Effects of Antiseptic Formulations on Oral Microbiota and Related Systemic Diseases: A Scoping Review
et al., Antibiotics, doi:10.3390/antibiotics14080815, Aug 2025
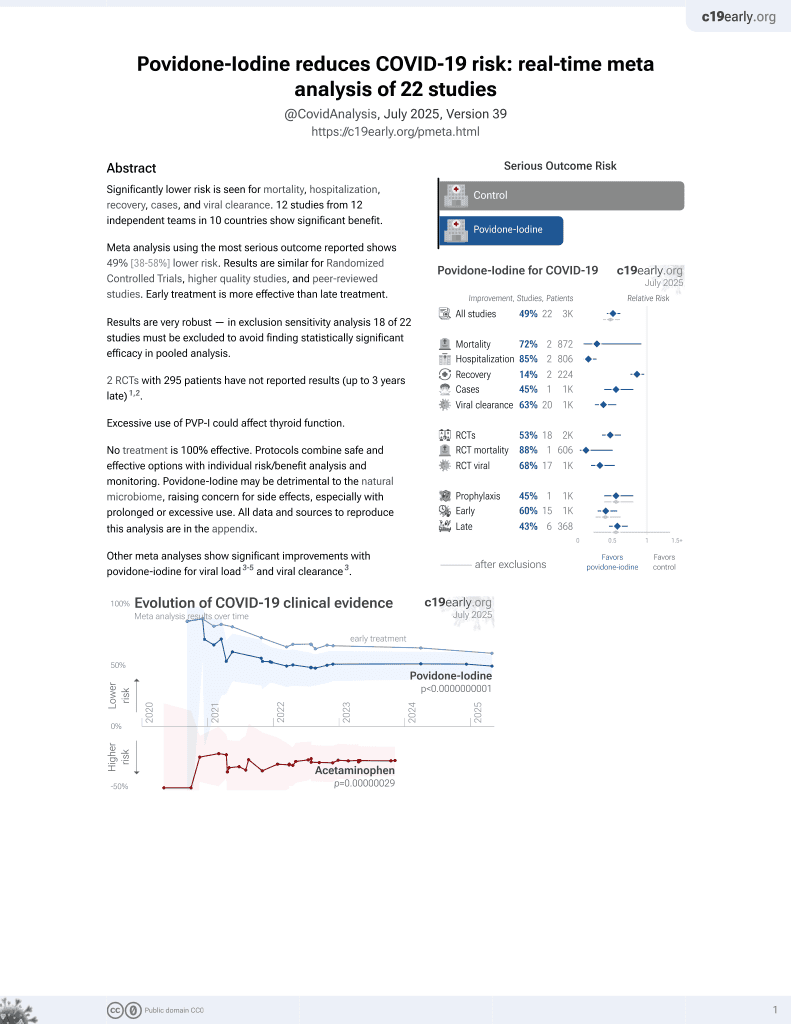
PVP-I for COVID-19
15th treatment shown to reduce risk in
February 2021, now with p = 0.000000000016 from 22 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
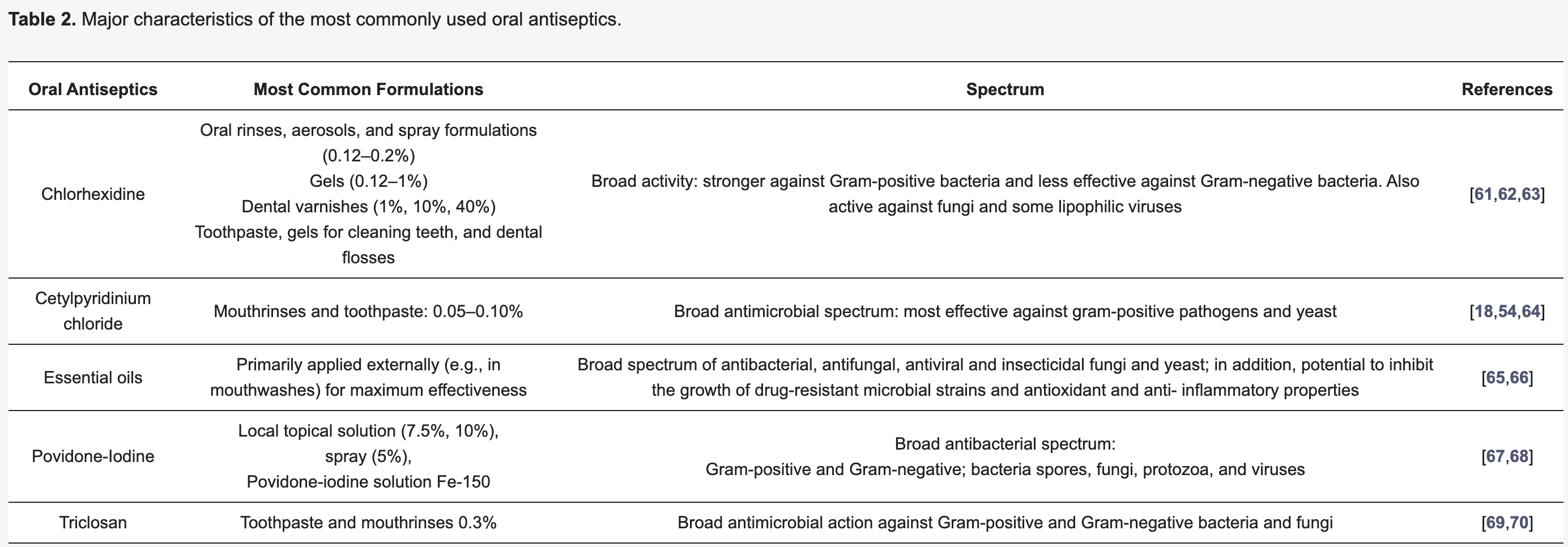
Review of oral antiseptic formulations and their effects on oral microbiota and systemic diseases. While antiseptics like chlorhexidine, essential oils, povidone-iodine, and cetylpyridinium chloride can effectively reduce pathogenic oral microorganisms and improve periodontal health, they may also disrupt beneficial commensal bacteria, potentially leading to oral dysbiosis.
Review covers chlorhexidine, cetylpyridinium chloride, and povidone-iodine.
1.
Angjelova et al., Effects of Antiseptic Formulations on Oral Microbiota and Related Systemic Diseases: A Scoping Review, Antibiotics, doi:10.3390/antibiotics14080815.
2.
Thangamani et al., Rinsing away the threat: Antiviral mouthwashes and their efficacy, World Academy of Sciences Journal, doi:10.3892/wasj.2025.366.
3.
Gunawan et al., The Role of Poly Vinyl Pyrrolidone Iodine (PVP-I) in Preventing Cross-Infection during Dental Procedures: A Systematic Review in the COVID-19 Context, Journal of International Society of Preventive and Community Dentistry, doi:10.4103/jispcd.jispcd_78_24.
4.
Okeke et al., Antiseptics: An expeditious third force in the prevention and management of coronavirus diseases, Current Research in Microbial Sciences, doi:10.1016/j.crmicr.2024.100293.
5.
Gandhi et al., Washing Illness Away: A Systematic Review of the Impact of Nasal Irrigation and Spray on COVID‐19, The Laryngoscope, doi:10.1002/lary.31761.
6.
Brito-Reia et al., Antiviral Mechanism and Clinical Benefits of Mouthwash Active Against SARS-CoV-2, Current Oral Health Reports, doi:10.1007/s40496-024-00368-1.
7.
Donzelli, A., Neglected Effective Early Therapies against COVID-19: Focus on Functional Foods and Related Active Substances. A Review, MDPI AG, doi:10.20944/preprints202312.1178.v1.
8.
Chavda et al., Nasal sprays for treating COVID-19: a scientific note, Pharmacological Reports, doi:10.1007/s43440-023-00463-7.
9.
Ting et al., The In Vitro Virucidal Effects of Mouthwashes on SARS-CoV-2, International Journal of Translational Medicine, doi:10.3390/ijtm2030030.
10.
Lim et al., Repurposing povidone-iodine to reduce the risk of SARS-CoV-2 infection and transmission: a narrative review, Annals of Medicine, doi:10.1080/07853890.2022.2076902.
Angjelova et al., 8 Aug 2025, Italy, peer-reviewed, 5 authors.
Contact: alessandro.polizzi@phd.unict.it (corresponding author), angela.angjelova@students.stomfak.ukim.mk, elena.jovanova@students.stomfak.ukim.mk, rleonard@unict.it, gaetano.isola@unict.it.
Effects of Antiseptic Formulations on Oral Microbiota and Related Systemic Diseases: A Scoping Review
Antibiotics, doi:10.3390/antibiotics14080815
Background: Oral antiseptic formulations are widely used as adjuncts in oral hygiene to reduce pathogenic microorganisms and prevent oral diseases. While these agents are effective in controlling biofilm, their broader effects may disrupt the oral microbiota's balance, potentially contributing to systemic health implications. The complex relationship between antiseptic use, microbial composition, and systemic outcomes remains insufficiently mapped. Objective: This scoping review aimed to explore and map the current evidence regarding the impact of antiseptic formulations on oral microbiota composition and to examine their potential associations with systemic diseases. Methods: A comprehensive literature search was performed using PubMed, Scopus, and Web of Science up to June 2025. Studies were included if they investigated antiseptic formulations commonly used in oral healthcare-such as chlorhexidine, essential oils, and cetylpyridinium chloride-and reported effects on oral microbiota and/or systemic health. Eligible study types included human clinical trials, observational studies, in vitro, and animal studies. Two reviewers independently screened and selected studies, with disagreements resolved by consensus. Data extraction focused on study design, antiseptic agents, microbial outcomes, and systemic implications. A total of 12 studies were included and charted. Results: The included studies demonstrated that oral antiseptics effectively reduce pathogenic microorganisms and improve clinical outcomes in oral diseases such as gingivitis and periodontitis. However, several studies also reported alterations in commensal microbial communities, suggesting a potential for dysbiosis. Some studies indicated possible links between antiseptic-induced microbial changes and systemic conditions, including cardiovascular and respiratory diseases. Conclusions: The evidence highlights a dual effect of antiseptic formulations: while beneficial in controlling oral pathogens, they may disrupt microbial homeostasis with possible systemic consequences. Further research is needed to evaluate long-term effects and develop targeted, microbiota-preserving oral hygiene strategies.
Author Contributions: Conceptualization, G.I.; methodology, A.A., E.J. and A.P.; validation, A.P. and R.L.; formal analysis, R.L. and G.I.; investigation, A.A. and E.J.; resources, A.P., R.L. and G.I.; data curation, A.A., E.J. and A.P.; writing-original draft preparation, A.A.; writing-review and editing, A.A. and A.P.; visualization, R.L.; supervision, R.L. and G.I. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest: The authors declare no conflicts of interest.
References
Abdelrahman, El Samak, El-Baz, Hanora, Satyal et al., Effects of Mint Oils on the Human Oral Microbiome: A Pilot Study, Microorganisms, doi:10.3390/microorganisms12081538
Abusleme, Dupuy, Dutzan, Silva, Burleson et al., The subgingival microbiome in health and periodontitis and its relationship with community biomass and inflammation, ISME J, doi:10.1038/ismej.2012.174
Aceves Argemí, González Navarro, Ochoa García-Seisdedos, Estrugo Devesa, López-López, Mouthwash With Alcohol and Oral Carcinogenesis: Systematic Review and Meta-analysis, J. Evid. Based Dent. Pract, doi:10.1016/j.jebdp.2020.101407
Ahrens, Pohlabeln, Foraita, Nelis, Lagiou et al., Oral health, dental care and mouthwash associated with upper aerodigestive tract cancer risk in Europe: The ARCAGE study, Oral Oncol, doi:10.1016/j.oraloncology.2014.03.001
Ali, Oral Microbiome and Adverse Pregnancy Outcomes: An Update, Online J. Health Allied Sci
Alrashdan, Leao, Doble, Mccullough, Porter, The Effects of Antimicrobial Mouthwashes on Systemic Disease: What Is the Evidence?, Int. Dent. J, doi:10.1016/j.identj.2023.08.012
Andres, Giraud, Gerente, Le Cloirec, Antibacterial Effects of Chitosan Powder: Mechanisms of Action, Environ. Technol, doi:10.1080/09593332808618893
Baker, Mark Welch, Kauffman, Mclean, He, The oral microbiome: Diversity, biogeography and human health, Nat. Rev. Microbiol, doi:10.1038/s41579-023-00963-6
Baker, Morton, Dinis, Alvarez, Tran et al., Deep metagenomics examines the oral microbiome during dental caries, revealing novel taxa and co-occurrences with host molecules, Genome Res, doi:10.1101/gr.265645.120
Bakkali, Averbeck, Averbeck, Idaomar, Biological effects of essential oils-A review, Food Chem. Toxicol, doi:10.1016/j.fct.2007.09.106
Barkvoll, Rølla, Svendsen, Interaction between chlorhexidine digluconate and sodium lauryl sulfate in vivo, J. Clin. Periodontol, doi:10.1111/j.1600-051X.1989.tb02143.x
Bartsch, Kohnert, Kreutz, Woelber, Anderson et al., Chlorhexidine digluconate mouthwash alters the oral microbial composition and affects the prevalence of antimicrobial resistance genes, Front. Microbiol, doi:10.3389/fmicb.2024.1429692
Basic, Dahlén, Microbial metabolites in the pathogenesis of periodontal diseases: A narrative review, Front. Oral Health, doi:10.3389/froh.2023.1210200
Belibasakis, Bostanci, Marsh, Zaura, Applications of the oral microbiome in personalized dentistry, Arch. Oral Biol, doi:10.1016/j.archoralbio.2019.05.023
Berezovska, Meiller, Marinesco, Nedellec, Giroud et al., Chlorhexidine digluconate exerts bactericidal activity vs Gram positive Staphylococci with bioelectrocatalytic compatibility: High level disinfection for implantable biofuel cells, Bioelectrochemistry, doi:10.1016/j.bioelechem.2023.108435
Bertolini, Ranjan, Thompson, Diaz, Sobue et al., Candida albicans induces mucosal bacterial dysbiosis that promotes invasive infection, PLoS Pathog, doi:10.1371/journal.ppat.1007717
Bondonno, Liu, Croft, Considine, Puddey et al., Antibacterial Mouthwash Blunts Oral Nitrate Reduction and Increases Blood Pressure in Treated Hypertensive Men and Women, Am. J. Hypertens, doi:10.1093/ajh/hpu192
Bostanci, Belibasakis, Precision periodontal care: From omics discoveries to chairside diagnostics, Clin. Oral. Investig, doi:10.1007/s00784-023-04878-7
Boulares, Jdidi, Bragazzi, Impact of Mouthwash-Induced Oral Microbiome Disruption on Alzheimer's Disease Risk: A Perspective Review, Int. Dent. J, doi:10.1016/j.identj.2024.07.005
Brookes, Teoh, Cieplik, Kumar, Mouthwash Effects on the Oral Microbiome: Are They Good, Bad, or Balanced?, Int. Dent. J, doi:10.1016/j.identj.2023.08.010
Bryan, Tribble, Angelov, Oral Microbiome and Nitric Oxide: The Missing Link in the Management of Blood Pressure, Curr. Hypertens. Rep, doi:10.1007/s11906-017-0725-2
Chatzigiannidou, Teughels, Van De Wiele, Boon, Oral biofilms exposure to chlorhexidine results in altered microbial composition and metabolic profile, npj Biofilms Microbiomes, doi:10.1038/s41522-020-0124-3
Chen, Joshipura, Habash, Lopez-Candales, Dentists and physicians' practices meet once again: Potential unfavorable clinical effects of frequent mouthwash use, Postgrad. Med, doi:10.1080/00325481.2020.1829854
Chouhan, Sharma, Guleria, Antimicrobial Activity of Some Essential Oils-Present Status and Future Perspectives, Medicines, doi:10.3390/medicines4030058
Ciancio, Mouthwashes: Rationale for use, Am. J. Dent
Costalonga, Herzberg, The oral microbiome and the immunobiology of periodontal disease and caries, Immunol. Lett, doi:10.1016/j.imlet.2014.08.017
Cousido, Tomás Carmona, García-Caballero, Limeres, Álvarez et al., In vivo substantivity of 0.12% and 0.2% chlorhexidine mouthrinses on salivary bacteria, Clin. Oral Investig, doi:10.1007/s00784-009-0320-2
Cui, Wang, Gao, Microbial dysbiosis in periodontitis and peri-implantitis: Pathogenesis, immune responses, and therapeutic, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2025.1517154
Czajkowski, Jafra, Quenching of acyl-homoserine lactone-dependent quorum sensing by enzymatic disruption of signal molecules, Acta Biochim. Pol, doi:10.18388/abp.2009_2512
Dabdoub, Ganesan, Kumar, Comparative metagenomics reveals taxonomically idiosyncratic yet functionally congruent communities in periodontitis, Sci. Rep, doi:10.1038/srep38993
Darveau, Tanner, Page, The microbial challenge in periodontitis, Periodontol, doi:10.1111/j.1600-0757.1997.tb00190.x
Dehghani, Abtahi, Hasanzadeh, Farahzad, Noori et al., Effect of Propolis mouthwash on plaque and gingival indices over fixed orthodontic patients, J. Clin. Exp. Dent, doi:10.4317/jced.55026
Deo, Deshmukh, Oral microbiome: Unveiling the fundamentals, J. Oral Maxillofac. Pathol, doi:10.4103/jomfp.JOMFP_304_18
Divaris, Moss, Beck, Biologically informed stratification of periodontal disease holds the key to achieving precision oral health, J. Periodontol, doi:10.1002/JPER.20-0096
Do Amaral, Hassan, Sloniak, Pannuti, Romito et al., Effects of antimicrobial mouthwashes on the human oral microbiome: Systematic review of controlled clinical trials, Int. J. Dent. Hyg, doi:10.1111/idh.12617
Donohoe, Garge, Zhang, Sun, O'connell et al., The Microbiome and Butyrate Regulate Energy Metabolism and Autophagy in the Mammalian Colon, Cell Metab, doi:10.1016/j.cmet.2011.02.018
Duane, Yap, Neelakantan, Anthonappa, Bescos et al., Mouthwashes: Alternatives and Future Directions, Int. Dent. J, doi:10.1016/j.identj.2023.08.011
Eggers, Infectious Disease Management and Control with Povidone Iodine, Infect. Dis. Ther, doi:10.1007/s40121-019-00260-x
Eley, Antibacterial agents in the control of supragingival plaque-A review, Br. Dent. J, doi:10.1038/sj.bdj.4800090
Ellepola, Chandy, Khan, In vitro Impact of Limited Exposure to Subtherapeutic Concentrations of Chlorhexidine Gluconate on the Adhesion-Associated Attributes of Oral Candida Species, Med. Princ. Pract, doi:10.1159/000445688
Etemadi, Barhaghi, Leylabadlo, Memar, Mohammadi et al., The synergistic effect of turmeric aqueous extract and chitosan against multidrug-resistant bacteria, New Microbes New Infect, doi:10.1016/j.nmni.2021.100861
Francisqueti-Ferron, Nakandakare-Maia, Siqueira, Ferron, Vieira et al., The role of gut dysbiosis-associated inflammation in heart failure, Rev. Assoc. Med. Bras, doi:10.1590/1806-9282.20220197
Fuse, Ito, Yamaguchi, Tsukada, High Ingestion Rate of Iodine from Povidone-Iodine Mouthwash, Biol. Trace Elem. Res, doi:10.1007/s12011-021-02978-7
Galimanas, Hall, Singh, Lynch, Goldberg et al., Bacterial community composition of chronic periodontitis and novel oral sampling sites for detecting disease indicators, Microbiome, doi:10.1186/2049-2618-2-32
Garrido, Lyra, Rodrigues, Viana, Mendes et al., Revisiting Oral Antiseptics, Microorganism Targets and Effectiveness, J. Pers. Med, doi:10.3390/jpm13091332
Gerba, Quaternary Ammonium Biocides: Efficacy in Application, Appl. Environ. Microbiol, doi:10.1128/AEM.02633-14
Gheisary, Mahmood, Harri Shivanantham, Liu, Lieffers et al., The Clinical, Microbiological, and Immunological Effects of Probiotic Supplementation on Prevention and Treatment of Periodontal Diseases: A Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu14051036
Giannelli, Chellini, Margheri, Tonelli, Tani, Effect of chlorhexidine digluconate on different cell types: A molecular and ultrastructural investigation, Toxicol. Vitr, doi:10.1016/j.tiv.2007.09.012
Guo, Joshipura, Ricart, Patel, Gower et al., Association of over-the-counter mouthwash use with markers of nitric oxide metabolism, inflammation, and endothelial function-A cross-sectional study, Front. Oral Health, doi:10.3389/froh.2025.1488286
Gusberti, Sampathkumar, Siegrist, Lang, Microbiological and clinical effects of chlorhexidine digluconate and hydrogen peroxide mouthrinses on developing plaque and gingivitis, J. Clin. Periodontol, doi:10.1111/j.1600-051X.1988.tb01556.x
Ha, Oh, Yang, Jun, Jin et al., Oral Health Behaviors, Periodontal Disease, and Pathogens in Preeclampsia: A Case-Control Study in Korea, J. Periodontol, doi:10.1902/jop.2011.110035
Halboub, Al-Maweri, Al-Wesabi, Al-Kamel, Shamala et al., Efficacy of propolis-based mouthwashes on dental plaque and gingival inflammation: A systematic review, BMC Oral Health, doi:10.1186/s12903-020-01185-5
Han, Wang, Mobile Microbiome, J. Dent. Res, doi:10.1177/0022034513487559
Haran, Bradley, Zeamer, Cincotta, Salive et al., Inflammation-type dysbiosis of the oral microbiome associates with the duration of COVID-19 symptoms and long COVID, JCI Insight, doi:10.1172/jci.insight.152346
Haydari, Bardakci, Koldsland, Aass, Sandvik et al., Comparing the effect of 0.06% -, 0.12% and 0.2% Chlorhexidine on plaque, bleeding and side effects in an experimental gingivitis model: A parallel group, double masked randomized clinical trial, BMC Oral Health, doi:10.1186/s12903-017-0400-7
Hemmingsen, Škalko-Basnet, Jøraholmen, The Expanded Role of Chitosan in Localized Antimicrobial Therapy, Mar. Drugs, doi:10.3390/md19120697
Herrera, Matesanz, Martín, Oud, Feres et al., Adjunctive effect of locally delivered antimicrobials in periodontitis therapy: A systematic review and meta-analysis, J. Clin. Periodontol, doi:10.1111/jcpe.13230
Hetta, Ramadan, Rashed, Alharbi, Alsharef et al., Quorum Sensing Inhibitors: An Alternative Strategy to Win the Battle against Multidrug-Resistant (MDR) Bacteria, Molecules, doi:10.3390/molecules29153466
Holmes, Villa, Durand, Jiang, Dallow et al., Microbiota responses to different prebiotics are conserved within individuals and associated with habitual fiber intake, Microbiome, doi:10.1186/s40168-022-01307-x
Homayouni Rad, Pourjafar, Mirzakhani, A comprehensive review of the application of probiotics and postbiotics in oral health, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2023.1120995
Hu, Li, Sreenivasan, Devizio, A randomized, double-blind clinical study to assess the antimicrobial effects of a cetylpyridinium chloride mouth rinse on dental plaque bacteria, Clin. Ther, doi:10.1016/j.clinthera.2009.11.004
Huyck, The Effect of Cetylpyridinium Chloride on the Bacterial Growth in the Oral Cavity, J. Am. Pharm. Assoc. (Sci. ed, doi:10.1002/jps.3030340103
Inchingolo, Inchingolo, Malcangi, De Leonardis, Sardano et al., The Benefits of Probiotics on Oral Health: Systematic Review of the Literature, Pharmaceuticals, doi:10.3390/ph16091313
Jastrz Ąb, Graczyk, Siedlecki, Molecular and Cellular Mechanisms Influenced by Postbiotics, Int. J. Mol. Sci, doi:10.3390/ijms222413475
Jia, Zhi, Lai, Wang, Xia et al., The oral microbiota-A mechanistic role for systemic diseases, Br. Dent. J, doi:10.1038/sj.bdj.2018.217
Joshipura, Muñoz-Torres, Fernández-Santiago, Patel, Lopez-Candales, Over-the-counter mouthwash use, nitric oxide and hypertension risk, doi:10.1080/08037051.2019.1680270
Joshipura, Muñoz-Torres, Morou-Bermudez, Patel, Over-the-counter mouthwash use and risk of prediabetes/diabetes, Nitric Oxide, doi:10.1016/j.niox.2017.09.004
Kanagalingam, Feliciano, Hah, Labib, Le et al., Practical use of povidone-iodine antiseptic in the maintenance of oral health and in the prevention and treatment of common oropharyngeal infections, Int. J. Clin. Pract, doi:10.1111/ijcp.12707
Kannosh, Staletovic, Toljic, Radunovic, Pucar et al., The presence of periopathogenic bacteria in subgingival and atherosclerotic plaques-An age related comparative analysis, J. Infect. Dev. Ctries, doi:10.3855/jidc.10980
Karbach, Ebenezer, Warnke, Behrens, Al-Nawas, Antimicrobial effect of Australian antibacterial essential oils as alternative to common antiseptic solutions against clinically relevant oral pathogens, Clin. Lab, doi:10.7754/Clin.Lab.2014.140714
Kaur, Kumar, Importance of Chlorhexidine in Maintaining Periodontal Health, Int. J. Dent. Res, doi:10.31254/dentistry.2016.1107
Kelly, El Karim, Periodontitis May Be Associated With Respiratory Diseases Such as Asthma, COPD, and Pneumonia, J. Evid. Based Dent. Pract, doi:10.1016/j.jebdp.2020.101498
Kilian, Chapple, Hannig, Marsh, Meuric et al., The oral microbiome-An update for oral healthcare professionals, Br. Dent. J, doi:10.1038/sj.bdj.2016.865
Kolahi, Soolari, Rinsing with chlorhexidine gluconate solution after brushing and flossing teeth: A systematic review of effectiveness, Quintessence Int
Koren, Spor, Felin, Fåk, Stombaugh et al., Human oral, gut, and plaque microbiota in patients with atherosclerosis, Proc. Natl. Acad. Sci, doi:10.1073/pnas.1011383107
Kozak, Pawlik, The Role of the Oral Microbiome in the Development of Diseases, Int. J. Mol. Sci, doi:10.3390/ijms24065231
Lee, Chen, Yang, Liang, Peng et al., Bacterial alterations in salivary microbiota and their association in oral cancer, Sci. Rep, doi:10.1038/s41598-017-16418-x
Leonov, Varaeva, Livantsova, Starodubova, The Complicated Relationship of Short-Chain Fatty Acids and Oral Microbiome: A Narrative Review, Biomedicines, doi:10.3390/biomedicines11102749
Li, Liu, Yang, Li, Song, The Oral Microbiota: Community Composition, Influencing Factors, Pathogenesis, and Interventions, Front. Microbiol, doi:10.3389/fmicb.2022.895537
Liang, Ren, Guo, Xing, Liu et al., Periodontal infection with Porphyromonas gingivalis induces preterm birth and lower birth weight in rats, Mol. Oral Microbiol, doi:10.1111/omi.12227
Liu, Huang, Huang, Wang, Ming et al., From nitrate to NO: Potential effects of nitratereducing bacteria on systemic health and disease, Eur. J. Med. Res, doi:10.1186/s40001-023-01413-y
Liu, Shi, Zeng, Bi, Mo et al., Oral microbiota and respiratory diseases: Advances and perspectives, Clin. Microbiol. Rev, doi:10.1128/cmr.00150-24
Liu, Werner, Kirsch, Zuckerman, Virk, Cytotoxicity evaluation of chlorhexidine gluconate on human fibroblasts, myoblasts, and osteoblasts, J. Bone Jt. Infect, doi:10.7150/jbji.26355
Lê, Cecchin-Albertoni, Thomas, Kemoun, Minty et al., The Role of Dysbiotic Oral Microbiota in Cardiometabolic Diseases: A Narrative Review, Diagnostics, doi:10.3390/diagnostics13203184
Ma, Tu, Chen, Postbiotics in Human Health: A Narrative Review, Nutrients, doi:10.3390/nu15020291
Magrin, Strauss, Benfatti, Maia, Gruber, Effects of Short-Chain Fatty Acids on Human Oral Epithelial Cells and the Potential Impact on Periodontal Disease: A Systematic Review of In Vitro Studies, Int. J. Mol. Sci, doi:10.3390/ijms21144895
Maksymowicz, Machowiec, Ręka, Korzeniowska, Leszczyk et al., Mechanism of action of triclosan as an endocrine-disrupting chemical with its impact on human health-Literature review, J. Pre-Clin. Clin. Res, doi:10.26444/jpccr/142065
Mao, Auer, Buchalla, Hiller, Maisch et al., Cetylpyridinium Chloride: Mechanism of Action, Antimicrobial Efficacy in Biofilms, and Potential Risks of Resistance, Antimicrob. Agents Chemother, doi:10.1128/AAC.00576-20
Mao, Hiergeist, Auer, Scholz, Muehler et al., Ecological Effects of Daily Antiseptic Treatment on Microbial Composition of Saliva-Grown Microcosm Biofilms and Selection of Resistant Phenotypes, Front. Microbiol, doi:10.3389/fmicb.2022.934525
Marinković, Rakašević, Nemoda, Nikolić, Marković et al., EO-based mouthwashes: Is there something that should be known? Balk, J. Dent. Med, doi:10.5937/bjdm2301032M
Mariotti, Rumpf, Chlorhexidine-Induced Changes to Human Gingival Fibroblast Collagen and Non-Collagen Protein Production, J. Periodontol, doi:10.1902/jop.1999.70.12.1443
Marques, Mariana, Cairrao, Triclosan and Its Consequences on the Reproductive, Cardiovascular and Thyroid Levels, Int. J. Mol. Sci, doi:10.3390/ijms231911427
Mcdonnell, Russell, Antiseptics and Disinfectants: Activity, Action, and Resistance, Clin. Microbiol. Rev, doi:10.1128/CMR.12.1.147
Merchant, Gupta Rdas Akonde, Reynolds, Smith-Warner, Liu et al., Association of Chlorhexidine Use and Scaling and Root Planing With Birth Outcomes in Pregnant Individuals With Periodontitis, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2022.47632
Min, Yang, Hu, Huang, Oral microbiota dysbiosis accelerates the development and onset of mucositis and oral ulcers, Front. Microbiol, doi:10.3389/fmicb.2023.1061032
Mitsui, Harasawa, The effects of essential oil, povidone-iodine, and chlorhexidine mouthwash on salivary nitrate/nitrite and nitrate-reducing bacteria, J. Oral Sci, doi:10.2334/josnusd.16-0593
Mosaddad, Mahootchi, Safari, Rahimi, Aghili, Interactions between systemic diseases and oral microbiota shifts in the aging community: A narrative review, J. Basic Microbiol, doi:10.1002/jobm.202300141
Muniz, Cavagni, Langa, Stewart, Malheiros et al., A Systematic Review of the Effect of Oral Rinsing with H 2 O 2 on Clinical and Microbiological Parameters Related to Plaque, Gingivitis, and Microbes, Int. J. Dent, doi:10.1155/2020/8841722
Muras, Mallo, Otero-Casal, Pose-Rodríguez, Otero, Quorum sensing systems as a new target to prevent biofilm-related oral diseases, Oral Dis, doi:10.1111/odi.13689
Murugesan, Venkat, The effect of iodine in patients using povidone-iodine mouth wash on thyroid function, Int. J. Otorhinolaryngol. Head Neck Surg, doi:10.18203/issn.2454-5929.ijohns20194927
Najafi, Taheri, Mokhtari, Forouzanfar, Farazi et al., Comparative study of 0.2% and 0.12% digluconate chlorhexidine mouth rinses on the level of dental staining and gingival indices, Dent. Res. J
Nikolić, Marković, Marković, Glamočlija, Ćirić et al., Antimicrobial activity of three Lamiaceae essential oils against common oral pathogens, Balk. J. Dent. Med, doi:10.1515/bjdm-2016-0026
Näse, Hatakka, Savilahti, Saxelin, Pönkä et al., Effect of Long-Term Consumption of a Probiotic Bacterium, Lactobacillus rhamnosus GG, in Milk on Dental Caries and Caries Risk in Children, Caries Res, doi:10.1159/000047484
Oliveira, Paula, Cardoso, Silva, Tavares et al., Exploring the antimicrobial efficacy of tea tree essential oil and chitosan against oral pathogens to overcome antimicrobial resistance, Microb. Pathog, doi:10.1016/j.micpath.2024.107006
Pathak, Yan, Zhang, Wang, Ge, The role of oral microbiome in respiratory health and diseases, Respir. Med, doi:10.1016/j.rmed.2021.106475
Peng, Cheng, You, Tang, Ren et al., Oral microbiota in human systematic diseases, Int. J. Oral Sci, doi:10.1038/s41368-022-00163-7
Pietiäinen, Liljestrand, Kopra, Pussinen, Mediators between oral dysbiosis and cardiovascular diseases, Eur. J. Oral Sci, doi:10.1111/eos.12423
Pignatelli, Fabietti, Ricci, Piattelli, Curia, How Periodontal Disease and Presence of Nitric Oxide Reducing Oral Bacteria Can Affect Blood Pressure, Int. J. Mol. Sci, doi:10.3390/ijms21207538
Polizzi, Donzella, Nicolosi, Santonocito, Pesce et al., Drugs for the Quorum Sensing Inhibition of Oral Biofilm: New Frontiers and Insights in the Treatment of Periodontitis, Pharmaceutics, doi:10.3390/pharmaceutics14122740
Pompilio, Scocchi, Mangoni, Shirooie, Serio et al., Bioactive compounds: A goldmine for defining new strategies against pathogenic bacterial biofilms?, Crit. Rev. Microbiol, doi:10.1080/1040841X.2022.2038082
Poppolo Deus, Ouanounou, Chlorhexidine in Dentistry: Pharmacology, Uses, and Adverse Effects, Int. Dent. J, doi:10.1016/j.identj.2022.01.005
Poppolo Deus, Ouanounou, Mouthwashes and their use in dentistry: A review, Oral Health
Prasanth, Antimicrobial efficacy of different toothpastes and mouthrinses: An in vitro study, Dent. Res. J
Preshaw, Mouthwash use and risk of diabetes, Br. Dent. J, doi:10.1038/sj.bdj.2018.1020
Pucher, Daniel, The Effects of Chlorhexidine Digluconate on Human Fibroblasts In Vitro, J. Periodontol, doi:10.1902/jop.1992.63.6.526
Radu, Radu, Bochis, Arbănas, Lucan et al., Revisiting the Therapeutic Effects of Essential Oils on the Oral Microbiome, Pharmacy, doi:10.3390/pharmacy11010033
Rajasekaran, Krishnamurthy, Bosco, Jayaraman, Krishna et al., Oral Microbiome: A Review of Its Impact on Oral and Systemic Health, Microorganisms, doi:10.3390/microorganisms12091797
Raszewski, Nowakowska-Toporowska, We Żgowiec, Nowakowska, Design and characteristics of new experimental chlorhexidine dental gels with anti-staining properties, Adv. Clin. Exp. Med, doi:10.17219/acem/94152
Relman, The human microbiome: Ecosystem resilience and health, Nutr. Rev, doi:10.1111/j.1753-4887.2012.00489.x
Ren, Zhang, Xiang, Hu, Cheng et al., The efficacy of mouthwashes on oral microorganisms and gingivitis in patients undergoing orthodontic treatment: A systematic review and meta-analysis, BMC Oral Health, doi:10.1186/s12903-023-02920-4
Rioboo, García, Serrano, O'connor, Herrera et al., Clinical and microbiological efficacy of an antimicrobial mouth rinse containing 0.05% cetylpyridinium chloride in patients with gingivitis, Int. J. Dent. Hyg, doi:10.1111/j.1601-5037.2011.00523.x
Rodríguez Zorrilla, Blanco Carrión, García García, Galindo Moreno, Marichalar Mendía et al., Effect of antiseptic gels in the microbiologic colonization of the suture threads after oral surgery, Sci. Rep, doi:10.1038/s41598-020-65007-y
Rosier, Buetas, Moya-Gonzalvez, Artacho, Mira, Nitrate as a potential prebiotic for the oral microbiome, Sci. Rep, doi:10.1038/s41598-020-69931-x
Rossi Ade Ferreira, Silva, Queiroz, Silva, Nelson-Filho, Antimicrobial Activity of Toothpastes Containing Natural Extracts, Chlorhexidine or Triclosan, Braz. Dent. J, doi:10.1590/0103-6440201300027
Rui, Zhong, Li, Tang, Wang et al., Evaluating the Role of Postbiotics in the Modulation of Human Oral Microbiota: A Randomized Controlled Clinical Trial, Probiotics Antimicrob Proteins, doi:10.1007/s12602-024-10238-y
Ruszkiewicz, Li, Rodriguez, Aschner, Is Triclosan a neurotoxic agent?, J. Toxicol. Environ. Health Part B, doi:10.1080/10937404.2017.1281181
Saeed, Khabeer, Faridi, Makhdoom, Effectiveness of propolis in maintaining oral health: A scoping review, Can. J. Dent. Hyg
Sanz, Herrera, Kebschull, Chapple, Jepsen et al., Treatment of stage I-III periodontitis-The EFP S3 level clinical practice guideline, J. Clin. Periodontol, doi:10.1111/jcpe.13290
Sanz-Martin, Doolittle-Hall, FRF Teles Exploring the microbiome of healthy and diseased peri-implant sites using Illumina sequencing, J. Clin. Periodontol, doi:10.1111/jcpe.12788
Schenkein, Loos, Inflammatory mechanisms linking periodontal diseases to cardiovascular diseases, J. Periodontol, doi:10.1902/jop.2013.134006
Serrano, Escribano, Roldán, Martín, Herrera, Efficacy of adjunctive anti-plaque chemical agents in managing gingivitis: A systematic review and meta-analysis, J. Clin. Periodontol, doi:10.1111/jcpe.12331
Shi, Chang, Martin, Mitreva, Lux et al., Dynamic Changes in the Subgingival Microbiome and Their Potential for Diagnosis and Prognosis of Periodontitis, mBio, doi:10.1128/mBio.01926-14
Sinicropi, Iacopetta, Ceramella, Catalano, Mariconda et al., Triclosan: A Small Molecule with Controversial Roles, Antibiotics, doi:10.3390/antibiotics11060735
Slomka, Hernandez-Sanabria, Herrero, Zaidel, Bernaerts et al., Nutritional stimulation of commensal oral bacteria suppresses pathogens: The prebiotic concept, J. Clin. Periodontol, doi:10.1111/jcpe.12700
Soares, Firoozi, Maria De Souza, Beatriz Lopes Martins, Gabriel Moreira Falci et al., Efficacy of Probiotics Compared to Chlorhexidine Mouthwash in Improving Periodontal Status: A Systematic Review and Meta-Analysis, Int. J. Dent, doi:10.1155/2023/4013004
Srivastava, Effect of Probiotic Curd on Salivary pH and Streptococcus mutans: A Double Blind Parallel Randomized Controlled Trial, J. Clin. Diagn. Res, doi:10.7860/JCDR/2016/15530.7178
Surana, Ahire, Pawar, Khairnar, Mahajan et al., Oral Health and Prebiotics, doi:10.1002/9781394167227.ch11
Takenaka, Ohsumi, Noiri, Evidence-based strategy for dental biofilms: Current evidence of mouthwashes on dental biofilm and gingivitis, Jpn. Dent. Sci. Rev, doi:10.1016/j.jdsr.2018.07.001
Takenaka, Sotozono, Ohkura, Noiri, Evidence on the Use of Mouthwash for the Control of Supragingival Biofilm and Its Potential Adverse Effects, Antibiotics, doi:10.3390/antibiotics11060727
Tan, Zhong, Liu, Chen, Zhao et al., Potential interaction between the oral microbiota and COVID-19: A meta-analysis and bioinformatics prediction, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2023.1193340
Tartaglia, Kumar, Fornari, Corti, Connelly, Mouthwashes in the 21st century: A narrative review about active molecules and effectiveness on the periodontal outcomes, Expert Opin. Drug Deliv, doi:10.1080/17425247.2017.1260118
Tartaglia, Tadakamadla, Connelly, Sforza, Martín, Adverse events associated with home use of mouthrinses: A systematic review, Ther. Adv. Drug Saf, doi:10.1177/2042098619854881
Teles, Teles, Frias-Lopez, Paster, Haffajee, Lessons learned and unlearned in periodontal microbiology, Periodontol, doi:10.1111/prd.12010
Teng, He, Huang, Bo, Li et al., Cetylpyridinium chloride mouth rinses alleviate experimental gingivitis by inhibiting dental plaque maturation, Int. J. Oral. Sci, doi:10.1038/ijos.2016.18
Thomas, Minty, Vinel, Canceill, Loubières et al., Oral Microbiota: A Major Player in the Diagnosis of Systemic Diseases, Diagnostics, doi:10.3390/diagnostics11081376
Tricco, Lillie, Zarin, O'brien, Colquhoun et al., PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation, Ann. Intern. Med
Van Der Weijden, Van Der Sluijs, Ciancio, Slot, Can Chemical Mouthwash Agents Achieve Plaque/Gingivitis Control?, Dent. Clin. N. Am, doi:10.1016/j.cden.2015.06.002
Verspecht, Rodriguez Herrero, Khodaparast, Khodaparast, Boon et al., Development of antiseptic adaptation and cross-adapatation in selected oral pathogens in vitro, Sci. Rep, doi:10.1038/s41598-019-44822-y
Wade, Addy, Antibacterial Activity of Some Triclosan-Containing Toothpastes and Their Ingredients, J. Periodontol, doi:10.1902/jop.1992.63.4.280
Wang, Kaplan, Burk, Qi, The Oral Microbiota, Microbial Metabolites, and Immuno-Inflammatory Mechanisms in Cardiovascular Disease, Int. J. Mol. Sci, doi:10.3390/ijms252212337
Wang, Yue, Jiang, Huang, Shen et al., Oral Microbiota Linking Associations of Dietary Factors with Recurrent Oral Ulcer, Nutrients, doi:10.3390/nu16101519
Weatherly, Gosse, Triclosan exposure, transformation, and human health effects, J. Toxicol. Environ. Health Part B, doi:10.1080/10937404.2017.1399306
Wirth, Pap, Maróti, Vályi, Komlósi et al., Toward Personalized Oral Diagnosis: Distinct Microbiome Clusters in Periodontitis Biofilms, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2021.747814
Wyganowska-Swiatkowska, Kotwicka, Urbaniak, Nowak, Skrzypczak-Jankun et al., Clinical implications of the growth-suppressive effects of chlorhexidine at low and high concentrations on human gingival fibroblasts and changes in morphology, Int. J. Mol. Med, doi:10.3892/ijmm.2016.2550
Wylie, Mihindukulasuriya, Zhou, Sodergren, Storch et al., Metagenomic analysis of doublestranded DNA viruses in healthy adults, BMC Biol, doi:10.1186/s12915-014-0071-7
Yang, Mu, Wang, Zhu, Zhang et al., Dysbiosis of the Salivary Microbiome Is Associated with Non-smoking Female Lung Cancer and Correlated with Immunocytochemistry Markers, Front. Oncol, doi:10.3389/fonc.2018.00520
Yayli, Tunc, Degirmenci, Dikilitas, Taspinar, Comparative Evaluation of the Cytotoxic Effects of Different Oral Antiseptics, Niger. J. Clin. Pract, doi:10.4103/njcp.njcp_253_20
Yoneyama, Shimizu, Tabata, Yashiro, Takata et al., In vitro Short-Time Killing Activity of Povidone-Iodine (Isodine ® Gargle) in the Presence of Oral Organic Matter, Dermatology, doi:10.1159/000089207
Zaura, Keijser, Huse, Crielaard, Defining the healthy "core microbiome" of oral microbial communities, BMC Microbiol, doi:10.1186/1471-2180-9-259
Zhang, Liu, Zheng, Zhang, The oral microbiota may have influence on oral cancer, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2019.00476
Zhang, Wang, Li, Ni, Du et al., Human oral microbiota and its modulation for oral health, Biomed. Pharmacother, doi:10.1016/j.biopha.2018.01.146
Zheng, Xie, Li, Qiao, Lu et al., Analysis of oral microbial dysbiosis associated with early childhood caries, BMC Oral Health, doi:10.1186/s12903-021-01543-x
DOI record:
{
"DOI": "10.3390/antibiotics14080815",
"ISSN": [
"2079-6382"
],
"URL": "http://dx.doi.org/10.3390/antibiotics14080815",
"abstract": "<jats:p>Background: Oral antiseptic formulations are widely used as adjuncts in oral hygiene to reduce pathogenic microorganisms and prevent oral diseases. While these agents are effective in controlling biofilm, their broader effects may disrupt the oral microbiota’s balance, potentially contributing to systemic health implications. The complex relationship between antiseptic use, microbial composition, and systemic outcomes remains insufficiently mapped. Objective: This scoping review aimed to explore and map the current evidence regarding the impact of antiseptic formulations on oral microbiota composition and to examine their potential associations with systemic diseases. Methods: A comprehensive literature search was performed using PubMed, Scopus, and Web of Science up to June 2025. Studies were included if they investigated antiseptic formulations commonly used in oral healthcare—such as chlorhexidine, essential oils, and cetylpyridinium chloride—and reported effects on oral microbiota and/or systemic health. Eligible study types included human clinical trials, observational studies, in vitro, and animal studies. Two reviewers independently screened and selected studies, with disagreements resolved by consensus. Data extraction focused on study design, antiseptic agents, microbial outcomes, and systemic implications. A total of 12 studies were included and charted. Results: The included studies demonstrated that oral antiseptics effectively reduce pathogenic microorganisms and improve clinical outcomes in oral diseases such as gingivitis and periodontitis. However, several studies also reported alterations in commensal microbial communities, suggesting a potential for dysbiosis. Some studies indicated possible links between antiseptic-induced microbial changes and systemic conditions, including cardiovascular and respiratory diseases. Conclusions: The evidence highlights a dual effect of antiseptic formulations: while beneficial in controlling oral pathogens, they may disrupt microbial homeostasis with possible systemic consequences. Further research is needed to evaluate long-term effects and develop targeted, microbiota-preserving oral hygiene strategies.</jats:p>",
"alternative-id": [
"antibiotics14080815"
],
"author": [
{
"ORCID": "https://orcid.org/0009-0008-3231-0704",
"affiliation": [
{
"name": "Unit of Periodontology, Department of General Surgery and Surgical-Medical Specialties, School of Dentistry, University of Catania, 95123 Catania, Italy"
}
],
"authenticated-orcid": false,
"family": "Angjelova",
"given": "Angela",
"sequence": "first"
},
{
"ORCID": "https://orcid.org/0009-0008-1089-2598",
"affiliation": [
{
"name": "Unit of Periodontology, Department of General Surgery and Surgical-Medical Specialties, School of Dentistry, University of Catania, 95123 Catania, Italy"
}
],
"authenticated-orcid": false,
"family": "Jovanova",
"given": "Elena",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0001-6717-8899",
"affiliation": [
{
"name": "Unit of Periodontology, Department of General Surgery and Surgical-Medical Specialties, School of Dentistry, University of Catania, 95123 Catania, Italy"
},
{
"name": "International Research Center on Periodontal and Systemic Health “PerioHealth”, University of Catania, 95123 Catania, Italy"
}
],
"authenticated-orcid": false,
"family": "Polizzi",
"given": "Alessandro",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0002-9433-9528",
"affiliation": [
{
"name": "Unit of Periodontology, Department of General Surgery and Surgical-Medical Specialties, School of Dentistry, University of Catania, 95123 Catania, Italy"
}
],
"authenticated-orcid": false,
"family": "Leonardi",
"given": "Rosalia",
"sequence": "additional"
},
{
"ORCID": "https://orcid.org/0000-0003-4267-6992",
"affiliation": [
{
"name": "Unit of Periodontology, Department of General Surgery and Surgical-Medical Specialties, School of Dentistry, University of Catania, 95123 Catania, Italy"
},
{
"name": "International Research Center on Periodontal and Systemic Health “PerioHealth”, University of Catania, 95123 Catania, Italy"
}
],
"authenticated-orcid": false,
"family": "Isola",
"given": "Gaetano",
"sequence": "additional"
}
],
"container-title": "Antibiotics",
"container-title-short": "Antibiotics",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2025,
8,
8
]
],
"date-time": "2025-08-08T15:30:52Z",
"timestamp": 1754667052000
},
"deposited": {
"date-parts": [
[
2025,
10,
9
]
],
"date-time": "2025-10-09T18:26:48Z",
"timestamp": 1760034408000
},
"indexed": {
"date-parts": [
[
2026,
1,
31
]
],
"date-time": "2026-01-31T05:19:57Z",
"timestamp": 1769836797091,
"version": "3.49.0"
},
"is-referenced-by-count": 6,
"issue": "8",
"issued": {
"date-parts": [
[
2025,
8,
8
]
]
},
"journal-issue": {
"issue": "8",
"published-online": {
"date-parts": [
[
2025,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
8,
8
]
],
"date-time": "2025-08-08T00:00:00Z",
"timestamp": 1754611200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2079-6382/14/8/815/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "815",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2025,
8,
8
]
]
},
"published-online": {
"date-parts": [
[
2025,
8,
8
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1038/sj.bdj.2016.865",
"article-title": "The oral microbiome—An update for oral healthcare professionals",
"author": "Kilian",
"doi-asserted-by": "crossref",
"first-page": "657",
"journal-title": "Br. Dent. J.",
"key": "ref_1",
"volume": "221",
"year": "2016"
},
{
"DOI": "10.20944/preprints202406.1923.v1",
"doi-asserted-by": "crossref",
"key": "ref_2",
"unstructured": "Rajasekaran, J.J., Krishnamurthy, H.K., Bosco, J., Jayaraman, V., Krishna, K., Wang, T., and Bei, K. (2024). Oral Microbiome: A Review of Its Impact on Oral and Systemic Health. Microorganisms, 12."
},
{
"DOI": "10.1016/j.biopha.2018.01.146",
"article-title": "Human oral microbiota and its modulation for oral health",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "883",
"journal-title": "Biomed. Pharmacother.",
"key": "ref_3",
"volume": "99",
"year": "2018"
},
{
"DOI": "10.1186/1471-2180-9-259",
"doi-asserted-by": "crossref",
"key": "ref_4",
"unstructured": "Zaura, E., Keijser, B.J.F., Huse, S.M., and Crielaard, W. (2009). Defining the healthy “core microbiome” of oral microbial communities. BMC Microbiol., 9."
},
{
"DOI": "10.4103/jomfp.JOMFP_304_18",
"article-title": "Oral microbiome: Unveiling the fundamentals",
"author": "Deo",
"doi-asserted-by": "crossref",
"first-page": "122",
"journal-title": "J. Oral Maxillofac. Pathol.",
"key": "ref_5",
"volume": "23",
"year": "2019"
},
{
"DOI": "10.1111/j.1753-4887.2012.00489.x",
"article-title": "The human microbiome: Ecosystem resilience and health",
"author": "Relman",
"doi-asserted-by": "crossref",
"first-page": "S2",
"journal-title": "Nutr. Rev.",
"key": "ref_6",
"volume": "70",
"year": "2012"
},
{
"DOI": "10.1016/j.cmet.2011.02.018",
"article-title": "The Microbiome and Butyrate Regulate Energy Metabolism and Autophagy in the Mammalian Colon",
"author": "Donohoe",
"doi-asserted-by": "crossref",
"first-page": "517",
"journal-title": "Cell Metab.",
"key": "ref_7",
"volume": "13",
"year": "2011"
},
{
"DOI": "10.1016/j.identj.2023.08.010",
"article-title": "Mouthwash Effects on the Oral Microbiome: Are They Good, Bad, or Balanced?",
"author": "Brookes",
"doi-asserted-by": "crossref",
"first-page": "S74",
"journal-title": "Int. Dent. J.",
"key": "ref_8",
"volume": "73",
"year": "2023"
},
{
"DOI": "10.1038/sj.bdj.2018.217",
"article-title": "The oral microbiota—A mechanistic role for systemic diseases",
"author": "Jia",
"doi-asserted-by": "crossref",
"first-page": "447",
"journal-title": "Br. Dent. J.",
"key": "ref_9",
"volume": "224",
"year": "2018"
},
{
"DOI": "10.3390/diagnostics11081376",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Thomas, C., Minty, M., Vinel, A., Canceill, T., Loubières, P., Burcelin, R., Groen, A.K., Serrano-Villar, S., Moreno, S., and Sokol, H. (2021). Oral Microbiota: A Major Player in the Diagnosis of Systemic Diseases. Diagnostics, 11."
},
{
"DOI": "10.1002/jobm.202300141",
"article-title": "Interactions between systemic diseases and oral microbiota shifts in the aging community: A narrative review",
"author": "Mosaddad",
"doi-asserted-by": "crossref",
"first-page": "831",
"journal-title": "J. Basic Microbiol.",
"key": "ref_11",
"volume": "63",
"year": "2023"
},
{
"DOI": "10.1016/j.identj.2023.08.012",
"article-title": "The Effects of Antimicrobial Mouthwashes on Systemic Disease: What Is the Evidence?",
"author": "Alrashdan",
"doi-asserted-by": "crossref",
"first-page": "S82",
"journal-title": "Int. Dent. J.",
"key": "ref_12",
"volume": "73",
"year": "2023"
},
{
"article-title": "Mouthwashes: Rationale for use",
"author": "Ciancio",
"first-page": "4A",
"journal-title": "Am. J. Dent.",
"key": "ref_13",
"volume": "28",
"year": "2015"
},
{
"DOI": "10.1002/JPER.20-0096",
"article-title": "Biologically informed stratification of periodontal disease holds the key to achieving precision oral health",
"author": "Divaris",
"doi-asserted-by": "crossref",
"first-page": "S50",
"journal-title": "J. Periodontol.",
"key": "ref_14",
"volume": "91",
"year": "2020"
},
{
"DOI": "10.1186/s12903-017-0400-7",
"doi-asserted-by": "crossref",
"key": "ref_15",
"unstructured": "Haydari, M., Bardakci, A.G., Koldsland, O.C., Aass, A.M., Sandvik, L., and Preus, H.R. (2017). Comparing the effect of 0.06% -, 0.12% and 0.2% Chlorhexidine on plaque, bleeding and side effects in an experimental gingivitis model: A parallel group, double masked randomized clinical trial. BMC Oral Health, 17."
},
{
"article-title": "Comparative study of 0.2% and 0.12% digluconate chlorhexidine mouth rinses on the level of dental staining and gingival indices",
"author": "Najafi",
"first-page": "305",
"journal-title": "Dent. Res. J.",
"key": "ref_16",
"volume": "9",
"year": "2012"
},
{
"DOI": "10.1007/s00784-009-0320-2",
"article-title": "In vivo substantivity of 0.12% and 0.2% chlorhexidine mouthrinses on salivary bacteria",
"author": "Cousido",
"doi-asserted-by": "crossref",
"first-page": "397",
"journal-title": "Clin. Oral Investig.",
"key": "ref_17",
"volume": "14",
"year": "2010"
},
{
"DOI": "10.1038/ijos.2016.18",
"article-title": "Cetylpyridinium chloride mouth rinses alleviate experimental gingivitis by inhibiting dental plaque maturation",
"author": "Teng",
"doi-asserted-by": "crossref",
"first-page": "182",
"journal-title": "Int. J. Oral. Sci.",
"key": "ref_18",
"volume": "8",
"year": "2016"
},
{
"DOI": "10.1016/j.clinthera.2009.11.004",
"article-title": "A randomized, double-blind clinical study to assess the antimicrobial effects of a cetylpyridinium chloride mouth rinse on dental plaque bacteria",
"author": "Hu",
"doi-asserted-by": "crossref",
"first-page": "2540",
"journal-title": "Clin. Ther.",
"key": "ref_19",
"volume": "31",
"year": "2009"
},
{
"DOI": "10.1111/j.1601-5037.2011.00523.x",
"article-title": "Clinical and microbiological efficacy of an antimicrobial mouth rinse containing 0.05% cetylpyridinium chloride in patients with gingivitis",
"author": "Rioboo",
"doi-asserted-by": "crossref",
"first-page": "98",
"journal-title": "Int. J. Dent. Hyg.",
"key": "ref_20",
"volume": "10",
"year": "2012"
},
{
"DOI": "10.7754/Clin.Lab.2014.140714",
"article-title": "Antimicrobial effect of Australian antibacterial essential oils as alternative to common antiseptic solutions against clinically relevant oral pathogens",
"author": "Karbach",
"doi-asserted-by": "crossref",
"first-page": "61",
"journal-title": "Clin. Lab.",
"key": "ref_21",
"volume": "61",
"year": "2015"
},
{
"DOI": "10.1515/bjdm-2016-0026",
"article-title": "Antimicrobial activity of three Lamiaceae essential oils against common oral pathogens",
"author": "Sokovic",
"doi-asserted-by": "crossref",
"first-page": "160",
"journal-title": "Balk. J. Dent. Med.",
"key": "ref_22",
"volume": "20",
"year": "2016"
},
{
"DOI": "10.2334/josnusd.16-0593",
"article-title": "The effects of essential oil, povidone-iodine, and chlorhexidine mouthwash on salivary nitrate/nitrite and nitrate-reducing bacteria",
"author": "Mitsui",
"doi-asserted-by": "crossref",
"first-page": "597",
"journal-title": "J. Oral Sci.",
"key": "ref_23",
"volume": "59",
"year": "2017"
},
{
"DOI": "10.1111/j.1600-051X.1988.tb01556.x",
"article-title": "Microbiological and clinical effects of chlorhexidine digluconate and hydrogen peroxide mouthrinses on developing plaque and gingivitis",
"author": "Gusberti",
"doi-asserted-by": "crossref",
"first-page": "60",
"journal-title": "J. Clin. Periodontol.",
"key": "ref_24",
"volume": "15",
"year": "1988"
},
{
"DOI": "10.1016/j.micpath.2024.107006",
"article-title": "Exploring the antimicrobial efficacy of tea tree essential oil and chitosan against oral pathogens to overcome antimicrobial resistance",
"author": "Oliveira",
"doi-asserted-by": "crossref",
"first-page": "107006",
"journal-title": "Microb. Pathog.",
"key": "ref_25",
"volume": "196",
"year": "2024"
},
{
"article-title": "Effect of Propolis mouthwash on plaque and gingival indices over fixed orthodontic patients",
"author": "Dehghani",
"first-page": "e244",
"journal-title": "J. Clin. Exp. Dent.",
"key": "ref_26",
"volume": "11",
"year": "2019"
},
{
"DOI": "10.1111/j.1600-0757.1997.tb00190.x",
"article-title": "The microbial challenge in periodontitis",
"author": "Darveau",
"doi-asserted-by": "crossref",
"first-page": "12",
"journal-title": "Periodontol. 2000",
"key": "ref_27",
"volume": "14",
"year": "1997"
},
{
"DOI": "10.1111/prd.12010",
"article-title": "Lessons learned and unlearned in periodontal microbiology",
"author": "Teles",
"doi-asserted-by": "crossref",
"first-page": "95",
"journal-title": "Periodontol. 2000",
"key": "ref_28",
"volume": "62",
"year": "2013"
},
{
"DOI": "10.1128/mBio.01926-14",
"article-title": "Dynamic Changes in the Subgingival Microbiome and Their Potential for Diagnosis and Prognosis of Periodontitis",
"author": "Shi",
"doi-asserted-by": "crossref",
"first-page": "e01926-14",
"journal-title": "mBio",
"key": "ref_29",
"volume": "6",
"year": "2015"
},
{
"DOI": "10.1038/srep38993",
"doi-asserted-by": "crossref",
"key": "ref_30",
"unstructured": "Dabdoub, S.M., Ganesan, S.M., and Kumar, P.S. (2016). Comparative metagenomics reveals taxonomically idiosyncratic yet functionally congruent communities in periodontitis. Sci. Rep., 6."
},
{
"DOI": "10.3389/fmicb.2023.1061032",
"doi-asserted-by": "crossref",
"key": "ref_31",
"unstructured": "Min, Z., Yang, L., Hu, Y., and Huang, R. (2023). Oral microbiota dysbiosis accelerates the development and onset of mucositis and oral ulcers. Front. Microbiol., 14."
},
{
"DOI": "10.3389/fmicb.2022.895537",
"doi-asserted-by": "crossref",
"key": "ref_32",
"unstructured": "Li, X., Liu, Y., Yang, X., Li, C., and Song, Z. (2022). The Oral Microbiota: Community Composition, Influencing Factors, Pathogenesis, and Interventions. Front. Microbiol., 13."
},
{
"DOI": "10.1186/s12915-014-0071-7",
"doi-asserted-by": "crossref",
"key": "ref_33",
"unstructured": "Wylie, K.M., Mihindukulasuriya, K.A., Zhou, Y., Sodergren, E., Storch, G.A., and Weinstock, G.M. (2014). Metagenomic analysis of double-stranded DNA viruses in healthy adults. BMC Biol., 12."
},
{
"DOI": "10.1038/s41579-023-00963-6",
"article-title": "The oral microbiome: Diversity, biogeography and human health",
"author": "Baker",
"doi-asserted-by": "crossref",
"first-page": "89",
"journal-title": "Nat. Rev. Microbiol.",
"key": "ref_34",
"volume": "22",
"year": "2024"
},
{
"DOI": "10.1186/s40001-023-01413-y",
"article-title": "From nitrate to NO: Potential effects of nitrate-reducing bacteria on systemic health and disease",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "425",
"journal-title": "Eur. J. Med. Res.",
"key": "ref_35",
"volume": "28",
"year": "2023"
},
{
"DOI": "10.3389/fcimb.2025.1517154",
"doi-asserted-by": "crossref",
"key": "ref_36",
"unstructured": "Cui, Z., Wang, P., and Gao, W. (2025). Microbial dysbiosis in periodontitis and peri-implantitis: Pathogenesis, immune responses, and therapeutic. Front. Cell. Infect. Microbiol., 15."
},
{
"DOI": "10.1038/s41598-017-16418-x",
"doi-asserted-by": "crossref",
"key": "ref_37",
"unstructured": "Lee, W.-H., Chen, H.-M., Yang, S.-F., Liang, C., Peng, C.-Y., Lin, F.-M., Lee, J.-C., Chen, C.-Y., Yang, S.-Y., and Huang, C.-C. (2017). Bacterial alterations in salivary microbiota and their association in oral cancer. Sci. Rep., 7."
},
{
"DOI": "10.1111/jcpe.12788",
"article-title": "FRF Teles Exploring the microbiome of healthy and diseased peri-implant sites using Illumina sequencing",
"doi-asserted-by": "crossref",
"first-page": "1274",
"journal-title": "J. Clin. Periodontol.",
"key": "ref_38",
"volume": "44",
"year": "2017"
},
{
"DOI": "10.3390/antibiotics11060727",
"doi-asserted-by": "crossref",
"key": "ref_39",
"unstructured": "Takenaka, S., Sotozono, M., Ohkura, N., and Noiri, Y. (2022). Evidence on the Use of Mouthwash for the Control of Supragingival Biofilm and Its Potential Adverse Effects. Antibiotics, 11."
},
{
"DOI": "10.3389/froh.2023.1210200",
"doi-asserted-by": "crossref",
"key": "ref_40",
"unstructured": "Basic, A., and Dahlén, G. (2023). Microbial metabolites in the pathogenesis of periodontal diseases: A narrative review. Front. Oral Health, 4."
},
{
"DOI": "10.1038/s41522-020-0124-3",
"doi-asserted-by": "crossref",
"key": "ref_41",
"unstructured": "Chatzigiannidou, I., Teughels, W., Van de Wiele, T., and Boon, N. (2020). Oral biofilms exposure to chlorhexidine results in altered microbial composition and metabolic profile. npj Biofilms Microbiomes, 6."
},
{
"DOI": "10.1016/j.imlet.2014.08.017",
"article-title": "The oral microbiome and the immunobiology of periodontal disease and caries",
"author": "Costalonga",
"doi-asserted-by": "crossref",
"first-page": "22",
"journal-title": "Immunol. Lett.",
"key": "ref_42",
"volume": "162",
"year": "2014"
},
{
"DOI": "10.1101/gr.265645.120",
"article-title": "Deep metagenomics examines the oral microbiome during dental caries, revealing novel taxa and co-occurrences with host molecules",
"author": "Baker",
"doi-asserted-by": "crossref",
"first-page": "64",
"journal-title": "Genome Res.",
"key": "ref_43",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.1186/s12903-021-01543-x",
"doi-asserted-by": "crossref",
"key": "ref_44",
"unstructured": "Zheng, H., Xie, T., Li, S., Qiao, X., Lu, Y., and Feng, Y. (2021). Analysis of oral microbial dysbiosis associated with early childhood caries. BMC Oral Health, 21."
},
{
"DOI": "10.1038/ismej.2012.174",
"article-title": "The subgingival microbiome in health and periodontitis and its relationship with community biomass and inflammation",
"author": "Abusleme",
"doi-asserted-by": "crossref",
"first-page": "1016",
"journal-title": "ISME J.",
"key": "ref_45",
"volume": "7",
"year": "2013"
},
{
"DOI": "10.1186/2049-2618-2-32",
"doi-asserted-by": "crossref",
"key": "ref_46",
"unstructured": "Galimanas, V., Hall, M.W., Singh, N., Lynch, M.D.J., Goldberg, M., Tenenbaum, H., Cvitkovitch, D.G., Neufeld, J.D., and Senadheera, D.B. (2014). Bacterial community composition of chronic periodontitis and novel oral sampling sites for detecting disease indicators. Microbiome, 2."
},
{
"DOI": "10.1080/10937404.2017.1399306",
"article-title": "Triclosan exposure, transformation, and human health effects",
"author": "Weatherly",
"doi-asserted-by": "crossref",
"first-page": "447",
"journal-title": "J. Toxicol. Environ. Health Part B",
"key": "ref_47",
"volume": "20",
"year": "2017"
},
{
"DOI": "10.3389/fcimb.2019.00476",
"doi-asserted-by": "crossref",
"key": "ref_48",
"unstructured": "Zhang, L., Liu, Y., Zheng, H.J., and Zhang, C.P. (2019). The oral microbiota may have influence on oral cancer. Front. Cell. Infect. Microbiol., 9."
},
{
"DOI": "10.1371/journal.ppat.1007717",
"doi-asserted-by": "crossref",
"key": "ref_49",
"unstructured": "Bertolini, M., Ranjan, A., Thompson, A., Diaz, P.I., Sobue, T., Maas, K., and Dongari-Bagtzoglou, A. (2019). Candida albicans induces mucosal bacterial dysbiosis that promotes invasive infection. PLoS Pathog., 15."
},
{
"DOI": "10.3390/nu16101519",
"doi-asserted-by": "crossref",
"key": "ref_50",
"unstructured": "Wang, Y., Yue, H., Jiang, Y., Huang, Q., Shen, J., Hailili, G., Sun, Z., Zhou, X., Pu, Y., and Song, H. (2024). Oral Microbiota Linking Associations of Dietary Factors with Recurrent Oral Ulcer. Nutrients, 16."
},
{
"DOI": "10.1177/0022034513487559",
"article-title": "Mobile Microbiome",
"author": "Han",
"doi-asserted-by": "crossref",
"first-page": "485",
"journal-title": "J. Dent. Res.",
"key": "ref_51",
"volume": "92",
"year": "2013"
},
{
"DOI": "10.1073/pnas.1011383107",
"article-title": "Human oral, gut, and plaque microbiota in patients with atherosclerosis",
"author": "Koren",
"doi-asserted-by": "crossref",
"first-page": "4592",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_52",
"volume": "108",
"year": "2011"
},
{
"DOI": "10.3389/fmicb.2022.934525",
"doi-asserted-by": "crossref",
"key": "ref_53",
"unstructured": "Mao, X., Hiergeist, A., Auer, D.L., Scholz, K.J., Muehler, D., Hiller, K.-A., Maisch, T., Buchalla, W., Hellwig, E., and Gessner, A. (2022). Ecological Effects of Daily Antiseptic Treatment on Microbial Composition of Saliva-Grown Microcosm Biofilms and Selection of Resistant Phenotypes. Front. Microbiol., 13."
},
{
"DOI": "10.1128/AAC.00576-20",
"article-title": "Cetylpyridinium Chloride: Mechanism of Action, Antimicrobial Efficacy in Biofilms, and Potential Risks of Resistance",
"author": "Mao",
"doi-asserted-by": "crossref",
"first-page": "e00576-20",
"journal-title": "Antimicrob. Agents Chemother.",
"key": "ref_54",
"volume": "64",
"year": "2020"
},
{
"DOI": "10.1111/jcpe.12331",
"article-title": "Efficacy of adjunctive anti-plaque chemical agents in managing gingivitis: A systematic review and meta-analysis",
"author": "Serrano",
"doi-asserted-by": "crossref",
"first-page": "S106",
"journal-title": "J. Clin. Periodontol.",
"key": "ref_55",
"volume": "42",
"year": "2015"
},
{
"DOI": "10.3390/jpm13091332",
"doi-asserted-by": "crossref",
"key": "ref_56",
"unstructured": "Garrido, L., Lyra, P., Rodrigues, J., Viana, J., Mendes, J.J., and Barroso, H. (2023). Revisiting Oral Antiseptics, Microorganism Targets and Effectiveness. J. Pers. Med., 13."
},
{
"DOI": "10.1177/2042098619854881",
"article-title": "Adverse events associated with home use of mouthrinses: A systematic review",
"author": "Tartaglia",
"doi-asserted-by": "crossref",
"first-page": "2042098619854881",
"journal-title": "Ther. Adv. Drug Saf.",
"key": "ref_57",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1111/jcpe.13290",
"article-title": "Treatment of stage I–III periodontitis—The EFP S3 level clinical practice guideline",
"author": "Sanz",
"doi-asserted-by": "crossref",
"first-page": "4",
"journal-title": "J. Clin. Periodontol.",
"key": "ref_58",
"volume": "47",
"year": "2020"
},
{
"DOI": "10.1111/jcpe.13230",
"article-title": "Adjunctive effect of locally delivered antimicrobials in periodontitis therapy: A systematic review and meta-analysis",
"author": "Herrera",
"doi-asserted-by": "crossref",
"first-page": "239",
"journal-title": "J. Clin. Periodontol.",
"key": "ref_59",
"volume": "47",
"year": "2020"
},
{
"DOI": "10.1080/17425247.2017.1260118",
"article-title": "Mouthwashes in the 21st century: A narrative review about active molecules and effectiveness on the periodontal outcomes",
"author": "Tartaglia",
"doi-asserted-by": "crossref",
"first-page": "973",
"journal-title": "Expert Opin. Drug Deliv.",
"key": "ref_60",
"volume": "14",
"year": "2017"
},
{
"DOI": "10.1016/j.bioelechem.2023.108435",
"doi-asserted-by": "crossref",
"key": "ref_61",
"unstructured": "Berezovska, A., Meiller, A., Marinesco, S., Nedellec, Y., Giroud, F., Gross, A.J., and Cosnier, S. (2023). Chlorhexidine digluconate exerts bactericidal activity vs Gram positive Staphylococci with bioelectrocatalytic compatibility: High level disinfection for implantable biofuel cells. Bioelectrochemistry, 152."
},
{
"DOI": "10.1016/j.identj.2022.01.005",
"article-title": "Chlorhexidine in Dentistry: Pharmacology, Uses, and Adverse Effects",
"author": "Ouanounou",
"doi-asserted-by": "crossref",
"first-page": "269",
"journal-title": "Int. Dent. J.",
"key": "ref_62",
"volume": "72",
"year": "2022"
},
{
"DOI": "10.17219/acem/94152",
"article-title": "Design and characteristics of new experimental chlorhexidine dental gels with anti-staining properties",
"author": "Raszewski",
"doi-asserted-by": "crossref",
"first-page": "885",
"journal-title": "Adv. Clin. Exp. Med.",
"key": "ref_63",
"volume": "28",
"year": "2019"
},
{
"DOI": "10.1002/jps.3030340103",
"article-title": "The Effect of Cetylpyridinium Chloride on the Bacterial Growth in the Oral Cavity",
"author": "Huyck",
"doi-asserted-by": "crossref",
"first-page": "5",
"journal-title": "J. Am. Pharm. Assoc. (Sci. ed.)",
"key": "ref_64",
"volume": "34",
"year": "1945"
},
{
"DOI": "10.3390/medicines4030058",
"doi-asserted-by": "crossref",
"key": "ref_65",
"unstructured": "Chouhan, S., Sharma, K., and Guleria, S. (2017). Antimicrobial Activity of Some Essential Oils—Present Status and Future Perspectives. Medicines, 4."
},
{
"DOI": "10.1016/j.fct.2007.09.106",
"article-title": "Biological effects of essential oils—A review",
"author": "Bakkali",
"doi-asserted-by": "crossref",
"first-page": "446",
"journal-title": "Food Chem. Toxicol.",
"key": "ref_66",
"volume": "46",
"year": "2008"
},
{
"DOI": "10.1159/000089207",
"article-title": "In vitro Short-Time Killing Activity of Povidone-Iodine (Isodine® Gargle) in the Presence of Oral Organic Matter",
"author": "Yoneyama",
"doi-asserted-by": "crossref",
"first-page": "103",
"journal-title": "Dermatology",
"key": "ref_67",
"volume": "212",
"year": "2006"
},
{
"DOI": "10.1007/s12011-021-02978-7",
"article-title": "High Ingestion Rate of Iodine from Povidone-Iodine Mouthwash",
"author": "Fuse",
"doi-asserted-by": "crossref",
"first-page": "3902",
"journal-title": "Biol. Trace Elem. Res.",
"key": "ref_68",
"volume": "200",
"year": "2022"
},
{
"DOI": "10.1590/0103-6440201300027",
"article-title": "Antimicrobial Activity of Toothpastes Containing Natural Extracts, Chlorhexidine or Triclosan",
"doi-asserted-by": "crossref",
"first-page": "186",
"journal-title": "Braz. Dent. J.",
"key": "ref_69",
"volume": "25",
"year": "2014"
},
{
"DOI": "10.1902/jop.1992.63.4.280",
"article-title": "Antibacterial Activity of Some Triclosan-Containing Toothpastes and Their Ingredients",
"author": "Wade",
"doi-asserted-by": "crossref",
"first-page": "280",
"journal-title": "J. Periodontol.",
"key": "ref_70",
"volume": "63",
"year": "1992"
},
{
"DOI": "10.3892/ijmm.2016.2550",
"article-title": "Clinical implications of the growth-suppressive effects of chlorhexidine at low and high concentrations on human gingival fibroblasts and changes in morphology",
"author": "Kotwicka",
"doi-asserted-by": "crossref",
"first-page": "1594",
"journal-title": "Int. J. Mol. Med.",
"key": "ref_71",
"volume": "37",
"year": "2016"
},
{
"DOI": "10.1186/s12903-023-02920-4",
"doi-asserted-by": "crossref",
"key": "ref_72",
"unstructured": "Ren, X., Zhang, Y., Xiang, Y., Hu, T., Cheng, R., and Cai, H. (2023). The efficacy of mouthwashes on oral microorganisms and gingivitis in patients undergoing orthodontic treatment: A systematic review and meta-analysis. BMC Oral Health, 23."
},
{
"DOI": "10.1902/jop.1999.70.12.1443",
"article-title": "Chlorhexidine-Induced Changes to Human Gingival Fibroblast Collagen and Non-Collagen Protein Production",
"author": "Mariotti",
"doi-asserted-by": "crossref",
"first-page": "1443",
"journal-title": "J. Periodontol.",
"key": "ref_73",
"volume": "70",
"year": "1999"
},
{
"DOI": "10.1902/jop.1992.63.6.526",
"article-title": "The Effects of Chlorhexidine Digluconate on Human Fibroblasts In Vitro",
"author": "Pucher",
"doi-asserted-by": "crossref",
"first-page": "526",
"journal-title": "J. Periodontol.",
"key": "ref_74",
"volume": "63",
"year": "1992"
},
{
"DOI": "10.7150/jbji.26355",
"article-title": "Cytotoxicity evaluation of chlorhexidine gluconate on human fibroblasts, myoblasts, and osteoblasts",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "165",
"journal-title": "J. Bone Jt. Infect.",
"key": "ref_75",
"volume": "3",
"year": "2018"
},
{
"DOI": "10.1016/j.tiv.2007.09.012",
"article-title": "Effect of chlorhexidine digluconate on different cell types: A molecular and ultrastructural investigation",
"author": "Giannelli",
"doi-asserted-by": "crossref",
"first-page": "308",
"journal-title": "Toxicol. Vitr.",
"key": "ref_76",
"volume": "22",
"year": "2008"
},
{
"DOI": "10.3389/fmicb.2024.1429692",
"doi-asserted-by": "crossref",
"key": "ref_77",
"unstructured": "Bartsch, S., Kohnert, E., Kreutz, C., Woelber, J.P., Anderson, A., Burkhardt, A.-S., Hellwig, E., Buchalla, W., Hiller, K.A., and Krueger, P.R. (2024). Chlorhexidine digluconate mouthwash alters the oral microbial composition and affects the prevalence of antimicrobial resistance genes. Front. Microbiol., 15."
},
{
"article-title": "Antibacterial agents in the control of supragingival plaque—A review",
"author": "Eley",
"first-page": "286",
"journal-title": "Br. Dent. J.",
"key": "ref_78",
"volume": "186",
"year": "1999"
},
{
"article-title": "Importance of Chlorhexidine in Maintaining Periodontal Health",
"author": "Kaur",
"first-page": "31",
"journal-title": "Int. J. Dent. Res.",
"key": "ref_79",
"volume": "1",
"year": "2016"
},
{
"DOI": "10.1111/j.1600-051X.1989.tb02143.x",
"article-title": "Interaction between chlorhexidine digluconate and sodium lauryl sulfate in vivo",
"author": "Barkvoll",
"doi-asserted-by": "crossref",
"first-page": "593",
"journal-title": "J. Clin. Periodontol.",
"key": "ref_80",
"volume": "16",
"year": "1989"
},
{
"article-title": "Rinsing with chlorhexidine gluconate solution after brushing and flossing teeth: A systematic review of effectiveness",
"author": "Kolahi",
"first-page": "605",
"journal-title": "Quintessence Int.",
"key": "ref_81",
"volume": "37",
"year": "2006"
},
{
"article-title": "Mouthwashes and their use in dentistry: A review",
"author": "Ouanounou",
"first-page": "22",
"journal-title": "Oral Health",
"key": "ref_82",
"volume": "1",
"year": "2021"
},
{
"DOI": "10.1128/AEM.02633-14",
"article-title": "Quaternary Ammonium Biocides: Efficacy in Application",
"author": "Gerba",
"doi-asserted-by": "crossref",
"first-page": "464",
"journal-title": "Appl. Environ. Microbiol.",
"key": "ref_83",
"volume": "81",
"year": "2015"
},
{
"DOI": "10.1016/j.cden.2015.06.002",
"article-title": "Can Chemical Mouthwash Agents Achieve Plaque/Gingivitis Control?",
"author": "Ciancio",
"doi-asserted-by": "crossref",
"first-page": "799",
"journal-title": "Dent. Clin. N. Am.",
"key": "ref_84",
"volume": "59",
"year": "2015"
},
{
"DOI": "10.5937/bjdm2301032M",
"article-title": "EO-based mouthwashes: Is there something that should be known?",
"author": "Nemoda",
"doi-asserted-by": "crossref",
"first-page": "32",
"journal-title": "Balk. J. Dent. Med.",
"key": "ref_85",
"volume": "27",
"year": "2023"
},
{
"DOI": "10.1016/j.jdsr.2018.07.001",
"article-title": "Evidence-based strategy for dental biofilms: Current evidence of mouthwashes on dental biofilm and gingivitis",
"author": "Takenaka",
"doi-asserted-by": "crossref",
"first-page": "33",
"journal-title": "Jpn. Dent. Sci. Rev.",
"key": "ref_86",
"volume": "55",
"year": "2019"
},
{
"DOI": "10.1016/j.identj.2023.08.011",
"article-title": "Mouthwashes: Alternatives and Future Directions",
"author": "Duane",
"doi-asserted-by": "crossref",
"first-page": "S89",
"journal-title": "Int. Dent. J.",
"key": "ref_87",
"volume": "73",
"year": "2023"
},
{
"DOI": "10.3390/pharmacy11010033",
"doi-asserted-by": "crossref",
"key": "ref_88",
"unstructured": "Radu, C.-M., Radu, C.C., Bochiș, S.-A., Arbănași, E.M., Lucan, A.I., Murvai, V.R., and Zaha, D.C. (2023). Revisiting the Therapeutic Effects of Essential Oils on the Oral Microbiome. Pharmacy, 11."
},
{
"DOI": "10.1111/ijcp.12707",
"article-title": "Practical use of povidone-iodine antiseptic in the maintenance of oral health and in the prevention and treatment of common oropharyngeal infections",
"author": "Kanagalingam",
"doi-asserted-by": "crossref",
"first-page": "1247",
"journal-title": "Int. J. Clin. Pract.",
"key": "ref_89",
"volume": "69",
"year": "2015"
},
{
"DOI": "10.1155/2020/8841722",
"article-title": "A Systematic Review of the Effect of Oral Rinsing with H2O2 on Clinical and Microbiological Parameters Related to Plaque, Gingivitis, and Microbes",
"author": "Muniz",
"doi-asserted-by": "crossref",
"first-page": "8841722",
"journal-title": "Int. J. Dent.",
"key": "ref_90",
"volume": "2020",
"year": "2020"
},
{
"DOI": "10.1128/CMR.12.1.147",
"article-title": "Antiseptics and Disinfectants: Activity, Action, and Resistance",
"author": "McDonnell",
"doi-asserted-by": "crossref",
"first-page": "147",
"journal-title": "Clin. Microbiol. Rev.",
"key": "ref_91",
"volume": "12",
"year": "1999"
},
{
"DOI": "10.1016/j.nmni.2021.100861",
"article-title": "The synergistic effect of turmeric aqueous extract and chitosan against multidrug-resistant bacteria",
"author": "Etemadi",
"doi-asserted-by": "crossref",
"first-page": "100861",
"journal-title": "New Microbes New Infect.",
"key": "ref_92",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1038/s41598-020-65007-y",
"doi-asserted-by": "crossref",
"key": "ref_93",
"unstructured": "Rodríguez Zorrilla, S., Blanco Carrión, A., García García, A., Galindo Moreno, P., Marichalar Mendía, X., Seoane Prado, R., and Estévez, A.J.P. (2020). Effect of antiseptic gels in the microbiologic colonization of the suture threads after oral surgery. Sci. Rep., 10."
},
{
"DOI": "10.1080/09593332808618893",
"article-title": "Antibacterial Effects of Chitosan Powder: Mechanisms of Action",
"author": "Andres",
"doi-asserted-by": "crossref",
"first-page": "1357",
"journal-title": "Environ. Technol.",
"key": "ref_94",
"volume": "28",
"year": "2007"
},
{
"DOI": "10.3390/md19120697",
"doi-asserted-by": "crossref",
"key": "ref_95",
"unstructured": "Hemmingsen, L.M., Škalko-Basnet, N., and Jøraholmen, M.W. (2021). The Expanded Role of Chitosan in Localized Antimicrobial Therapy. Mar. Drugs, 19."
},
{
"article-title": "Antimicrobial efficacy of different toothpastes and mouthrinses: An in vitro study",
"author": "Prasanth",
"first-page": "85",
"journal-title": "Dent. Res. J.",
"key": "ref_96",
"volume": "8",
"year": "2011"
},
{
"DOI": "10.26444/jpccr/142065",
"article-title": "Mechanism of action of triclosan as an endocrine-disrupting chemical with its impact on human health—Literature review",
"author": "Maksymowicz",
"doi-asserted-by": "crossref",
"first-page": "169",
"journal-title": "J. Pre-Clin. Clin. Res.",
"key": "ref_97",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.3390/ijms231911427",
"doi-asserted-by": "crossref",
"key": "ref_98",
"unstructured": "Marques, A.C., Mariana, M., and Cairrao, E. (2022). Triclosan and Its Consequences on the Reproductive, Cardiovascular and Thyroid Levels. Int. J. Mol. Sci., 23."
},
{
"DOI": "10.1080/10937404.2017.1281181",
"article-title": "Is Triclosan a neurotoxic agent?",
"author": "Ruszkiewicz",
"doi-asserted-by": "crossref",
"first-page": "104",
"journal-title": "J. Toxicol. Environ. Health Part B",
"key": "ref_99",
"volume": "20",
"year": "2017"
},
{
"DOI": "10.3390/antibiotics11060735",
"doi-asserted-by": "crossref",
"key": "ref_100",
"unstructured": "Sinicropi, M.S., Iacopetta, D., Ceramella, J., Catalano, A., Mariconda, A., Pellegrino, M., Saturnino, C., Longo, P., and Aquaro, S. (2022). Triclosan: A Small Molecule with Controversial Roles. Antibiotics, 11."
},
{
"DOI": "10.1186/s12903-020-01185-5",
"doi-asserted-by": "crossref",
"key": "ref_101",
"unstructured": "Halboub, E., Al-Maweri, S.A., Al-Wesabi, M., Al-Kamel, A., Shamala, A., Al-Sharani, A., and Koppolu, P. (2020). Efficacy of propolis-based mouthwashes on dental plaque and gingival inflammation: A systematic review. BMC Oral Health, 20."
},
{
"article-title": "Effectiveness of propolis in maintaining oral health: A scoping review",
"author": "Saeed",
"first-page": "167",
"journal-title": "Can. J. Dent. Hyg.",
"key": "ref_102",
"volume": "55",
"year": "2021"
},
{
"DOI": "10.4103/njcp.njcp_253_20",
"article-title": "Comparative Evaluation of the Cytotoxic Effects of Different Oral Antiseptics",
"author": "Tunc",
"doi-asserted-by": "crossref",
"first-page": "313",
"journal-title": "Niger. J. Clin. Pract.",
"key": "ref_103",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.3390/ijms21207538",
"doi-asserted-by": "crossref",
"key": "ref_104",
"unstructured": "Pignatelli, P., Fabietti, G., Ricci, A., Piattelli, A., and Curia, M.C. (2020). How Periodontal Disease and Presence of Nitric Oxide Reducing Oral Bacteria Can Affect Blood Pressure. Int. J. Mol. Sci., 21."
},
{
"DOI": "10.1016/j.identj.2024.07.005",
"article-title": "Impact of Mouthwash-Induced Oral Microbiome Disruption on Alzheimer’s Disease Risk: A Perspective Review",
"author": "Boulares",
"doi-asserted-by": "crossref",
"first-page": "45",
"journal-title": "Int. Dent. J.",
"key": "ref_105",
"volume": "75",
"year": "2025"
},
{
"DOI": "10.1159/000445688",
"article-title": "In vitro Impact of Limited Exposure to Subtherapeutic Concentrations of Chlorhexidine Gluconate on the Adhesion-Associated Attributes of Oral Candida Species",
"author": "Ellepola",
"doi-asserted-by": "crossref",
"first-page": "355",
"journal-title": "Med. Princ. Pract.",
"key": "ref_106",
"volume": "25",
"year": "2016"
},
{
"DOI": "10.1111/idh.12617",
"article-title": "Effects of antimicrobial mouthwashes on the human oral microbiome: Systematic review of controlled clinical trials",
"author": "Hassan",
"doi-asserted-by": "crossref",
"first-page": "128",
"journal-title": "Int. J. Dent. Hyg.",
"key": "ref_107",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.20944/preprints202406.0073.v1",
"doi-asserted-by": "crossref",
"key": "ref_108",
"unstructured": "Abdelrahman, S.M., El Samak, M., El-Baz, L.M.F., Hanora, A.M.S., Satyal, P., and Dosoky, N.S. (2024). Effects of Mint Oils on the Human Oral Microbiome: A Pilot Study. Microorganisms, 12."
},
{
"DOI": "10.1038/s41598-019-44822-y",
"doi-asserted-by": "crossref",
"key": "ref_109",
"unstructured": "Verspecht, T., Rodriguez Herrero, E., Khodaparast, L., Khodaparast, L., Boon, N., Bernaerts, K.K., Quirynen, M., and Teughels, W. (2019). Development of antiseptic adaptation and cross-adapatation in selected oral pathogens in vitro. Sci. Rep., 9."
},
{
"DOI": "10.1080/08037051.2019.1680270",
"article-title": "Over-the-counter mouthwash use, nitric oxide and hypertension risk",
"author": "Joshipura",
"doi-asserted-by": "crossref",
"first-page": "103",
"journal-title": "Blood Press.",
"key": "ref_110",
"volume": "29",
"year": "2020"
},
{
"DOI": "10.1093/ajh/hpu192",
"article-title": "Antibacterial Mouthwash Blunts Oral Nitrate Reduction and Increases Blood Pressure in Treated Hypertensive Men and Women",
"author": "Bondonno",
"doi-asserted-by": "crossref",
"first-page": "572",
"journal-title": "Am. J. Hypertens.",
"key": "ref_111",
"volume": "28",
"year": "2015"
},
{
"DOI": "10.1007/s11906-017-0725-2",
"article-title": "Oral Microbiome and Nitric Oxide: The Missing Link in the Management of Blood Pressure",
"author": "Bryan",
"doi-asserted-by": "crossref",
"first-page": "33",
"journal-title": "Curr. Hypertens. Rep.",
"key": "ref_112",
"volume": "19",
"year": "2017"
},
{
"DOI": "10.1016/j.niox.2017.09.004",
"article-title": "Over-the-counter mouthwash use and risk of pre-diabetes/diabetes",
"author": "Joshipura",
"doi-asserted-by": "crossref",
"first-page": "14",
"journal-title": "Nitric Oxide",
"key": "ref_113",
"volume": "71",
"year": "2017"
},
{
"DOI": "10.1038/sj.bdj.2018.1020",
"article-title": "Mouthwash use and risk of diabetes",
"author": "Preshaw",
"doi-asserted-by": "crossref",
"first-page": "923",
"journal-title": "Br. Dent. J.",
"key": "ref_114",
"volume": "225",
"year": "2018"
},
{
"DOI": "10.3389/froh.2025.1488286",
"doi-asserted-by": "crossref",
"key": "ref_115",
"unstructured": "Guo, K., Joshipura, K., Ricart, K., Patel, R.P., Gower, B.A., Andriankaja, O.M., and Bermudez, E.M. (2025). Association of over-the-counter mouthwash use with markers of nitric oxide metabolism, inflammation, and endothelial function—A cross-sectional study. Front. Oral Health, 6."
},
{
"DOI": "10.1080/00325481.2020.1829854",
"article-title": "Dentists and physicians’ practices meet once again: Potential unfavorable clinical effects of frequent mouthwash use",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "123",
"journal-title": "Postgrad. Med.",
"key": "ref_116",
"volume": "133",
"year": "2021"
},
{
"DOI": "10.18203/issn.2454-5929.ijohns20194927",
"article-title": "The effect of iodine in patients using povidone-iodine mouth wash on thyroid function",
"author": "Murugesan",
"doi-asserted-by": "crossref",
"first-page": "1562",
"journal-title": "Int. J. Otorhinolaryngol. Head Neck Surg.",
"key": "ref_117",
"volume": "5",
"year": "2019"
},
{
"DOI": "10.1007/s40121-019-00260-x",
"article-title": "Infectious Disease Management and Control with Povidone Iodine",
"author": "Eggers",
"doi-asserted-by": "crossref",
"first-page": "581",
"journal-title": "Infect. Dis. Ther.",
"key": "ref_118",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1016/j.oraloncology.2014.03.001",
"article-title": "Oral health, dental care and mouthwash associated with upper aerodigestive tract cancer risk in Europe: The ARCAGE study",
"author": "Ahrens",
"doi-asserted-by": "crossref",
"first-page": "616",
"journal-title": "Oral Oncol.",
"key": "ref_119",
"volume": "50",
"year": "2014"
},
{
"DOI": "10.1016/j.jebdp.2020.101407",
"article-title": "Mouthwash With Alcohol and Oral Carcinogenesis: Systematic Review and Meta-analysis",
"doi-asserted-by": "crossref",
"first-page": "101407",
"journal-title": "J. Evid. Based Dent. Pract.",
"key": "ref_120",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1016/j.rmed.2021.106475",
"article-title": "The role of oral microbiome in respiratory health and diseases",
"author": "Pathak",
"doi-asserted-by": "crossref",
"first-page": "106475",
"journal-title": "Respir. Med.",
"key": "ref_121",
"volume": "185",
"year": "2021"
},
{
"DOI": "10.20944/preprints202411.0213.v1",
"doi-asserted-by": "crossref",
"key": "ref_122",
"unstructured": "Wang, Z., Kaplan, R.C., Burk, R.D., and Qi, Q. (2024). The Oral Microbiota, Microbial Metabolites, and Immuno-Inflammatory Mechanisms in Cardiovascular Disease. Int. J. Mol. Sci., 25."
},
{
"DOI": "10.3390/diagnostics13203184",
"doi-asserted-by": "crossref",
"key": "ref_123",
"unstructured": "Lê, S., Cecchin-Albertoni, C., Thomas, C., Kemoun, P., Minty, M., and Blasco-Baque, V. (2023). The Role of Dysbiotic Oral Microbiota in Cardiometabolic Diseases: A Narrative Review. Diagnostics, 13."
},
{
"DOI": "10.1590/1806-9282.20220197",
"article-title": "The role of gut dysbiosis-associated inflammation in heart failure",
"author": "Siqueira",
"doi-asserted-by": "crossref",
"first-page": "1120",
"journal-title": "Rev. Assoc. Med. Bras.",
"key": "ref_124",
"volume": "68",
"year": "2022"
},
{
"DOI": "10.3855/jidc.10980",
"article-title": "The presence of periopathogenic bacteria in subgingival and atherosclerotic plaques—An age related comparative analysis",
"author": "Kannosh",
"doi-asserted-by": "crossref",
"first-page": "1088",
"journal-title": "J. Infect. Dev. Ctries.",
"key": "ref_125",
"volume": "12",
"year": "2018"
},
{
"DOI": "10.1902/jop.2013.134006",
"article-title": "Inflammatory mechanisms linking periodontal diseases to cardiovascular diseases",
"author": "Schenkein",
"doi-asserted-by": "crossref",
"first-page": "S51",
"journal-title": "J. Periodontol.",
"key": "ref_126",
"volume": "84",
"year": "2013"
},
{
"DOI": "10.1111/eos.12423",
"article-title": "Mediators between oral dysbiosis and cardiovascular diseases",
"author": "Liljestrand",
"doi-asserted-by": "crossref",
"first-page": "26",
"journal-title": "Eur. J. Oral Sci.",
"key": "ref_127",
"volume": "126",
"year": "2018"
},
{
"DOI": "10.1038/s41368-022-00163-7",
"article-title": "Oral microbiota in human systematic diseases",
"author": "Peng",
"doi-asserted-by": "crossref",
"first-page": "14",
"journal-title": "Int. J. Oral Sci.",
"key": "ref_128",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.3390/ijms24065231",
"doi-asserted-by": "crossref",
"key": "ref_129",
"unstructured": "Kozak, M., and Pawlik, A. (2023). The Role of the Oral Microbiome in the Development of Diseases. Int. J. Mol. Sci., 24."
},
{
"DOI": "10.1172/jci.insight.152346",
"article-title": "Inflammation-type dysbiosis of the oral microbiome associates with the duration of COVID-19 symptoms and long COVID",
"author": "Haran",
"doi-asserted-by": "crossref",
"first-page": "e152346",
"journal-title": "JCI Insight",
"key": "ref_130",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.3389/fcimb.2023.1193340",
"doi-asserted-by": "crossref",
"key": "ref_131",
"unstructured": "Tan, L., Zhong, M.-M., Liu, Q., Chen, Y., Zhao, Y.-Q., Zhao, J., Dusenge, M.A., Feng, Y., Ye, Q., and Hu, J. (2023). Potential interaction between the oral microbiota and COVID-19: A meta-analysis and bioinformatics prediction. Front. Cell. Infect. Microbiol., 13."
},
{
"DOI": "10.1016/j.jebdp.2020.101498",
"article-title": "Periodontitis May Be Associated With Respiratory Diseases Such as Asthma, COPD, and Pneumonia",
"author": "Kelly",
"doi-asserted-by": "crossref",
"first-page": "101498",
"journal-title": "J. Evid. Based Dent. Pract.",
"key": "ref_132",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.3389/fonc.2018.00520",
"doi-asserted-by": "crossref",
"key": "ref_133",
"unstructured": "Yang, J., Mu, X., Wang, Y., Zhu, D., Zhang, J., Liang, C., Zhang, Y., Li, H., Chen, X., and Wang, W. (2018). Dysbiosis of the Salivary Microbiome Is Associated with Non-smoking Female Lung Cancer and Correlated with Immunocytochemistry Markers. Front. Oncol., 8."
},
{
"DOI": "10.1128/cmr.00150-24",
"article-title": "Oral microbiota and respiratory diseases: Advances and perspectives",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "e00150-24",
"journal-title": "Clin. Microbiol. Rev.",
"key": "ref_134",
"volume": "38",
"year": "2025"
},
{
"DOI": "10.1111/omi.12227",
"article-title": "Periodontal infection with Porphyromonas gingivalis induces preterm birth and lower birth weight in rats",
"author": "Liang",
"doi-asserted-by": "crossref",
"first-page": "312",
"journal-title": "Mol. Oral Microbiol.",
"key": "ref_135",
"volume": "33",
"year": "2018"
},
{
"DOI": "10.1902/jop.2011.110035",
"article-title": "Oral Health Behaviors, Periodontal Disease, and Pathogens in Preeclampsia: A Case-Control Study in Korea",
"author": "Ha",
"doi-asserted-by": "crossref",
"first-page": "1685",
"journal-title": "J. Periodontol.",
"key": "ref_136",
"volume": "82",
"year": "2011"
},
{
"DOI": "10.1001/jamanetworkopen.2022.47632",
"article-title": "Association of Chlorhexidine Use and Scaling and Root Planing With Birth Outcomes in Pregnant Individuals With Periodontitis",
"author": "Merchant",
"doi-asserted-by": "crossref",
"first-page": "e2247632",
"journal-title": "JAMA Netw. Open",
"key": "ref_137",
"volume": "5",
"year": "2022"
},
{
"article-title": "Oral Microbiome and Adverse Pregnancy Outcomes: An Update",
"author": "Ali",
"first-page": "6",
"journal-title": "Online J. Health Allied Sci.",
"key": "ref_138",
"volume": "21",
"year": "2022"
},
{
"DOI": "10.1159/000047484",
"article-title": "Effect of Long–Term Consumption of a Probiotic Bacterium, Lactobacillus rhamnosus GG, in Milk on Dental Caries and Caries Risk in Children",
"author": "Hatakka",
"doi-asserted-by": "crossref",
"first-page": "412",
"journal-title": "Caries Res.",
"key": "ref_139",
"volume": "35",
"year": "2001"
},
{
"article-title": "Effect of Probiotic Curd on Salivary pH and Streptococcus mutans: A Double Blind Parallel Randomized Controlled Trial",
"author": "Srivastava",
"first-page": "ZC13",
"journal-title": "J. Clin. Diagn. Res.",
"key": "ref_140",
"volume": "10",
"year": "2016"
},
{
"article-title": "Efficacy of Probiotics Compared to Chlorhexidine Mouthwash in Improving Periodontal Status: A Systematic Review and Meta-Analysis",
"author": "Firoozi",
"first-page": "4013004",
"journal-title": "Int. J. Dent.",
"key": "ref_141",
"volume": "2023",
"year": "2023"
},
{
"DOI": "10.3390/nu14051036",
"doi-asserted-by": "crossref",
"key": "ref_142",
"unstructured": "Gheisary, Z., Mahmood, R., Harri Shivanantham, A., Liu, J., Lieffers, J.R.L., Papagerakis, P., and Papagerakis, S. (2022). The Clinical, Microbiological, and Immunological Effects of Probiotic Supplementation on Prevention and Treatment of Periodontal Diseases: A Systematic Review and Meta-Analysis. Nutrients, 14."
},
{
"DOI": "10.3390/ph16091313",
"doi-asserted-by": "crossref",
"key": "ref_143",
"unstructured": "Inchingolo, F., Inchingolo, A.M., Malcangi, G., De Leonardis, N., Sardano, R., Pezzolla, C., Di Cosola, M., Fiorillo, L., Cantore, S., and Palmieri, B. (2023). The Benefits of Probiotics on Oral Health: Systematic Review of the Literature. Pharmaceuticals, 16."
},
{
"DOI": "10.1186/s40168-022-01307-x",
"doi-asserted-by": "crossref",
"key": "ref_144",
"unstructured": "Holmes, Z.C., Villa, M.M., Durand, H.K., Jiang, S., Dallow, E.P., Petrone, B.L., Silverman, J.D., Lin, P.-H., and David, L.A. (2022). Microbiota responses to different prebiotics are conserved within individuals and associated with habitual fiber intake. Microbiome, 10."
},
{
"DOI": "10.1002/9781394167227.ch11",
"doi-asserted-by": "crossref",
"key": "ref_145",
"unstructured": "Surana, K., Ahire, E.D., Pawar, R., Khairnar, R., Mahajan, S., Kshirsagar, S., Talele, S.G., Thombre, N., Ahire, B., and Keservani, R.K. (2022). Oral Health and Prebiotics. Prebiotics and Probiotics in Disease Regulation and Management, Wiley."
},
{
"DOI": "10.1111/jcpe.12700",
"article-title": "Nutritional stimulation of commensal oral bacteria suppresses pathogens: The prebiotic concept",
"author": "Slomka",
"doi-asserted-by": "crossref",
"first-page": "344",
"journal-title": "J. Clin. Periodontol.",
"key": "ref_146",
"volume": "44",
"year": "2017"
},
{
"DOI": "10.1038/s41598-020-69931-x",
"doi-asserted-by": "crossref",
"key": "ref_147",
"unstructured": "Rosier, B.T., Buetas, E., Moya-Gonzalvez, E.M., Artacho, A., and Mira, A. (2020). Nitrate as a potential prebiotic for the oral microbiome. Sci. Rep., 10."
},
{
"DOI": "10.3390/ijms21144895",
"doi-asserted-by": "crossref",
"key": "ref_148",
"unstructured": "Magrin, G.L., Strauss, F.J., Benfatti, C.A.M., Maia, L.C., and Gruber, R. (2020). Effects of Short-Chain Fatty Acids on Human Oral Epithelial Cells and the Potential Impact on Periodontal Disease: A Systematic Review of In Vitro Studies. Int. J. Mol. Sci., 21."
},
{
"DOI": "10.3390/biomedicines11102749",
"doi-asserted-by": "crossref",
"key": "ref_149",
"unstructured": "Leonov, G.E., Varaeva, Y.R., Livantsova, E.N., and Starodubova, A.V. (2023). The Complicated Relationship of Short-Chain Fatty Acids and Oral Microbiome: A Narrative Review. Biomedicines, 11."
},
{
"DOI": "10.3389/fcimb.2023.1120995",
"doi-asserted-by": "crossref",
"key": "ref_150",
"unstructured": "Homayouni Rad, A., Pourjafar, H., and Mirzakhani, E. (2023). A comprehensive review of the application of probiotics and postbiotics in oral health. Front. Cell. Infect. Microbiol., 13."
},
{
"DOI": "10.3390/ijms222413475",
"doi-asserted-by": "crossref",
"key": "ref_151",
"unstructured": "Jastrząb, R., Graczyk, D., and Siedlecki, P. (2021). Molecular and Cellular Mechanisms Influenced by Postbiotics. Int. J. Mol. Sci., 22."
},
{
"DOI": "10.3390/nu15020291",
"doi-asserted-by": "crossref",
"key": "ref_152",
"unstructured": "Ma, L., Tu, H., and Chen, T. (2023). Postbiotics in Human Health: A Narrative Review. Nutrients, 15."
},
{
"DOI": "10.1007/s12602-024-10238-y",
"doi-asserted-by": "crossref",
"key": "ref_153",
"unstructured": "Rui, W., Zhong, S., Li, X., Tang, X., Wang, L., and Yang, J. (2024). Evaluating the Role of Postbiotics in the Modulation of Human Oral Microbiota: A Randomized Controlled Clinical Trial. Probiotics Antimicrob Proteins."
},
{
"DOI": "10.3390/molecules29153466",
"doi-asserted-by": "crossref",
"key": "ref_154",
"unstructured": "Hetta, H.F., Ramadan, Y.N., Rashed, Z.I., Alharbi, A.A., Alsharef, S., Alkindy, T.T., Alkhamali, A., Albalawi, A.S., Battah, B., and Donadu, M.G. (2024). Quorum Sensing Inhibitors: An Alternative Strategy to Win the Battle against Multidrug-Resistant (MDR) Bacteria. Molecules, 29."
},
{
"DOI": "10.3390/pharmaceutics14122740",
"doi-asserted-by": "crossref",
"key": "ref_155",
"unstructured": "Polizzi, A., Donzella, M., Nicolosi, G., Santonocito, S., Pesce, P., and Isola, G. (2022). Drugs for the Quorum Sensing Inhibition of Oral Biofilm: New Frontiers and Insights in the Treatment of Periodontitis. Pharmaceutics, 14."
},
{
"DOI": "10.1111/odi.13689",
"article-title": "Quorum sensing systems as a new target to prevent biofilm-related oral diseases",
"author": "Muras",
"doi-asserted-by": "crossref",
"first-page": "307",
"journal-title": "Oral Dis.",
"key": "ref_156",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.18388/abp.2009_2512",
"article-title": "Quenching of acyl-homoserine lactone-dependent quorum sensing by enzymatic disruption of signal molecules",
"author": "Czajkowski",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Acta Biochim. Pol.",
"key": "ref_157",
"volume": "56",
"year": "2009"
},
{
"DOI": "10.1080/1040841X.2022.2038082",
"article-title": "Bioactive compounds: A goldmine for defining new strategies against pathogenic bacterial biofilms?",
"author": "Pompilio",
"doi-asserted-by": "crossref",
"first-page": "117",
"journal-title": "Crit. Rev. Microbiol.",
"key": "ref_158",
"volume": "49",
"year": "2023"
},
{
"DOI": "10.1007/s00784-023-04878-7",
"article-title": "Precision periodontal care: From omics discoveries to chairside diagnostics",
"author": "Bostanci",
"doi-asserted-by": "crossref",
"first-page": "971",
"journal-title": "Clin. Oral. Investig.",
"key": "ref_159",
"volume": "27",
"year": "2023"
},
{
"DOI": "10.3389/fcimb.2021.747814",
"doi-asserted-by": "crossref",
"key": "ref_160",
"unstructured": "Wirth, R., Pap, B., Maróti, G., Vályi, P., Komlósi, L., Barta, N., Strang, O., Minárovits, J., and Kovács, K.L. (2021). Toward Personalized Oral Diagnosis: Distinct Microbiome Clusters in Periodontitis Biofilms. Front. Cell. Infect. Microbiol., 11."
},
{
"DOI": "10.1016/j.archoralbio.2019.05.023",
"article-title": "Applications of the oral microbiome in personalized dentistry",
"author": "Belibasakis",
"doi-asserted-by": "crossref",
"first-page": "7",
"journal-title": "Arch. Oral Biol.",
"key": "ref_161",
"volume": "104",
"year": "2019"
},
{
"DOI": "10.7326/M18-0850",
"article-title": "PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation",
"author": "Tricco",
"doi-asserted-by": "crossref",
"first-page": "467",
"journal-title": "Ann. Intern. Med.",
"key": "ref_162",
"volume": "169",
"year": "2018"
}
],
"reference-count": 162,
"references-count": 162,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2079-6382/14/8/815"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Effects of Antiseptic Formulations on Oral Microbiota and Related Systemic Diseases: A Scoping Review",
"type": "journal-article",
"update-policy": "https://doi.org/10.3390/mdpi_crossmark_policy",
"volume": "14"
}
angjelova