Characteristics of patients with non-severe infections of different SARS-CoV-2 omicron subvariants in China
et al., Frontiers in Medicine, doi:10.3389/fmed.2024.1511227, Dec 2024
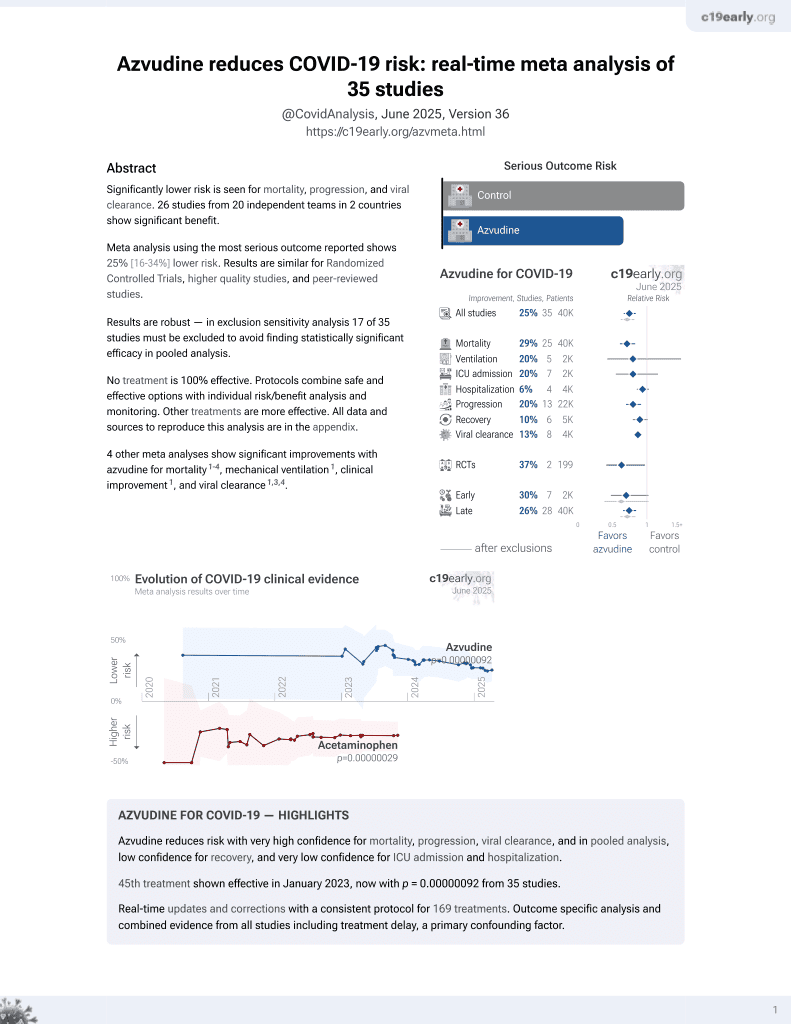
Azvudine for COVID-19
48th treatment shown to reduce risk in
January 2023, now with p = 0.0000000041 from 40 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 244 non-severe COVID-19 patients in China infected with Omicron BA.2.76 or BA.5.1 subvariants, showing improved viral clearance with azvudine.
Viral load measured by PCR may not accurately reflect infectious virus measured by viral culture. Porter et al. show that viral load early in infection was correlated with infectious virus, but viral load late in infection could be high even with low or undetectable infectious virus. Assessing viral load later in infection may underestimate reductions in infectious virus with treatment.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments4.
This study is excluded in the after exclusion results of meta-analysis:
substantial unadjusted confounding by indication likely.
|
time to viral-, 9.1% lower, relative time 0.91, p = 0.03, treatment 121, control 123.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Xiong et al., Real-world data of Azvudine-induced hepatotoxicity among hospitalized COVID-19 patients in China: a retrospective case-control study, Frontiers in Pharmacology, doi:10.3389/fphar.2025.1558054.
2.
Wang et al., Development and validation of a nomogram to assess the occurrence of liver dysfunction in patients with COVID-19 pneumonia in the ICU, BMC Infectious Diseases, doi:10.1186/s12879-025-10684-1.
Yuan et al., 18 Dec 2024, retrospective, China, peer-reviewed, 10 authors, study period 10 August, 2022 - 9 October, 2022.
Contact: daieh2008@126.com, yongzhelipumch@126.com.
Characteristics of patients with non-severe infections of different SARS-CoV-2 omicron subvariants in China
Frontiers in Medicine, doi:10.3389/fmed.2024.1511227
Objective: The aim of this study was to explore the clinical characteristics of patients infected with different Omicron subvariants presenting non-severe disease, evaluate the safety and efficacy of Azvudine for treatment of COVID-19, in order to broaden understanding of Omicron subvariant infections. Method: A total of 244 individuals with Omicron subvariant (BA.2.76, n = 158; BA.5.1, n = 86) were included in the study. Demographic, clinical, and laboratory data of the study participants were collected and analyzed. Result: Patients infected with BA.5.1 exhibited a higher incidence of clinical symptoms like fatigue (25.58% vs. 2.53%, p < 0.001), headache/dizziness (12.79% vs. 4.43%, p = 0.017), nausea/vomiting (10.47% vs. 1.27%, p = 0.002), viral loads and inflammatory factors, and shorter virus shedding time than those with BA.2.76. There are 28.1% patients reporting mild adverse events following Azvudine administration. After treatment, the levels of anti-SARS-CoV-2 IgG/ IgM, white blood cell, and lymphocyte obviously increased, while C-reactive protein, procalcitonin, and D-dimer reduced. Azvudine speeded up the time for virus clearance compared to control treatment (10 vs. 11 days, p = 0.032). Low lymphocyte counts (odd ratio (OR) = 0.607, p = 0.001) and anti-SARS-CoV-2 IgG titer (OR = 0.990, p = 0.028) were the independent risk factors for long nucleic acid negativization duration after infection. Patients with pneumonia were often accompanied by dyspnea, fatigue and high level of D-dimer. Dyspnea (OR = 10.176, p = 0.019) could be used to identify the occurrence of pneumonia in patients infected with Omicron.
Conclusion: The study demonstrated the difference in clinical and laboratory parameters between patients infected with Omicron BA.2.76 and BA.5.1, as well as the safety and efficacy of Azvudine therapy. Our study linked patient manifestations to Omicron subvariant, treatment, and clinical outcomes, which is conducive to healthcare providers/policymakers to revise and implement appropriate countermeasures, facilitating appropriately advise for individuals with Omicron subvariant infections.
Ethics statement The study was approved by the Ethics Committee of the Fifth Hospital of Shijiazhuang (2022001). Informed consent was obtained from all participants. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
Funding The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by Key Research and Development Plan of Hebei Province, Special Health Innovation Project (22377744D), the Beijing Natural
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1511227/..
References
Adjei, Hong, Molinari, Bull-Otterson, Ajani et al., Mortality risk among patients hospitalized primarily for COVID-19 during the omicron and Delta variant pandemic periods -United States, April 2020-June 2022, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm7137a4
Castro Dopico, Ols, Lore, Hedestam, Immunity to SARS-CoV-2 induced by infection or vaccination, J Intern Med, doi:10.1111/joim.13372
Chen, Tian, Efficacy and safety of azvudine in patients with COVID-19: a systematic review and meta-analysis, Heliyon, doi:10.1016/j.heliyon.2023.e20153
Chen, Wang, Hozumi, Liu, Qiu et al., Emerging dominant SARS-CoV-2 variants, J Chem Inf Model, doi:10.1021/acs.jcim.2c01352
De Souza, Cabral, Da Silva, Arruda, Cabral et al., Phase III, randomized, double-blind, placebo-controlled clinical study: a study on the safety and clinical efficacy of AZVUDINE in moderate COVID-19 patients, Front Med, doi:10.3389/fmed.2023.1215916
Fiolet, Kherabi, Macdonald, Ghosn, Peiffer-Smadja, Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV-2 and variants of concern: a narrative review, Clin Microbiol Infect, doi:10.1016/j.cmi.2021.10.005
Groza, Totschnig, Wenisch, Atamaniuk, Zoufaly, A retrospective analysis of clinical features of patients hospitalized with SARS-CoV-2 omicron variants BA, 1 and BA, doi:10.1038/s41598-023-34712-9
Guo, Liu, Gu, Jiang, Yang et al., Distinct and relatively mild clinical characteristics of SARS-CoV-2 BA.5 infections against BA.2, Signal Transduct Target Ther, doi:10.1038/s41392-023-01443-2
He, Fang, Yang, Association between immunity and viral shedding duration in non-severe SARS-CoV-2 omicron variant-infected patients, Front Public Health, doi:10.3389/fpubh.2022.1032957
Huo, Yu, Shen, Pan, Li et al., A comparison of clinical characteristics of infections with SARS-CoV-2 omicron subvariants BF.7.14 and BA.5.2.48 -China, China CDC Wkly, doi:10.46234/ccdcw2023.096
Ikuse, Aizawa, Yamanaka, Hasegawa, Hayashi et al., Comparison of clinical characteristics of children infected with coronavirus disease 2019 between omicron variant BA.5 and BA.1/BA.2 in Japan, Pediatr Infect Dis J, doi:10.1097/INF.0000000000003894
Iwamura, Da Silva, Hummelgen, Pereira, Falcai et al., Immunity and inflammatory biomarkers in COVID-19: a systematic review, Rev Med Virol, doi:10.1002/rmv.2199
Jafarzadeh, Jafarzadeh, Nozari, Mokhtari, Nemati, Lymphopenia an important immunological abnormality in patients with COVID-19: possible mechanisms, Scand J Immunol, doi:10.1111/sji.12967
Kang, Park, Kim, Lim, Lee et al., Comparison of the clinical and virological characteristics of SARS-CoV-2 omicron BA.1/BA.2 and omicron BA.5 variants: a prospective cohort study, J Infect, doi:10.1016/j.jinf.2023.01.015
Karyakarte, Das, Dudhate, Agarasen, Pillai et al., Clinical characteristics and outcomes of laboratory-confirmed SARS-CoV-2 cases infected with omicron subvariants and the XBB recombinant variant, Cureus, doi:10.7759/cureus.35261
Khodeir, Shabana, Alkhamiss, Rasheed, Alsoghair et al., Early prediction keys for COVID-19 cases progression: a meta-analysis, J Infect Public Health, doi:10.1016/j.jiph.2021.03.001
Lee, Hwang, Kim, Chung, Jeong et al., Comparison of clinical outcomes and imaging features in hospitalized patients with SARS-CoV-2 omicron subvariants, Radiology, doi:10.1148/radiol.230653
Lewnard, Hong, Kim, Shaw, Lewin et al., Association of SARS-CoV-2 BA.4/BA.5 omicron lineages with immune escape and clinical outcome, Nat Commun, doi:10.1038/s41467-023-37051-5
Li, Lin, Chen, Li, Li et al., Unvaccinated children are an important link in the transmission of SARS-CoV-2 Delta variant (B1.617.2): comparative clinical evidence from a recent community surge, Front Cell Infect Microbiol, doi:10.3389/fcimb.2022.814782
Li, Zhu, Yu, Qian, Huang et al., The effects of vaccination on the disease severity and factors for viral clearance and hospitalization in omicron-infected patients: a retrospective observational cohort study from recent regional outbreaks in China, Front Cell Infect Microbiol, doi:10.3389/fcimb.2022.988694
Mistry, Barmania, Mellet, Peta, Strydom et al., SARS-CoV-2 variants, vaccines, and host immunity, Front Immunol, doi:10.3389/fimmu.2021.809244
Napoli, Benincasa, Criscuolo, Faenza, Liberato et al., Immune reactivity during COVID-19: implications for treatment, Immunol Lett, doi:10.1016/j.imlet.2021.01.001
Savellini, Anichini, Cusi, SARS-CoV-2 omicron sub-lineages differentially modulate interferon response in human lung epithelial cells, Virus Res, doi:10.1016/j.virusres.2023.199134
Shang, Fu, Geng, Zhang, Zhang et al., Azvudine therapy of common COVID-19 in hemodialysis patients, J Med Virol, doi:10.1002/jmv.29007
Sun, Wang, Dong, Xu, Evolutionary analysis of omicron variant BF.7 and BA.5.2 pandemic in China, J Biosaf Biosecur, doi:10.1016/j.jobb.2023.01.002
Suzuki, Yamasoba, Kimura, Wang, Kishimoto et al., Attenuated fusogenicity and pathogenicity of SARS-CoV-2 omicron variant, Nature, doi:10.1038/s41586-022-04462-1
Valyi-Nagy, Uher, Rakoczi, Szekanecz, Adaptive immunity to viruses: what did we learn from SARS-CoV-2 infection?, Int J Mol Sci
Wang, Xie, Wang, Fan, Zhang et al., Effectiveness of azvudine in reducing mortality of COVID-19 patients: a systematic review and meta-analysis, Virol J, doi:10.1186/s12985-024-02316-y
Yang, Wang, Jiang, Zhang, Zhang et al., Oral azvudine for mildto-moderate COVID-19 in high risk, nonhospitalized adults: results of a real-world study, J Med Virol, doi:10.1002/jmv.28947
Yang, Wang, Wang, Zhang, Han, Cost-effectiveness of Azvudine for high-risk outpatients with mild-to-moderate coronavirus disease 2019 in China, Clin Ther, doi:10.1016/j.clinthera.2024.07.009
Yin, Lu, Jiao, Lin, Wang et al., Characteristics and related factors of viral nucleic acid negative conversion in children infected with omicron variant strain of SARS-CoV-2, Zhonghua Er Ke Za Zhi, doi:10.3760/cma.j.cn112140-20220623-00582
Yu, Chang, Azvudine (FNC): a promising clinical candidate for COVID-19 treatment, Signal Transduct Target Ther, doi:10.1038/s41392-020-00351-z
Yu, Chang, The first Chinese oral anti-COVID-19 drug Azvudine launched, Innovation, doi:10.1016/j.xinn.2022.100321
Zhan, Gao, Liu, Zhang, Li et al., Booster shot of inactivated SARS-CoV-2 vaccine induces potent immune responses in people living with HIV, J Med Virol, doi:10.1002/jmv.28428
DOI record:
{
"DOI": "10.3389/fmed.2024.1511227",
"ISSN": [
"2296-858X"
],
"URL": "http://dx.doi.org/10.3389/fmed.2024.1511227",
"abstract": "<jats:sec><jats:title>Objective</jats:title><jats:p>The aim of this study was to explore the clinical characteristics of patients infected with different Omicron subvariants presenting non-severe disease, evaluate the safety and efficacy of Azvudine for treatment of COVID-19, in order to broaden understanding of Omicron subvariant infections.</jats:p></jats:sec><jats:sec><jats:title>Method</jats:title><jats:p>A total of 244 individuals with Omicron subvariant (BA.2.76, <jats:italic>n</jats:italic> = 158; BA.5.1, <jats:italic>n</jats:italic> = 86) were included in the study. Demographic, clinical, and laboratory data of the study participants were collected and analyzed.</jats:p></jats:sec><jats:sec><jats:title>Result</jats:title><jats:p>Patients infected with BA.5.1 exhibited a higher incidence of clinical symptoms like fatigue (25.58% vs. 2.53%, <jats:italic>p</jats:italic> &lt; 0.001), headache/dizziness (12.79% vs. 4.43%, <jats:italic>p</jats:italic> = 0.017), nausea/vomiting (10.47% vs. 1.27%, <jats:italic>p</jats:italic> = 0.002), viral loads and inflammatory factors, and shorter virus shedding time than those with BA.2.76. There are 28.1% patients reporting mild adverse events following Azvudine administration. After treatment, the levels of anti-SARS-CoV-2 IgG/IgM, white blood cell, and lymphocyte obviously increased, while C-reactive protein, procalcitonin, and D-dimer reduced. Azvudine speeded up the time for virus clearance compared to control treatment (10 vs. 11 days, <jats:italic>p</jats:italic> = 0.032). Low lymphocyte counts (odd ratio (OR) = 0.607, <jats:italic>p</jats:italic> = 0.001) and anti-SARS-CoV-2 IgG titer (OR = 0.990, <jats:italic>p</jats:italic> = 0.028) were the independent risk factors for long nucleic acid negativization duration after infection. Patients with pneumonia were often accompanied by dyspnea, fatigue and high level of D-dimer. Dyspnea (OR = 10.176, <jats:italic>p</jats:italic> = 0.019) could be used to identify the occurrence of pneumonia in patients infected with Omicron.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>The study demonstrated the difference in clinical and laboratory parameters between patients infected with Omicron BA.2.76 and BA.5.1, as well as the safety and efficacy of Azvudine therapy. Our study linked patient manifestations to Omicron subvariant, treatment, and clinical outcomes, which is conducive to healthcare providers/policymakers to revise and implement appropriate countermeasures, facilitating appropriately advise for individuals with Omicron subvariant infections.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fmed.2024.1511227"
],
"author": [
{
"affiliation": [],
"family": "Yuan",
"given": "Wenfang",
"sequence": "first"
},
{
"affiliation": [],
"family": "Liu",
"given": "Yongmei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhan",
"given": "Haoting",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wei",
"given": "Feng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Qian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gao",
"given": "Huixia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yan",
"given": "Huimin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Huang",
"given": "Tao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Yongzhe",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dai",
"given": "Erhei",
"sequence": "additional"
}
],
"container-title": "Frontiers in Medicine",
"container-title-short": "Front. Med.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2024,
12,
18
]
],
"date-time": "2024-12-18T06:47:20Z",
"timestamp": 1734504440000
},
"deposited": {
"date-parts": [
[
2024,
12,
18
]
],
"date-time": "2024-12-18T06:47:23Z",
"timestamp": 1734504443000
},
"indexed": {
"date-parts": [
[
2024,
12,
19
]
],
"date-time": "2024-12-19T05:14:20Z",
"timestamp": 1734585260989,
"version": "3.30.2"
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
12,
18
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
12,
18
]
],
"date-time": "2024-12-18T00:00:00Z",
"timestamp": 1734480000000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2024.1511227/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2024,
12,
18
]
]
},
"published-online": {
"date-parts": [
[
2024,
12,
18
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.3389/fimmu.2021.809244",
"article-title": "SARS-CoV-2 variants, vaccines, and host immunity",
"author": "Mistry",
"doi-asserted-by": "publisher",
"first-page": "809244",
"journal-title": "Front Immunol",
"key": "ref1",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/s41586-022-04462-1",
"article-title": "Attenuated fusogenicity and pathogenicity of SARS-CoV-2 omicron variant",
"author": "Suzuki",
"doi-asserted-by": "publisher",
"first-page": "700",
"journal-title": "Nature",
"key": "ref2",
"volume": "603",
"year": "2022"
},
{
"DOI": "10.15585/mmwr.mm7137a4",
"article-title": "Mortality risk among patients hospitalized primarily for COVID-19 during the omicron and Delta variant pandemic periods - United States, April 2020-June 2022",
"author": "Adjei",
"doi-asserted-by": "publisher",
"first-page": "1182",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "ref3",
"volume": "71",
"year": "2022"
},
{
"DOI": "10.7759/cureus.35261",
"article-title": "Clinical characteristics and outcomes of laboratory-confirmed SARS-CoV-2 cases infected with omicron subvariants and the XBB recombinant variant",
"author": "Karyakarte",
"doi-asserted-by": "publisher",
"first-page": "e35261",
"journal-title": "Cureus",
"key": "ref4",
"volume": "15",
"year": "2023"
},
{
"DOI": "10.1097/INF.0000000000003894",
"article-title": "Comparison of clinical characteristics of children infected with coronavirus disease 2019 between omicron variant BA.5 and BA.1/BA.2 in Japan",
"author": "Ikuse",
"doi-asserted-by": "publisher",
"first-page": "503",
"journal-title": "Pediatr Infect Dis J",
"key": "ref5",
"volume": "42",
"year": "2023"
},
{
"DOI": "10.1038/s41598-023-34712-9",
"article-title": "A retrospective analysis of clinical features of patients hospitalized with SARS-CoV-2 omicron variants BA.1 and BA.2",
"author": "Groza",
"doi-asserted-by": "publisher",
"first-page": "7896",
"journal-title": "Sci Rep",
"key": "ref6",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1016/j.virusres.2023.199134",
"article-title": "SARS-CoV-2 omicron sub-lineages differentially modulate interferon response in human lung epithelial cells",
"author": "Gori Savellini",
"doi-asserted-by": "publisher",
"first-page": "199134",
"journal-title": "Virus Res",
"key": "ref7",
"volume": "332",
"year": "2023"
},
{
"DOI": "10.1016/j.jobb.2023.01.002",
"article-title": "Evolutionary analysis of omicron variant BF.7 and BA.5.2 pandemic in China",
"author": "Sun",
"doi-asserted-by": "publisher",
"first-page": "14",
"journal-title": "J Biosaf Biosecur",
"key": "ref8",
"volume": "5",
"year": "2023"
},
{
"DOI": "10.46234/ccdcw2023.096",
"article-title": "A comparison of clinical characteristics of infections with SARS-CoV-2 omicron subvariants BF.7.14 and BA.5.2.48 - China, October-December 2022",
"author": "Huo",
"doi-asserted-by": "publisher",
"first-page": "511",
"journal-title": "China CDC Wkly",
"key": "ref9",
"volume": "5",
"year": "2023"
},
{
"DOI": "10.1021/acs.jcim.2c01352",
"article-title": "Emerging dominant SARS-CoV-2 variants",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "335",
"journal-title": "J Chem Inf Model",
"key": "ref10",
"volume": "63",
"year": "2023"
},
{
"DOI": "10.1148/radiol.230653",
"article-title": "Comparison of clinical outcomes and imaging features in hospitalized patients with SARS-CoV-2 omicron subvariants",
"author": "Lee",
"doi-asserted-by": "publisher",
"first-page": "e230653",
"journal-title": "Radiology",
"key": "ref11",
"volume": "308",
"year": "2023"
},
{
"DOI": "10.1038/s41392-023-01443-2",
"article-title": "Distinct and relatively mild clinical characteristics of SARS-CoV-2 BA.5 infections against BA.2",
"author": "Guo",
"doi-asserted-by": "publisher",
"first-page": "171",
"journal-title": "Signal Transduct Target Ther",
"key": "ref12",
"volume": "8",
"year": "2023"
},
{
"DOI": "10.1016/j.jinf.2023.01.015",
"article-title": "Comparison of the clinical and virological characteristics of SARS-CoV-2 omicron BA.1/BA.2 and omicron BA.5 variants: a prospective cohort study",
"author": "Kang",
"doi-asserted-by": "publisher",
"first-page": "e148",
"journal-title": "J Infect",
"key": "ref13",
"volume": "86",
"year": "2023"
},
{
"DOI": "10.1038/s41467-023-37051-5",
"article-title": "Association of SARS-CoV-2 BA.4/BA.5 omicron lineages with immune escape and clinical outcome",
"author": "Lewnard",
"doi-asserted-by": "publisher",
"first-page": "1407",
"journal-title": "Nat Commun",
"key": "ref14",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1038/s41392-020-00351-z",
"article-title": "Azvudine (FNC): a promising clinical candidate for COVID-19 treatment",
"author": "Yu",
"doi-asserted-by": "publisher",
"first-page": "236",
"journal-title": "Signal Transduct Target Ther",
"key": "ref15",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.xinn.2022.100321",
"article-title": "The first Chinese oral anti-COVID-19 drug Azvudine launched",
"author": "Yu",
"doi-asserted-by": "publisher",
"first-page": "100321",
"journal-title": "Innovation",
"key": "ref16",
"volume": "3",
"year": "2022"
},
{
"DOI": "10.1016/j.clinthera.2024.07.009",
"article-title": "Cost-effectiveness of Azvudine for high-risk outpatients with mild-to-moderate coronavirus disease 2019 in China",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "e1",
"journal-title": "Clin Ther",
"key": "ref17",
"volume": "46",
"year": "2024"
},
{
"key": "ref18",
"year": "2023"
},
{
"article-title": "National Health Commission and National Administration of Traditional Chinese Medicine. Novel Coronavirus Pneumonia Diagnosis and Treatment Plan (Trial Version 9)",
"first-page": "161",
"journal-title": "Chinese J Viral Dis",
"key": "ref19",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1111/joim.13372",
"article-title": "Immunity to SARS-CoV-2 induced by infection or vaccination",
"author": "Castro Dopico",
"doi-asserted-by": "publisher",
"first-page": "32",
"journal-title": "J Intern Med",
"key": "ref20",
"volume": "291",
"year": "2022"
},
{
"DOI": "10.1016/j.cmi.2021.10.005",
"article-title": "Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV-2 and variants of concern: a narrative review",
"author": "Fiolet",
"doi-asserted-by": "publisher",
"first-page": "202",
"journal-title": "Clin Microbiol Infect",
"key": "ref21",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1186/s12985-024-02316-y",
"article-title": "Effectiveness of azvudine in reducing mortality of COVID-19 patients: a systematic review and meta-analysis",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "46",
"journal-title": "Virol J",
"key": "ref22",
"volume": "21",
"year": "2024"
},
{
"DOI": "10.3389/fmed.2023.1215916",
"article-title": "Phase III, randomized, double-blind, placebo-controlled clinical study: a study on the safety and clinical efficacy of AZVUDINE in moderate COVID-19 patients",
"author": "de Souza",
"doi-asserted-by": "publisher",
"first-page": "1215916",
"journal-title": "Front Med",
"key": "ref23",
"volume": "10",
"year": "2023"
},
{
"DOI": "10.1016/j.heliyon.2023.e20153",
"article-title": "Efficacy and safety of azvudine in patients with COVID-19: a systematic review and meta-analysis",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "e20153",
"journal-title": "Heliyon",
"key": "ref24",
"volume": "9",
"year": "2023"
},
{
"DOI": "10.1002/jmv.28947",
"article-title": "Oral azvudine for mild-to-moderate COVID-19 in high risk, nonhospitalized adults: results of a real-world study",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "e28947",
"journal-title": "J Med Virol",
"key": "ref25",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.1002/jmv.29007",
"article-title": "Azvudine therapy of common COVID-19 in hemodialysis patients",
"author": "Shang",
"doi-asserted-by": "publisher",
"first-page": "e29007",
"journal-title": "J Med Virol",
"key": "ref26",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.3389/fcimb.2022.988694",
"article-title": "The effects of vaccination on the disease severity and factors for viral clearance and hospitalization in omicron-infected patients: a retrospective observational cohort study from recent regional outbreaks in China",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "988694",
"journal-title": "Front Cell Infect Microbiol",
"key": "ref27",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.3389/fcimb.2022.814782",
"article-title": "Unvaccinated children are an important link in the transmission of SARS-CoV-2 Delta variant (B1.617.2): comparative clinical evidence from a recent community surge",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "814782",
"journal-title": "Front Cell Infect Microbiol",
"key": "ref28",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.3389/fpubh.2022.1032957",
"article-title": "Association between immunity and viral shedding duration in non-severe SARS-CoV-2 omicron variant-infected patients",
"author": "He",
"doi-asserted-by": "publisher",
"first-page": "1032957",
"journal-title": "Front Public Health",
"key": "ref29",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.3760/cma.j.cn112140-20220623-00582",
"article-title": "Characteristics and related factors of viral nucleic acid negative conversion in children infected with omicron variant strain of SARS-CoV-2",
"author": "Yin",
"doi-asserted-by": "publisher",
"first-page": "1307",
"journal-title": "Zhonghua Er Ke Za Zhi",
"key": "ref30",
"volume": "60",
"year": "2022"
},
{
"DOI": "10.1111/sji.12967",
"article-title": "Lymphopenia an important immunological abnormality in patients with COVID-19: possible mechanisms",
"author": "Jafarzadeh",
"doi-asserted-by": "publisher",
"first-page": "e12967",
"journal-title": "Scand J Immunol",
"key": "ref31",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.3390/ijms232213951",
"article-title": "Adaptive immunity to viruses: what did we learn from SARS-CoV-2 infection?",
"author": "Valyi-Nagy",
"doi-asserted-by": "publisher",
"first-page": "13951",
"journal-title": "Int J Mol Sci",
"key": "ref32",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1016/j.jiph.2021.03.001",
"article-title": "Early prediction keys for COVID-19 cases progression: a meta-analysis",
"author": "Khodeir",
"doi-asserted-by": "publisher",
"first-page": "561",
"journal-title": "J Infect Public Health",
"key": "ref33",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1016/j.imlet.2021.01.001",
"article-title": "Immune reactivity during COVID-19: implications for treatment",
"author": "Napoli",
"doi-asserted-by": "publisher",
"first-page": "28",
"journal-title": "Immunol Lett",
"key": "ref34",
"volume": "231",
"year": "2021"
},
{
"DOI": "10.1002/rmv.2199",
"article-title": "Immunity and inflammatory biomarkers in COVID-19: a systematic review",
"author": "Iwamura",
"doi-asserted-by": "publisher",
"first-page": "e2199",
"journal-title": "Rev Med Virol",
"key": "ref35",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.1002/jmv.28428",
"article-title": "Booster shot of inactivated SARS-CoV-2 vaccine induces potent immune responses in people living with HIV",
"author": "Zhan",
"doi-asserted-by": "publisher",
"first-page": "e28428",
"journal-title": "J Med Virol",
"key": "ref36",
"volume": "95",
"year": "2023"
}
],
"reference-count": 36,
"references-count": 36,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2024.1511227/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Characteristics of patients with non-severe infections of different SARS-CoV-2 omicron subvariants in China",
"type": "journal-article",
"update-policy": "https://doi.org/10.3389/crossmark-policy",
"volume": "11"
}