Effect of Aspirin Use on the Adverse Outcomes in Patients Hospitalized for COVID-19
et al., Cardiology Research, doi:10.14740/cr1645, Jun 2024
Retrospective 376 hospitalized COVID-19 patients in the United States showing no significant differences with aspirin. Mortality, mechanical ventilation, and hypoxia were lower with treatment, without statistical significance.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
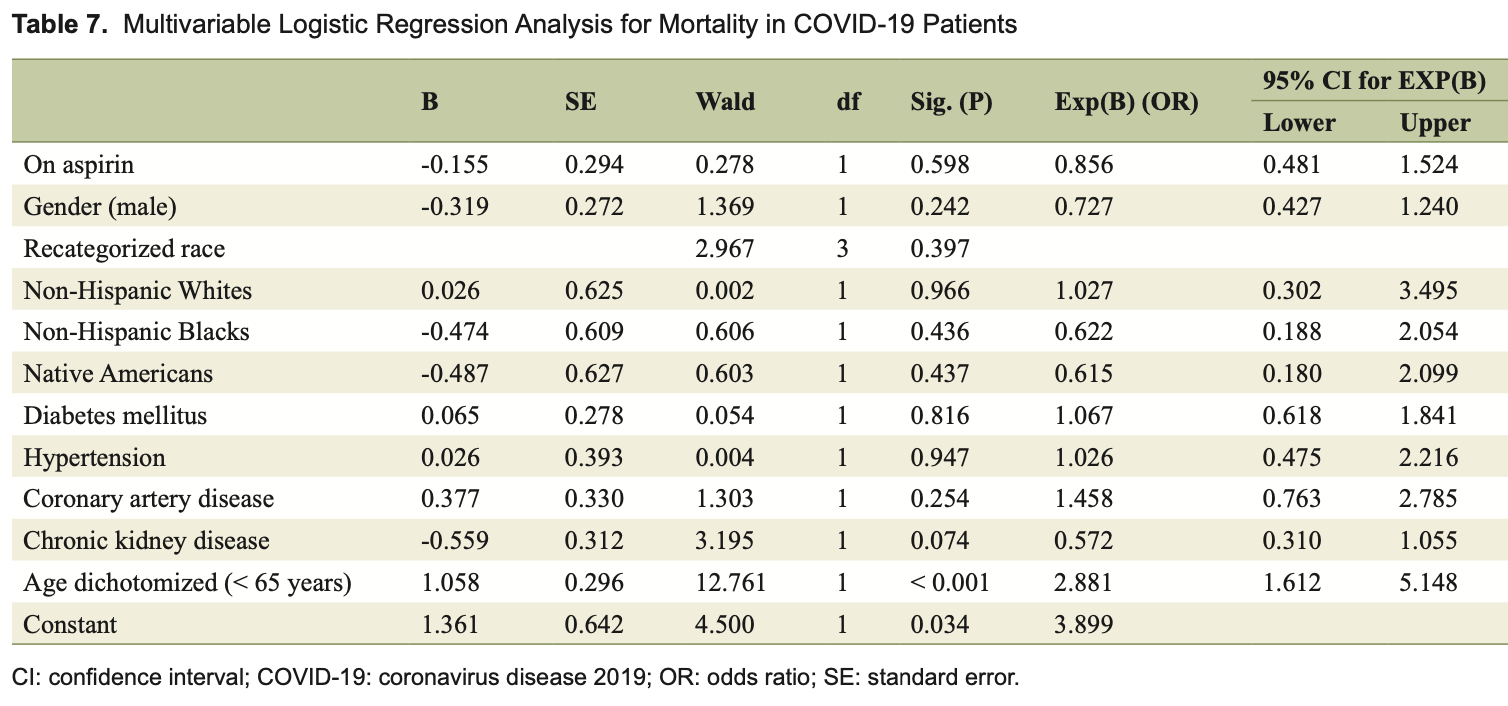
risk of death, 14.4% lower, OR 0.86, p = 0.61, treatment 128, control 248, adjusted per study, multivariable, RR approximated with OR.
|
|
risk of mechanical ventilation, 30.3% lower, OR 0.70, p = 0.24, treatment 128, control 248, adjusted per study, multivariable, RR approximated with OR.
|
|
hypoxia, 39.6% lower, OR 0.60, p = 0.0497, treatment 128, control 248, adjusted per study, multivariable, RR approximated with OR.
|
|
readmisson, 5.8% higher, OR 1.06, p = 0.88, treatment 128, control 248, adjusted per study, multivariable, RR approximated with OR.
|
|
DVT/PE, 17.7% lower, OR 0.82, p = 0.77, treatment 128, control 248, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Vinod et al., 24 Jun 2024, retrospective, USA, peer-reviewed, mean age 66.8, 8 authors, study period March 2020 - October 2020.
Contact: poornima.vinod@unchealth.unc.edu, drpoornimavinod@yahoo.com.
Effect of Aspirin Use on the Adverse Outcomes in Patients Hospitalized for COVID-19
Cardiology Research, doi:10.14740/cr1645
Background: Coronavirus disease 2019 (COVID-19) triggers multiple components of the immune system and causes inflammation of endothelial walls across vascular beds, resulting in respiratory failure, arterial and venous thrombosis, myocardial injury, and multi-organ failure leading to death. Early in the COVID-19 pandemic, aspirin was suggested for the treatment of symptomatic individuals, given its analgesic, antipyretic, anti-inflammatory, anti-thrombotic, and antiviral effects. This study aimed to evaluate the association of aspirin use with various clinical outcomes in patients hospitalized for COVID-19.
Methods: This was a retrospective study involving patients aged ≥ 18 years and hospitalized for COVID-19 from March 2020 to October 2020. Primary outcomes were acute cardiovascular events (ST elevation myocardial infarction (STEMI), type 1 non-ST elevation myocardial infarction (NSTEMI), acute congestive heart failure (CHF), and acute stroke) and death. Secondary outcomes were respiratory failure, need for mechanical ventilation, and acute deep vein thrombosis (DVT)/pulmonary embolism (PE). Results: Of 376 patients hospitalized for COVID-19, 128 were taking aspirin. Significant proportions of native Americans were hospitalized for COVID-19 in both aspirin (22.7%) and non-aspirin (24.6%) groups. Between aspirin and non-aspirin groups, no significant differences were found with regard to mechanical ventilator support (21.1% vs. 15.3%, P = 0.16), acute cardiovascular events (7.8% vs. 5.2%, P = 0.32), acute DVT/PE (3.9% vs. 5.2%, P = 0.9), readmission rate (13.3% vs. 12.9%, P = 0.91) and mortality (23.4% vs. 20.2%, P = 0.5); however, the median duration of mechanical ventilation was significantly shorter (7 vs. 9 days, P = 0.04) and median length of hospitalization was significantly longer (5.5 vs. 4 days, P = 0.01) in aspirin group compared to non-aspirin group.
Conclusion: No significant differences were found in acute cardiovascular events, acute DVT/PE, mechanical ventilator support, and mortality rate between hospitalized COVID-19 patients who were taking aspirin compared to those not taking aspirin. However, larger studies are required to confirm our findings.
Conflict of Interest Authors have no conflict of interest to declare.
Informed Consent Informed consent was not required.
Author Contributions Poornima Vinod: writing-original draft, writing and editing, visualization, supervision, resources, project administration, methodology, investigation, data curation, and conceptualization. Vinod Krishnappa: writing-original draft, writing-review and editing, resources, investigation, data curation, and conceptualization. William Rathell: writing-original draft, writing-review and editing, resources, investigation, data curation, and conceptualization. Saira Amir: writing-review and editing, resources, investigation, data curation, and conceptualization. Subrina Sundil: writing-review and editing, resources, investigation, data curation, and conceptualization. Godwin Dogbey: statistical analysis, methodology, investigation, data curation, and conceptualization. Hiten Patel: writing-review and editing, conceptualization, and supervision. William Herzog: writingreview and editing, conceptualization, and supervision.
References
Aly, Ibrahim, Should aspirin be used for prophylaxis of COVID-19-induced coagulopathy?, Med Hypotheses, doi:10.1016/j.mehy.2020.109975
Babapoor-Farrokhran, Gill, Walker, Rasekhi, Bozorgnia et al., Myocardial injury and COV-ID-19: possible mechanisms, Life Sci, doi:10.1016/j.lfs.2020.117723
Bianconi, Violi, Fallarino, Pignatelli, Sahebkar et al., Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID-19?, Drugs, doi:10.1007/s40265-020-01365-1
Chiang, Gupta, Aspirin resistance in obese and elderly patients with COVID-19?, Am J Med, doi:10.1016/j.amjmed.2020.09.006
Chow, Khanna, Kethireddy, Yamane, Levine et al., Aspirin use is associated with decreased mechanical ventilation, intensive care unit admission, and in-hospital mortality in hospitalized patients with coronavirus disease 2019, Anesth Analg, doi:10.1213/ANE.0000000000005292
Connors, Brooks, Sciurba, Krishnan, Bledsoe et al., Effect of antithrombotic therapy on clinical outcomes in outpatients with clinically stable symptomatic COVID-19: the ACTIV-4B randomized clinical trial, JAMA, doi:10.1001/jama.2021.17272
Coulombe, Jaworska, Verway, Tzelepis, Massoud et al., Targeted prostaglandin E2 inhibition enhances antiviral immunity through induction of type I interferon and apoptosis in macrophages, Immunity, doi:10.1016/j.immuni.2014.02.013
Cui, Chen, Li, Liu, Wang, Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia, J Thromb Haemost, doi:10.1111/jth.14830
Declercq, Leeuw, Lambrecht, Inflammasomes and IL-1 family cytokines in SARS-CoV-2 infection: from prognostic marker to therapeutic agent, Cytokine, doi:10.1016/j.cyto.2022.155934
Eikelboom, Jolly, Belley-Cote, Whitlock, Rangarajan et al., Colchicine and the combination of rivaroxaban and aspirin in patients hospitalised with COVID-19 (ACT): an open-label, factorial, randomised, controlled trial, Lancet Respir Med, doi:10.1016/S2213-2600(22)00298-3
Garcia, Immune response, inflammation, and the clinical spectrum of COVID-19, Front Immunol, doi:10.3389/fimmu.2020.01441
Geiger, Konig, Oberwinkler, Roll, Diesendorf et al., Acetylsalicylic acid and salicylic acid inhibit SARS-CoV-2 replication in precisioncut lung slices, Vaccines, doi:10.3390/vaccines10101619
Group, Aspirin in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial, Lancet, doi:10.1016/S0140-6736(21)01825-0
Kazama, Senzaki, Does immunosuppressive property of non-steroidal anti-inflammatory drugs (NSAIDs) reduce COVID-19 vaccine-induced systemic side effects?, Drug Discov Ther, doi:10.5582/ddt.2021.01094
Klok, Kruip, Van Der Meer, Arbous, Gommers et al., Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an Vinod et al, Cardiol Res, doi:10.1016/j.thromres.2020.04.041
Lal, Garces, Bansal, Tekin, Zec et al., Pre-hospital aspirin use and patient outcomes in COVID-19: results from the International Viral Infection and Respiratory Illness Universal Study (VIRUS), Arch Bronconeumol, doi:10.1016/j.arbres.2022.07.017
Lima-Morales, Mendez-Hernandez, Flores, Osorno-Romero, Hernandez et al., Effectiveness of a multidrug therapy consisting of ivermectin, azithromycin, montelukast, and acetylsalicylic acid to prevent hospitalization and death among ambulatory COVID-19 cases in Tlaxcala, Mexico, Int J Infect Dis, doi:10.1016/j.ijid.2021.02.014
Lund, Kristensen, Reilev, Christensen, Thomsen et al., anti-inflammatory drugs who tested positive for SARS-CoV-2: a Danish nationwide cohort study, Cardiol Res, doi:10.1371/journal.pmed.1003308
Martha, Pranata, Lim, Wibowo, Akbar, Active prescription of low-dose aspirin during or prior to hospitalization and mortality in COVID-19: a systematic review and meta-analysis of adjusted effect estimates, Int J Infect Dis, doi:10.1016/j.ijid.2021.05.016
Meizlish, Goshua, Liu, Fine, Amin et al., Intermediate-dose anticoagulation, aspirin, and in-hospital mortality in COVID-19: a propensity score-matched analysis, Am J Hematol, doi:10.1002/ajh.26102
Middeldorp, Coppens, Van Haaps, Foppen, Vlaar et al., Incidence of venous thromboembolism in hospitalized patients with COVID-19, J Thromb Haemost, doi:10.1111/jth.14888
Morrison, Su, Turchin, COVID-19 outcomes in patients taking cardioprotective medications, PLoS One, doi:10.1371/journal.pone.0275787
Nunns, Moore, Chapman, Moore, Stettler et al., The hypercoagulability paradox of chronic kidney disease: the role of fibrinogen, Am J Surg, doi:10.1016/j.amjsurg.2017.08.039
Rapkiewicz, Mai, Carsons, Pittaluga, Kleiner et al., Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: a case series, EClinical-Medicine, doi:10.1016/j.eclinm.2020.100434
Sayed Ahmed, Merrell, Ismail, Joudeh, Riley et al., Rationales and uncertainties for aspirin use in COVID-19: a narrative review, Fam Med Community Health, doi:10.1136/fmch-2020-000741
Sisinni, Rossi, Battista, Poletti, Battista et al., Pre-admission acetylsalicylic acid therapy and impact on in-hospital outcome in COVID-19 patients: the ASA-CARE study, Int J Cardiol, doi:10.1016/j.ijcard.2021.09.058
Srinivasan, Brown, Krishnamani, Cornett, Kesavan et al., Aspirin use is associated with decreased inpatient mortality in patients with COVID-19: a meta-analysis, Am Heart J Plus, doi:10.1016/j.ahjo.2022.100191
Su, Miao, Guo, Chen, Huang et al., Associations between the use of aspirin or other antiplatelet drugs and all-cause mortality among patients with COVID-19: a meta-analysis, Front Pharmacol, doi:10.3389/fphar.2022.989903
Varga, Flammer, Steiger, Haberecker, Andermatt et al., Endothelial cell infection and endotheliitis in COVID-19, Lancet, doi:10.1016/S0140-6736(20)30937-5
Wijaya, Andhika, Huang, Purwiga, Budiman, The effects of aspirin on the outcome of COVID-19: a systematic review and meta-analysis, Clin Epidemiol Glob Health, doi:10.1016/j.cegh.2021.100883
Yuan, Chen, Li, Chen, Wang et al., Mortality and pre-hospitalization use of low-dose aspirin in COVID-19 patients with coronary artery disease, J Cell Mol Med, doi:10.1111/jcmm.16198
Zhao, Huang, Huang, Liu, Shao et al., Prevalence of NSAID use among people with COVID-19 and the association with COVID-19-related outcomes: systematic review and meta-analysis, Br J Clin Pharmacol, doi:10.1111/bcp.15512
Zong, Wang, Liu, Li, Wei et al., Antiplatelet therapy for patients with COVID-19: systematic review and meta-analysis of observational studies and randomized controlled trials, Front Med, doi:10.3389/fmed.2022.965790
DOI record:
{
"DOI": "10.14740/cr1645",
"ISSN": [
"1923-2829",
"1923-2837"
],
"URL": "http://dx.doi.org/10.14740/cr1645",
"alternative-id": [
"10.14740/cr1645"
],
"author": [
{
"affiliation": [],
"family": "Vinod",
"given": "Poornima",
"sequence": "first"
},
{
"affiliation": [],
"family": "Krishnappa",
"given": "Vinod",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rathell",
"given": "William",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Amir",
"given": "Saira",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sundil",
"given": "Subrina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dogbey",
"given": "Godwin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Patel",
"given": "Hiten",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Herzog",
"given": "William",
"sequence": "additional"
}
],
"container-title": "Cardiology Research",
"container-title-short": "Cardiol Res",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.cardiologyres.org"
]
},
"created": {
"date-parts": [
[
2024,
6,
25
]
],
"date-time": "2024-06-25T09:33:47Z",
"timestamp": 1719308027000
},
"deposited": {
"date-parts": [
[
2024,
6,
25
]
],
"date-time": "2024-06-25T09:34:01Z",
"timestamp": 1719308041000
},
"indexed": {
"date-parts": [
[
2024,
6,
26
]
],
"date-time": "2024-06-26T00:23:24Z",
"timestamp": 1719361404240
},
"is-referenced-by-count": 0,
"issue": "3",
"issued": {
"date-parts": [
[
2024,
6
]
]
},
"journal-issue": {
"issue": "3"
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
6,
1
]
],
"date-time": "2024-06-01T00:00:00Z",
"timestamp": 1717200000000
}
}
],
"link": [
{
"URL": "http://www.cardiologyres.org/index.php/Cardiologyres/article/download/1645/1588",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "5784",
"original-title": [],
"page": "179-188",
"prefix": "10.14740",
"published": {
"date-parts": [
[
2024,
6
]
]
},
"published-print": {
"date-parts": [
[
2024,
6
]
]
},
"publisher": "Elmer Press, Inc.",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://www.cardiologyres.org/index.php/Cardiologyres/article/view/1645"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Effect of Aspirin Use on the Adverse Outcomes in Patients Hospitalized for COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.14740/elmerpress-crossmark-policy",
"volume": "15"
}