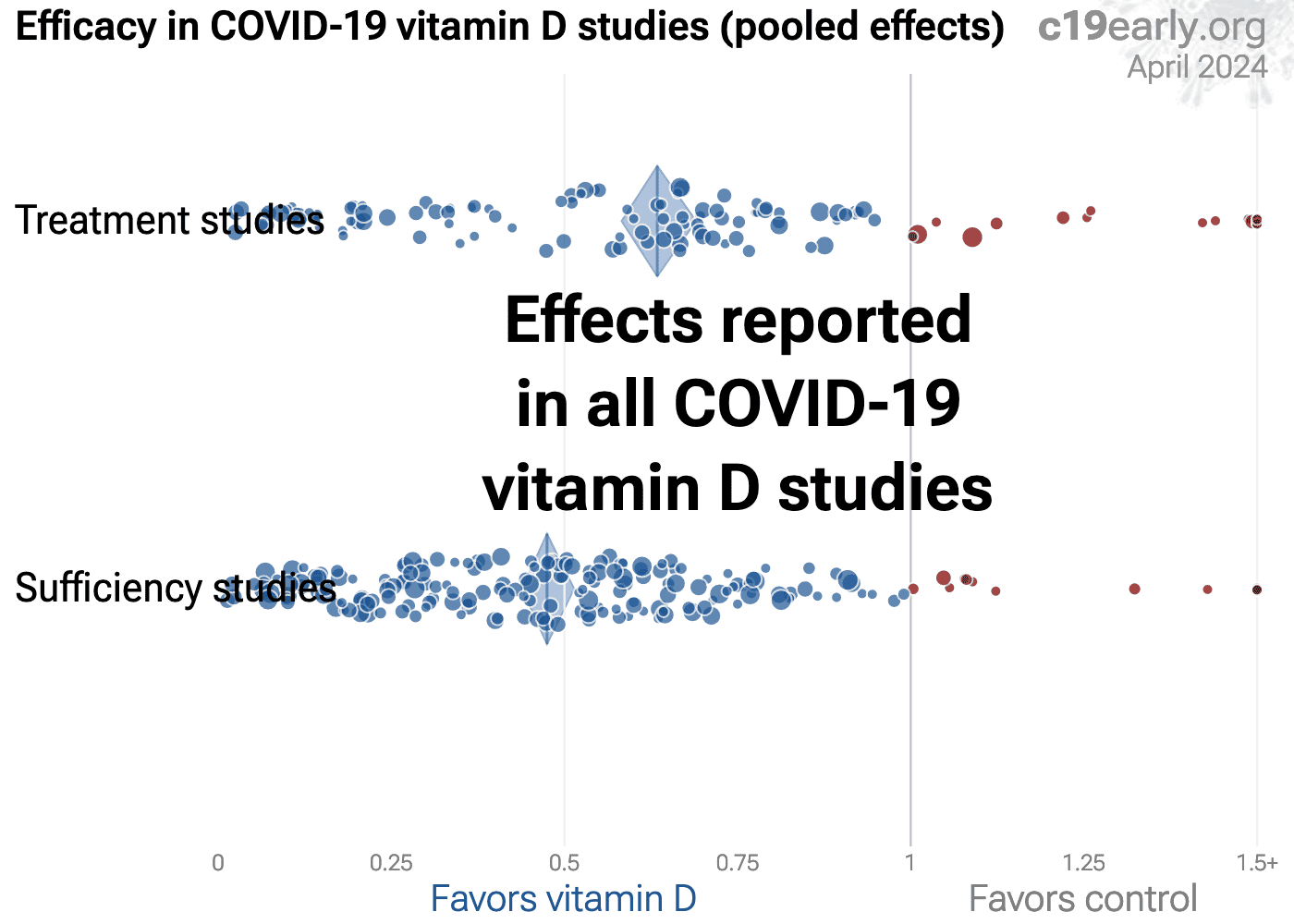
Vitamin D reduces COVID-19 risk: real-time meta analysis of 362 studies (136 treatment studies and 226 sufficiency studies)
, Dec 2025
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,300+ studies for
210+ treatments. c19early.org
|
136 treatment studies show statistically significant lower risk for mortality, ICU admission, hospitalization, and cases.
73 studies from 68 independent teams in 25 countries show significantly lower risk.
Meta analysis using the most serious outcome reported shows 56% [37‑70%] and 38% [33‑43%] lower risk for early treatment and for all studies. Results are similar for higher quality studies, peer-reviewed studies, and mortality: early treatment - 63% [40‑77%], 53% [34‑67%], 62% [35‑77%]; all - 39% [33‑44%], 42% [37‑47%], 39% [31‑45%].
Late stage treatment with calcitriol/calcifediol and analogs is more effective than cholecalciferol: 66% [47‑78%] vs. 44% [33‑53%].
Ongoing treatment with multiple doses is more effective than single bolus doses: 60% [50‑68%] vs. 22% [1‑38%]
Control Vitamin D
226 sufficiency studies show a strong association between vitamin D sufficiency and outcomes, with 50% [47‑53%] lower risk for higher levels.
No treatment is 100% effective. Protocols combine safe and effective options with individual risk/benefit analysis and monitoring. Other treatments are more effective. Sunlight or dietary sources may be preferred.
The quality of non-prescription supplements varies widely1-3.
All data and sources to reproduce this analysis are in the appendix.
20 other meta analyses show significant improvements with vitamin D treatment for mortality4-17, mechanical ventilation4,8,9,14,18-20, ICU admission4,6,8,9,12,14,16,18-22, hospitalization14, severity5,7,8,13,23, and cases10,22,23.
20 meta analyses show significant improvements with vitamin D treatment for mortality1-14,
mechanical ventilation1,5,6,11,15-17 ,
ICU admission1,3,5,6,9,11,13,15-19 ,
hospitalization11,
severity2,4,5,10,20 , and
cases7,19,20 .
1.
Shah et al., Does vitamin D supplementation reduce COVID-19 severity? - a systematic review, QJM: An International Journal of Medicine, doi:10.1093/qjmed/hcac040.
2.
Nikniaz et al., The impact of vitamin D supplementation on mortality rate and clinical outcomes of COVID-19 patients: A systematic review and meta-analysis, Pharmaceutical Sciences, doi:10.34172/PS.2021.13.
3.
Hosseini et al., Effects of Vitamin D Supplementation on COVID-19 Related Outcomes: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu14102134.
4.
D’Ecclesiis et al., Vitamin D and SARS-CoV2 infection, severity and mortality: A systematic review and meta-analysis, PLOS ONE, doi:10.1371/journal.pone.0268396.
5.
Xie et al., Micronutrient perspective on COVID-19: Umbrella review and reanalysis of meta-analyses, Critical Reviews in Food Science and Nutrition, doi:10.1080/10408398.2023.2174948.
6.
Hariyanto et al., Vitamin D supplementation and Covid‐19 outcomes: A systematic review, meta‐analysis and meta‐regression, Reviews in Medical Virology, doi:10.1002/rmv.2269.
7.
Begum et al., The Role of Vitamin D in COVID-19 Survival and Prevention: A Meta-analysis, Sudan Journal of Medical Sciences, doi:10.18502/sjms.v19i1.15776.
8.
Jamilian et al., The role of vitamin D in outcomes of critical care in COVID-19 patients: Evidence from an umbrella meta-analysis of interventional and observational studies, Public Health Nutrition, doi:10.1017/S1368980024000934.
9.
Sobczak et al., Effect of Vitamin D3 Supplementation on Severe COVID-19: A Meta-Analysis of Randomized Clinical Trials, Nutrients, doi:10.3390/nu16101402.
10.
Petrelli et al., Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2021.105883.
11.
Asla et al., Vitamin D on COVID-19 Patients During the Pandemic, 2022. A Systematic Review and Meta-Analysis, Current Research in Nutrition and Food Science Journal, doi:10.12944/CRNFSJ.11.1.3.
12.
Kow et al., The impact of vitamin D administration on mortality in COVID-19 patients: a systematic review and meta-analysis of randomized controlled trials, Inflammopharmacology, doi:10.1007/s10787-024-01564-2.
13.
Zhang et al., The impact of supplementing vitamin D through different methods on the prognosis of COVID-19 patients: a systematic review and meta-analysis, Frontiers in Nutrition, doi:10.3389/fnut.2024.1441847.
14.
Doustmohammadian et al., Impact of vitamin D supplementation on COVID-19 mortality: A systematic review and meta-analysis, Nutrition Clinique et Métabolisme, doi:10.1016/j.nupar.2025.12.001.
15.
Meng et al., The role of vitamin D in the prevention and treatment of SARS-CoV-2 infection: A meta-analysis of randomized controlled trials, Clinical Nutrition, doi:10.1016/j.clnu.2023.09.008.
16.
Yang et al., Therapeutic effects of vitamin D supplementation on COVID-19 aggravation: a systematic review and meta-analysis of randomized controlled trials, Frontiers in Pharmacology, doi:10.3389/fphar.2024.1367686.
17.
Szarpak et al., Vitamin D supplementation to treat SARS-CoV-2 positive patients. Evidence from meta-analysis, Cardiology Journal, doi:10.5603/CJ.a2021.0122.
18.
Tentolouris et al., The effect of vitamin D supplementation on mortality and intensive care unit admission of COVID-19 patients. A systematic review, meta-analysis and meta-regression, Diabetes/Metabolism Research and Reviews, doi:10.1002/dmrr.3517.
