Combating pan-coronavirus infection by indomethacin through simultaneously inhibiting viral replication and inflammatory response
et al., iScience, doi:10.1016/j.isci.2023.107631, Aug 2023
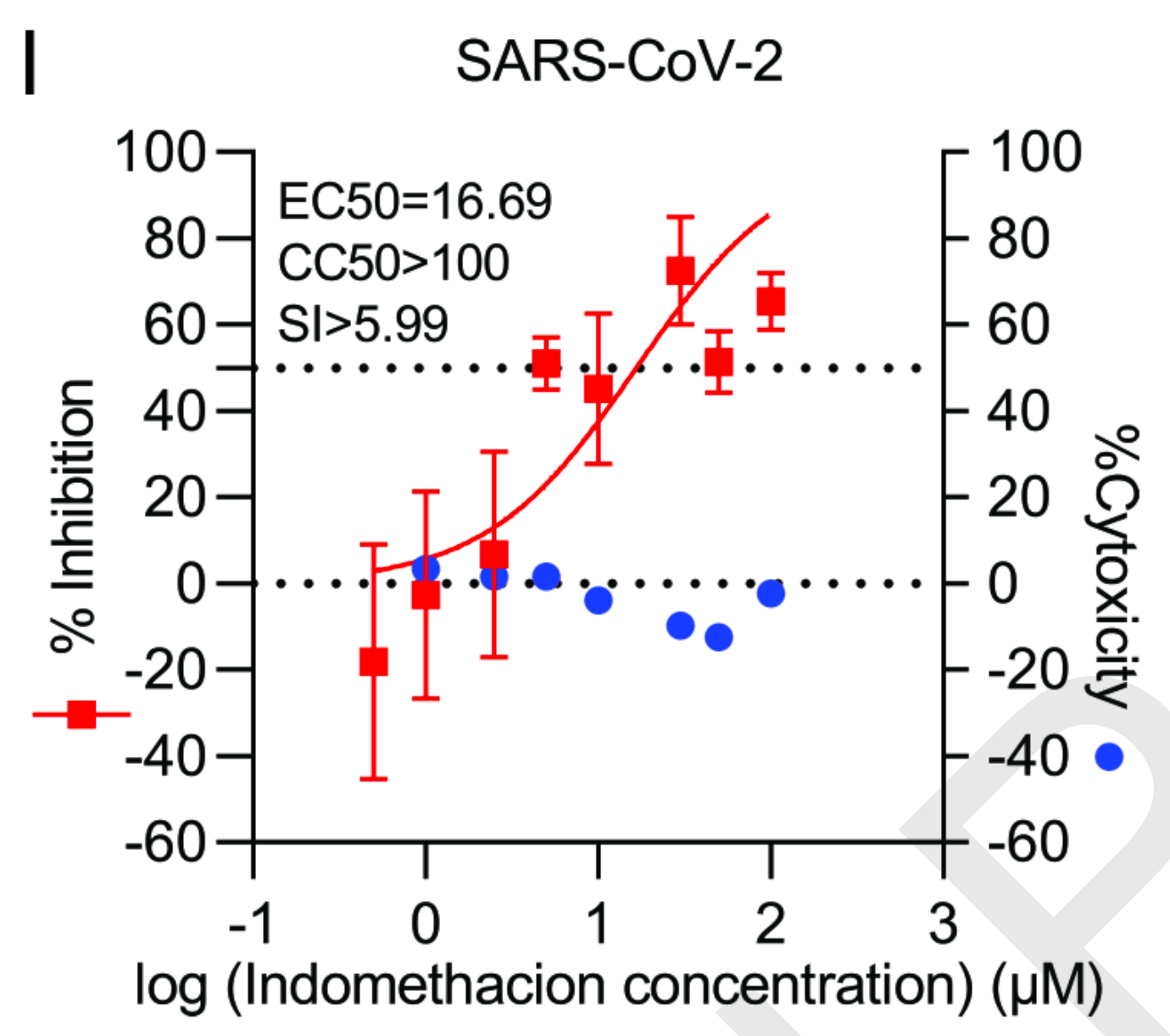
In vitro analysis of indomethacin for multiple human coronaviruses including SARS-CoV-2. Indomethacin exhibited antiviral activity against SARS-CoV-2 infection in human cell lines and lung airway organoid models. Treatment with indomethacin reduced SARS-CoV-2 viral RNA levels and infectious virus production. The anti-SARS-CoV-2 effect occurred at the post-entry stage of the viral life cycle. The EC50 (half maximal effective concentration) of indomethacin against SARS-CoV-2 was 16.69 μM, with a selectivity index around 6, indicating a reasonable therapeutic window between antiviral activity and cytotoxicity. Combining indomethacin with other antivirals showed synergistic effects.
7 preclinical studies support the efficacy of indomethacin for COVID-19:
1.
Metwaly et al., Discovery of potential FDA-approved SARS-CoV-2 Papain-like protease inhibitors: A multi-phase in silico approach, Journal of Chemical Research, doi:10.1177/17475198241298547.
2.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
3.
Chakraborty et al., In-silico screening and in-vitro assay show the antiviral effect of Indomethacin against SARS-CoV-2, Computers in Biology and Medicine, doi:10.1016/j.compbiomed.2022.105788.
4.
Tramontozzi et al., Indomethacin inhibits human seasonal coronaviruses at late stages of viral replication in lung cells: Impact on virus-induced COX-2 expression, Journal of Virus Eradication, doi:10.1016/j.jve.2024.100387.
Wang et al., 15 Aug 2023, peer-reviewed, 10 authors.
Contact: q.pan@erasmusmc.nl.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Combating pan-coronavirus infection by indomethacin through simultaneously inhibiting viral replication and inflammatory response
iScience, doi:10.1016/j.isci.2023.107631
This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author contributions Conceptualization, Y.W., and Q.P.; Methodology, Y.W., P.L., L.X., and W.W.; Resources, R.J.R., P.L., and D.E.K; Formal analysis, P.L., and Y.W.; Project discussion, M.B.C., R.J.R., DE.K., M.P.P., and A.C.V.; Writing-Original Draft, Y.W., and Q.P.; Funding acquisition, Q.P., and R.J.R.; Writing-Review & Editing, R.J.R., M.B.C., D.E.K., M.P.P., A.C.V., and Q.P.
Declaration of interest The authors disclose no conflicts.
Highlights • Indomethacin exerts pan-coronavirus antiviral activity • Indomethacin promotes interferon response through enhancing STAT1 phosphorylation • Indomethacin inhibits coronavirus-triggered inflammatory response
References
Abdellatif, Abdelall, Elshemy, El-Nahass, Abdel-Fattah et al., New indomethacin analogs as selective COX-2 inhibitors: Synthesis, COX-1/2 inhibitory activity, anti-inflammatory, ulcerogenicity, histopathological, and docking studies, Arch Pharm (Weinheim), doi:10.1002/ardp.202000328
Ader, Study, An open-label randomized, controlled trial of the effect of lopinavir and ritonavir, lopinavir and ritonavir plus interferon-beta-1a, and J o u r n a l P r e -p r o o f hydroxychloroquine in hospitalized patients with COVID-19: final results, Clin Microbiol Infect, doi:10.1016/j.cmi.2022.04.016
Al-Tawfiq, Sah, Altawfiq, Pan, Mpox-associated myopericarditis, New Microbes New Infect, doi:10.1016/j.nmni.2023.101085
Amici, Di Caro, Ciucci, Chiappa, Castilletti et al., Indomethacin has a potent antiviral activity against SARS coronavirus, Antivir Ther
Andersen, Ianevski, Lysvand, Vitkauskiene, Oksenych et al., Discovery and development of safe-in-man broadspectrum antiviral agents, Int J Infect Dis, doi:10.1016/j.ijid.2020.02.018
Bahrami, Daryani, Haghpanah, Moayyeri, Moghadam et al., Effects of indomethacin on viral replication markers in asymptomatic carriers of hepatitis B: a randomized, placebo-controlled trial, Am J Gastroenterol, doi:10.1111/j.1572-0241.2005.41144.x
Buchynskyi, Kamyshna, Lyubomirskaya, Moshynets, Kobyliak et al., Efficacy of interferon alpha for the treatment of hospitalized patients with COVID-19: A meta-analysis, Front Immunol, doi:10.3389/fimmu.2023.1069894
Cannon, Cannon, COX-2 inhibitors and cardiovascular risk, Physiology, doi:10.1126/science.1224398
Chakraborty, Bhattacharje, Baral, Manna, Mullick et al., In-silico screening and in-vitro assay show the antiviral effect of Indomethacin against SARS-CoV-2, Comput Biol Med, doi:10.1016/j.compbiomed.2022.105788
Chen, Alfajaro, Chow, Wei, Filler et al., Non-steroidal anti-inflammatory drugs dampen the cytokine and antibody response to SARS-CoV-2 infection, J Virol, doi:10.1128/JVI.00014-21
Daelemans, Pauwels, De Clercq, Pannecouque, A time-of-drug addition approach to target identification of antiviral compounds, Nat Protoc, doi:10.1038/nprot.2011.330
De Almeida, Da Silva, Rodrigues, Oliveira, Ishimoto et al., Identification of immunomodulatory drugs that inhibit multiple inflammasomes and impair SARS-CoV-2 infection, Sci Adv, doi:10.1126/sciadv.abo5400
Desantis, Mercorelli, Celegato, Croci, Bazzacco et al., Indomethacin-based PROTACs as pancoronavirus antiviral agents, Eur J Med Chem, doi:10.1016/j.ejmech.2021.113814
Faist, Schloer, Mecate-Zambrano, Janowski, Schreiber et al., Inhibition of p38 signaling curtails the SARS-CoV-2 induced inflammatory response but retains the IFN-dependent antiviral defense of the lung epithelial barrier, Antiviral Res, doi:10.1016/j.antiviral.2022.105475
Fajgenbaum, Cytokine Storm, N Engl J Med, doi:10.1056/NEJMra2026131
Gomeni, Xu, Gao, Bressolle-Gomeni, Model based approach for estimating the dosage regimen of indomethacin a potential antiviral treatment of patients infected with SARS CoV-2, J Pharmacokinet Pharmacodyn, doi:10.1007/s10928-020-09690-4
Gordon, Hiatt, Bouhaddou, Rezelj, Ulferts et al., Comparative host-coronavirus protein interaction networks reveal pan-viral disease mechanisms, Science, doi:10.1126/science.abe9403
Hart, Boardman, Indomethacin: A New Non-Steroid Anti-Inflammatory Agent, Br Med J, doi:10.1136/bmj.2.5363.965
Higgins, Sohaei, Diamandis, Prassas, COVID-19: from an acute to chronic disease? Potential long-term health consequences, Crit Rev Clin Lab Sci, doi:10.1080/10408363.2020.1860895
Hofmann, Pyrc, Van Der Hoek, Geier, Berkhout et al., Human coronavirus NL63 employs the severe acute respiratory syndrome coronavirus receptor for cellular entry, Proc Natl Acad Sci U S A, doi:10.1073/pnas.0409465102
Hu, Huang, Yin, The cytokine storm and COVID-19, J Med Virol, doi:10.1002/jmv.26232
Huskisson, Taylor, Burston, Chuter, Hart, Evening indomethacin in the treatment of rheumatoid arthritis, Ann Rheum Dis, doi:10.1136/ard.29.4.393
Ianevski, Giri, Aittokallio, SynergyFinder 3.0: an interactive analysis and consensus interpretation of multi-drug synergies across multiple samples
Ianevski, Yao, Lysvand, Grodeland, Legrand et al., Nafamostat-Interferon-alpha Combination Suppresses SARS-CoV-2 Infection In Vitro and In Vivo by Cooperatively Targeting Host TMPRSS2, Viruses, doi:10.3390/v13091768
Ianevski, Yao, Simonsen, Myhre, Ravlo et al., Mono-and combinational drug therapies for global viral pandemic preparedness, doi:10.1016/j.isci.2022.104112
Ianevski, Yao, Zusinaite, Lello, Wang et al., Synergistic Interferon-Alpha-Based Combinations for Treatment of SARS-CoV-2 and Other Viral Infections, Viruses, doi:10.3390/v13122489
Ianevski, Zusinaite, Kuivanen, Strand, Lysvand et al., Novel activities of safe-in-human broad-spectrum antiviral agents, Antiviral Res, doi:10.1016/j.antiviral.2018.04.016
Kalil, Mehta, Patterson, Erdmann, Gomez et al., Efficacy of interferon beta-1a plus remdesivir compared with remdesivir alone in hospitalised adults with COVID-19: a double-bind, randomised, placebo-controlled, phase 3 trial, Lancet Respir Med, doi:10.1016/S2213-2600(21)00384-2
Kamyshnyi, Koval, Kobevko, Buchynskyi, Oksenych et al., Therapeutic Effectiveness of Interferon-alpha2b against COVID-19 with Community-Acquired Pneumonia: The Ukrainian Experience, Int J Mol Sci, doi:10.3390/ijms24086887
Kiani, Scholey, Dahl, Mcmann, Iversen et al., Vitro Assessment of the Antiviral Activity of Ketotifen, Indomethacin and Naproxen, Alone and in Combination, against SARS-CoV-2. Viruses 13, doi:10.3390/v13040558
Li, De Vries, Kamar, Peppelenbosch, Pan, Monitoring and managing SARS-CoV-2 evolution in immunocompromised populations, Lancet Microbe, doi:10.1016/S2666-5247(22)00061-1
Li, Liu, Ma, Bramer, Peppelenbosch et al., Estimating Global Epidemiology of Low-Pathogenic Human Coronaviruses in Relation to the COVID-19 Context, J Infect Dis, doi:10.1093/infdis/jiaa321
Li, Wang, Lamers, Lavrijsen, Iriondo et al., Recapitulating infection, thermal sensitivity and antiviral treatment of seasonal coronaviruses in human airway organoids, EBioMedicine, doi:10.1016/j.ebiom.2022.104132
Li, Wang, Lavrijsen, Lamers, De Vries et al., SARS-CoV-2 Omicron variant is highly sensitive to molnupiravir, nirmatrelvir, and the combination, Cell Res, doi:10.1038/s41422-022-00618-w
Li, Wang, Solanki, Atre, Lavrijsen et al., Nirmatrelvir exerts distinct antiviral potency against different human coronaviruses, Antiviral Res, doi:10.1016/j.antiviral.2023.105555
Liu, Li, Xu, Wu, Luo et al., Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19, J Clin Virol, doi:10.1016/j.jcv.2020.104370
Pan, Tilanus, Janssen, Van Der Laan, Ribavirin enhances interferon-stimulated gene transcription by activation of the interferon-stimulated response element, Hepatology, doi:10.1002/hep.24202
Petersen, Koopmans, Go, Hamer, Petrosillo et al., Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics, Lancet Infect Dis, doi:10.1016/S1473-3099(20)30484-9
Ravichandran, Mohan, Sukumaran, Kamaraj, Daivasuga et al., An open label randomized clinical trial of Indomethacin for mild and moderate hospitalised Covid-19 patients, Sci Rep, doi:10.1038/s41598-022-10370-1
Ray, Bisher, Enquist, Cyclooxygenase-1 and -2 are required for production of infectious pseudorabies virus, J Virol, doi:10.1128/JVI.78.23.12964-12974.2004
Rubin, From Positive to Negative to Positive Again-The Mystery of Why COVID-19 Rebounds in Some Patients Who Take Paxlovid, JAMA, doi:10.1001/jama.2022.9925
Telenti, Hodcroft, Robertson, The Evolution and Biology of SARS-CoV-2 Variants. Cold Spring Harb Perspect Med 12, doi:10.1101/cshperspect.a041390
Terracciano, Preiano, Fregola, Pelaia, Montalcini et al., Mapping the SARS-CoV-2-Host Protein-Protein Interactome by Affinity Purification Mass Spectrometry and Proximity-Dependent Biotin Labeling: A Rational and Straightforward Route to Discover Host-Directed Anti-SARS-CoV-2 Therapeutics, Int J Mol Sci, doi:10.3390/ijms22020532
Travaglini, Nabhan, Penland, Sinha, Gillich et al., A molecular cell atlas of the human lung from single-cell RNA sequencing, Nature, doi:10.1038/s41586-020-2922-4
Van Kleef, De Knegt, Ayada, Pan, Brouwer, The Steatosisassociated fibrosis estimator (SAFE) score: validation in the general US population, Hepatol Commun, doi:10.1097/HC9.0000000000000075
Veiga, Martins, Riediger, Mazetto, Debur et al., More than just a common cold: Endemic coronaviruses OC43, HKU1, NL63, and 229E associated with severe acute respiratory infection and fatality cases among healthy adults, J Med Virol, doi:10.1002/jmv.26362
Wang, Berger, Davis, Kaelber, Volkow et al., COVID-19 rebound after Paxlovid and Molnupiravir during January, doi:10.1101/2022.06.21.22276724
Wang, Xu, Su, Peppelenbosch, Pan, Transcriptional Regulation of Antiviral Interferon-Stimulated Genes, Trends Microbiol, doi:10.1016/j.tim.2017.01.001
Wong, Au, Lau, Lau, Cowling et al., r e -p r o o f hospitalisation, and in-hospital outcomes among community-dwelling, ambulatory patients with confirmed SARS-CoV-2 infection during the omicron wave in Hong Kong: an observational study, J o u r n a l P, doi:10.1016/S0140-6736(22)01586-0
Xu, Wang, Peppelenbosch, Pan, Noncanonical Antiviral Mechanisms of ISGs: Dispensability of Inducible Interferons, doi:10.1016/j.it.2016.11.002
Yip, Lui, Lai, Wong, Tse et al., Impact of the Use of Oral Antiviral Agents on the Risk of Hospitalization in Community Coronavirus Disease 2019 Patients (COVID-19), Clin Infect Dis, doi:10.1093/cid/ciac687
Zhao, Guo, Liu, Cuconati, Chang et al., Interferon induction of IFITM proteins promotes infection by human coronavirus OC43, Proc Natl Acad Sci U S A, doi:10.1073/pnas.1320856111
Zhou, Yang, Wang, Hu, Zhang et al., A pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature, doi:10.1038/s41586-020-2012-7
Zielecki, Weber, Eickmann, Spiegelberg, Zaki et al., Human cell tropism and innate immune system interactions of human respiratory coronavirus EMC compared to those of severe acute respiratory syndrome coronavirus, J Virol, doi:10.1128/JVI.03496-12
DOI record:
{
"DOI": "10.1016/j.isci.2023.107631",
"ISSN": [
"2589-0042"
],
"URL": "http://dx.doi.org/10.1016/j.isci.2023.107631",
"alternative-id": [
"S258900422301708X"
],
"article-number": "107631",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Combating pan-coronavirus infection by indomethacin through simultaneously inhibiting viral replication and inflammatory response"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "iScience"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.isci.2023.107631"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2023 The Author(s)."
}
],
"author": [
{
"affiliation": [],
"family": "Wang",
"given": "Yining",
"sequence": "first"
},
{
"affiliation": [],
"family": "Li",
"given": "Pengfei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xu",
"given": "Lei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "de Vries",
"given": "Annemarie C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rottier",
"given": "Robbert J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wang",
"given": "Wenshi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Crombag",
"given": "Marie-Rose B.S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Peppelenbosch",
"given": "Maikel P.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kainov",
"given": "Denis E.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9982-6184",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pan",
"given": "Qiuwei",
"sequence": "additional"
}
],
"container-title": "iScience",
"container-title-short": "iScience",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"cell.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
8,
16
]
],
"date-time": "2023-08-16T06:02:29Z",
"timestamp": 1692165749000
},
"deposited": {
"date-parts": [
[
2023,
8,
16
]
],
"date-time": "2023-08-16T06:02:30Z",
"timestamp": 1692165750000
},
"indexed": {
"date-parts": [
[
2023,
8,
17
]
],
"date-time": "2023-08-17T05:07:15Z",
"timestamp": 1692248835782
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
8
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
8,
1
]
],
"date-time": "2023-08-01T00:00:00Z",
"timestamp": 1690848000000
}
},
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 10,
"start": {
"date-parts": [
[
2023,
8,
11
]
],
"date-time": "2023-08-11T00:00:00Z",
"timestamp": 1691712000000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S258900422301708X?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S258900422301708X?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "107631",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
8
]
]
},
"published-print": {
"date-parts": [
[
2023,
8
]
]
},
"publisher": "Elsevier BV",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S258900422301708X"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Combating pan-coronavirus infection by indomethacin through simultaneously inhibiting viral replication and inflammatory response",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy"
}