 hospitalized patients, Mayo Clin. Proc, doi:10.1016/j.mayocp.2021.01.001
Bahat, Talma, Bestel, Selcuki, Aydın et al., Micronutrients in COVID-19 Positive Pregnancies, Cureus, doi:10.7759/cureus.10609
Bikle, Extraskeletal actions of vitamin D, Ann. N. Y. Acad. Sci, doi:10.1111/nyas.13219
Brenner, Hearing, The protective role of melanin against UV damage in human skin, Photochem. Photobiol, doi:10.1111/j.1751-1097.2007.00226.x
Caprio, Infante, Calanchini, Mammi, Fabbri et al., Not just the bone. Evidence for beneficial pleiotropic extraskeletal effects, Eat. Weight. Disord, doi:10.1007/s40519-016-0312-6
Chauss, Freiwald, Mcgregor, Yan, Wang et al., Autocrine vitamin D signaling switches off pro-inflammatory programs of TH1 cells, Nat. Immunol, doi:10.1038/s41590-021-01080-3
Di Mascio, Khalil, Saccone, Rizzo, Buca et al., Outcome of Coronavirus spectrum infections (SARS, MERS, COVID 1-19) during pregnancy: A systematic review and meta-analysis, AJOG MFM, doi:10.1016/j.ajogmf.2020.100107
Ferrari, Locatelli, Briguglio, Lombardi, Is there a link between vitamin D status, SARS-CoV-2 infection risk and COVID-19 severity?, Cell Biochem. Funct, doi:10.1002/cbf.3597
Gil, Plaza-Diaz, Mesa, Vitamin D: Classic and novel actions, Ann. Nutr. Metab, doi:10.1159/000486536
Katz, Yue, Xue, Increased risk for COVID-19 in patients with vitamin D deficiency, Nutrition, doi:10.1016/j.nut.2020.111106
Leino, Turpeinen, Koskinen, Automated measurement of 25-OH vitamin D3 on the Roche Modular E170 Analyzer, Clin. Chem, doi:10.1373/clinchem.2008.111732
Luo, Liao, Shen, Li, Cheng, Vitamin D deficiency is inversely associated with COVID-19 incidence and disease severity in Chinese people, J. Nutr, doi:10.1093/jn/nxaa332
Madjunkov, Dviri, Librach, A comprehensive review of the impact of COVID-19 on human reproductive biology, assisted reproduction care and pregnancy: A Canadian perspective, J. Ovarian Res, doi:10.1186/s13048-020-00737-1
Mansur, Tajer, Mariani, Inserra, Ferder et al., Vitamin D high doses supplementation could represent a promising alternative to prevent or treat COVID-19 infection, Clín. Investig. Arter, doi:10.1016/j.artere.2020.11.003
Martineau, Cates, Urashima, Jensen, Griffiths et al., Vitamin D for the management to asthma, Cochrane Database Syst. Rev, doi:10.1002/14651858.CD011511.pub2
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: An Israeli population-based study, FEBS J, doi:10.1111/febs.15495
Musavi, Abazari, Barartabar, Kalaki-Jouybari, Hemmati-Dinarvand et al., The benefits of Vitamin D in the COVID-19 pandemic: Biochemical and immunological mechanisms, Arch. Physiol. Biochem, doi:10.1080/13813455.2020.1826530
Narang, Enninga, Gunaratne, Ibirogba, Trad et al., SARS-CoV-2 infection and COVID-19 during pregnancy: A multidisciplinary review, Mayo Clin. Proc, doi:10.1016/j.mayocp.2020.05.011
Norman, From vitamin D to hormone D: Fundamentals of the vitamin D endocrine system essential for good health, Am J. Clin. Nutr, doi:10.1093/ajcn/88.2.491S
Pereira, Dantas Damascena, Galvão Azevedo, De Almeida Oliveira, Da Mota Santana, Vitamin D deficiency aggravates COVID-19: Systematic review and metaanalysis, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408398.2020.1841090
Pfeffer, Lu, Mann, Chen, Ho et al., Effects of vitamin D on inflammatory and oxidative stress responses of human bronchial epithelial cells exposed to particulate matter, PLoS ONE, doi:10.1371/journal.pone.0200040
Qin, Lu, Yang, Xu, Luo, Does maternal vitamin D deficiency increase the risk of preterm birth: A meta-analysis of observational studies, Nutrients, doi:10.3390/nu8050301
Santamaria, Bi, Leduc, Tabatabaei, Jantchou et al., Prenatal vitamin D status and offspring's growth, adiposity and metabolic health: A systematic review and meta-analysis, Br. J. Nutr, doi:10.1017/S0007114517003646
Schulz, Cruze, Wei, Gehris, Wagner, Maternal vitamin D sufficiency and reduced placental gene expression in angiogenic biomarkers related to comorbidities of pregnancy, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2017.02.003
Sinaci, Ocal, Yetiskin, Hendem, Buyuk et al., Impact of vitamin D on the course of COVID-19 during pregnancy: A case control study, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2021.105964
Smith, Kirkpatrick, Kovilam, Agrawal, Immunomodulatory role of vitamin D in the pathogenesis of preeclampsia, Expert Rev. Clin. Immunol, doi:10.1586/1744666X.2015.1056780
Tekin, Yassa, Birol, Unlu, Sahin et al., Vitamin D status is not associated with clinical severity of COVID-19 in pregnant women, Eur. J. Nutr, doi:10.1007/s00394-021-02709-7
Umar, Sastry, Chouchane, Role of vitamin D beyond the skeletal function: A review of the molecular and clinical studies, Int. J. Mol. Sci, doi:10.3390/ijms19061618
Vassiliou, Jahaj, Pratikaki, Keskinidou, Detsika et al., Vitamin D deficiency correlates with a reduced number of natural killer cells in intensive care unit (ICU) and non-ICU patients with COVID-19 pneumonia, Hell. J. Cardiol. C, doi:10.1016/j.hjc.2020.11.011
Wang, Zhang, Song, Zhang, Serum vitamin D deficiency and risk of gestational diabetes mellitus: A meta-analysis, Arch. Med. Sci, doi:10.5114/aoms.2020.94433
Wastnedge, Reynolds, Van Boeckel, Stock, Denison et al., Pregnancy and COVID-19, Physiol. Rev, doi:10.1152/physrev.00024.2020
Weishaar, Rajan, Keller, Probability of vitamin D deficiency by body weight and race/ethnicity, J. Am. Board Fam. Med, doi:10.3122/jabfm.2016.02.150251
DOI record:
{
"DOI": "10.3390/ijerph19073965",
"ISSN": [
"1660-4601"
],
"URL": "http://dx.doi.org/10.3390/ijerph19073965",
"abstract": "<jats:p>The physiological changes during pregnancy may increase the risk of complications in pregnant women with coronavirus disease 2019 (COVID-19). Vitamin D is a fat-soluble secosteroid hormone and its role in immunity is appears to be of particular importance in this recent pandemic. Nevertheless, there is little research about the role of vitamin D levels regarding COVID-19 in pregnant women to date. This study aimed to establish a relationship between serum 25-hydroxyvitamin D (25(OH)D) levels in pregnant women and COVID-19. A comparative case-control study was performed with a study population of 256 pregnant women (82 pregnant women with infection and 174 women in control group). Serum 25(OH)D levels were significantly lower in pregnant women with COVID-19 infection than in those without infection. In addition, 89% of COVID-19-positive pregnant women had 25(OH)D deficiency, while in the control group the percentage was 75.30%, finding statistically significant differences (ORa = 2.68; 95% CI 1.19–6.06; p = 0.01). Our results find a relationship between vitamin D deficiency in pregnant women and COVID-19 infection. This finding could be relevant for actual clinical practice. Thus, more research is needed in this field.</jats:p>",
"alternative-id": [
"ijerph19073965"
],
"author": [
{
"affiliation": [],
"family": "Ferrer-Sánchez",
"given": "Nazaret",
"sequence": "first"
},
{
"affiliation": [],
"family": "Díaz-Goicoechea",
"given": "Marina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mayoral-Cesar",
"given": "Victoria",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9043-7745",
"affiliation": [],
"authenticated-orcid": false,
"family": "García-Solbas",
"given": "Silvia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5917-7404",
"affiliation": [],
"authenticated-orcid": false,
"family": "Nievas-Soriano",
"given": "Bruno José",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Parrón-Carreño",
"given": "Tesifón",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4844-2145",
"affiliation": [],
"authenticated-orcid": false,
"family": "Fernández-Alonso",
"given": "Ana María",
"sequence": "additional"
}
],
"container-title": [
"International Journal of Environmental Research and Public Health"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
3,
28
]
],
"date-time": "2022-03-28T01:27:51Z",
"timestamp": 1648430871000
},
"deposited": {
"date-parts": [
[
2022,
3,
28
]
],
"date-time": "2022-03-28T01:59:06Z",
"timestamp": 1648432746000
},
"indexed": {
"date-parts": [
[
2022,
3,
28
]
],
"date-time": "2022-03-28T02:41:45Z",
"timestamp": 1648435305410
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "1660-4601"
}
],
"issue": "7",
"issued": {
"date-parts": [
[
2022,
3,
26
]
]
},
"journal-issue": {
"issue": "7",
"published-online": {
"date-parts": [
[
2022,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
3,
26
]
],
"date-time": "2022-03-26T00:00:00Z",
"timestamp": 1648252800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1660-4601/19/7/3965/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "3965",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
3,
26
]
]
},
"published-online": {
"date-parts": [
[
2022,
3,
26
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref1",
"unstructured": "Coronavirus (COVID-19)https://who.sprinklr.com/"
},
{
"DOI": "10.1186/s13048-020-00737-1",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1152/physrev.00024.2020",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1016/j.ajogmf.2020.100107",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1016/j.mayocp.2020.05.011",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1093/ajcn/88.2.491S",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1159/000486536",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1111/nyas.13219",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.3390/ijms19061618",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1007/s40519-016-0312-6",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1136/bmj.i6583",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1586/1744666X.2015.1056780",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1016/j.jsbmb.2017.02.003",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.3390/nu8050301",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.5114/aoms.2020.94433",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1017/S0007114517003646",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1111/j.1751-1097.2007.00226.x",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.3122/jabfm.2016.02.150251",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"key": "ref19",
"unstructured": "Living Guidance for Clinical Management of COVID-19https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2"
},
{
"DOI": "10.1373/clinchem.2008.111732",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1016/j.jsbmb.2021.105964",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1007/s00394-021-02709-7",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.7759/cureus.10609",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1111/febs.15495",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1016/j.nut.2020.111106",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1080/10408398.2020.1841090",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1093/jn/nxaa332",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1016/j.mayocp.2021.01.001",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1002/14651858.CD011511.pub2",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1371/journal.pone.0200040",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1080/13813455.2020.1826530",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1016/j.artere.2020.11.003",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1002/cbf.3597",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1038/s41590-021-01080-3",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1016/j.hjc.2020.11.011",
"doi-asserted-by": "publisher",
"key": "ref35"
}
],
"reference-count": 35,
"references-count": 35,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1660-4601/19/7/3965"
}
},
"score": 1,
"short-container-title": [
"IJERPH"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Health, Toxicology and Mutagenesis",
"Public Health, Environmental and Occupational Health"
],
"subtitle": [],
"title": [
"Serum 25(OH) Vitamin D Levels in Pregnant Women with Coronavirus Disease 2019 (COVID-19): A Case-Control Study"
],
"type": "journal-article",
"volume": "19"
}
