Impact of treatment of COVID-19 with sotrovimab on post-acute sequelae of COVID-19 (PASC): an analysis of National COVID Cohort Collaborative (N3C) data
et al., Infection, doi:10.1007/s15010-025-02505-z, Mar 2025
Sotrovimab for COVID-19
45th treatment shown to reduce risk in
August 2022, now with p = 0.00048 from 29 studies, recognized in 42 countries.
Efficacy is variant dependent.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
N3C retrospective 9,504 sotrovimab-treated high-risk COVID-19 patients versus 619,668 untreated high-risk controls showing reduced risk of post-acute sequelae of COVID-19 (PASC) with treatment.
Confounding by treatment propensity. This study analyzes a population
where only a fraction of eligible patients received the treatment. Patients
receiving treatment may be more likely to follow other recommendations, more
likely to receive additional care, and more likely to use additional
treatments that are not tracked in the data (e.g., nasal/oral hygiene1,2, vitamin D3, etc.) — either because the physician
recommending sotrovimab also recommended them, or
because the patient seeking out sotrovimab is more
likely to be familiar with the efficacy of additional treatments and more
likely to take the time to use them.
Therefore, these kind of studies may
overestimate efficacy.
ATT weighting failed to adjust for "healthcare encounters during acute phase before index", with the weighted sample still having 2.75x mean encounters for the treatment group, where patients are likely to also receive advice for beneficial non-prescription treatments.
Efficacy is variant dependent. In Vitro studies predict lower efficacy for BA.14-6, BA.4, BA.57, XBB.1.9.3, XBB.1.5.24, XBB.2.9, CH.1.18, and no efficacy for BA.29, XBB, XBB.1.5, ХВВ.1.9.110, XBB.1.16, BQ.1.1.45, and CL.18. US EUA has been revoked.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments11.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
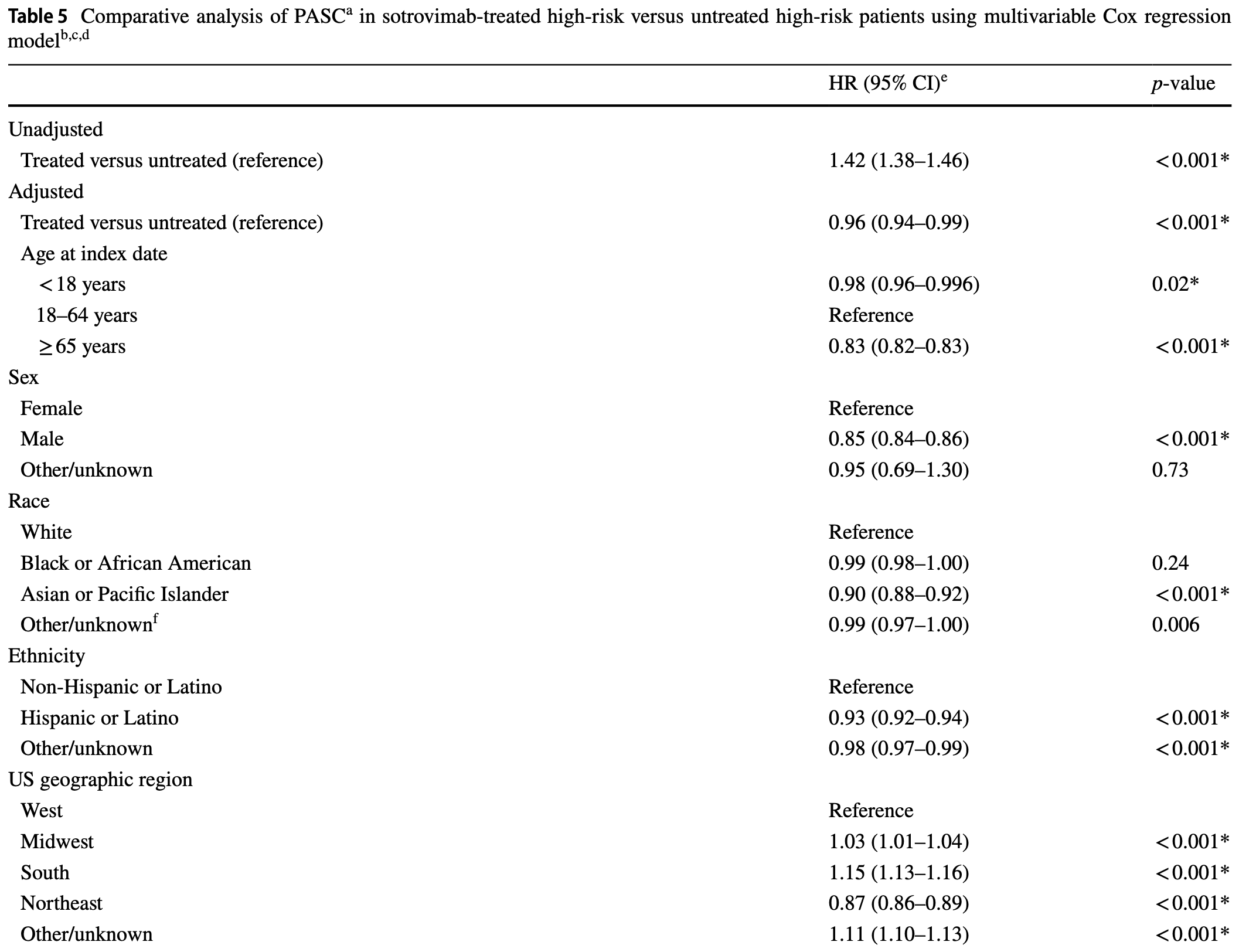
risk of long COVID, 4.0% lower, HR 0.96, p = 0.002, adjusted per study, multivariable, Cox proportional hazards, RR approximated with OR.
|
|
risk of long COVID, 8.0% lower, OR 0.92, p < 0.001, treatment 9,504, control 9,523, ATT, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
4.
Liu et al., Striking Antibody Evasion Manifested by the Omicron Variant of SARS-CoV-2, bioRxiv, doi:10.1101/2021.12.14.472719.
5.
Sheward et al., Variable loss of antibody potency against SARS-CoV-2 B.1.1.529 (Omicron), bioRxiv, doi:10.1101/2021.12.19.473354.
6.
VanBlargan et al., An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by several therapeutic monoclonal antibodies, bioRxiv, doi:10.1101/2021.12.15.472828.
7.
Haars et al., Prevalence of SARS-CoV-2 Omicron Sublineages and Spike Protein Mutations Conferring Resistance against Monoclonal Antibodies in a Swedish Cohort during 2022–2023, Microorganisms, doi:10.3390/microorganisms11102417.
8.
Pochtovyi et al., In Vitro Efficacy of Antivirals and Monoclonal Antibodies against SARS-CoV-2 Omicron Lineages XBB.1.9.1, XBB.1.9.3, XBB.1.5, XBB.1.16, XBB.2.4, BQ.1.1.45, CH.1.1, and CL.1, Vaccines, doi:10.3390/vaccines11101533.
9.
Zhou et al., SARS-CoV-2 Omicron BA.2 Variant Evades Neutralization by Therapeutic Monoclonal Antibodies, bioRxiv, doi:10.1101/2022.02.15.480166.
Drysdale et al., 22 Mar 2025, retrospective, USA, peer-reviewed, 12 authors, study period 26 May, 2021 - 5 April, 2022.
Contact: myriam.g.drysdale@gsk.com.
Impact of treatment of COVID-19 with sotrovimab on post-acute sequelae of COVID-19 (PASC): an analysis of National COVID Cohort Collaborative (N3C) data
Infection, doi:10.1007/s15010-025-02505-z
Purpose To assess the impact of early sotrovimab treatment versus no treatment on the risk of developing post-acute sequelae of COVID-19 (PASC; long COVID) in patients (age ≥ 12 years) with COVID-19 at high risk for progression to severe disease. Methods Retrospective cohort study using the US National COVID Cohort Collaborative (N3C) data. Phase 1 identified and assessed multiple definitions of PASC; Phase 2 evaluated the effectiveness of sotrovimab for reducing the risk of PASC, utilizing definitions from Phase 1. Average treatment effect in the treated (ATT)-weighted Cox proportional hazards regression models were used to compare time to event for PASC between high-risk patients who received sotrovimab treatment between May 26, 2021 and April 5, 2022, and high-risk patients with COVID-19 diagnosed between May 26, 2021 and March 26, 2022 who did not receive any treatment for COVID-19 during the acute phase or any pre-exposure prophylaxis against SARS-CoV-2. Results A total of 9,504 sotrovimab-treated and 619,668 untreated patients were included in the main analysis. Most baseline characteristics were balanced between the two cohorts after ATT weighting. The doubly robust ATT-weighted hazard ratio (95% confidence interval) was 0.92 (0.89-0.96) (p < 0.001), indicating that sotrovimab use was associated with a significantly lower risk of PASC. Results remained consistent in sensitivity analyses. Conclusion In patients at high risk for severe COVID-19, the benefits of early sotrovimab treatment may extend beyond the acute phase of COVID-19 and contribute to the prevention of PASC symptoms.
Supplementary Information The online version contains supplementary material available at https:// doi . org/ 10. 1007/ s15010-025-02505-z. Author contributions All authors made a significant contribution to the work reported, whether that was in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the manuscript; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Declarations Conflict of interest MD, JH, HB, CS, MVD, and IAG are employed by and hold financial equities in GSK. RC, TG, MSD, DL, SK, and MDS are employees of Analysis Group; Analysis Group received funding from GSK to conduct the study. Disclaimer: This article was prepared while SK was an employee of Analysis Group. The opinions expressed in this article are her own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
Ethical approval and consent to participate This study complies with all applicable laws regarding subject privacy. No direct subject contact or primary collection of individual human subject data occurred. Study results were in tabular form and aggregate analyses that omit subject identification, therefore informed consent, ethics committee or Institutional Review..
References
Addetia, Piccoli, Case, Park, Beltramello et al., Therapeutic and vaccine-induced cross-reactive antibodies with effector function against emerging Omicron variants, bioRxiv, doi:10.1101/2023.01.17.523798
Aggarwal, Beaty, Bennett, Carlson, Davis et al., Real-world evidence of the neutralizing monoclonal antibody sotrovimab for preventing hospitalization and mortality in COVID-19 outpatients, J Infect Dis, doi:10.1093/infdis/jiac206
Al-Aly, Bowe, Xie, Long COVID after breakthrough SARS-CoV-2 infection, Nat Med, doi:10.1038/s41591-022-01840-0
Austin, Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples, Stat Med, doi:10.1002/sim.3697
Bennett, Moffitt, Hajagos, Amor, Anand et al., Clinical characterization and prediction of clinical severity of SARS-CoV-2 infection among US adults using data from the US National COVID Cohort Collaborative, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.16901
Bull-Otterson, Baca, Saydah, Boehmer, Adjei et al., Post-COVID conditions among adult COVID-19 survivors aged 18-64 and ≥65 years -United States, March 2020-November 2021, MMWR Morb Mortal Wkly Rep
Case, Mackin, Errico, Chong, Madden et al., Resilience of S309 and AZD7442 monoclonal antibody treatments against infection by SARS-CoV-2 Omicron lineage strains, Nat Commun, doi:10.1038/s41467-022-31615-7
Cathcart, Havenar-Daughton, Lempp, Ma, Schmid et al., The dual function monoclonal antibodies VIR-7831 and VIR-7832 demonstrate potent in vitro and in vivo activity against SARS-CoV-2, bioRxiv, doi:10.1101/2021.03.09.434607
Chen, Haupert, Zimmermann, Shi, Fritsche et al., Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: a meta-analysis and systematic review, J Infect Dis, doi:10.1093/infdis/jiac136
Cheng, Reyes, Satram, Birch, Gibbons et al., Real-world effectiveness of sotrovimab for the early treatment of COVID-19 during SARS-CoV-2 Delta and Omicron waves in the USA, Infect Dis Ther, doi:10.1007/s40121-022-00755-0
Davis, Assaf, Mccorkell, Wei, Low et al., Characterizing long COVID in an international cohort: 7 months of symptoms and their impact, EClinicalMedicine, doi:10.1016/j.eclinm.2021.101019
Doykov, Hallqvist, Gilmour, Grandjean, Mills et al., The long tail of Covid-19' -The detection of a prolonged inflammatory response after a SARS-CoV-2 infection in asymptomatic and mildly affected patients, F1000Res, doi:10.12688/f1000research.27287.2
Drysdale, Berktas, Gibbons, Rolland, Lavoie et al., Real-world effectiveness of sotrovimab for the treatment of SARS-CoV-2 infection during Omicron BA.2 and BA.5 subvariant predominance: a systematic literature review, Infection, doi:10.1007/s15010-024-02245-6
Drysdale, Gibbons, Singh, Rolland, Lavoie et al., Real-world effectiveness of sotrovimab for the treatment of SARS-CoV-2 infection during Omicron BA.2 subvariant predominance: a systematic literature review, Infection, doi:10.1007/s15010-023-02098-5
Durstenfeld, Peluso, Lin, Peyser, Isasi et al., Association of nirmatrelvir for acute SARS-CoV-2 infection with subsequent Long COVID symptoms in an observational cohort study, J Med Virol, doi:10.1002/jmv.29333
Greenhalgh, Knight, Court, Buxton, Husain, Management of post-acute covid-19 in primary care, BMJ, doi:10.1136/bmj.m3026
Hill, Mehta, Sharma, Mane, Xie et al., Risk factors associated with post-acute sequelae of SARS-CoV-2 in an EHR cohort: a National COVID Cohort Collaborative (N3C) analysis as part of the NIH RECOVER program, medRxiv, doi:10.1101/2022.08.15.22278603
Ioannou, Berry, Rajeevan, Li, Mutalik et al., Effectiveness of nirmatrelvir-ritonavir against the development of post-COVID-19 conditions among U.S. veterans: a target trial emulation, Ann Intern Med, doi:10.7326/M23-1394
Kff, As recommendations for isolation end, how common is long COVID?
Lin, Henderson, Carlile, Dillingham, Butler-Cole et al., Healthcare utilisation in people with long COVID: an OpenSAFELY cohort study, BMC Med, doi:10.1101/2023.12.21.23300305
O'mahoney, Routen, Gillies, Ekezie, Welford et al., The prevalence and long-term health effects of Long Covid among hospitalised and non-hospitalised populations: a systematic review and meta-analysis, EClinicalMedicine, doi:10.1016/j.eclinm.2022.101762
Park, Pinto, Walls, Liu, Marco et al., Imprinted antibody responses against SARS-CoV-2 Omicron sublineages, Science, doi:10.1126/science.adc9127
Parotto, Gyongyosi, Howe, Myatra, Ranzani et al., Post-acute sequelae of COVID-19: understanding and addressing the burden of multisystem manifestations, Lancet Respir Med, doi:10.1016/S2213-2600(23)00239-4
Patel, Levick, Boult, Gibbons, Drysdale et al., Characteristics and outcomes of COVID-19 patients presumed to be treated with sotrovimab in NHS hospitals in England, BMC Infect Dis, doi:10.1186/s12879-024-09311-2
Patel, Yarwood, Levick, Gibbons, Drysdale et al., Characteristics and outcomes of patients with COVID-19 at high-risk of disease progression receiving sotrovimab, oral antivirals or no treatment in England, Curr Med Res Opin, doi:10.1080/03007995.2024.2376144
Peluso, Lu, Tang, Durstenfeld, Ho et al., Markers of immune activation and inflammation in individuals with postacute sequelae of severe acute respiratory syndrome coronavirus 2 infection, J Infect Dis, doi:10.1093/infdis/jiab490
Pfaff, Madlock-Brown, Baratta, Bhatia, Davis et al., Coding long COVID: characterizing a new disease through an ICD-10 lens, BMC Med, doi:10.1186/s12916-023-02737-6
Pinto, Park, Beltramello, Walls, Tortorici et al., Cross-neutralization of SARS-CoV-2 by a human monoclonal SARS-CoV antibody, Nature, doi:10.1038/s41586-020-2349-y
Tannous, Pan, Potter, Bako, Dlouhy et al., Real-world effectiveness of COVID-19 vaccines and anti-SARS-CoV-2 monoclonal antibodies against postacute sequelae of SARS-CoV-2: analysis of a COVID-19 observational registry for a diverse US metropolitan population, BMJ Open, doi:10.1136/bmjopen-2022-067611
Tazare, Nab, Zheng, Hulme, Green, Effectiveness of sotrovimab and molnupiravir in community settings in England across the Omicron BA.1 and BA.2 sublineages: emulated target trials using the Open-SAFELY platform, medRxiv, doi:10.1101/2023.05.12.23289914
Thaweethai, Jolley, Karlson, Levitan, Levy et al., Development of a definition of postacute sequelae of SARS-CoV-2 infection, JAMA, doi:10.1001/jama.2023.8823
Uraki, Kiso, Iida, Imai, Takashita et al., Characterization and antiviral susceptibility of SARS-CoV-2 Omicron BA.2, Nature, doi:10.1038/s41586-022-04856-1
Visvabharathy, Hanson, Orban, Lim, Palacio et al., T cell responses to SARS-CoV-2 in people with and without neurologic symptoms of long COVID, medRxiv, doi:10.1101/2021.08.08.21261763
Walker, Schnell, Kerr, Antiviral agents against Omicron subvariant BA.4.6 in vitro, N Engl J Med, doi:10.1056/NEJMc2216611
Wang, Mao, Klein, Dai, Huck et al., Diverse functional autoantibodies in patients with COVID-19, Nature, doi:10.1038/s41586-021-03631-y
Wang, Ramasamy, Verduzco-Gutierrez, Brode, Melamed, Acute and post-acute sequelae of SARS-CoV-2 infection: a review of risk factors and social determinants, Virol J, doi:10.1186/s12985-023-02061-8
Wang, Zhao, Shi, Jia, Paxlovid reduces the risk of Long COVID in patients six months after hospital discharge, J Med Virol, doi:10.1002/jmv.29014
Xie, Choi, Al-Aly, Association of treatment with nirmatrelvir and the risk of post-COVID-19 condition, JAMA Intern Med, doi:10.1001/jamainternmed.2023.0743
Zheng, Green, Tazare, Comparative effectiveness of sotrovimab and molnupiravir for prevention of severe covid-19 outcomes in patients in the community: observational cohort study with the OpenSAFELY platform, BMJ, doi:10.1136/bmj-2022-071932
Zheng, Tazare, Nab, Mehrkar, Mackenna et al., Comparative effectiveness of paxlovid versus sotrovimab and molnupiravir for preventing severe COVID-19 outcomes in non-hospitalised patients: observational cohort study using the OpenSAFELY platform, medRxiv, doi:10.1101/2023.01.20.23284849
DOI record:
{
"DOI": "10.1007/s15010-025-02505-z",
"ISSN": [
"0300-8126",
"1439-0973"
],
"URL": "http://dx.doi.org/10.1007/s15010-025-02505-z",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:sec>\n <jats:title>Purpose</jats:title>\n <jats:p>To assess the impact of early sotrovimab treatment versus no treatment on the risk of developing post-acute sequelae of COVID-19 (PASC; long COVID) in patients (age ≥ 12 years) with COVID-19 at high risk for progression to severe disease.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>Retrospective cohort study using the US National COVID Cohort Collaborative (N3C) data. Phase 1 identified and assessed multiple definitions of PASC; Phase 2 evaluated the effectiveness of sotrovimab for reducing the risk of PASC, utilizing definitions from Phase 1. Average treatment effect in the treated (ATT)-weighted Cox proportional hazards regression models were used to compare time to event for PASC between high-risk patients who received sotrovimab treatment between May 26, 2021 and April 5, 2022, and high-risk patients with COVID-19 diagnosed between May 26, 2021 and March 26, 2022 who did not receive any treatment for COVID-19 during the acute phase or any pre-exposure prophylaxis against SARS-CoV-2.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>A total of 9,504 sotrovimab-treated and 619,668 untreated patients were included in the main analysis. Most baseline characteristics were balanced between the two cohorts after ATT weighting. The doubly robust ATT-weighted hazard ratio (95% confidence interval) was 0.92 (0.89–0.96) (<jats:italic>p</jats:italic> < 0.001), indicating that sotrovimab use was associated with a significantly lower risk of PASC. Results remained consistent in sensitivity analyses.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusion</jats:title>\n <jats:p>In patients at high risk for severe COVID-19, the benefits of early sotrovimab treatment may extend beyond the acute phase of COVID-19 and contribute to the prevention of PASC symptoms.</jats:p>\n </jats:sec>",
"alternative-id": [
"2505"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "24 July 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "1 March 2025"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "22 March 2025"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "MD, JH, HB, CS, MVD, and IAG are employed by and hold financial equities in GSK. RC, TG, MSD, DL, SK, and MDS are employees of Analysis Group; Analysis Group received funding from GSK to conduct the study. Disclaimer: This article was prepared while SK was an employee of Analysis Group. The opinions expressed in this article are her own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government."
},
{
"group": {
"label": "Ethical approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "This study complies with all applicable laws regarding subject privacy. No direct subject contact or primary collection of individual human subject data occurred. Study results were in tabular form and aggregate analyses that omit subject identification, therefore informed consent, ethics committee or Institutional Review Board (IRB) approval was not required. However, use of the N3C Limited Dataset requires IRB review. A request for a waiver of authorization was obtained from WCG IRB."
},
{
"group": {
"label": "Consent to publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "All named authors meet the International Committee of Medical Journal Editors criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published."
}
],
"author": [
{
"ORCID": "https://orcid.org/0000-0002-8994-2816",
"affiliation": [],
"authenticated-orcid": false,
"family": "Drysdale",
"given": "Myriam",
"sequence": "first"
},
{
"affiliation": [],
"family": "Chang",
"given": "Rose",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guo",
"given": "Tracy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Duh",
"given": "Mei Sheng",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0003-4744-8067",
"affiliation": [],
"authenticated-orcid": false,
"family": "Han",
"given": "Jennifer",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-4924-4810",
"affiliation": [],
"authenticated-orcid": false,
"family": "Birch",
"given": "Helen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sharpe",
"given": "Catherine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liu",
"given": "Daisy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kalia",
"given": "Sarah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Van Dyke",
"given": "Melissa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "DerSarkissian",
"given": "Maral",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-2265-9506",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gillespie",
"given": "Iain A.",
"sequence": "additional"
}
],
"container-title": "Infection",
"container-title-short": "Infection",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2025,
3,
23
]
],
"date-time": "2025-03-23T07:52:01Z",
"timestamp": 1742716321000
},
"deposited": {
"date-parts": [
[
2025,
3,
23
]
],
"date-time": "2025-03-23T07:52:05Z",
"timestamp": 1742716325000
},
"indexed": {
"date-parts": [
[
2025,
3,
24
]
],
"date-time": "2025-03-24T04:07:07Z",
"timestamp": 1742789227695,
"version": "3.40.2"
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2025,
3,
22
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
3,
22
]
],
"date-time": "2025-03-22T00:00:00Z",
"timestamp": 1742601600000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
3,
22
]
],
"date-time": "2025-03-22T00:00:00Z",
"timestamp": 1742601600000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s15010-025-02505-z.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s15010-025-02505-z/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s15010-025-02505-z.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1007",
"published": {
"date-parts": [
[
2025,
3,
22
]
]
},
"published-online": {
"date-parts": [
[
2025,
3,
22
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.15585/mmwr.mm7121e1",
"author": "L Bull-Otterson",
"doi-asserted-by": "publisher",
"first-page": "713",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "2505_CR1",
"unstructured": "Bull-Otterson L, Baca S, Saydah S, Boehmer TK, Adjei S, Gray S, et al. Post–COVID conditions among adult COVID-19 survivors aged 18–64 and ≥65 years — United States, March 2020–November 2021. MMWR Morb Mortal Wkly Rep. 2022;71:713–7.",
"volume": "71",
"year": "2022"
},
{
"DOI": "10.1016/S2213-2600(23)00239-4",
"author": "M Parotto",
"doi-asserted-by": "publisher",
"first-page": "739",
"issue": "8",
"journal-title": "Lancet Respir Med",
"key": "2505_CR2",
"unstructured": "Parotto M, Gyongyosi M, Howe K, Myatra SN, Ranzani O, Shankar-Hari M, et al. Post-acute sequelae of COVID-19: understanding and addressing the burden of multisystem manifestations. Lancet Respir Med. 2023;11(8):739–54. https://doi.org/10.1016/S2213-2600(23)00239-4.",
"volume": "11",
"year": "2023"
},
{
"key": "2505_CR3",
"unstructured": "National Center for Health Statistics. Long COVID. Household pulse survey. https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm. Accessed March 19, 2024."
},
{
"key": "2505_CR4",
"unstructured": "KFF. As recommendations for isolation end, how common is long COVID? https://www.kff.org/coronavirus-covid-19/issue-brief/as-recommendations-for-isolation-end-how-common-is-long-covid/. Accessed June 10, 2024."
},
{
"DOI": "10.1101/2023.12.21.23300305",
"author": "L-Y Lin",
"doi-asserted-by": "publisher",
"first-page": "255",
"issue": "1",
"journal-title": "BMC Med",
"key": "2505_CR5",
"unstructured": "Lin L-Y, Henderson AD, Carlile O, Dillingham I, Butler-Cole BF, Marks M, et al. Healthcare utilisation in people with long COVID: an OpenSAFELY cohort study. BMC Med. 2024;22(1):255. https://doi.org/10.1101/2023.12.21.23300305.",
"volume": "22",
"year": "2024"
},
{
"DOI": "10.1186/s12985-023-02061-8",
"author": "C Wang",
"doi-asserted-by": "publisher",
"first-page": "124",
"issue": "1",
"journal-title": "Virol J",
"key": "2505_CR6",
"unstructured": "Wang C, Ramasamy A, Verduzco-Gutierrez M, Brode WM, Melamed E. Acute and post-acute sequelae of SARS-CoV-2 infection: a review of risk factors and social determinants. Virol J. 2023;20(1):124. https://doi.org/10.1186/s12985-023-02061-8.",
"volume": "20",
"year": "2023"
},
{
"DOI": "10.1038/s41591-022-01840-0",
"author": "Z Al-Aly",
"doi-asserted-by": "publisher",
"first-page": "1461",
"issue": "7",
"journal-title": "Nat Med",
"key": "2505_CR7",
"unstructured": "Al-Aly Z, Bowe B, Xie Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat Med. 2022;28(7):1461–7. https://doi.org/10.1038/s41591-022-01840-0.",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1016/j.eclinm.2021.101019",
"author": "HE Davis",
"doi-asserted-by": "publisher",
"first-page": "101019",
"journal-title": "EClinicalMedicine",
"key": "2505_CR8",
"unstructured": "Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re’em Y, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 2021;38: 101019. https://doi.org/10.1016/j.eclinm.2021.101019.",
"volume": "38",
"year": "2021"
},
{
"DOI": "10.12688/f1000research.27287.2",
"author": "I Doykov",
"doi-asserted-by": "publisher",
"first-page": "1349",
"journal-title": "F1000Res",
"key": "2505_CR9",
"unstructured": "Doykov I, Hallqvist J, Gilmour KC, Grandjean L, Mills K, Heywood WE. ‘The long tail of Covid-19’ –The detection of a prolonged inflammatory response after a SARS-CoV-2 infection in asymptomatic and mildly affected patients. F1000Res. 2020;9:1349. https://doi.org/10.12688/f1000research.27287.2.",
"volume": "9",
"year": "2020"
},
{
"key": "2505_CR10",
"unstructured": "Centers for Disease Control. Management of post-COVID conditions. (2024). https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-management.html. Accessed March 19, 2024."
},
{
"DOI": "10.1136/bmj.m3026",
"author": "T Greenhalgh",
"doi-asserted-by": "publisher",
"journal-title": "BMJ",
"key": "2505_CR11",
"unstructured": "Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370: m3026. https://doi.org/10.1136/bmj.m3026.",
"volume": "370",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2349-y",
"author": "D Pinto",
"doi-asserted-by": "publisher",
"first-page": "290",
"issue": "7815",
"journal-title": "Nature",
"key": "2505_CR12",
"unstructured": "Pinto D, Park YJ, Beltramello M, Walls AC, Tortorici MA, Bianchi S, et al. Cross-neutralization of SARS-CoV-2 by a human monoclonal SARS-CoV antibody. Nature. 2020;583(7815):290–5. https://doi.org/10.1038/s41586-020-2349-y.",
"volume": "583",
"year": "2020"
},
{
"DOI": "10.1126/science.adc9127",
"author": "YJ Park",
"doi-asserted-by": "publisher",
"first-page": "619",
"issue": "6620",
"journal-title": "Science",
"key": "2505_CR13",
"unstructured": "Park YJ, Pinto D, Walls AC, Liu Z, De Marco A, Benigni F, et al. Imprinted antibody responses against SARS-CoV-2 Omicron sublineages. Science. 2022;378(6620):619–27. https://doi.org/10.1126/science.adc9127.",
"volume": "378",
"year": "2022"
},
{
"DOI": "10.1007/s15010-024-02245-6",
"author": "M Drysdale",
"doi-asserted-by": "publisher",
"first-page": "1839",
"issue": "(5)",
"journal-title": "Infection",
"key": "2505_CR14",
"unstructured": "Drysdale M, Berktas M, Gibbons DC, Rolland C, Lavoie L, Lloyd EJ. Real-world effectiveness of sotrovimab for the treatment of SARS-CoV-2 infection during Omicron BA.2 and BA.5 subvariant predominance: a systematic literature review. Infection. 2024. https://doi.org/10.1007/s15010-024-02245-6.",
"volume": "52",
"year": "2024"
},
{
"DOI": "10.1007/s15010-023-02098-5",
"author": "M Drysdale",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1",
"journal-title": "Infection",
"key": "2505_CR15",
"unstructured": "Drysdale M, Gibbons DC, Singh M, Rolland C, Lavoie L, Skingsley A, et al. Real-world effectiveness of sotrovimab for the treatment of SARS-CoV-2 infection during Omicron BA.2 subvariant predominance: a systematic literature review. Infection. 2024;52(1):1–17. https://doi.org/10.1007/s15010-023-02098-5.",
"volume": "52",
"year": "2024"
},
{
"key": "2505_CR16",
"unstructured": "N3C Dashboards. https://covid.cd2h.org/dashboard/. Accessed March 19, 2024."
},
{
"DOI": "10.1001/jamanetworkopen.2021.16901",
"author": "TD Bennett",
"doi-asserted-by": "publisher",
"issue": "7",
"journal-title": "JAMA Netw Open",
"key": "2505_CR17",
"unstructured": "Bennett TD, Moffitt RA, Hajagos JG, Amor B, Anand A, Bissell MM, et al. Clinical characterization and prediction of clinical severity of SARS-CoV-2 infection among US adults using data from the US National COVID Cohort Collaborative. JAMA Netw Open. 2021;4(7): e2116901. https://doi.org/10.1001/jamanetworkopen.2021.16901.",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1002/sim.3697",
"author": "PC Austin",
"doi-asserted-by": "publisher",
"first-page": "3083",
"issue": "25",
"journal-title": "Stat Med",
"key": "2505_CR18",
"unstructured": "Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–107. https://doi.org/10.1002/sim.3697.",
"volume": "28",
"year": "2009"
},
{
"DOI": "10.1136/bmjopen-2022-067611",
"author": "J Tannous",
"doi-asserted-by": "publisher",
"issue": "4",
"journal-title": "BMJ Open",
"key": "2505_CR19",
"unstructured": "Tannous J, Pan AP, Potter T, Bako AT, Dlouhy K, Drews A, et al. Real-world effectiveness of COVID-19 vaccines and anti-SARS-CoV-2 monoclonal antibodies against postacute sequelae of SARS-CoV-2: analysis of a COVID-19 observational registry for a diverse US metropolitan population. BMJ Open. 2023;13(4): e067611. https://doi.org/10.1136/bmjopen-2022-067611.",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1093/infdis/jiab490",
"author": "MJ Peluso",
"doi-asserted-by": "publisher",
"first-page": "1839",
"issue": "11",
"journal-title": "J Infect Dis",
"key": "2505_CR20",
"unstructured": "Peluso MJ, Lu S, Tang AF, Durstenfeld MS, Ho HE, Goldberg SA, et al. Markers of immune activation and inflammation in individuals with postacute sequelae of severe acute respiratory syndrome coronavirus 2 infection. J Infect Dis. 2021;224(11):1839–48. https://doi.org/10.1093/infdis/jiab490.",
"volume": "224",
"year": "2021"
},
{
"DOI": "10.1101/2021.08.08.21261763",
"author": "L Visvabharathy",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "2505_CR21",
"unstructured": "Visvabharathy L, Hanson BA, Orban ZS, Lim PH, Palacio NM, Jimenez M, et al. T cell responses to SARS-CoV-2 in people with and without neurologic symptoms of long COVID. medRxiv. 2022. https://doi.org/10.1101/2021.08.08.21261763.",
"year": "2022"
},
{
"DOI": "10.1038/s41586-021-03631-y",
"author": "EY Wang",
"doi-asserted-by": "publisher",
"first-page": "283",
"issue": "7866",
"journal-title": "Nature",
"key": "2505_CR22",
"unstructured": "Wang EY, Mao T, Klein J, Dai Y, Huck JD, Jaycox JR, et al. Diverse functional autoantibodies in patients with COVID-19. Nature. 2021;595(7866):283–8. https://doi.org/10.1038/s41586-021-03631-y.",
"volume": "595",
"year": "2021"
},
{
"DOI": "10.1002/jmv.29014",
"author": "Y Wang",
"doi-asserted-by": "publisher",
"first-page": "e29014",
"issue": "8",
"journal-title": "J Med Virol",
"key": "2505_CR23",
"unstructured": "Wang Y, Zhao D, Xiao W, Shi J, Chen W, Jia Q, et al. Paxlovid reduces the risk of Long COVID in patients six months after hospital discharge. J Med Virol. 2023;95(8): e29014. https://doi.org/10.1002/jmv.29014.",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.7326/M23-1394",
"author": "GN Ioannou",
"doi-asserted-by": "publisher",
"first-page": "1486",
"issue": "11",
"journal-title": "Ann Intern Med",
"key": "2505_CR24",
"unstructured": "Ioannou GN, Berry K, Rajeevan N, Li Y, Mutalik P, Yan L, et al. Effectiveness of nirmatrelvir-ritonavir against the development of post-COVID-19 conditions among U.S. veterans: a target trial emulation. Ann Intern Med. 2023;176(11):1486–97. https://doi.org/10.7326/M23-1394.",
"volume": "176",
"year": "2023"
},
{
"DOI": "10.1001/jamainternmed.2023.0743",
"author": "Y Xie",
"doi-asserted-by": "publisher",
"first-page": "554",
"issue": "6",
"journal-title": "JAMA Intern Med",
"key": "2505_CR25",
"unstructured": "Xie Y, Choi T, Al-Aly Z. Association of treatment with nirmatrelvir and the risk of post-COVID-19 condition. JAMA Intern Med. 2023;183(6):554–64. https://doi.org/10.1001/jamainternmed.2023.0743.",
"volume": "183",
"year": "2023"
},
{
"DOI": "10.1002/jmv.29333",
"author": "MS Durstenfeld",
"doi-asserted-by": "publisher",
"first-page": "e29333",
"issue": "1",
"journal-title": "J Med Virol",
"key": "2505_CR26",
"unstructured": "Durstenfeld MS, Peluso MJ, Lin F, Peyser ND, Isasi C, Carton TW, et al. Association of nirmatrelvir for acute SARS-CoV-2 infection with subsequent Long COVID symptoms in an observational cohort study. J Med Virol. 2024;96(1): e29333. https://doi.org/10.1002/jmv.29333.",
"volume": "96",
"year": "2024"
},
{
"DOI": "10.1001/jama.2023.8823",
"author": "T Thaweethai",
"doi-asserted-by": "publisher",
"first-page": "1934",
"issue": "22",
"journal-title": "JAMA",
"key": "2505_CR27",
"unstructured": "Thaweethai T, Jolley SE, Karlson EW, Levitan EB, Levy B, McComsey GA, et al. Development of a definition of postacute sequelae of SARS-CoV-2 infection. JAMA. 2023;329(22):1934–46. https://doi.org/10.1001/jama.2023.8823.",
"volume": "329",
"year": "2023"
},
{
"DOI": "10.1093/infdis/jiac136",
"author": "C Chen",
"doi-asserted-by": "publisher",
"first-page": "1593",
"issue": "9",
"journal-title": "J Infect Dis",
"key": "2505_CR28",
"unstructured": "Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: a meta-analysis and systematic review. J Infect Dis. 2022;226(9):1593–607. https://doi.org/10.1093/infdis/jiac136.",
"volume": "226",
"year": "2022"
},
{
"DOI": "10.1016/j.eclinm.2022.101762",
"author": "LL O'Mahoney",
"doi-asserted-by": "publisher",
"first-page": "101762",
"journal-title": "EClinicalMedicine",
"key": "2505_CR29",
"unstructured": "O’Mahoney LL, Routen A, Gillies C, Ekezie W, Welford A, Zhang A, et al. The prevalence and long-term health effects of Long Covid among hospitalised and non-hospitalised populations: a systematic review and meta-analysis. EClinicalMedicine. 2023;55: 101762. https://doi.org/10.1016/j.eclinm.2022.101762.",
"volume": "55",
"year": "2023"
},
{
"DOI": "10.1101/2022.08.15.22278603",
"author": "E Hill",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "2505_CR30",
"unstructured": "Hill E, Mehta H, Sharma S, Mane K, Xie C, Cathey E, et al. Risk factors associated with post-acute sequelae of SARS-CoV-2 in an EHR cohort: a National COVID Cohort Collaborative (N3C) analysis as part of the NIH RECOVER program. medRxiv. 2022. https://doi.org/10.1101/2022.08.15.22278603.",
"year": "2022"
},
{
"DOI": "10.1186/s12916-023-02737-6",
"author": "ER Pfaff",
"doi-asserted-by": "publisher",
"first-page": "58",
"issue": "1",
"journal-title": "BMC Med",
"key": "2505_CR31",
"unstructured": "Pfaff ER, Madlock-Brown C, Baratta JM, Bhatia A, Davis H, Girvin A, et al. Coding long COVID: characterizing a new disease through an ICD-10 lens. BMC Med. 2023;21(1):58. https://doi.org/10.1186/s12916-023-02737-6.",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.1056/NEJMc2216611",
"author": "J Walker",
"doi-asserted-by": "publisher",
"first-page": "e12",
"journal-title": "N Engl J Med",
"key": "2505_CR32",
"unstructured": "Walker J, Schnell G, Kerr W. Antiviral agents against Omicron subvariant BA.4.6 in vitro. N Engl J Med. 2023;388:e12. https://doi.org/10.1056/NEJMc2216611.",
"volume": "388",
"year": "2023"
},
{
"DOI": "10.1101/2021.03.09.434607",
"author": "AL Cathcart",
"doi-asserted-by": "publisher",
"journal-title": "bioRxiv",
"key": "2505_CR33",
"unstructured": "Cathcart AL, Havenar-Daughton C, Lempp FA, Ma D, Schmid MA, Agostini ML, et al. The dual function monoclonal antibodies VIR-7831 and VIR-7832 demonstrate potent in vitro and in vivo activity against SARS-CoV-2. bioRxiv. 2022. https://doi.org/10.1101/2021.03.09.434607.",
"year": "2022"
},
{
"DOI": "10.1038/s41467-022-31615-7",
"author": "JB Case",
"doi-asserted-by": "publisher",
"first-page": "3824",
"journal-title": "Nat Commun",
"key": "2505_CR34",
"unstructured": "Case JB, Mackin S, Errico JM, Chong Z, Madden EA, Whitener B, et al. Resilience of S309 and AZD7442 monoclonal antibody treatments against infection by SARS-CoV-2 Omicron lineage strains. Nat Commun. 2022;13:3824. https://doi.org/10.1038/s41467-022-31615-7.",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1038/s41586-022-04856-1",
"author": "R Uraki",
"doi-asserted-by": "publisher",
"first-page": "119",
"journal-title": "Nature",
"key": "2505_CR35",
"unstructured": "Uraki R, Kiso M, Iida S, Imai M, Takashita E, Kuroda M, et al. Characterization and antiviral susceptibility of SARS-CoV-2 Omicron BA.2. Nature. 2022;607:119–27. https://doi.org/10.1038/s41586-022-04856-1.",
"volume": "607",
"year": "2022"
},
{
"DOI": "10.1101/2023.01.17.523798",
"author": "A Addetia",
"doi-asserted-by": "publisher",
"journal-title": "bioRxiv",
"key": "2505_CR36",
"unstructured": "Addetia A, Piccoli L, Case JB, Park Y-J, Beltramello M, Guarino B, et al. Therapeutic and vaccine-induced cross-reactive antibodies with effector function against emerging Omicron variants. bioRxiv. 2023. https://doi.org/10.1101/2023.01.17.523798.",
"year": "2023"
},
{
"DOI": "10.1007/s40121-022-00755-0",
"author": "MM Cheng",
"doi-asserted-by": "publisher",
"first-page": "607",
"journal-title": "Infect Dis Ther",
"key": "2505_CR37",
"unstructured": "Cheng MM, Reyes C, Satram S, Birch H, Gibbons DC, Drysdale M, et al. Real-world effectiveness of sotrovimab for the early treatment of COVID-19 during SARS-CoV-2 Delta and Omicron waves in the USA. Infect Dis Ther. 2023;12:607–21. https://doi.org/10.1007/s40121-022-00755-0.",
"volume": "12",
"year": "2023"
},
{
"DOI": "10.1093/infdis/jiac206",
"author": "NR Aggarwal",
"doi-asserted-by": "publisher",
"first-page": "2129",
"journal-title": "J Infect Dis",
"key": "2505_CR38",
"unstructured": "Aggarwal NR, Beaty LE, Bennett TD, Carlson NE, Davis CB, Kwan BM, et al. Real-world evidence of the neutralizing monoclonal antibody sotrovimab for preventing hospitalization and mortality in COVID-19 outpatients. J Infect Dis. 2022;226:2129–36. https://doi.org/10.1093/infdis/jiac206.",
"volume": "226",
"year": "2022"
},
{
"DOI": "10.1101/2023.05.12.23289914",
"author": "J Tazare",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "2505_CR39",
"unstructured": "Tazare J, Nab L, Zheng B, Hulme WJ, Green ACA, The Open Safely Collaborative, et al. Effectiveness of sotrovimab and molnupiravir in community settings in England across the Omicron BA.1 and BA.2 sublineages: emulated target trials using the OpenSAFELY platform. medRxiv. 2023. https://doi.org/10.1101/2023.05.12.23289914.",
"year": "2023"
},
{
"DOI": "10.1080/03007995.2024.2376144",
"author": "V Patel",
"doi-asserted-by": "publisher",
"first-page": "1323",
"journal-title": "Curr Med Res Opin",
"key": "2505_CR40",
"unstructured": "Patel V, Yarwood MJ, Levick B, Gibbons DC, Drysdale M, Kerr W, et al. Characteristics and outcomes of patients with COVID-19 at high-risk of disease progression receiving sotrovimab, oral antivirals or no treatment in England. Curr Med Res Opin. 2024;40:1323–34. https://doi.org/10.1080/03007995.2024.2376144.",
"volume": "40",
"year": "2024"
},
{
"DOI": "10.1186/s12879-024-09311-2",
"author": "V Patel",
"doi-asserted-by": "publisher",
"first-page": "428",
"journal-title": "BMC Infect Dis",
"key": "2505_CR41",
"unstructured": "Patel V, Levick B, Boult S, Gibbons DC, Drysdale M, Lloyd EJ, et al. Characteristics and outcomes of COVID-19 patients presumed to be treated with sotrovimab in NHS hospitals in England. BMC Infect Dis. 2024;24:428. https://doi.org/10.1186/s12879-024-09311-2.",
"volume": "24",
"year": "2024"
},
{
"DOI": "10.1101/2023.01.20.23284849",
"author": "B Zheng",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "2505_CR42",
"unstructured": "Zheng B, Tazare J, Nab L, Mehrkar M, MacKenna B, Goldacre B, et al. Comparative effectiveness of paxlovid versus sotrovimab and molnupiravir for preventing severe COVID-19 outcomes in non-hospitalised patients: observational cohort study using the OpenSAFELY platform. medRxiv. 2023. https://doi.org/10.1101/2023.01.20.23284849.",
"year": "2023"
},
{
"DOI": "10.1136/bmj-2022-071932",
"author": "B Zheng",
"doi-asserted-by": "publisher",
"journal-title": "BMJ",
"key": "2505_CR43",
"unstructured": "Zheng B, Green ACA, Tazare J, et al. Comparative effectiveness of sotrovimab and molnupiravir for prevention of severe covid-19 outcomes in patients in the community: observational cohort study with the OpenSAFELY platform. BMJ. 2022;379: e071932. https://doi.org/10.1136/bmj-2022-071932.",
"volume": "379",
"year": "2022"
}
],
"reference-count": 43,
"references-count": 43,
"relation": {},
"resource": {
"primary": {
"URL": "https://link.springer.com/10.1007/s15010-025-02505-z"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Impact of treatment of COVID-19 with sotrovimab on post-acute sequelae of COVID-19 (PASC): an analysis of National COVID Cohort Collaborative (N3C) data",
"type": "journal-article",
"update-policy": "https://doi.org/10.1007/springer_crossmark_policy"
}
