Effects of Antidepressants on COVID-19 Outcomes: Retrospective Study on Large-Scale Electronic Health Record Data
et al., Interactive Journal of Medical Research, doi:10.2196/39455, Apr 2023
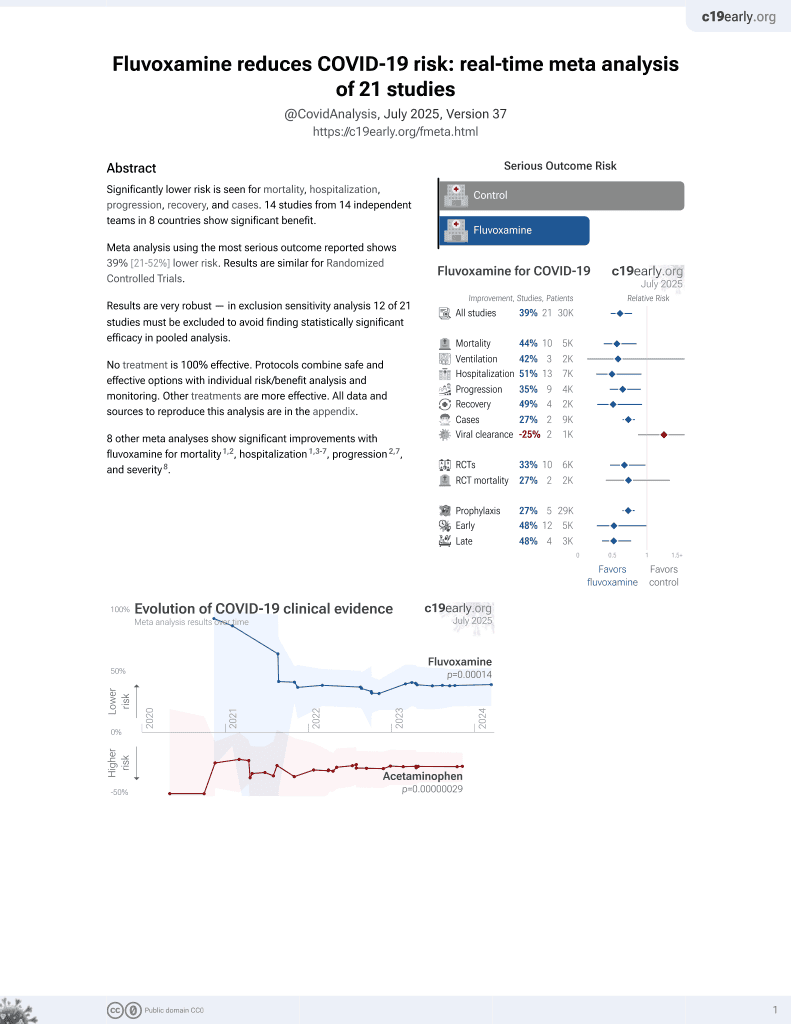
30th treatment shown to reduce risk in
November 2021, now with p = 0.00014 from 21 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
N3C retrospective reporting that common antidepressants may increase the risk of COVID-19 complications, while certain antidepressants were associated with a lower risk of worse outcomes. Machine learning methods as used in this study can improve accuracy, however they add complexity and can also reduce accuracy. In this case, the results of the two methods are conflicting. The first method raises concern for overfitting - authors use an 18,584 dimension covariate vector for each person, which is larger than the number of patients for each medication analyzed. The second 128 dimension embedding should improve results but authors report more extreme effects including biased results for the control outcomes. It's also not clear why the control outcomes includes items like bone fracture as opposed to common COVID-19 confounding factors.
Rahman et al., 11 Apr 2023, retrospective, France, peer-reviewed, 4 authors.
Contact: mohammadariful_alam@uml.edu.
Effects of Antidepressants on COVID-19 Outcomes: Retrospective Study on Large-Scale Electronic Health Record Data
Interactive Journal of Medical Research, doi:10.2196/39455
Background: Antidepressants exert an anticholinergic effect in varying degrees, and various classes of antidepressants can produce a different effect on immune function. While the early use of antidepressants has a notional effect on COVID-19 outcomes, the relationship between the risk of COVID-19 severity and the use of antidepressants has not been properly investigated previously owing to the high costs involved with clinical trials. Large-scale observational data and recent advancements in statistical analysis provide ample opportunity to virtualize a clinical trial to discover the detrimental effects of the early use of antidepressants. Objective: We primarily aimed to investigate electronic health records for causal effect estimation and use the data for discovering the causal effects of early antidepressant use on COVID-19 outcomes. As a secondary aim, we developed methods for validating our causal effect estimation pipeline. Methods: We used the National COVID Cohort Collaborative (N3C), a database aggregating health history for over 12 million people in the United States, including over 5 million with a positive COVID-19 test. We selected 241,952 COVID-19-positive patients (age >13 years) with at least 1 year of medical history. The study included a 18,584-dimensional covariate vector for each person and 16 different antidepressants. We used propensity score weighting based on the logistic regression method to estimate causal effects on the entire data. Then, we used the Node2Vec embedding method to encode SNOMED-CT (Systematized Nomenclature of Medicine-Clinical Terms) medical codes and applied random forest regression to estimate causal effects. We used both methods to estimate causal effects of antidepressants on COVID-19 outcomes. We also selected few negatively effective conditions for COVID-19 outcomes and estimated their effects using our proposed methods to validate their efficacy.
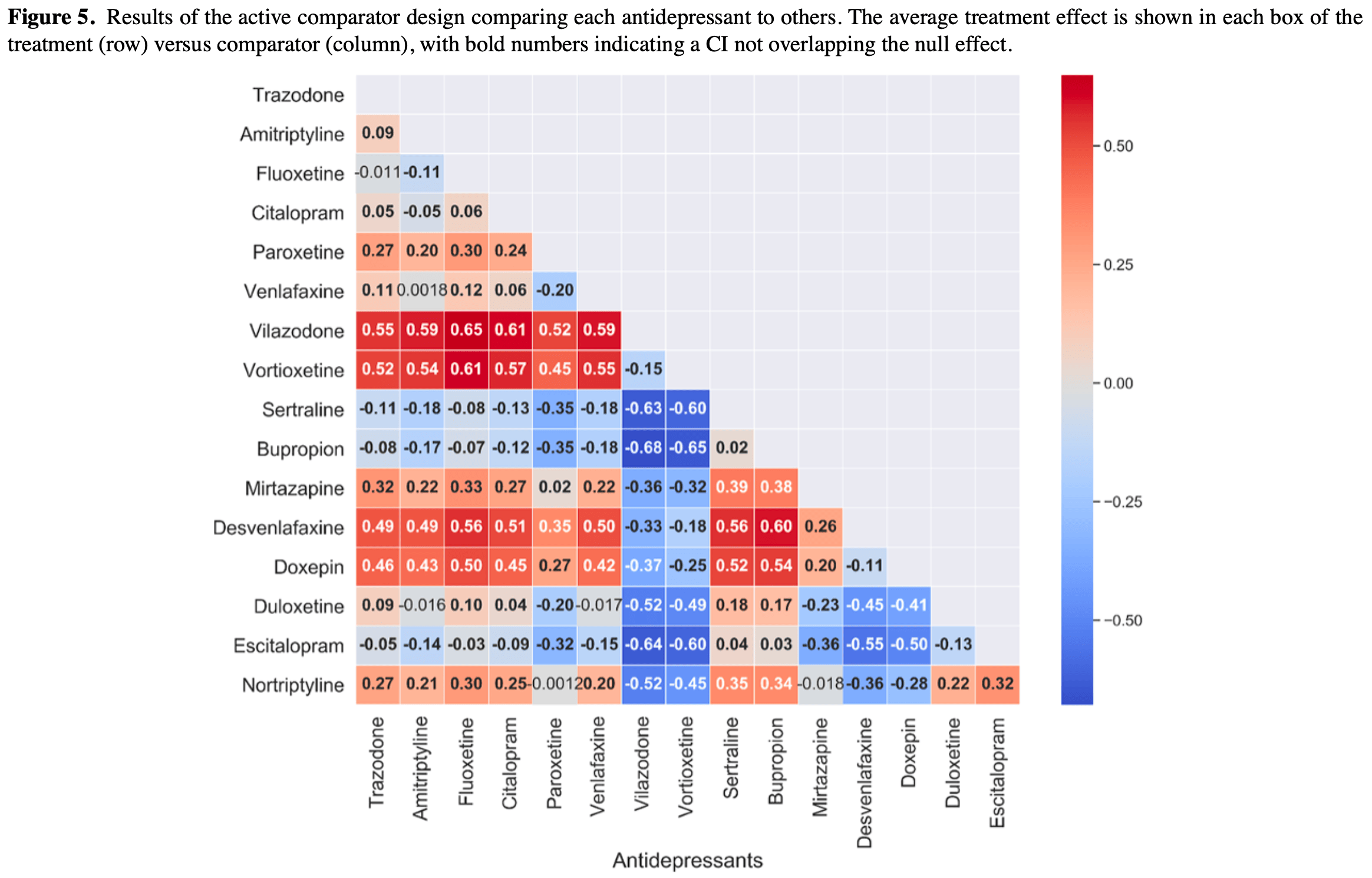
Results: The average treatment effect (ATE) of using any one of the antidepressants was −0.076 (95% CI −0.082 to −0.069; P<.001) with the propensity score weighting method. For the method using SNOMED-CT medical embedding, the ATE of using any one of the antidepressants was −0.423 (95% CI −0.382 to −0.463; P<.001).
Conclusions: We applied multiple causal inference methods with novel application of health embeddings to investigate the effects of antidepressants on COVID-19 outcomes. Additionally, we proposed a novel drug effect analysis-based evaluation technique to justify the efficacy of the proposed method. This study offers causal inference methods on large-scale electronic health record data to discover the effects of common antidepressants on COVID-19 hospitalization or a worse outcome. We found that common antidepressants may increase the risk of COVID-19 complications and uncovered a pattern where certain antidepressants were associated with a lower risk of hospitalization. While discovering the detrimental effects of these drugs on..
Conflicts of Interest None declared.
Abbreviations
References
Abramovich, Grinshtein, High-Dimensional Classification by Sparse Logistic Regression, IEEE Trans. Inform. Theory, doi:10.1109/tit.2018.2884963
Aygün, Kaya, Alhajj, Identifying side effects of commonly used drugs in the treatment of Covid 19, Sci Rep, doi:10.1038/s41598-020-78697-1
Beigel, Tomashek, Dodd, Mehta, Zingman et al., Remdesivir for the Treatment of Covid-19 -Final Report, N Engl J Med, doi:10.1056/nejmoa2007764
Bennett, Moffitt, Hajagos, Amor, Anand et al., The National COVID Cohort Collaborative: Clinical Characterization and Early Severity Prediction, medRxiv Preprint posted online on, doi:10.1101/2021.01.12.21249511
Bhatti, Khamis, Khatib, Shiraz, Matfin, Clinical Characteristics and Outcomes of Patients With Diabetes Admitted for COVID-19 Treatment in Dubai: Single-Centre Cross-Sectional Study, JMIR Public Health Surveill, doi:10.2196/22471
Biswas, Rahaman, Biswas, Haque, Association of Sex, Age, and Comorbidities with Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis, Intervirology, doi:10.1159/000512592
Bonner, Cvejic, Ayre, Isautier, Semsarian et al., The Psychological Impact of Hypertension During COVID-19 Restrictions: Retrospective Case-Control Study, JMIRx Med, doi:10.2196/25610
Brody, Gu, Antidepressant Use Among Adults: United States
Clelland, Ramiah, Steinberg, Clelland, Analysis of the impact of antidepressants and other medications on COVID-19 infection risk in a chronic psychiatric in-patient cohort, BJPsych Open, doi:10.1192/bjo.2021.1053
Fang, Karakiulakis, Roth, Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?, The Lancet Respiratory Medicine, doi:10.1016/s2213-2600(20)30116-8
Fitzgerald, Misguided drug advice for COVID-19, Science, doi:10.1126/science.abb8034
Gamble, Pham, Goyal, Cafazzo, The Challenges of COVID-19 for People Living With Diabetes: Considerations for Digital Health, JMIR Diabetes, doi:10.2196/19581
Gao, Zheng, Wang, Sun, Pan et al., Obesity Is a Risk Factor for Greater COVID-19 Severity, Diabetes Care, doi:10.2337/dc20-0682
Gerayeli, Milne, Cheung, Li, Yang et al., COPD and the risk of poor outcomes in COVID-19: A systematic review and meta-analysis, EClinicalMedicine, doi:10.1016/j.eclinm.2021.100789
Ghassemi, Marshall, Singh, Stone, Celi, Leveraging a critical care database: selective serotonin reuptake inhibitor use prior to ICU admission is associated with increased hospital mortality, Chest, doi:10.1378/chest.13-1722
Goldstein, Lee, Demographic perspectives on the mortality of COVID-19 and other epidemics, Proc Natl Acad Sci U S A, doi:10.1073/pnas.2006392117
Haendel, Chute, Bennett, Eichmann, Guinney et al., The National COVID Cohort Collaborative (N3C): Rationale, design, infrastructure, and deployment, J Am Med Inform Assoc, doi:10.1093/jamia/ocaa196
Hernán, Robins, Using Big Data to Emulate a Target Trial When a Randomized Trial Is Not Available, Am J Epidemiol, doi:10.1093/aje/kwv254
Hippisley-Cox, Young, Coupland, Channon, Tan et al., Risk of severe COVID-19 disease with ACE inhibitors and angiotensin receptor blockers: cohort study including 8.3 million people, Heart, doi:10.1136/heartjnl-2020-317393
Hoertel, Do the Selective Serotonin Reuptake Inhibitor Antidepressants Fluoxetine and Fluvoxamine Reduce Mortality Among Patients With COVID-19?, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.36510
Hoertel, Sánchez-Rico, Cougoule, Gulbins, Kornhuber et al., Repurposing antidepressants inhibiting the sphingomyelinase acid/ceramide system against COVID-19: current evidence and potential mechanisms, Mol Psychiatry, doi:10.1038/s41380-021-01254-3
Hoertel, Sánchez-Rico, Vernet, Beeker, Jannot et al., Universities / INSERM COVID-19 Research CollaborationAP-HP COVID CDR Initiative. Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study, Mol Psychiatry, doi:10.1038/s41380-021-01021-4
Israel, Schäffer, Cicurel, Cheng, Sinha et al., Identification of drugs associated with reduced severity of COVID-19 -a case-control study in a large population, Elife, doi:10.7554/eLife.68165
Kamyari, Soltanian, Mahjub, Moghimbeigi, Diet, Nutrition, Obesity, and Their Implications for COVID-19 Mortality: Development of a Marginalized Two-Part Model for Semicontinuous Data, JMIR Public Health Surveill, doi:10.2196/22717
Kang, Jung, Age-Related Morbidity and Mortality among Patients with COVID-19, Infect Chemother, doi:10.3947/ic.2020.52.2.154
Kornhuber, Hoertel, Gulbins, The acid sphingomyelinase/ceramide system in COVID-19, Mol Psychiatry, doi:10.1038/s41380-021-01309-5
Lee, Lessler, Stuart, Improving propensity score weighting using machine learning, Stat Med, doi:10.1002/sim.3782
Lenze, Mattar, Zorumski, Stevens, Schweiger et al., Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients With Symptomatic COVID-19: A Randomized Clinical Trial, JAMA, doi:10.1001/jama.2020.22760
Leung, Niikura, Yang, Sin, COVID-19 and COPD, Eur Respir J, doi:10.1183/13993003.02108-2020
Li, Morgan, Zaslavsky, Balancing Covariates via Propensity Score Weighting, Journal of the American Statistical Association, doi:10.1080/01621459.2016.1260466
Mas, García-Vicente, Estrada-Gelonch, Pérez-Mañá, Papaseit et al., Antidepressant Drugs and COVID-19: A Review of Basic and Clinical Evidence, J Clin Med, doi:10.3390/jcm11144038
Melamed, Using indication embeddings to represent patient health for drug safety studies, JAMIA Open, doi:10.1093/jamiaopen/ooaa040
Mesas, Cavero-Redondo, Álvarez-Bueno, Cabrera, De Andrade et al., Predictors of in-hospital COVID-19 mortality: A comprehensive systematic review and meta-analysis exploring differences by age, sex and health conditions, PLoS One, doi:10.1371/journal.pone.0241742
Oskotsky, Maric, Tang, Oskotsky, Wong et al., Mortality Risk Among Patients With COVID-19 Prescribed Selective Serotonin Reuptake Inhibitor Antidepressants, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.33090
Pan, Bai, Propensity score methods for causal inference: an overview, Behaviormetrika, doi:10.1007/s41237-018-0058-8
Pattisapu, Patil, Palshikar, Varma, Medical Concept Normalization by Encoding Target Knowledge
Popkin, Du, Green, Beck, Algaith et al., Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships, Obes Rev, doi:10.1111/obr.13128
Rahman, Mahi, Melamed, National COVID Cohort Collaborative SNOMED-CT: Systematized Nomenclature of Medicine-Clinical Terms SNRI: serotonin and norepinephrine reuptake inhibitor SSRI: selective serotonin reuptake inhibitor Edited by T Leung, A Mavragani, Data Interact J Med Res
Reese, Coleman, Chan, Blau, Callahan et al., NSAID use and clinical outcomes in COVID-19 patients: a 38-center retrospective cohort study, Virol J, doi:10.1186/s12985-022-01813-2
Ryan, Schuemie, Gruber, Zorych, Madigan, Empirical performance of a new user cohort method: lessons for developing a risk identification and analysis system, Drug Saf, doi:10.1007/s40264-013-0099-6
Schiffrin, Flack, Ito, Muntner, Webb, Hypertension and COVID-19, Am J Hypertens, doi:10.1093/ajh/hpaa057
Schneeweiss, Rassen, Glynn, Avorn, Mogun et al., High-dimensional propensity score adjustment in studies of treatment effects using health care claims data, Epidemiology, doi:10.1097/EDE.0b013e3181a663cc
Schuemie, Ryan, Dumouchel, Suchard, Madigan, Interpreting observational studies: why empirical calibration is needed to correct p-values, Stat Med, doi:10.1002/sim.5925
Sidik, Common antidepressant slashes risk of COVID death, study says, Nature, doi:10.1038/d41586-021-02988-4
Smoller, Allison, Cochrane, Curb, Perlis et al., Antidepressant use and risk of incident cardiovascular morbidity and mortality among postmenopausal women in the Women's Health Initiative study, Arch Intern Med, doi:10.1001/archinternmed.2009.436
Tal-Singer, Crapo, COPD at the Time of COVID-19: A COPD Foundation Perspective, Chronic Obstr Pulm Dis, doi:10.15326/jcopdf.7.2.2020.0149
Vancouver, None
Wingert, Pillay, Gates, Guitard, Rahman et al., Risk factors for severity of COVID-19: a rapid review to inform vaccine prioritisation in Canada, BMJ Open, doi:10.1136/bmjopen-2020-044684
Zhao, Meng, Kumar, Wu, Huang et al., The impact of COPD and smoking history on the severity of COVID-19: A systemic review and meta-analysis, J Med Virol, doi:10.1002/jmv.25889
Zhu, Zhang, Li, Yang, Song, A Novel Coronavirus from Patients with Pneumonia in China, 2019, N Engl J Med, doi:10.1056/nejmoa2001017
©md Mahmudur Rahman, Munawara Mahi, Melamed, Arif, Alam, Originally published in the Interactive Journal of Medical Research
DOI record:
{
"DOI": "10.2196/39455",
"ISSN": [
"1929-073X"
],
"URL": "http://dx.doi.org/10.2196/39455",
"abstract": "<jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>Antidepressants exert an anticholinergic effect in varying degrees, and various classes of antidepressants can produce a different effect on immune function. While the early use of antidepressants has a notional effect on COVID-19 outcomes, the relationship between the risk of COVID-19 severity and the use of antidepressants has not been properly investigated previously owing to the high costs involved with clinical trials. Large-scale observational data and recent advancements in statistical analysis provide ample opportunity to virtualize a clinical trial to discover the detrimental effects of the early use of antidepressants.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Objective</jats:title>\n <jats:p>We primarily aimed to investigate electronic health records for causal effect estimation and use the data for discovering the causal effects of early antidepressant use on COVID-19 outcomes. As a secondary aim, we developed methods for validating our causal effect estimation pipeline.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>We used the National COVID Cohort Collaborative (N3C), a database aggregating health history for over 12 million people in the United States, including over 5 million with a positive COVID-19 test. We selected 241,952 COVID-19–positive patients (age >13 years) with at least 1 year of medical history. The study included a 18,584-dimensional covariate vector for each person and 16 different antidepressants. We used propensity score weighting based on the logistic regression method to estimate causal effects on the entire data. Then, we used the Node2Vec embedding method to encode SNOMED-CT (Systematized Nomenclature of Medicine-Clinical Terms) medical codes and applied random forest regression to estimate causal effects. We used both methods to estimate causal effects of antidepressants on COVID-19 outcomes. We also selected few negatively effective conditions for COVID-19 outcomes and estimated their effects using our proposed methods to validate their efficacy.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>The average treatment effect (ATE) of using any one of the antidepressants was −0.076 (95% CI −0.082 to −0.069; P<.001) with the propensity score weighting method. For the method using SNOMED-CT medical embedding, the ATE of using any one of the antidepressants was −0.423 (95% CI −0.382 to −0.463; P<.001).</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusions</jats:title>\n <jats:p>We applied multiple causal inference methods with novel application of health embeddings to investigate the effects of antidepressants on COVID-19 outcomes. Additionally, we proposed a novel drug effect analysis–based evaluation technique to justify the efficacy of the proposed method. This study offers causal inference methods on large-scale electronic health record data to discover the effects of common antidepressants on COVID-19 hospitalization or a worse outcome. We found that common antidepressants may increase the risk of COVID-19 complications and uncovered a pattern where certain antidepressants were associated with a lower risk of hospitalization. While discovering the detrimental effects of these drugs on outcomes could guide preventive care, identification of beneficial effects would allow us to propose drug repurposing for COVID-19 treatment.</jats:p>\n </jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-8546-2970",
"affiliation": [],
"authenticated-orcid": false,
"family": "Rahman",
"given": "Md Mahmudur",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-3771-0295",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mahi",
"given": "Atqiya Munawara",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3089-9806",
"affiliation": [],
"authenticated-orcid": false,
"family": "Melamed",
"given": "Rachel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2240-0916",
"affiliation": [],
"authenticated-orcid": false,
"family": "Alam",
"given": "Mohammad Arif Ul",
"sequence": "additional"
}
],
"container-title": "Interactive Journal of Medical Research",
"container-title-short": "Interact J Med Res",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
3,
5
]
],
"date-time": "2023-03-05T07:36:41Z",
"timestamp": 1678001801000
},
"deposited": {
"date-parts": [
[
2023,
4,
11
]
],
"date-time": "2023-04-11T13:30:43Z",
"timestamp": 1681219843000
},
"indexed": {
"date-parts": [
[
2023,
4,
12
]
],
"date-time": "2023-04-12T04:19:49Z",
"timestamp": 1681273189397
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
4,
11
]
]
},
"language": "en",
"member": "1010",
"original-title": [],
"page": "e39455",
"prefix": "10.2196",
"published": {
"date-parts": [
[
2023,
4,
11
]
]
},
"published-online": {
"date-parts": [
[
2023,
4,
11
]
]
},
"publisher": "JMIR Publications Inc.",
"reference": [
{
"DOI": "10.1056/nejmoa2001017",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"key": "ref2",
"unstructured": "Responding to community spread of COVID-19World Health Organization2023-03-09https://www.who.int/publications/i/item/responding-to-community-spread-of-covid-19"
},
{
"DOI": "10.1101/2021.01.12.21249511",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1136/bmjopen-2020-044684",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.3947/ic.2020.52.2.154",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1159/000512592",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1371/journal.pone.0241742",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1073/pnas.2006392117",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.2337/dc20-0682",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1111/obr.13128",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.2196/22717",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1002/jmv.25889",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1016/j.eclinm.2021.100789",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1183/13993003.02108-2020",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.15326/jcopdf.7.2.2020.0149",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.2196/19581",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.2196/22471",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1016/s2213-2600(20)30116-8",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1093/ajh/hpaa057",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.2196/25610",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1038/s41598-020-78697-1",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1126/science.abb8034",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1186/s12985-022-01813-2",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1056/nejmoa2007764",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1136/heartjnl-2020-317393",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"key": "ref26",
"unstructured": "BrodyDJGuQAntidepressant Use Among Adults: United States, 2015-2018CDC20202023-03-09https://www.cdc.gov/nchs/products/databriefs/db377.htm"
},
{
"DOI": "10.1001/archinternmed.2009.436",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1378/chest.13-1722",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1038/s41380-021-01021-4",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1192/bjo.2021.1053",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1001/jamanetworkopen.2021.36510",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1038/d41586-021-02988-4",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.3390/jcm11144038",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.7554/eLife.68165",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1097/EDE.0b013e3181a663cc",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"key": "ref36",
"unstructured": "PattisapuNPatilSPalshikarGVarmaVMedical Concept Normalization by Encoding Target KnowledgeProceedings of the Machine Learning for Health NeurIPS Workshop, PMLR2019Machine Learning for Health WorkshopDecember 13, 2019Vancouver, BC, Canada246259"
},
{
"key": "ref37",
"unstructured": "All about antidepressantsMedical News Today2023-03-09https://www.medicalnewstoday.com/articles/248320"
},
{
"DOI": "10.1093/jamia/ocaa196",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1080/01621459.2016.1260466",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1002/sim.3782",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1007/s41237-018-0058-8",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1109/tit.2018.2884963",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.1093/jamiaopen/ooaa040",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1093/aje/kwv254",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.1007/s40264-013-0099-6",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1002/sim.5925",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.1001/jama.2020.22760",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.1001/jamanetworkopen.2021.33090",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.1038/s41380-021-01254-3",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1038/s41380-021-01309-5",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"key": "ref51",
"unstructured": "National COVID Cohort Collaborative2023-04-10https://covid.cd2h.org/"
}
],
"reference-count": 51,
"references-count": 51,
"relation": {
"has-preprint": [
{
"asserted-by": "object",
"id": "10.2196/preprints.39455",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "https://www.i-jmr.org/2023/1/e39455"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Effects of Antidepressants on COVID-19 Outcomes: Retrospective Study on Large-Scale Electronic Health Record Data",
"type": "journal-article",
"volume": "12"
}