Pre-admission acetylsalicylic acid therapy and impact on in-hospital outcome in COVID-19 patients: The ASA-CARE study
et al., International Journal of Cardiology, doi:10.1016/j.ijcard.2021.09.058, Oct 2021
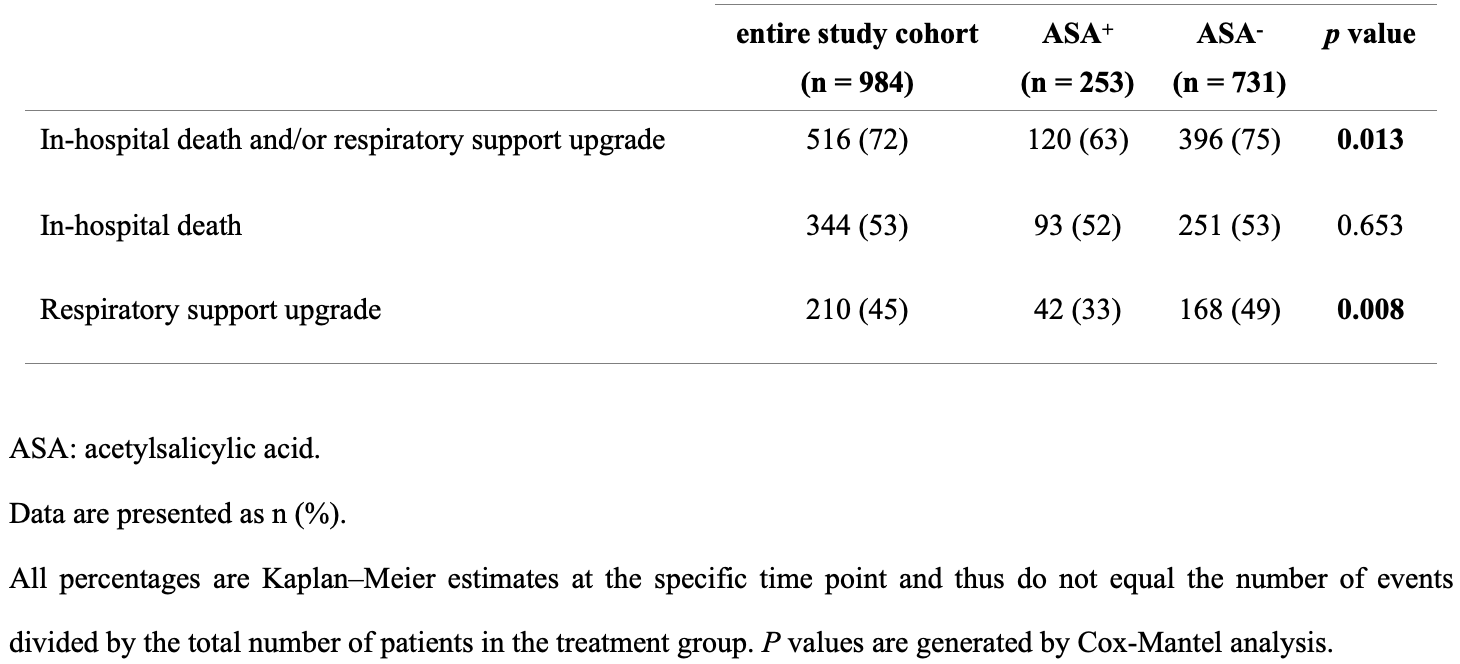
Retrospective 984 COVID-19 patients, 253 taking aspirin prior to admission, showing lower risk of respiratory support upgrade with treatment.
|
risk of death, 7.1% higher, RR 1.07, p = 0.65, treatment 93 of 253 (36.8%), control 251 of 731 (34.3%).
|
|
risk of death or respiratory support upgrade, 30.3% lower, RR 0.70, p = 0.01, treatment 253, control 731, multivariate.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Sisinni et al., 4 Oct 2021, retrospective, Italy, peer-reviewed, 18 authors.
Pre-admission acetylsalicylic acid therapy and impact on in-hospital outcome in COVID-19 patients: The ASA-CARE study
International Journal of Cardiology, doi:10.1016/j.ijcard.2021.09.058
This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
b Values are avaible for 97% of the entire study cohort. c Fever was classified as highest patient temperature 37.3 °C or higher. To minimize interference of treatment, the highest patient temperature was defined using the self-reported highest temperature before taking antipyretic drug. d ACE-I/ARB use was defined as use of these drugs at the time of admission that continued through hospitalization. e Values are avaible for 25% of the entire study cohort. f Including azithromycin 500 mg daily dose p.o. and/or ceftriaxone 2000 mg daily dose i.v.
J o u r n a l P r e -p r o o f Journal Pre-proof J o u r n a l P r e -p r o o f
References
Ackermann, Verleden, Kuehnel, Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19, N Engl J Med, doi:10.1056/NEJMoa2015432
Asia, Mediterranean, Pacific, COVID-19 Weekly Epidemiological Update
Bianconi, Violi, Fallarino, Pignatelli, Sahebkar et al., Is Acetylsalicylic Acid a Safe and P i Ch i A P i wi h CO D -19 ?, Drugs, doi:10.1007/s40265-020-01365-1
Bikdeli, Madhavan, Jimenez, COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Followup, J Am Coll Cardiol, doi:10.1016/j.jacc.2020.04.031
Bilaloglu, Aphinyanaphongs, Jones, Iturrate, Hochman et al., Thrombosis in Hospitalized Patients With COVID-19 in a New York City Health System, JAMA, doi:10.1001/jama.2020.13372
Chaudhary, Kreutz, Bliden, Gurbel, Personalizing Antithrombotic Therapy in COVID-19 : Th b g h nd Thromboelastometry
Chiarito, Sanz-Sánchez, Cannata, Monotherapy with a P2Y 12 inhibitor or aspirin for secondary prevention in patients with established atherosclerosis: a systematic review and meta-analysis, Lancet, doi:10.1016/S0140-6736(20)30315-9
Chow, Khanna, Kethireddy, Aspirin Use is Associated with Decreased Mechanical Ventilation, ICU Admission, and In-Hospital Mortality in Hospitalized Patients with COVID-19, Anesth Analg
Ciceri, Beretta, Scandroglio, Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis, Crit Care Resusc
Eikelboom, Hirsh, Spencer, Baglin, Weitz, Antiplatelet drugs: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines, Chest, doi:10.1378/chest.11-2293
Fox, Akmatbekov, Harbert, Li, Brown et al., Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans, Lancet Respir Med, doi:10.1016/S2213-2600(20)30243-5
Ganatra, Hammond, Nohria, The Novel Coronavirus Disease (COVID-19) Threat for Patients With Cardiovascular Disease and Cancer, JACC CardioOncology, doi:10.1016/j.jaccao.2020.03.001
Godino, Scotti, Maugeri, Antithrombotic therapy in patients with COVID-19? -Rationale and Evidence, Int J Cardiol, doi:10.1016/j.ijcard.2020.09.064
Gu, Tyagi, Jain, Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation, Nat Rev Cardiol, doi:10.1038/s41569-020-00469-1
Gurbel, Bliden, Butler, Randomized Double-Blind Assessment of the ONSET and OFFSET of the Antiplatelet Effects of Ticagrelor Versus Clopidogrel in Patients With Stable Coronary Artery Disease The ONSET / OFFSET Study, doi:10.1161/CIRCULATIONAHA.109.912550
Gurbel, Bliden, Rout, Bedside thromboelastography to rapidly assess the pharmacodynamic response of anticoagulants and aspirin in COVID-19: evidence of inadequate therapy in a predominantly minority population, J Thromb Thrombolysis, doi:10.1007/s11239-021-02435-1
Gurbel, Bliden, Schrör, Can an Old Ally Defeat a New Enemy?, Circulation, doi:10.1161/CIRCULATIONAHA.120.047830
J O U R N A L P R E, -p r o o f
J O U R N A L P R E, -p r o o f Journal Pre-proof
J O U R N A L P R E, -p r o o f Journal Pre-proof
Lemos, Do, Santo, Salvetti, Therapeutic versus prophylactic anticoagulation for severe COVID-19: A randomized phase II clinical trial (HESACOVID)
Levey, Stevens, Schmid, A new equation to estimate glomerular filtration rate, Ann Intern Med, doi:10.7326/0003-4819-150-9-200905050-00006
Mj, Hannah, Karlheinz, The Emerging Threat of (Micro)Thrombosis in COVID-19 and Its Therapeutic Implications, Circ Res, doi:10.1161/CIRCRESAHA.120.317447
Nishiga, Wang, Han, Lewis, Wu, COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives, Nat Rev Cardiol, doi:10.1038/s41569-020-0413-9
Organization, When COVID-19 Disease Is Suspected: Interim Guidance
Ouyang, Wang, Liu, Ma, Ding, Effects of antiplatelet therapy on the mortality rate of patients with sepsis: A meta-analysis, J Crit Care, doi:10.1016/j.jcrc.2018.12.004
Panka, De Grooth, Spoelstra-De Man, Looney, Tuinman, Prevention or Treatment of Ards With Aspirin: A Review of Preclinical Models and Meta-Analysis of Clinical Studies, Shock, doi:10.1097/SHK.0000000000000745
Paranjpe, Fuster, Lala, Association of Treatment Dose Anticoagulation With In-Hospital Survival Among Hospitalized Patients With COVID-19, J Am Coll Cardiol, doi:10.1016/j.jacc.2020
Sholzberg, Tang, Rahhal, Heparin for Moderately Ill Patients with Covid-19, medRxiv Prepr Serv Heal Sci, doi:10.1101/2021.07.08.21259351
The, Activ-4a, Investigators, Therapeutic Anticoagulation with Heparin in Noncritically Ill Patients with Covid-19, N Engl J Med, doi:10.1056/NEJMoa2105911
Varga, Flammer, Steiger, Endothelial cell infection and endotheliitis in COVID-19, Lancet, doi:10.1016/S0140-6736(20)30937-5
Younes, Platelets Can Associate With SARS-CoV-2 RNA and Are Hyperactivated in COVID-19, Circ Res, doi:10.1161/CIRCRESAHA.120.317703
Zhang, Liu, Wang, SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19, J Hematol Oncol, doi:10.1186/s13045-020-00954-7
Zhu, Zhang, Wang, A Novel Coronavirus from Patients with Pneumonia in China, 2019, N Engl J Med, doi:10.1056/NEJMoa2001017
DOI record:
{
"DOI": "10.1016/j.ijcard.2021.09.058",
"ISSN": [
"0167-5273"
],
"URL": "http://dx.doi.org/10.1016/j.ijcard.2021.09.058",
"alternative-id": [
"S0167527321014996"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Pre-admission acetylsalicylic acid therapy and impact on in-hospital outcome in COVID-19 patients: The ASA-CARE study"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "International Journal of Cardiology"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.ijcard.2021.09.058"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 Elsevier B.V. All rights reserved."
}
],
"author": [
{
"affiliation": [],
"family": "Sisinni",
"given": "Antonio",
"sequence": "first"
},
{
"affiliation": [],
"family": "Rossi",
"given": "Luca",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Battista",
"given": "Antonio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Poletti",
"given": "Enrico",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Battista",
"given": "Federica",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Battista",
"given": "Rosa Alessia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Malagoli",
"given": "Alessandro",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Biagi",
"given": "Andrea",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zanni",
"given": "Alessia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sticozzi",
"given": "Concetta",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Comastri",
"given": "Greta",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Marrocco-Trischitta",
"given": "Massimiliano M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Monello",
"given": "Alberto",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Margonato",
"given": "Alberto",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bandera",
"given": "Francesco",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vergara",
"given": "Pasquale",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guazzi",
"given": "Marco",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Godino",
"given": "Cosmo",
"sequence": "additional"
}
],
"container-title": "International Journal of Cardiology",
"container-title-short": "International Journal of Cardiology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"internationaljournalofcardiology.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
10,
5
]
],
"date-time": "2021-10-05T00:08:48Z",
"timestamp": 1633392528000
},
"deposited": {
"date-parts": [
[
2023,
1,
9
]
],
"date-time": "2023-01-09T00:53:28Z",
"timestamp": 1673225608000
},
"indexed": {
"date-parts": [
[
2024,
3,
4
]
],
"date-time": "2024-03-04T16:07:55Z",
"timestamp": 1709568475812
},
"is-referenced-by-count": 17,
"issued": {
"date-parts": [
[
2021,
12
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T00:00:00Z",
"timestamp": 1638316800000
}
},
{
"URL": "https://doi.org/10.15223/policy-017",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T00:00:00Z",
"timestamp": 1638316800000
}
},
{
"URL": "https://doi.org/10.15223/policy-037",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T00:00:00Z",
"timestamp": 1638316800000
}
},
{
"URL": "https://doi.org/10.15223/policy-012",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T00:00:00Z",
"timestamp": 1638316800000
}
},
{
"URL": "https://doi.org/10.15223/policy-029",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T00:00:00Z",
"timestamp": 1638316800000
}
},
{
"URL": "https://doi.org/10.15223/policy-004",
"content-version": "stm-asf",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T00:00:00Z",
"timestamp": 1638316800000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0167527321014996?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0167527321014996?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "240-245",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
12
]
]
},
"published-print": {
"date-parts": [
[
2021,
12
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1056/NEJMoa2001017",
"article-title": "A novel coronavirus from patients with pneumonia in China, 2019",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "727",
"issue": "8",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.ijcard.2021.09.058_bb0005",
"volume": "382",
"year": "2020"
},
{
"author": "Asia",
"key": "10.1016/j.ijcard.2021.09.058_bb0010",
"series-title": "COVID-19 Weekly Epidemiological Update",
"year": "2020"
},
{
"DOI": "10.1038/s41569-020-0413-9",
"article-title": "COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives",
"author": "Nishiga",
"doi-asserted-by": "crossref",
"first-page": "543",
"issue": "9",
"journal-title": "Nat. Rev. Cardiol.",
"key": "10.1016/j.ijcard.2021.09.058_bb0015",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.jaccao.2020.03.001",
"article-title": "The novel coronavirus disease (COVID-19) threat for patients with cardiovascular disease and cancer",
"author": "Ganatra",
"doi-asserted-by": "crossref",
"first-page": "350",
"issue": "2",
"journal-title": "JACC CardioOncol.",
"key": "10.1016/j.ijcard.2021.09.058_bb0020",
"volume": "2",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30243-5",
"article-title": "Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans",
"author": "Fox",
"doi-asserted-by": "crossref",
"first-page": "681",
"issue": "7",
"journal-title": "Lancet Respir. Med.",
"key": "10.1016/j.ijcard.2021.09.058_bb0025",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.13372",
"article-title": "Thrombosis in hospitalized patients with COVID-19 in a New York City health system",
"author": "Bilaloglu",
"doi-asserted-by": "crossref",
"first-page": "799",
"issue": "8",
"journal-title": "JAMA",
"key": "10.1016/j.ijcard.2021.09.058_bb0030",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2020.04.031",
"article-title": "COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up",
"author": "Bikdeli",
"doi-asserted-by": "crossref",
"journal-title": "J. Am. Coll. Cardiol.",
"key": "10.1016/j.ijcard.2021.09.058_bb0035",
"year": "2020"
},
{
"article-title": "Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation",
"author": "Gu",
"journal-title": "Nat. Rev. Cardiol.",
"key": "10.1016/j.ijcard.2021.09.058_bb0040",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1186/s13045-020-00954-7",
"article-title": "SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "120",
"issue": "1",
"journal-title": "J. Hematol. Oncol.",
"key": "10.1016/j.ijcard.2021.09.058_bb0045",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30937-5",
"article-title": "Endothelial cell infection and endotheliitis in COVID-19",
"author": "Varga",
"doi-asserted-by": "crossref",
"journal-title": "Lancet",
"key": "10.1016/j.ijcard.2021.09.058_bb0050",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2015432",
"article-title": "Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19",
"author": "Ackermann",
"doi-asserted-by": "crossref",
"first-page": "120",
"issue": "2",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.ijcard.2021.09.058_bb0055",
"volume": "383",
"year": "2020"
},
{
"article-title": "Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis",
"author": "Ciceri",
"first-page": "95",
"issue": "2",
"journal-title": "Crit Care Resusc",
"key": "10.1016/j.ijcard.2021.09.058_bb0060",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1016/j.jcrc.2018.12.004",
"article-title": "Effects of antiplatelet therapy on the mortality rate of patients with sepsis: a meta-analysis",
"author": "Ouyang",
"doi-asserted-by": "crossref",
"first-page": "162",
"journal-title": "J. Crit. Care",
"key": "10.1016/j.ijcard.2021.09.058_bb0065",
"volume": "50",
"year": "2019"
},
{
"DOI": "10.1097/SHK.0000000000000745",
"article-title": "Prevention or treatment of ards with aspirin: a review of preclinical models and meta-analysis of clinical studies",
"author": "Panka",
"doi-asserted-by": "crossref",
"first-page": "13",
"issue": "1",
"journal-title": "Shock",
"key": "10.1016/j.ijcard.2021.09.058_bb0070",
"volume": "47",
"year": "2017"
},
{
"DOI": "10.1007/s40265-020-01365-1",
"article-title": "Is acetylsalicylic acid a safe and potentially useful choice for adult patients with COVID - 19 ?",
"author": "Bianconi",
"doi-asserted-by": "crossref",
"first-page": "1383",
"issue": "14",
"journal-title": "Drugs",
"key": "10.1016/j.ijcard.2021.09.058_bb0075",
"volume": "80",
"year": "2020"
},
{
"key": "10.1016/j.ijcard.2021.09.058_bb0080",
"series-title": "Clinical Management of Severe Acute Respiratory Infection (SARI) When COVID-19 Disease Is Suspected: Interim Guidance",
"year": "2020"
},
{
"author": "Gurbel",
"key": "10.1016/j.ijcard.2021.09.058_bb0085",
"series-title": "Randomized Double-Blind Assessment of the ONSET and OFFSET of the Antiplatelet Effects of Ticagrelor Versus Clopidogrel in Patients With Stable Coronary Artery Disease The ONSET / OFFSET Study",
"year": "2009"
},
{
"DOI": "10.1378/chest.11-2293",
"article-title": "Antiplatelet drugs: antithrombotic therapy and prevention of thrombosis, 9th ed: american College of Chest Physicians Evidence-Based Clinical Practice Guidelines",
"author": "Eikelboom",
"doi-asserted-by": "crossref",
"first-page": "e89S",
"issue": "2 Suppl",
"journal-title": "Chest",
"key": "10.1016/j.ijcard.2021.09.058_bb0090",
"volume": "141",
"year": "2012"
},
{
"DOI": "10.7326/0003-4819-150-9-200905050-00006",
"article-title": "A new equation to estimate glomerular filtration rate",
"author": "Levey",
"doi-asserted-by": "crossref",
"first-page": "604",
"issue": "9",
"journal-title": "Ann. Intern. Med.",
"key": "10.1016/j.ijcard.2021.09.058_bb0095",
"volume": "150",
"year": "2009"
},
{
"article-title": "Antithrombotic therapy in patients with COVID-19? -Rationale and evidence",
"author": "Godino",
"first-page": "33894",
"issue": "20",
"journal-title": "Int. J. Cardiol.",
"key": "10.1016/j.ijcard.2021.09.058_bb0100",
"volume": "S0167–5273",
"year": "2020"
},
{
"DOI": "10.1016/j.thromres.2020.09.026",
"article-title": "Therapeutic versus prophylactic anticoagulation for severe COVID-19: arandomized phase II clinical trial (HESACOVID)",
"author": "ACB",
"doi-asserted-by": "crossref",
"first-page": "359",
"journal-title": "Thromb. Res",
"key": "10.1016/j.ijcard.2021.09.058_bb0105",
"volume": "196",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2020.05.001",
"article-title": "Association of treatment dose anticoagulation withwith in-hospitalin-hospital survival amongamong hospitalized patients with COVID-19",
"author": "Paranjpe",
"doi-asserted-by": "crossref",
"first-page": "122",
"issue": "1",
"journal-title": "J. Am. Coll. Cardiol.",
"key": "10.1016/j.ijcard.2021.09.058_bb0110",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1213/ANE.0000000000005292",
"article-title": "Aspirin use is associated with decreased mechanical ventilation, Intensive Care Unit admission, and in-hospital mortality in hospitalized patients with Coronavirus Disease 2019",
"author": "Chow",
"doi-asserted-by": "crossref",
"first-page": "930",
"issue": "4",
"journal-title": "Anesth Analg",
"key": "10.1016/j.ijcard.2021.09.058_bb0115",
"volume": "132",
"year": "2020"
},
{
"DOI": "10.1007/s11239-021-02435-1",
"article-title": "Bedside thromboelastography to rapidly assess the pharmacodynamic response of anticoagulants and aspirin in COVID-19: evidence of inadequate therapy in a predominantly minority population",
"author": "Gurbel",
"doi-asserted-by": "crossref",
"first-page": "902",
"issue": "4",
"journal-title": "J. Thromb. Thrombolysis",
"key": "10.1016/j.ijcard.2021.09.058_bb0120",
"volume": "51",
"year": "2021"
},
{
"DOI": "10.1161/CIRCRESAHA.120.317447",
"article-title": "The emerging threat of (Micro)Thrombosis in COVID-19 and its therapeutic implications",
"author": "Mj",
"doi-asserted-by": "crossref",
"first-page": "571",
"issue": "4",
"journal-title": "Circ. Res.",
"key": "10.1016/j.ijcard.2021.09.058_bb0125",
"volume": "127",
"year": "2020"
},
{
"DOI": "10.1161/CIRCRESAHA.120.317703",
"article-title": "Platelets can associate with SARS-CoV-2 RNA and are hyperactivated in COVID-19",
"author": "Younes",
"doi-asserted-by": "crossref",
"first-page": "1404",
"issue": "11",
"journal-title": "Circ. Res.",
"key": "10.1016/j.ijcard.2021.09.058_bb0130",
"volume": "127",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30315-9",
"article-title": "Monotherapy with a P2Y12 inhibitor or aspirin for secondary prevention in patients with established atherosclerosis: a systematic review and meta-analysis",
"author": "Chiarito",
"doi-asserted-by": "crossref",
"first-page": "1487",
"issue": "10235",
"journal-title": "Lancet",
"key": "10.1016/j.ijcard.2021.09.058_bb0135",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2103417",
"article-title": "Therapeutic anticoagulation with heparin in noncritically ill patients with Covid-19",
"author": "The REMAP-CAP, ACTIV-4a, and ATTACC Investigators",
"doi-asserted-by": "crossref",
"journal-title": "N Engl J Med.",
"key": "10.1016/j.ijcard.2021.09.058_bb0140",
"year": "2021"
},
{
"article-title": "Heparin for moderately Ill patients with Covid-19",
"author": "Sholzberg",
"journal-title": "medRxiv Prepr Serv Heal Sci",
"key": "10.1016/j.ijcard.2021.09.058_bb0145",
"year": "2021"
},
{
"author": "Chaudhary",
"first-page": "1594",
"key": "10.1016/j.ijcard.2021.09.058_bb0150",
"series-title": "Personalizing Antithrombotic Therapy in COVID-19 : Role of Thromboelastography and Thromboelastometry",
"year": "2020"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047830",
"article-title": "Can an old ally defeat a new Enemy?",
"author": "Gurbel",
"doi-asserted-by": "crossref",
"first-page": "315",
"issue": "4",
"journal-title": "Circulation",
"key": "10.1016/j.ijcard.2021.09.058_bb0155",
"volume": "142",
"year": "2020"
}
],
"reference-count": 31,
"references-count": 31,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0167527321014996"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cardiology and Cardiovascular Medicine"
],
"subtitle": [],
"title": "Pre-admission acetylsalicylic acid therapy and impact on in-hospital outcome in COVID-19 patients: The ASA-CARE study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "344"
}