Exploiting Bacteria for Improving Hypoxemia of COVID-19 Patients
et al., Biomedicines, doi:10.3390/biomedicines10081851, Aug 2022
Probiotics for COVID-19
20th treatment shown to reduce risk in
March 2021, now with p = 0.00000044 from 29 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective COVID-19 patients requiring CPAP, 21 treated with SLAB51 probiotics and 15 control patients, showing improved outcomes with treatment, despite significantly lower blood oxygenation at baseline in the treatment group.
Probiotic efficacy depends on the specific strains used. Specific microbes may decrease or increase COVID-19 risk1.
|
risk of death, 77.8% lower, RR 0.22, p = 0.28, treatment 1 of 21 (4.8%), control 3 of 14 (21.4%), NNT 6.0.
|
|
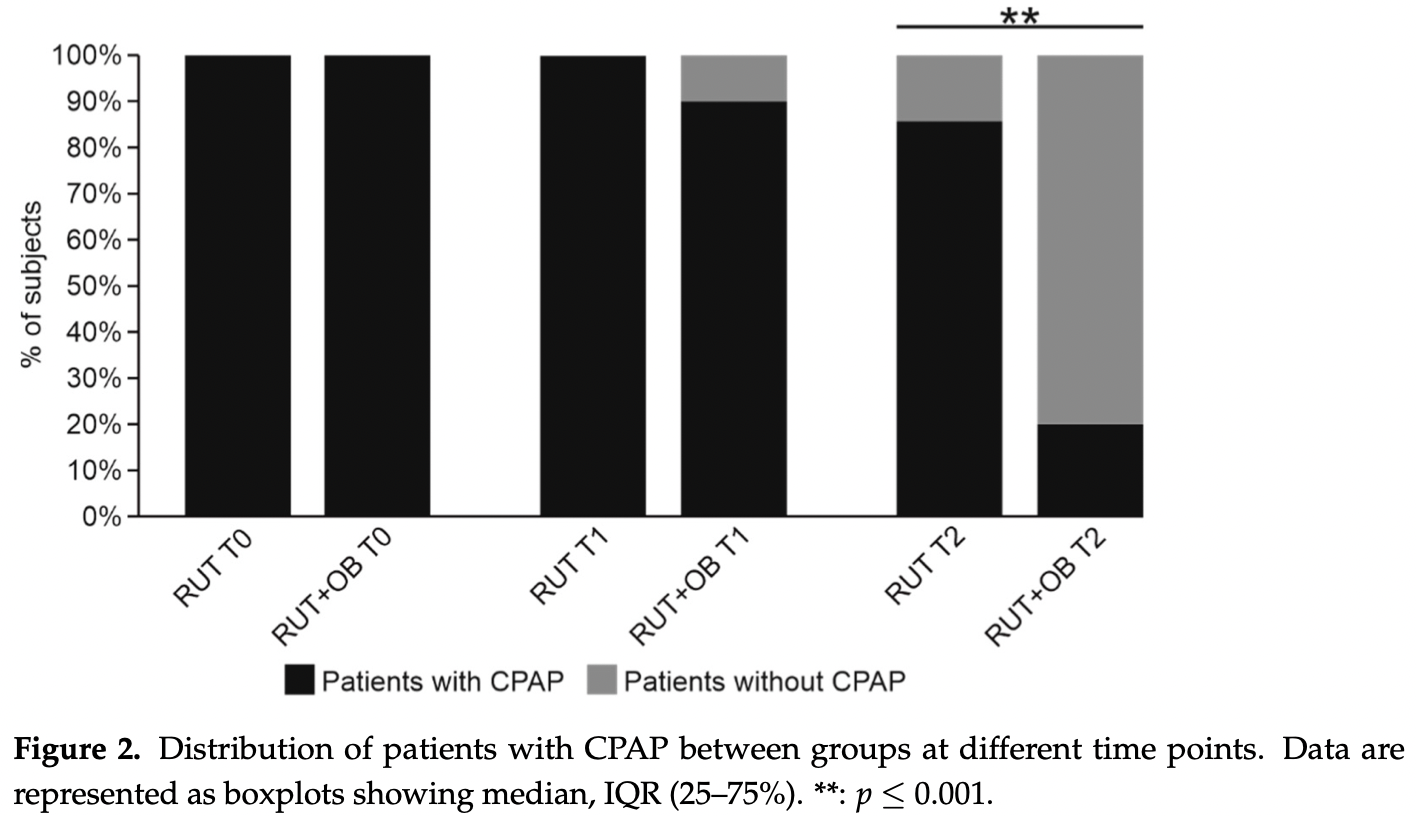
risk of miscellaneous, 77.8% lower, RR 0.22, p < 0.001, treatment 4 of 21 (19.0%), control 12 of 14 (85.7%), NNT 1.5, CPAP, day 7.
|
|
risk of miscellaneous, 9.5% lower, RR 0.90, p = 0.51, treatment 19 of 21 (90.5%), control 14 of 14 (100.0%), NNT 10, CPAP, day 3.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Trinchieri et al., 1 Aug 2022, retrospective, Italy, peer-reviewed, 10 authors, study period November 2020 - March 2021.
Contact: giancarlo.ceccarelli@uniroma1.it (corresponding author), vito.trinchieri@uniroma1.it, massimiliano.marazzato@uniroma1.it, letizia.santinelli@uniroma1.it, luca.maddaloni@uniroma1.it, paolo.vassilini@uniroma1.it, claudio.mastroianni@uniroma1.it, gabriella.dettorre@uniroma1.it, francesca.lombardi@univaq.it, alessandra.piccirilli@univaq.it.
Exploiting Bacteria for Improving Hypoxemia of COVID-19 Patients
Biomedicines, doi:10.3390/biomedicines10081851
Background: Although useful in the time-race against COVID-19, CPAP cannot provide oxygen over the physiological limits imposed by severe pulmonary impairments. In previous studies, we reported that the administration of the SLAB51 probiotics reduced risk of developing respiratory failure in severe COVID-19 patients through the activation of oxygen sparing mechanisms providing additional oxygen to organs critical for survival. Methods: This "real life" study is a retrospective analysis of SARS-CoV-2 infected patients with hypoxaemic acute respiratory failure secondary to COVID-19 pneumonia undergoing CPAP treatment. A group of patients managed with ad interim routinely used therapy (RUT) were compared to a second group treated with RUT associated with SLAB51 oral bacteriotherapy (OB). Results: At baseline, patients receiving SLAB51 showed significantly lower blood oxygenation than controls. An opposite condition was observed after 3 days of treatment, despite the significantly reduced amount of oxygen received by patients taking SLAB51. At 7 days, a lower prevalence of COVID-19 patients needing CPAP in the group taking probiotics was observed. The administration of SLAB51 is a complementary approach for ameliorating oxygenation conditions at the systemic level. Conclusion: This study proves that probiotic administration results in an additional boost in alleviating hypoxic conditions, permitting to limit on the use of CPAP and its contraindications.
Conflicts of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Acosta, Garrigos, Marcelin, Vijayvargiya, COVID-19 Pathogenesis and Clinical Manifestations, Infect. Dis. Clin. N. Am, doi:10.1016/j.idc.2022.01.003
Aliberti, Radovanovic, Billi, Sotgiu, Costanzo et al., Helmet CPAP treatment in patients with COVID-19 pneumonia: A multicentre cohort study, Eur. Respir. J, doi:10.1183/13993003.01935-2020
Andrew, Enzymatic function of nitric oxide synthases, Cardiovasc. Res, doi:10.1016/S0008-6363(99)00115-7
Bao, Tao, Cui, Yi, Pan et al., SARS-CoV-2 induced thrombocytopenia as an important biomarker significantly correlated with abnormal coagulation function, increased intravascular blood clot risk and mortality in COVID-19 patients, Exp. Hematol. Oncol, doi:10.1186/s40164-020-00172-4
Barrett, Bilaloglu, Cornwell, Burgess, Virginio et al., Platelets contribute to disease severity in COVID-19, J. Thromb. Haemost, doi:10.1111/jth.15534
Bonfili, Gong, Lombardi, Cifone, Eleuteri, Strategic Modification of Gut Microbiota through Oral Bacteriotherapy Influences Hypoxia Inducible Factor-1α: Therapeutic Implication in Alzheimer's Disease, Int. J. Mol. Sci
Brusasco, Corradi, Di Domenico, Raggi, Timossi et al., CPAP-COVID-19 Study Group; Collaborators of the Galliera CPAP-COVID-19 Study Group. Continuous positive airway pressure in COVID-19 patients with moderate-to-severe respiratory failure, Eur. Respir. J, doi:10.1183/13993003.02524-2020
Callapina, Zhou, Schnitzer, Metzen, Lohr et al., Nitric oxide reverses desferrioxamine-and hypoxia-evoked HIF-1α accumulation-Implications for prolyl hydroxylase activity and iron, Exp. Cell Res, doi:10.1016/j.yexcr.2005.02.018
Ceccarelli, Borrazzo, Pinacchio, Santinelli, Innocenti et al., Oral Bacteriotherapy in Patients With COVID-19: A Retrospective Cohort Study, Front. Nutr
Ceccarelli, Marazzato, Celani, Lombardi, Piccirilli et al., Oxygen Sparing Effect of Bacteriotherapy in COVID-19, Nutrients, doi:10.3390/nu13082898
Ceccarelli, Scagnolari, Pugliese, Mastroianni, ; D'ettorre, Probiotics and COVID-19, Lancet Gastroenterol. Hepatol, doi:10.1016/S2468-1253(20)30196-5
Chaurasia, Kushwaha, Kulkarni, Mallick, Latheef et al., Platelet HIF-2α promotes thrombogenicity through PAI-1 synthesis and extracellular vesicle release, Haematologica, doi:10.3324/haematol.2019.217463
Chavez, Brady, Gottlieb, Carius, Liang et al., Clinical update on COVID-19 for the emergency clinician: Airway and resuscitation, Am. J. Emerg. Med, doi:10.1016/j.ajem.2022.05.011
D'ettorre, Ceccarelli, Marazzato, Campagna, Pinacchio et al., Challenges in the Management of SARS-CoV-2 Infection: The Role of Oral Bacteriotherapy as Complementary Therapeutic Strategy to Avoid the Progression of COVID-19, Front. Med, doi:10.3389/fmed.2020.00389
De Angelis, Mariotti, Rossi, Servili, Fox et al., Arginine Catabolism by Sourdough Lactic Acid Bacteria: Purification and Characterization of the Arginine Deiminase Pathway Enzymes from Lactobacillus sanfranciscensis CB1, Appl. Environ. Microbiol, doi:10.1128/AEM.68.12.6193-6201.2002
Dillon, Holtsberg, Ensor, Bomalaski, Clark, Biochemical characterization of the arginine degrading enzymes arginase and arginine deiminase and their effect on nitric oxide production, Med. Sci. Monit
Duca, Memaj, Zanardi, Preti, Alesi et al., Severity of respiratory failure and outcome of patients needing a ventilatory support in the Emergency Department during Italian novel coronavirus SARS-CoV-2 outbreak: Preliminary data on the role of Helmet CPAP and Non-Invasive Positive Pressure Ventilation, eClinicalMedicine, doi:10.1016/j.eclinm.2020.100419
Fernández-Ferreiro, Formigo-Couceiro, Veiga-Gutierrez, Maldonado-Lobón, Hermida-Cao et al., Effects of Loigolactobacillus coryniformis K8 CECT 5711 on the Immune Response of Elderly Subjects to COVID-19 Vaccination: A Randomized Controlled Trial, Nutrients, doi:10.3390/nu14010228
Forcados, Muhammad, Oladipo, Makama, Meseko, Metabolic Implications of Oxidative Stress and Inflammatory Process in SARS-CoV-2 Pathogenesis: Therapeutic Potential of Natural Antioxidants, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2021.654813
Ito, Sono, Ito, Measurement and Clinical Significance of Lipid Peroxidation as a Biomarker of Oxidative Stress: Oxidative Stress in Diabetes, Atherosclerosis, and Chronic Inflammation, Antioxidants, doi:10.3390/antiox8030072
Jevtic, Nazy, The COVID Complex: A Review of Platelet Activation and Immune Complexes in COVID-19, Front. Immunol, doi:10.3389/fimmu.2022.807934
Kosanovic, Sagic, Djukic, Pljesa-Ercegovac, Savic-Radojevic et al., Time Course of Redox Biomarkers in COVID-19 Pneumonia: Relation with Inflammatory, Multiorgan Impairment Biomarkers and CT Findings, Antioxidants, doi:10.3390/antiox10071126
Król, Kepinska, Human Nitric Oxide Synthase-Its Functions, Polymorphisms, and Inhibitors in the Context of Inflammation, Diabetes and Cardiovascular Diseases, Int. J. Mol. Sci, doi:10.3390/ijms22010056
Lau, Ng, Yu, the Gut Microbiota in Coronavirus Disease 2019: Hype or Hope?, Gastroenterology, doi:10.1053/j.gastro.2021.09.009
Lundquist, Artursson, Oral absorption of peptides and nanoparticles across the human intestine: Opportunities, limitations and studies in human tissues, Adv. Drug Deliv. Rev, doi:10.1016/j.addr.2016.07.007
Mussini, Falcone, Nozza, Sagnelli, Parrella et al., Therapeutic strategies for severe COVID-19: A position paper from the Italian Society of Infectious and Tropical Diseases (SIMIT), Clin. Microbiol. Infect, doi:10.1016/j.cmi.2020.12.011
Okabe, Toyofumi, Yoshikawa, Yoneyama, Yokoyama et al., Mammalian enteral ventilation ameliorates respiratory failure, Med, doi:10.1016/j.medj.2021.04.004
Radovanovic, Rizzi, Pini, Saad, Chiumello et al., Helmet CPAP to Treat Acute Hypoxemic Respiratory Failure in Patients with COVID-19: A Management Strategy Proposal, J. Clin. Med, doi:10.3390/jcm9041191
Riccia, Bizzini, Perilli, Polimeni, Trinchieri et al., Anti-inflammatory effects of Lactobacillus brevis (CD2) on periodontal disease, Oral Dis, doi:10.1111/j.1601-0825.2006.01291.x
Rohlfing, Rath, Geisler, Gawaz, Platelets and COVID-19, Hamostaseologie, doi:10.1055/a-1581-4355
Shen, Wang, Effects of hypoxia on platelet activation in pilots, Aviat. Space Environ. Med
Singhal, Shah, Oxygen battle in the gut: Hypoxia and hypoxia-inducible factors in metabolic and inflammatory responses in the intestine, J. Biol. Chem, doi:10.1074/jbc.REV120.011188
Sundararaman, Ray, Ravindra, Halami, Role of probiotics to combat viral infections with emphasis on COVID-19, Appl. Microbiol. Biotechnol, doi:10.1007/s00253-020-10832-4
Wischmeyer, Tang, Ren, Bohannon, Ramirez et al., Daily Lactobacillus Probiotic versus Placebo in COVID-19-Exposed Household Contacts (PROTECT-EHC): A Randomized Clinical Trial, doi:10.1101/2022.01.04.21268275
Wozniak, Rubino, Tan, Jones, Webb et al., Positive role of continuous positive airway pressure for intensive care unit patients with severe hypoxaemic respiratory failure due to COVID-19 pneumonia: A single centre experience, J. Intensiv. Care Soc, doi:10.1177/1751143720971543
DOI record:
{
"DOI": "10.3390/biomedicines10081851",
"ISSN": [
"2227-9059"
],
"URL": "http://dx.doi.org/10.3390/biomedicines10081851",
"abstract": "<jats:p>Background: Although useful in the time-race against COVID-19, CPAP cannot provide oxygen over the physiological limits imposed by severe pulmonary impairments. In previous studies, we reported that the administration of the SLAB51 probiotics reduced risk of developing respiratory failure in severe COVID-19 patients through the activation of oxygen sparing mechanisms providing additional oxygen to organs critical for survival. Methods: This “real life” study is a retrospective analysis of SARS-CoV-2 infected patients with hypoxaemic acute respiratory failure secondary to COVID-19 pneumonia undergoing CPAP treatment. A group of patients managed with ad interim routinely used therapy (RUT) were compared to a second group treated with RUT associated with SLAB51 oral bacteriotherapy (OB). Results: At baseline, patients receiving SLAB51 showed significantly lower blood oxygenation than controls. An opposite condition was observed after 3 days of treatment, despite the significantly reduced amount of oxygen received by patients taking SLAB51. At 7 days, a lower prevalence of COVID-19 patients needing CPAP in the group taking probiotics was observed. The administration of SLAB51 is a complementary approach for ameliorating oxygenation conditions at the systemic level. Conclusion: This study proves that probiotic administration results in an additional boost in alleviating hypoxic conditions, permitting to limit on the use of CPAP and its contraindications.</jats:p>",
"alternative-id": [
"biomedicines10081851"
],
"author": [
{
"affiliation": [],
"family": "Trinchieri",
"given": "Vito",
"sequence": "first"
},
{
"affiliation": [],
"family": "Marazzato",
"given": "Massimiliano",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5921-3180",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ceccarelli",
"given": "Giancarlo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0551-5076",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lombardi",
"given": "Francesca",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Piccirilli",
"given": "Alessandra",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5621-058X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Santinelli",
"given": "Letizia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Maddaloni",
"given": "Luca",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vassalini",
"given": "Paolo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1286-467X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mastroianni",
"given": "Claudio Maria",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3571-5677",
"affiliation": [],
"authenticated-orcid": false,
"family": "d’Ettorre",
"given": "Gabriella",
"sequence": "additional"
}
],
"container-title": "Biomedicines",
"container-title-short": "Biomedicines",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
8,
2
]
],
"date-time": "2022-08-02T01:01:24Z",
"timestamp": 1659402084000
},
"deposited": {
"date-parts": [
[
2022,
8,
2
]
],
"date-time": "2022-08-02T01:21:26Z",
"timestamp": 1659403286000
},
"indexed": {
"date-parts": [
[
2022,
8,
2
]
],
"date-time": "2022-08-02T04:26:05Z",
"timestamp": 1659414365123
},
"is-referenced-by-count": 0,
"issue": "8",
"issued": {
"date-parts": [
[
2022,
8,
1
]
]
},
"journal-issue": {
"issue": "8",
"published-online": {
"date-parts": [
[
2022,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
1
]
],
"date-time": "2022-08-01T00:00:00Z",
"timestamp": 1659312000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2227-9059/10/8/1851/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1851",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
8,
1
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
1
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/j.idc.2022.01.003",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1016/j.ajem.2022.05.011",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1016/j.medj.2021.04.004",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1074/jbc.REV120.011188",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1016/j.yexcr.2005.02.018",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.3390/nu13082898",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.3390/ijms23010357",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"key": "ref8",
"unstructured": "Case Definition for Coronavirus Disease 2019 (COVID-19)\nhttps://www.ecdc.europa.eu/en/covid-19/surveillance/case-definition"
},
{
"first-page": "1",
"key": "ref9",
"series-title": "Clinical Management of COVID-19",
"year": "2020"
},
{
"DOI": "10.1016/j.cmi.2020.12.011",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1016/j.eclinm.2020.100419",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1183/13993003.02524-2020",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1007/s00253-020-10832-4",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1053/j.gastro.2021.09.009",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.3390/nu14010228",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1101/2022.01.04.21268275",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.3389/fmed.2020.00389",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.3389/fnut.2020.613928",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1016/S2468-1253(20)30196-5",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1128/AEM.68.12.6193-6201.2002",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"article-title": "Biochemical characterization of the arginine degrading enzymes arginase and arginine deiminase and their effect on nitric oxide production",
"author": "Dillon",
"first-page": "BR248",
"journal-title": "Med. Sci. Monit.",
"key": "ref21",
"volume": "8",
"year": "2002"
},
{
"DOI": "10.1111/j.1601-0825.2006.01291.x",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1016/S0008-6363(99)00115-7",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.3390/ijms22010056",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1016/j.addr.2016.07.007",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1055/a-1581-4355",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1186/s40164-020-00172-4",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1111/jth.15534",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.3389/fimmu.2022.807934",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"article-title": "Effects of hypoxia on platelet activation in pilots",
"author": "Shen",
"first-page": "646",
"journal-title": "Aviat. Space Environ. Med.",
"key": "ref30",
"volume": "65",
"year": "1994"
},
{
"DOI": "10.3324/haematol.2019.217463",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.3389/fcimb.2021.654813",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.3390/antiox8030072",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.3390/antiox10071126",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1177/1751143720971543",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.3390/jcm9041191",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1183/13993003.01935-2020",
"doi-asserted-by": "publisher",
"key": "ref37"
}
],
"reference-count": 37,
"references-count": 37,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2227-9059/10/8/1851"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Biochemistry, Genetics and Molecular Biology",
"Medicine (miscellaneous)"
],
"subtitle": [],
"title": "Exploiting Bacteria for Improving Hypoxemia of COVID-19 Patients",
"type": "journal-article",
"volume": "10"
}
