The association between vitamin D deficiency and the clinical outcomes of hospitalized COVID-19 patients
et al., F1000Research, doi:10.12688/f1000research.132214.4, Apr 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of hospitalized patients in Indonesia, showing higher risk of mortality and severe cases with vitamin D deficiency.
This is the 174th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 94.8% lower, RR 0.05, p = 0.04, high D levels (≥20ng/mL) 0 of 45 (0.0%), low D levels (<20ng/mL) 14 of 146 (9.6%), NNT 10, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm).
|
|
risk of severe case, 77.6% lower, RR 0.22, p = 0.01, high D levels (≥20ng/mL) 2 of 45 (4.4%), low D levels (<20ng/mL) 29 of 146 (19.9%), NNT 6.5.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Rachman et al., 13 Apr 2023, prospective, Indonesia, peer-reviewed, 4 authors, study period October 2021 - February 2022.
Contact: andhika.rachman@office.ui.ac.id.
Impact of vitamin D deficiency in relation to the clinical outcomes of hospitalized COVID-19 patients
F1000Research, doi:10.12688/f1000research.132214.1
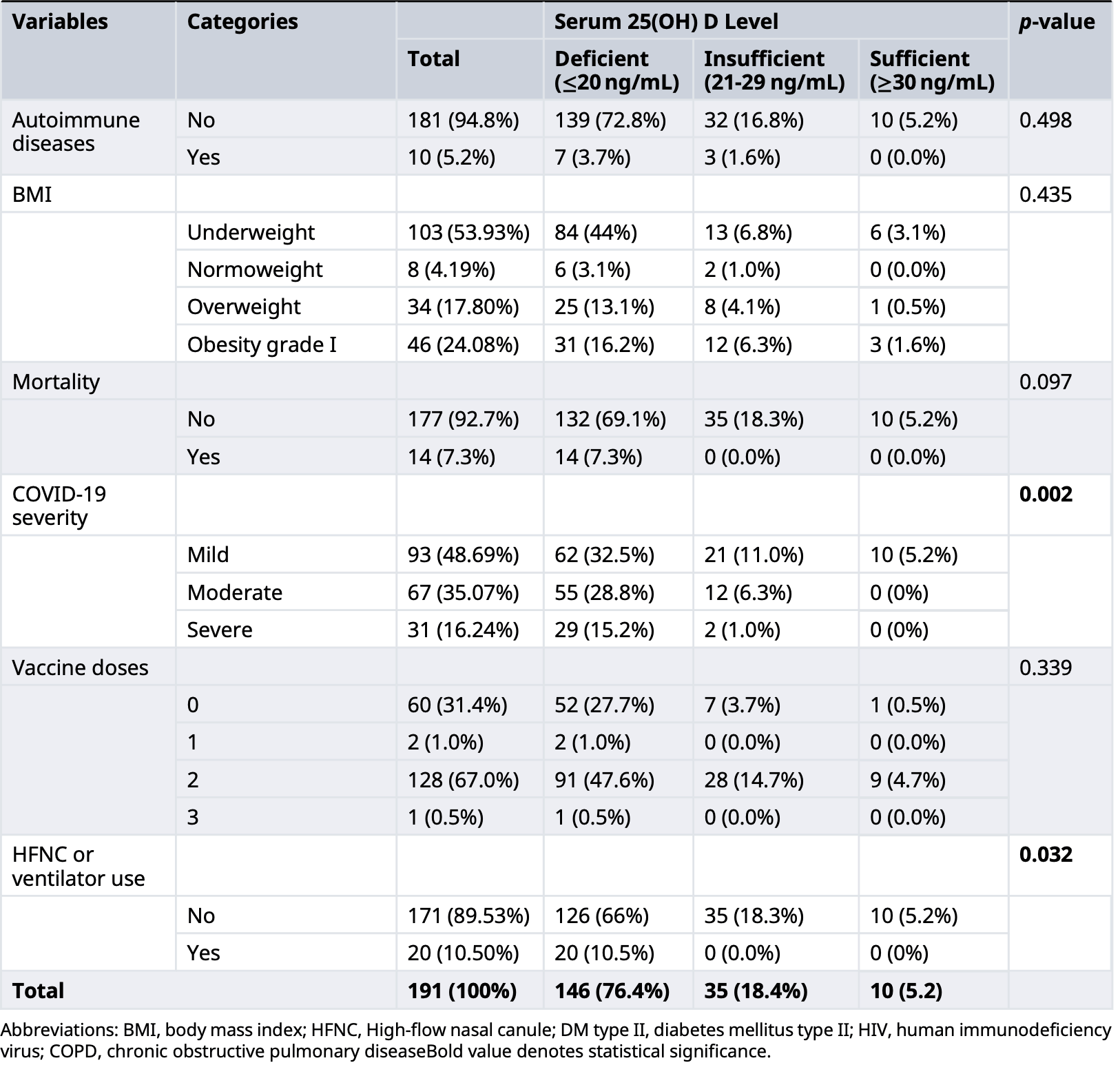
Background: Vitamin D deficiency is an emerging public health problem that affects more than one billion people worldwide. Vitamin D has been shown to be effective in preventing and reducing the severity of viral respiratory diseases, including influenza. However, the role of vitamin D in COVID-19 infection remains controversial. This study aimed to analyze the impact of vitamin D deficiency on the clinical outcome of hospitalized COVID-19 patients. Methods: A prospective cohort study was conducted among hospitalized COVID-19 patients at two COVID-19 referral hospitals in Indonesia from October 2021 until February 2022. Results: The median serum 25(OH)D level in 191 hospitalized COVID-19 patients was 13.6 [IQR=10.98] ng/mL. The serum 25(OH)D levels were significantly lower among COVID-19 patients with vitamin D deficiency who had cardiovascular disease (p-value=0.04), the use of a ventilator (p-value=0.004), more severe COVID-19 cases (p-value=0.047), and mortality (p-value=0.002). Furthermore, serum 25(OH)D levels were significantly different between patients with mild and severe COVID-19 cases (p-value=0.019). Serum 25(OH)D levels in moderate and severe COVID-19 cases were significantly different (p-value=0.031). Lower serum 25(OH)D levels were significantly associated with an increased number of comorbidities (p-value=0.03), the severity of COVID-19 (p-value=0.002), and the use of mechanical ventilation (p-value=0.032). Mortality was found in 7.3% of patients with deficient vitamin D levels. However, patients with either sufficient or insufficient vitamin D levels did not develop mortality. Conclusions: COVID-19 patients with vitamin D deficiency were significantly associated with having cardiovascular disease, mortality, more severe COVID-19 cases, and the used of mechanical ventilation. Lower serum 25(OH)D levels were associated with an increased Open Peer Review Approval Status AWAITING PEER REVIEW Any reports and responses or comments on the article can be found at the end of the article.
References
Adams, Ren, Liu, Vitamin D-Directed Rheostatic Regulation of Monocyte Antibacterial Responses, J. Immunol
Alathari, Aji, Ariyasra, Interaction between Vitamin D-Related Genetic Risk Score and Carbohydrate Intake on Body Fat Composition: A Study in Southeast Asian Minangkabau Women, Nutrients, doi:10.3390/nu13020326
Angelidi, Belanger, Lorinsky, Vitamin D Status Is Associated With In-Hospital Mortality and Mechanical Ventilation: A Cohort of COVID-19 Hospitalized Patients, Mayo Clin. Proc
Antonopoulos, Sanna, Sabharwal, Detecting human coronary inflammation by imaging perivascular fat, Sci. Transl. Med
Benskin, A Basic Review of the Preliminary Evidence That COVID-19 Risk and Severity Is Increased in Vitamin D Deficiency, Front. Public Health, doi:10.3389/fpubh.2020.00513
Boucher, The problems of vitamin d insufficiency in older people, Aging Dis
Bouillon, Marcocci, Carmeliet, Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105719
Cannell, Vieth, Umhau, Epidemic influenza and vitamin D, Epidemiol. Infect, doi:10.1017/S0950268806007175
Cantorna, Snyder, Lin, Vitamin D and 1,25(OH)2D Regulation of T cells, Nutrients, doi:10.3390/nu7043011
Cao, Wu, Faucon, SARS-CoV-2 & Covid-19: Key-Roles of the 'Renin-Angiotensin' System/Vitamin D Impacting Drug and Vaccine Developments, Infect. Disord. Drug Targets
Chiodini, Gatti, Soranna, Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes, Front. Public Health, doi:10.3389/fpubh.2021.736665
Cosentino, Campodonico, Milazzo, Vitamin D and Cardiovascular Disease: Current Evidence and Future Perspectives, Nutrients, doi:10.3390/nu13103603
Daneshkhah, Agrawal, Eshein, The Possible Role of Vitamin D in Suppressing Cytokine Storm and Associated Mortality in COVID-19 Patients, doi:10.1101/2020.04.08.20058578
De La Guía-Galipienso, Martínez-Ferran, Vallecillo, Vitamin D and cardiovascular health, Clin. Nutr, doi:10.1016/j.clnu.2020.12.025
Demer, Hsu, Tintut, Steroid Hormone Vitamin D, Circ. Res
Dürr, Sudheendra, Ramamoorthy, LL-37, the only human member of the cathelicidin family of antimicrobial peptides, Biochimica et Biophysica Acta (BBA), doi:10.1016/j.bbamem.2006.03.030
Franczyk, Stolarz-Skrzypek, Wesołowska, Vitamin D and Vitamin D Receptor Activators in Treatment of Hypertension and Cardiovascular Disease, Cardiovasc. Hematol. Disord. Drug Targets, doi:10.2174/1871529X14666140228122836
Freundlich, Li, Quiroz, Paricalcitol Downregulates Myocardial Renin-Angiotensin and Fibroblast Growth Factor Expression and Attenuates Cardiac Hypertrophy in Uremic Rats, Am. J. Hypertens, doi:10.1093/ajh/hpt177
Godlee, Covid-19: Transparency and communication are key, BMJ, doi:10.1136/bmj.m4764
Grant, Lahore, Mcdonnell, Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Gruber-Bzura, Vitamin D and Influenza-Prevention or Therapy?, Int. J. Mol. Sci, doi:10.3390/ijms19082419
Gupta, Harrison, Ho, Development and validation of the ISARIC 4C Deterioration model for adults hospitalised with COVID-19: a prospective cohort study, Lancet Respir. Med
Hafez, Saleh, Arya, Vitamin D Status in Relation to the Clinical Outcome of Hospitalized COVID-19 Patients, Front. Med, doi:10.3389/fmed.2022.843737
Hiemstra, Lim, Thadhani, Vitamin D and Atherosclerotic Cardiovascular Disease, J. Clin. Endocrinol. Metab
Holick, Vitamin, Deficiency, N. Engl. J. Med, doi:10.1056/NEJMra070553
Hribar, Cobbold, Church, Potential Role of Vitamin D in the Elderly to Resist COVID-19 and to Slow Progression of Parkinson's Disease, Brain Sci, doi:10.3390/brainsci10050284
Hu, Guo, Zhou, Characteristics of SARS-CoV-2 and COVID-19, Nat. Rev. Microbiol, doi:10.1038/s41579-020-00459-7
Huang, Soleimani, Herasevich, Clinical Characteristics, Treatment, and Outcomes of Critically Ill Patients With COVID-19: A Scoping Review, Mayo Clin. Proc, doi:10.1016/j.mayocp.2020.10.022
Jeffery, Burke, Mura, 1,25-Dihydroxyvitamin D3 and IL-2 Combine to Inhibit T Cell Production of Inflammatory Cytokines and Promote Development of Regulatory T Cells Expressing CTLA-4 and FoxP3, J. Immunol, doi:10.4049/jimmunol.0803217
Kalichuran, Van Blydenstein, Venter, Vitamin D status and COVID-19 severity, S. Afr. J. Infect. Dis, doi:10.4102/sajid.v37i1.359
Kankova, Luini, Pedrazzoni, Inhibition of cytokine production by vitamin D3 deficiency, Int. J. Immunopharmacol, doi:10.1016/0192-0561(91)90315-X
Khammissa, Fourie, Motswaledi, The Biological Activities of Vitamin D and Its Receptor in Relation to Calcium and Bone Homeostasis, Cancer, Immune and Cardiovascular Systems, Skin Biology, and Oral Health, Biomed. Res. Int
Knight, Ho, Pius, Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score, BMJ, doi:10.1136/bmj.m3339
Laing, Lewis, New Concepts in Vitamin D Requirements for Children and Adolescents: A Controversy Revisited
Lemire, Adams, Kermani-Arab, 1,25-Dihydroxyvitamin D3 suppresses human T helper/inducer lymphocyte activity in vitro, J. Immunol
Liss, Frishman, Vitamin D, Cardiol. Rev, doi:10.1097/CRD.0b013e31822c5380
Liu, Stenger, Li, Toll-Like Receptor Triggering of a Vitamin D-Mediated Human Antimicrobial Response, Science
Louw, Werbeck, Louw, Blood vitamin concentrations during the acute-phase response, Crit. Care Med, doi:10.1097/00003246-199207000-00007
Ludvigsson, Appelros, Askling, Adaptation of the Charlson Comorbidity Index for Register-Based Research in Sweden, Clin. Epidemiol, doi:10.2147/CLEP.S282475
Mancuso, Rahman, Hershey, 1,25-Dihydroxyvitamin-D3 Treatment Reduces Cardiac Hypertrophy and Left Ventricular Diameter in Spontaneously Hypertensive Heart Failure-prone (cp/+) Rats Independent of Changes in Serum Leptin, J. Cardiovasc. Pharmacol, doi:10.1097/FJC.0b013e3181761906
Manson, Bassuk, Eliminating vitamin D deficiency during the COVID-19 pandemic: A call to action, Metabolism, doi:10.1016/j.metabol.2020.154322
Mansur, Letter: low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity, Aliment. Pharmacol. Ther
Mccullough, Lehrer, Amend, Daily oral dosing of vitamin D3 using 5000 TO 50,000 international units a day in long-term hospitalized patients: Insights from a seven year experience, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2018.12.010
Mohamed, Abdelsalam, Maghraby, Performance Features and Mortality Prediction of the 4C Score Early in COVID-19 Infection: A Retrospective Study in Saudi Arabia, J. Investig. Med, doi:10.1136/jim-2021-001940
Mohammad, Mishra, Ashraf, Emerging Role of Vitamin D and its Associated Molecules in Pathways Related to Pathogenesis of Thrombosis, Biomolecules, doi:10.3390/biom9110649
Mohan, Cherian, Sharma, Schoor, Exploring links between vitamin D deficiency and COVID-19, Best Pract. Res. Clin. Endocrinol. Metab, doi:10.1016/j.beem.2011.06.007
Mora, Iwata, Von Andrian, Vitamin effects on the immune system: vitamins A and D take centre stage, Nat. Rev. Immunol
Nair, Maseeh, Vitamin D: The "sunshine" vitamin, J. Pharmacol. Pharmacother
Ni, Watts, Ng, Elimination of Vitamin D Receptor in Vascular Endothelial Cells Alters Vascular Function
Nimitphong, Holick, Vitamin D and Respiratory Tract Infections: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, Dermatoendocrinology, doi:10.1371/journal.pone.0065835
Oh, Matkovich, Riek, Macrophage secretion of miR-106b-5p causes renin-dependent hypertension, Nat. Commun, doi:10.1038/s41467-020-18538-x
Pal, Banerjee, Bhadada, Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis, doi:10.1098/rsos.201912
Palacios, Gonzalez, Is vitamin D deficiency a major global public health problem?, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2013.11.003
Patients, Figshare, None, Journal Contribution, doi:10.6084/m9.figshare.22145768.v2
Pilz, Tomaschitz, Role of vitamin D in arterial hypertension, Expert. Rev. Cardiovasc. Ther, doi:10.1586/erc.10.142
Pinzon, Angela, Pradana, Vitamin D deficiency among patients with COVID-19: case series and recent literature review, Trop. Med. Health, doi:10.1186/s41182-020-00277-w
Pulungan, Soesanti, Tridjaja, Vitamin D insufficiency and its contributing factors in primary school-aged children in Indonesia, a sun-rich country, Ann. Pediatr. Endocrinol. Metab
Quraishi, De Pascale, Needleman, Effect of Cholecalciferol Supplementation on Vitamin D Status and Cathelicidin Levels in Sepsis, Crit. Care Med, doi:10.1097/CCM.0000000000001148
Reid, Talwar, Toole, PP434 ACUTE CHANGES IN THE SYSTEMIC INFLAMMATORY RESPONSE IS ASSOCIATED WITH TRANSIENT DECREASES IN CIRCULATING 25-HYDROXYVITAMIN D CONCENTRATIONS FOLLOWING ELECTIVE KNEE ARTHROPLASTY, Clin. Nutr. Suppl, doi:10.1016/S1744-1161(10)70509-3
Sabetta, Depetrillo, Cipriani, Serum 25-Hydroxyvitamin D and the Incidence of Acute Viral Respiratory Tract Infections in Healthy Adults, PLoS One, doi:10.1371/journal.pone.0011088
Sawicki, Van Rompay, Au, Sun-Exposed Skin Color Is Associated with Changes in Serum 25-Hydroxyvitamin D in Racially/Ethnically Diverse Children, J. Nutr, doi:10.3945/jn.115.222505
Shen, Mei, Zhang, The Effect of Vitamin D Supplementation on Clinical Outcomes for Critically Ill Patients: A Systemic Review and Meta-Analysis of Randomized Clinical Trials, Front. Nutr, doi:10.3389/fnut.2021.664940
Siddiqee, Bhattacharjee, Siddiqi, High prevalence of vitamin D deficiency among the South Asian adults: a systematic review and meta-analysis, BMC Public Health, doi:10.1186/s12889-021-11888-1
Teymoori-Rad, Shokri, Salimi, The interplay between vitamin D and viral infections, Rev. Med. Virol, doi:10.1002/rmv.2032
Tian, Rong, Letter: Covid-19, and vitamin D. Authors' reply, Aliment. Pharmacol. Ther, doi:10.1111/apt.15764
Vazquez, Huerta-Delgado, Castillo, Correlation of Vitamin D with Inflammatory Cytokines, Atherosclerotic Parameters, and Lifestyle Factors in the Setting of Heart Failure: A 12-Month Follow-Up Study, Int. J. Mol. Sci, doi:10.3390/ijms20225811
Wang, Nestel, Bourdeau, Cutting Edge: 1,25-Dihydroxyvitamin D3 Is a Direct Inducer of Antimicrobial Peptide Gene Expression, J. Immunol
Weishaar, Simpson, Involvement of vitamin D3 with cardiovascular function. II. Direct and indirect effects, Am. J. Physiol. Endocrinol. Metab, doi:10.1152/ajpendo.1987.253.6.E675
Wellbelove, Walsh, Perinpanathan, Comparing the 4C mortality score for COVID-19 to established scores (CURB65, CRB65, qSOFA, NEWS) for respiratory infection patients, J. Infect
Wöbke, Sorg, Steinhilber, Vitamin D in inflammatory diseases, Front. Physiol, doi:10.3389/fphys.2014.00244
Xu, Yang, Chen, Vitamin D alleviates lipopolysaccharideinduced acute lung injury via regulation of the reninangiotensin system, Mol. Med. Rep, doi:10.3892/mmr.2017.7546
Zhou, Zhang, Qu, Coronavirus disease 2019 (COVID-19): a clinical update, Front. Med, doi:10.1007/s11684-020-0767-8
DOI record:
{
"DOI": "10.12688/f1000research.132214.4",
"ISSN": [
"2046-1402"
],
"URL": "http://dx.doi.org/10.12688/f1000research.132214.4",
"abstract": "<ns3:p>Background Vitamin D deficiency is an emerging public health problem that affects more than one billion people worldwide. Vitamin D has been shown to be effective in preventing and reducing the severity of viral respiratory diseases, including influenza. However, the role of vitamin D in COVID-19 infection remains controversial. This study aimed to analyze the association of vitamin D deficiency on the clinical outcome of hospitalized COVID-19 patients. Methods A prospective cohort study was conducted among hospitalized COVID-19 patients at two COVID-19 referral hospitals in Indonesia from October 2021 until February 2022. Results The median serum 25(OH)D level in 191 hospitalized COVID-19 patients was 13.6 [IQR=10.98] ng/mL. The serum 25(OH)D levels were significantly lower among COVID-19 patients with vitamin D deficiency who had cardiovascular disease (p-value=0.04), the use of a ventilator (p-value=0.004), more severe COVID-19 cases (p-value=0.047), and mortality (p-value=0.002). Furthermore, serum 25(OH)D levels were significantly different between patients with mild and severe COVID-19 cases (p-value=0.019). Serum 25(OH)D levels in moderate and severe COVID-19 cases were significantly different (p-value=0.031). Lower serum 25(OH)D levels were significantly associated with an increased number of comorbidities (p-value=0.03), the severity of COVID-19 (p-value=0.002), and the use of mechanical ventilation (p-value=0.032). Mortality was found in 7.3% of patients with deficient vitamin D levels. However, patients with either sufficient or insufficient vitamin D levels did not develop mortality. Conclusions COVID-19 patients with vitamin D deficiency were significantly associated with having cardiovascular disease, mortality, more severe COVID-19 cases, and the used of mechanical ventilation. Lower serum 25(OH)D levels were associated with an increased number of comorbidities, COVID-19 severity, and the use of mechanical-ventilation. Thus, we suggest hospitalized COVID-19 patients to reach a sufficient vitamin D status to improve the clinical outcome of the disease.</ns3:p>",
"assertion": [
{
"URL": "https://f1000research.com/articles/12-394/v4#article-reports",
"group": {
"label": "Current Referee Status",
"name": "current-referee-status"
},
"label": "Referee status",
"name": "referee-status",
"order": 0,
"value": "Indexed"
},
{
"URL": "https://f1000research.com/articles/12-394/v2#referee-response-178400",
"group": {
"label": "Article Reports",
"name": "article-reports"
},
"label": "Referee Report",
"name": "referee-response-178400",
"order": 0,
"value": "10.5256/f1000research.148441.r178400, Shaun Sabico, Department of Biochemistry College of Science, King Saud University, Riyadh, Riyadh Province, 14 Jun 2023, version 2, 1 approved, 1 not approved"
},
{
"URL": "https://f1000research.com/articles/12-394/v3#referee-response-205417",
"group": {
"label": "Article Reports",
"name": "article-reports"
},
"label": "Referee Report",
"name": "referee-response-205417",
"order": 1,
"value": "10.5256/f1000research.155718.r205417, Parvaiz Koul, Department of Pulmonary Medicine, Sher-i-Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, 17 Oct 2023, version 3, 1 approved, 1 approved with reservations, 2 not approved"
},
{
"URL": "https://f1000research.com/articles/12-394/v4#referee-response-243971",
"group": {
"label": "Article Reports",
"name": "article-reports"
},
"label": "Referee Report",
"name": "referee-response-243971",
"order": 2,
"value": "10.5256/f1000research.162135.r243971, Luigi di Filippo, Institute of Endocrine and Metabolic Sciences, Università Vita-Salute San Raffaele, IRCCS Ospedale San Raffaele, Milan, 27 Feb 2024, version 4, indexed"
},
{
"URL": "https://f1000research.com/articles/12-394/v3#referee-response-233579",
"group": {
"label": "Article Reports",
"name": "article-reports"
},
"label": "Referee Report",
"name": "referee-response-233579",
"order": 3,
"value": "10.5256/f1000research.155718.r233579, Guo-Xun Chen, Department of Nutrition, University of Tennessee, Knoxville, 19 Jan 2024, version 3, 1 approved, 1 approved with reservations, 2 not approved"
},
{
"label": "Grant Information",
"name": "grant-information",
"order": 4,
"value": "This research was funded by Directorate of Research and Development, Universitas Indonesia’s grant program “Hibah PUTI 2022” (grant number: ND-5463/UN2.F1.D1.4/PPM.00.00/2022). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript."
},
{
"label": "Copyright",
"name": "copyright-info",
"order": 0,
"value": "This is an open access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3246-3352",
"affiliation": [],
"authenticated-orcid": false,
"family": "Rachman",
"given": "Andhika",
"sequence": "first"
},
{
"affiliation": [],
"family": "Rahmaniyah",
"given": "Rizky",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Khomeini",
"given": "Andi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Iriani",
"given": "Anggraini",
"sequence": "additional"
}
],
"container-title": "F1000Research",
"container-title-short": "F1000Res",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"f1000research.com"
]
},
"created": {
"date-parts": [
[
2024,
2,
5
]
],
"date-time": "2024-02-05T16:15:14Z",
"timestamp": 1707149714000
},
"deposited": {
"date-parts": [
[
2024,
2,
27
]
],
"date-time": "2024-02-27T06:00:18Z",
"timestamp": 1709013618000
},
"funder": [
{
"award": [
"ND-5463/UN2.F1.D1.4/PPM.00.00/2022"
],
"name": "This research was funded by Directorate of Research and Development, Universitas Indonesia’s grant program “Hibah PUTI 2022”"
}
],
"indexed": {
"date-parts": [
[
2024,
3,
3
]
],
"date-time": "2024-03-03T00:18:04Z",
"timestamp": 1709425084653
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2024,
2,
5
]
]
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
2,
5
]
],
"date-time": "2024-02-05T00:00:00Z",
"timestamp": 1707091200000
}
}
],
"link": [
{
"URL": "https://f1000research.com/articles/12-394/v4/xml",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://f1000research.com/articles/12-394/v4/pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://f1000research.com/articles/12-394/v4/iparadigms",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "2560",
"original-title": [],
"page": "394",
"prefix": "10.12688",
"published": {
"date-parts": [
[
2024,
2,
5
]
]
},
"published-online": {
"date-parts": [
[
2024,
2,
5
]
]
},
"publisher": "F1000 Research Ltd",
"reference": [
{
"DOI": "10.3389/fpubh.2021.736665",
"article-title": "Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes.",
"author": "I Chiodini",
"doi-asserted-by": "publisher",
"journal-title": "Front. Public Health.",
"key": "ref1",
"volume": "9",
"year": "2021 Dec 22"
},
{
"DOI": "10.1007/s11684-020-0767-8",
"article-title": "Coronavirus disease 2019 (COVID-19): a clinical update.",
"author": "M Zhou",
"doi-asserted-by": "publisher",
"first-page": "126-135",
"journal-title": "Front. Med.",
"key": "ref2",
"volume": "14",
"year": "2020 Apr 2"
},
{
"DOI": "10.1038/s41579-020-00459-7",
"article-title": "Characteristics of SARS-CoV-2 and COVID-19.",
"author": "B Hu",
"doi-asserted-by": "publisher",
"first-page": "141-154",
"journal-title": "Nat. Rev. Microbiol.",
"key": "ref3",
"volume": "19",
"year": "2021 Mar 6"
},
{
"DOI": "10.4102/sajid.v37i1.359",
"article-title": "Vitamin D status and COVID-19 severity.",
"author": "S Kalichuran",
"doi-asserted-by": "publisher",
"journal-title": "S. Afr. J. Infect. Dis.",
"key": "ref4",
"volume": "37",
"year": "2022 Apr 26"
},
{
"DOI": "10.1016/j.mayocp.2020.10.022",
"article-title": "Clinical Characteristics, Treatment, and Outcomes of Critically Ill Patients With COVID-19: A Scoping Review.",
"author": "C Huang",
"doi-asserted-by": "publisher",
"first-page": "183-202",
"journal-title": "Mayo Clin. Proc.",
"key": "ref5",
"volume": "96",
"year": "2021 Jan"
},
{
"DOI": "10.1136/jim-2021-001940",
"article-title": "Performance Features and Mortality Prediction of the 4C Score Early in COVID-19 Infection: A Retrospective Study in Saudi Arabia.",
"author": "R Mohamed",
"doi-asserted-by": "publisher",
"first-page": "421-427",
"journal-title": "J. Investig. Med.",
"key": "ref6",
"volume": "70",
"year": "2022 Feb 5"
},
{
"DOI": "10.3389/fmed.2022.843737",
"article-title": "Vitamin D Status in Relation to the Clinical Outcome of Hospitalized COVID-19 Patients.",
"author": "W Hafez",
"doi-asserted-by": "publisher",
"journal-title": "Front. Med. (Lausanne).",
"key": "ref7",
"volume": "9",
"year": "2022 Mar 29"
},
{
"DOI": "10.3390/ijms19082419",
"article-title": "Vitamin D and Influenza—Prevention or Therapy?",
"author": "B Gruber-Bzura",
"doi-asserted-by": "publisher",
"first-page": "2419",
"journal-title": "Int. J. Mol. Sci.",
"key": "ref8",
"volume": "19",
"year": "2018 Aug 16"
},
{
"DOI": "10.1002/rmv.2032",
"article-title": "The interplay between vitamin D and viral infections.",
"author": "M Teymoori-Rad",
"doi-asserted-by": "publisher",
"first-page": "e2032",
"journal-title": "Rev. Med. Virol.",
"key": "ref9",
"volume": "29",
"year": "2019 Mar"
},
{
"DOI": "10.1210/er.2018-00126",
"article-title": "Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions.",
"author": "R Bouillon",
"doi-asserted-by": "publisher",
"first-page": "1109-1151",
"journal-title": "Endocr. Rev.",
"key": "ref10",
"volume": "40",
"year": "2019 Aug 1"
},
{
"DOI": "10.1016/j.jsbmb.2020.105719",
"article-title": "Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections.",
"author": "J Quesada-Gomez",
"doi-asserted-by": "publisher",
"first-page": "105719",
"journal-title": "J. Steroid Biochem. Mol. Biol.",
"key": "ref11",
"volume": "202",
"year": "2020 Sep"
},
{
"DOI": "10.1371/journal.ppat.1008874",
"article-title": "Exploring links between vitamin D deficiency and COVID-19.",
"author": "M Mohan",
"doi-asserted-by": "publisher",
"first-page": "e1008874",
"journal-title": "PLoS Pathog.",
"key": "ref12",
"volume": "16",
"year": "2020 Sep 18"
},
{
"DOI": "10.1016/j.beem.2011.06.007",
"article-title": "Worldwide vitamin D status.",
"author": "N Schoor",
"doi-asserted-by": "publisher",
"first-page": "671-680",
"journal-title": "Best Pract. Res. Clin. Endocrinol. Metab.",
"key": "ref13",
"volume": "25",
"year": "2011 Aug"
},
{
"DOI": "10.1016/j.jsbmb.2013.11.003",
"article-title": "Is vitamin D deficiency a major global public health problem?",
"author": "C Palacios",
"doi-asserted-by": "publisher",
"first-page": "138-145",
"journal-title": "J. Steroid Biochem. Mol. Biol.",
"key": "ref14",
"volume": "144",
"year": "2014 Oct"
},
{
"DOI": "10.1186/s12889-021-11888-1",
"article-title": "High prevalence of vitamin D deficiency among the South Asian adults: a systematic review and meta-analysis.",
"author": "M Siddiqee",
"doi-asserted-by": "publisher",
"first-page": "1823",
"journal-title": "BMC Public Health.",
"key": "ref15",
"volume": "21",
"year": "2021 Dec 9"
},
{
"DOI": "10.4103/0976-500X.95506",
"article-title": "Vitamin D: The “sunshine” vitamin.",
"author": "R Nair",
"doi-asserted-by": "publisher",
"first-page": "118-126",
"journal-title": "J. Pharmacol. Pharmacother.",
"key": "ref16",
"volume": "3",
"year": "2012 Apr"
},
{
"DOI": "10.1056/NEJMra070553",
"article-title": "Deficiency.",
"author": "M Holick",
"doi-asserted-by": "publisher",
"first-page": "266-281",
"journal-title": "N. Engl. J. Med.",
"key": "ref17",
"volume": "357",
"year": "2007 Jul 19"
},
{
"DOI": "10.4161/derm.24054",
"article-title": "Vitamin D status and sun exposure in southeast Asia.",
"author": "H Nimitphong",
"doi-asserted-by": "publisher",
"first-page": "34-37",
"journal-title": "Dermatoendocrinology.",
"key": "ref18",
"volume": "5",
"year": "2013 Jan 27"
},
{
"DOI": "10.1371/journal.pone.0065835",
"article-title": "Vitamin D and Respiratory Tract Infections: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.",
"author": "P Bergman",
"doi-asserted-by": "publisher",
"first-page": "e65835",
"journal-title": "PLoS One.",
"key": "ref19",
"volume": "8",
"year": "2013 Jun 19"
},
{
"DOI": "10.1017/S0950268806007175",
"article-title": "Epidemic influenza and vitamin D.",
"author": "J Cannell",
"doi-asserted-by": "publisher",
"first-page": "1129-1140",
"journal-title": "Epidemiol. Infect.",
"key": "ref20",
"volume": "134",
"year": "2006 Dec 7"
},
{
"DOI": "10.1371/journal.pone.0274158",
"article-title": "Using ISARIC 4C mortality score to predict dynamic changes in mortality risk in COVID-19 patients during hospital admission.",
"author": "T Crocker-Buque",
"doi-asserted-by": "publisher",
"journal-title": "PLoS One.",
"key": "ref81",
"volume": "17",
"year": "2022 Oct 12"
},
{
"DOI": "10.1136/bmj.m4764",
"article-title": "Covid-19: Transparency and communication are key.",
"author": "F Godlee",
"doi-asserted-by": "publisher",
"first-page": "m4764",
"journal-title": "BMJ.",
"key": "ref21",
"year": "2020 Dec 10"
},
{
"DOI": "10.1016/S1744-1161(10)70509-3",
"article-title": "PP434 ACUTE CHANGES IN THE SYSTEMIC INFLAMMATORY RESPONSE IS ASSOCIATED WITH TRANSIENT DECREASES IN CIRCULATING 25-HYDROXYVITAMIN D CONCENTRATIONS FOLLOWING ELECTIVE KNEE ARTHROPLASTY.",
"author": "D Reid",
"doi-asserted-by": "publisher",
"first-page": "193",
"journal-title": "Clin. Nutr. Suppl.",
"key": "ref22",
"volume": "5",
"year": "2010 Jan"
},
{
"DOI": "10.1097/00003246-199207000-00007",
"article-title": "Blood vitamin concentrations during the acute-phase response.",
"author": "J Louw",
"doi-asserted-by": "publisher",
"first-page": "934-941",
"journal-title": "Crit. Care Med.",
"key": "ref23",
"volume": "20",
"year": "1992 Jul"
},
{
"DOI": "10.21109/kesmas.v0i0.5233",
"article-title": "Epidemiological and Clinical Features of COVID-19 Patients at National Emergency Hospital Wisma Atlet Kemayoran, Jakarta, Indonesia.",
"author": "A Susanto",
"doi-asserted-by": "publisher",
"first-page": "11-16",
"journal-title": "Kesmas.",
"key": "ref82",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1177/0145561320953231",
"article-title": "Diagnosis of SARS-CoV-2 by RT-PCR Using Different Sample Sources: Review of the Literature.",
"author": "S Torretta",
"doi-asserted-by": "publisher",
"journal-title": "Ear Nose Throat J.",
"key": "ref77",
"volume": "100",
"year": "2021 Apr"
},
{
"DOI": "10.1016/j.clnu.2020.12.025",
"article-title": "Vitamin D and cardiovascular health.",
"author": "F Guía-Galipienso",
"doi-asserted-by": "publisher",
"first-page": "2946-2957",
"journal-title": "Clin. Nutr.",
"key": "ref31",
"volume": "40",
"year": "2021 May"
},
{
"DOI": "10.2147/CLEP.S282475",
"article-title": "Adaptation of the Charlson Comorbidity Index for Register-Based Research in Sweden.",
"author": "J Ludvigsson",
"doi-asserted-by": "publisher",
"first-page": "21-41",
"journal-title": "Clin. Epidemiol.",
"key": "ref24",
"volume": "13",
"year": "2021 Jan"
},
{
"DOI": "10.1016/S2213-2600(20)30559-2",
"article-title": "Development and validation of the ISARIC 4C Deterioration model for adults hospitalised with COVID-19: a prospective cohort study.",
"author": "R Gupta",
"doi-asserted-by": "publisher",
"first-page": "349-359",
"journal-title": "Lancet Respir. Med.",
"key": "ref25",
"volume": "9",
"year": "2021 Apr"
},
{
"DOI": "10.1186/s41182-020-00277-w",
"article-title": "Vitamin D deficiency among patients with COVID-19: case series and recent literature review.",
"author": "R Pinzon",
"doi-asserted-by": "publisher",
"first-page": "102",
"journal-title": "Trop. Med. Health.",
"key": "ref26",
"volume": "48",
"year": "2020 Dec 20"
},
{
"DOI": "10.3390/nu13020326",
"article-title": "Interaction between Vitamin D-Related Genetic Risk Score and Carbohydrate Intake on Body Fat Composition: A Study in Southeast Asian Minangkabau Women.",
"author": "B Alathari",
"doi-asserted-by": "publisher",
"first-page": "326",
"journal-title": "Nutrients.",
"key": "ref27",
"volume": "13",
"year": "2021 Jan 23"
},
{
"DOI": "10.6065/apem.2040132.066",
"article-title": "Vitamin D insufficiency and its contributing factors in primary school-aged children in Indonesia, a sun-rich country.",
"author": "A Pulungan",
"doi-asserted-by": "publisher",
"first-page": "92-98",
"journal-title": "Ann. Pediatr. Endocrinol. Metab.",
"key": "ref28",
"volume": "26",
"year": "2021 Jun 30"
},
{
"DOI": "10.3945/jn.115.222505",
"article-title": "Sun-Exposed Skin Color Is Associated with Changes in Serum 25-Hydroxyvitamin D in Racially/Ethnically Diverse Children.",
"author": "C Sawicki",
"doi-asserted-by": "publisher",
"first-page": "751-757",
"journal-title": "J. Nutr.",
"key": "ref29",
"volume": "146",
"year": "2016 Apr"
},
{
"article-title": "New Concepts in Vitamin D Requirements for Children and Adolescents: A Controversy Revisited.",
"author": "E Laing",
"first-page": "42-65",
"key": "ref30",
"year": "2018"
},
{
"DOI": "10.1007/s12020-023-03481-w",
"article-title": "Lack of vitamin D predicts impaired long-term immune response to COVID-19 vaccination.",
"author": "L Filippo",
"doi-asserted-by": "publisher",
"first-page": "536-541",
"journal-title": "Endocrine.",
"key": "ref96",
"volume": "82",
"year": "2023"
},
{
"DOI": "10.1210/clinem/dgad327",
"article-title": "Response to the Letter to the Editor From Min et al: Low Vitamin D Levels are Associated With Long COVID Syndrome in COVID-19 Survivors.",
"author": "L Filippo",
"doi-asserted-by": "publisher",
"first-page": "e438-e439",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref97",
"volume": "109",
"year": "2023"
},
{
"DOI": "10.1210/clinem/dgad207",
"article-title": "Low Vitamin D Levels Are Associated With Long COVID Syndrome in COVID-19 Survivors.",
"author": "L Filippo",
"doi-asserted-by": "publisher",
"first-page": "e1106-e1116",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref98",
"volume": "108",
"year": "2023"
},
{
"DOI": "10.1097/CRD.0b013e31822c5380",
"article-title": "Vitamin D.",
"author": "Y Liss",
"doi-asserted-by": "publisher",
"first-page": "038-044",
"journal-title": "Cardiol. Rev.",
"key": "ref32",
"volume": "20",
"year": "2012 Jan"
},
{
"DOI": "10.3390/nu13103603",
"article-title": "Vitamin D and Cardiovascular Disease: Current Evidence and Future Perspectives.",
"author": "N Cosentino",
"doi-asserted-by": "publisher",
"first-page": "3603",
"journal-title": "Nutrients.",
"key": "ref33",
"volume": "13",
"year": "2021 Oct 14"
},
{
"DOI": "10.2174/1871529X14666140228122836",
"article-title": "Vitamin D and Vitamin D Receptor Activators in Treatment of Hypertension and Cardiovascular Disease.",
"author": "A Franczyk",
"doi-asserted-by": "publisher",
"first-page": "34-44",
"journal-title": "Cardiovasc. Hematol. Disord. Drug Targets.",
"key": "ref34",
"volume": "14",
"year": "2014 Feb 28"
},
{
"DOI": "10.1161/HYPERTENSIONAHA.114.03971",
"article-title": "Elimination of Vitamin D Receptor in Vascular Endothelial Cells Alters Vascular Function.",
"author": "W Ni",
"doi-asserted-by": "publisher",
"first-page": "1290-1298",
"journal-title": "Hypertension.",
"key": "ref35",
"volume": "64",
"year": "2014 Dec"
},
{
"DOI": "10.1155/2018/9276380",
"article-title": "The Biological Activities of Vitamin D and Its Receptor in Relation to Calcium and Bone Homeostasis, Cancer, Immune and Cardiovascular Systems, Skin Biology, and Oral Health.",
"author": "R Khammissa",
"doi-asserted-by": "publisher",
"first-page": "1-9",
"journal-title": "Biomed. Res. Int.",
"key": "ref36",
"volume": "2018",
"year": "2018"
},
{
"DOI": "10.1152/ajpendo.1987.253.6.E675",
"article-title": "Involvement of vitamin D3 with cardiovascular function. II. Direct and indirect effects.",
"author": "R Weishaar",
"doi-asserted-by": "publisher",
"first-page": "E675-E683",
"journal-title": "Am. J. Physiol. Endocrinol. Metab.",
"key": "ref37",
"volume": "253",
"year": "1987 Dec 1"
},
{
"DOI": "10.1097/FJC.0b013e3181761906",
"article-title": "1,25-Dihydroxyvitamin-D3 Treatment Reduces Cardiac Hypertrophy and Left Ventricular Diameter in Spontaneously Hypertensive Heart Failure-prone (cp/+) Rats Independent of Changes in Serum Leptin.",
"author": "P Mancuso",
"doi-asserted-by": "publisher",
"first-page": "559-564",
"journal-title": "J. Cardiovasc. Pharmacol.",
"key": "ref38",
"volume": "51",
"year": "2008 Jun"
},
{
"DOI": "10.1586/erc.10.142",
"article-title": "Role of vitamin D in arterial hypertension.",
"author": "S Pilz",
"doi-asserted-by": "publisher",
"first-page": "1599-1608",
"journal-title": "Expert. Rev. Cardiovasc. Ther.",
"key": "ref39",
"volume": "8",
"year": "2010 Nov 10"
},
{
"DOI": "10.1210/jc.2019-00194",
"article-title": "Vitamin D and Atherosclerotic Cardiovascular Disease.",
"author": "T Hiemstra",
"doi-asserted-by": "publisher",
"first-page": "4033-4050",
"journal-title": "J. Clin. Endocrinol. Metab.",
"key": "ref40",
"volume": "104",
"year": "2019 Sep 1"
},
{
"DOI": "10.1093/ajh/hpt177",
"article-title": "Paricalcitol Downregulates Myocardial Renin-Angiotensin and Fibroblast Growth Factor Expression and Attenuates Cardiac Hypertrophy in Uremic Rats.",
"author": "M Freundlich",
"doi-asserted-by": "publisher",
"first-page": "720-726",
"journal-title": "Am. J. Hypertens.",
"key": "ref41",
"volume": "27",
"year": "2014 May 1"
},
{
"DOI": "10.3892/mmr.2017.7546",
"article-title": "Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system.",
"author": "J Xu",
"doi-asserted-by": "publisher",
"first-page": "7432-7438",
"journal-title": "Mol. Med. Rep.",
"key": "ref42",
"volume": "16",
"year": "2017 May"
},
{
"DOI": "10.1038/s41467-020-18538-x",
"article-title": "Macrophage secretion of miR-106b-5p causes renin-dependent hypertension.",
"author": "J Oh",
"doi-asserted-by": "publisher",
"first-page": "4798",
"journal-title": "Nat. Commun.",
"key": "ref43",
"volume": "11",
"year": "2020 Sep 23"
},
{
"DOI": "10.3390/ijms20225811",
"article-title": "Correlation of Vitamin D with Inflammatory Cytokines, Atherosclerotic Parameters, and Lifestyle Factors in the Setting of Heart Failure: A 12-Month Follow-Up Study.",
"author": "D Roffe-Vazquez",
"doi-asserted-by": "publisher",
"first-page": "5811",
"journal-title": "Int. J. Mol. Sci.",
"key": "ref44",
"volume": "20",
"year": "2019 Nov 19"
},
{
"DOI": "10.3389/fphys.2014.00244",
"article-title": "Vitamin D in inflammatory diseases.",
"author": "T Wöbke",
"doi-asserted-by": "publisher",
"journal-title": "Front. Physiol.",
"key": "ref45",
"volume": "5",
"year": "2014 Jul 2"
},
{
"DOI": "10.1126/scitranslmed.aal2658",
"article-title": "Detecting human coronary inflammation by imaging perivascular fat.",
"author": "A Antonopoulos",
"doi-asserted-by": "publisher",
"journal-title": "Sci. Transl. Med.",
"key": "ref46",
"volume": "9",
"year": "2017 Jul 12"
},
{
"DOI": "10.3389/fpubh.2020.00513",
"article-title": "A Basic Review of the Preliminary Evidence That COVID-19 Risk and Severity Is Increased in Vitamin D Deficiency.",
"author": "L Benskin",
"doi-asserted-by": "publisher",
"journal-title": "Front. Public Health.",
"key": "ref47",
"volume": "8",
"year": "2020 Sep 10"
},
{
"DOI": "10.3390/brainsci10050284",
"article-title": "Potential Role of Vitamin D in the Elderly to Resist COVID-19 and to Slow Progression of Parkinson’s Disease.",
"author": "C Hribar",
"doi-asserted-by": "publisher",
"first-page": "284",
"journal-title": "Brain Sci.",
"key": "ref48",
"volume": "10",
"year": "2020 May 8"
},
{
"DOI": "10.3390/nu12040988",
"article-title": "Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths.",
"author": "W Grant",
"doi-asserted-by": "publisher",
"first-page": "988",
"journal-title": "Nutrients.",
"key": "ref49",
"volume": "12",
"year": "2020 Apr 2"
},
{
"article-title": "The problems of vitamin d insufficiency in older people.",
"author": "B Boucher",
"first-page": "313-329",
"journal-title": "Aging Dis.",
"key": "ref50",
"volume": "3",
"year": "2012 Aug"
},
{
"DOI": "10.1371/journal.pone.0011088",
"article-title": "Serum 25-Hydroxyvitamin D and the Incidence of Acute Viral Respiratory Tract Infections in Healthy Adults.",
"author": "J Sabetta",
"doi-asserted-by": "publisher",
"first-page": "e11088",
"journal-title": "PLoS One.",
"key": "ref51",
"volume": "5",
"year": "2010 Jun 14"
},
{
"DOI": "10.1101/2020.04.08.20058578",
"article-title": "The Possible Role of Vitamin D in Suppressing Cytokine Storm and Associated Mortality in COVID-19 Patients.",
"author": "A Daneshkhah",
"doi-asserted-by": "publisher",
"key": "ref52",
"year": "2020"
},
{
"DOI": "10.1111/apt.15764",
"article-title": "Letter: Covid-19, and vitamin D. Authors’ reply.",
"author": "Y Tian",
"doi-asserted-by": "publisher",
"first-page": "995-996",
"journal-title": "Aliment. Pharmacol. Ther.",
"key": "ref53",
"volume": "51",
"year": "2020 May"
},
{
"DOI": "10.1111/apt.15820",
"article-title": "Letter: low population mortality from COVID-19 in countries south of latitude 35 degrees North supports vitamin D as a factor determining severity.",
"author": "J Mansur",
"doi-asserted-by": "publisher",
"first-page": "411-412",
"journal-title": "Aliment. Pharmacol. Ther.",
"key": "ref54",
"volume": "52",
"year": "2020 Jul"
},
{
"DOI": "10.3390/biom9110649",
"article-title": "Emerging Role of Vitamin D and its Associated Molecules in Pathways Related to Pathogenesis of Thrombosis.",
"author": "M Mohammad",
"doi-asserted-by": "publisher",
"first-page": "649",
"journal-title": "Biomolecules.",
"key": "ref55",
"volume": "9",
"year": "2019 Oct 24"
},
{
"DOI": "10.2174/1871526520999200505174704",
"article-title": "SARS-CoV-2 & Covid-19: Key-Roles of the ‘Renin-Angiotensin’ System/Vitamin D Impacting Drug and Vaccine Developments.",
"author": "Z Cao",
"doi-asserted-by": "publisher",
"first-page": "348-349",
"journal-title": "Infect. Disord. Drug Targets.",
"key": "ref56",
"volume": "20",
"year": "2020 Jul 20"
},
{
"DOI": "10.3390/nu13072170",
"article-title": "Effects of a 2-Week 5000 IU versus 1000 IU Vitamin D3 Supplementation on Recovery of Symptoms in Patients with Mild to Moderate Covid-19: A Randomized Clinical Trial.",
"author": "S Sabico",
"doi-asserted-by": "publisher",
"first-page": "2170",
"journal-title": "Nutrients.",
"key": "ref78",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/j.jinf.2020.10.015",
"article-title": "Comparing the 4C mortality score for COVID-19 to established scores (CURB65, CRB65, qSOFA, NEWS) for respiratory infection patients.",
"author": "Z Wellbelove",
"doi-asserted-by": "publisher",
"first-page": "414-451",
"journal-title": "J. Infect.",
"key": "ref57",
"volume": "82",
"year": "2021 Mar"
},
{
"DOI": "10.1136/bmj.m3339",
"article-title": "Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score.",
"author": "S Knight",
"doi-asserted-by": "publisher",
"first-page": "m3339",
"journal-title": "BMJ.",
"key": "ref58",
"volume": "370",
"year": "2020 Sep 9"
},
{
"DOI": "10.1016/j.mayocp.2021.01.001",
"article-title": "Vitamin D Status Is Associated With In-Hospital Mortality and Mechanical Ventilation: A Cohort of COVID-19 Hospitalized Patients.",
"author": "A Angelidi",
"doi-asserted-by": "publisher",
"first-page": "875-886",
"journal-title": "Mayo Clin. Proc.",
"key": "ref59",
"volume": "96",
"year": "2021 Apr"
},
{
"DOI": "10.1007/s40520-021-01831-0",
"article-title": "Severe vitamin D deficiency is not related to SARS-CoV-2 infection but may increase mortality risk in hospitalized adults: a retrospective case–control study in an Arab Gulf country.",
"author": "A Alguwaihes",
"doi-asserted-by": "publisher",
"first-page": "1415-1422",
"journal-title": "Aging Clin. Exp. Res.",
"key": "ref79",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.1016/j.metabol.2020.154322",
"article-title": "Commentary. Eliminating vitamin D deficiency during the COVID-19 pandemic: A call to action.",
"author": "J Manson",
"doi-asserted-by": "publisher",
"first-page": "154322",
"journal-title": "Metabolism.",
"key": "ref60",
"volume": "112",
"year": "2020 Nov"
},
{
"DOI": "10.1186/s12967-021-02838-x",
"article-title": "Vitamin D status of Arab Gulf residents screened for SARS-CoV-2 and its association with COVID-19 infection: a multi-centre case–control study.",
"author": "N Al-Daghri",
"doi-asserted-by": "publisher",
"first-page": "166",
"journal-title": "J. Transl. Med.",
"key": "ref80",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.7759/cureus.26704",
"article-title": "Vitamin D Levels and Length of Hospitalization in Indian Patients With COVID-19: A Single-Center Prospective Study.",
"author": "A Dhar",
"doi-asserted-by": "publisher",
"journal-title": "Cureus.",
"key": "ref83",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1007/s12020-023-03331-9",
"article-title": "Low vitamin D levels predict outcomes of COVID-19 in patients with both severe and non-severe disease at hospitalization.",
"author": "L Filippo",
"doi-asserted-by": "publisher",
"first-page": "669-683",
"journal-title": "Endocrine.",
"key": "ref99",
"volume": "80",
"year": "2023"
},
{
"DOI": "10.1161/CIRCRESAHA.118.311585",
"article-title": "Steroid Hormone Vitamin D.",
"author": "L Demer",
"doi-asserted-by": "publisher",
"first-page": "1576-1585",
"journal-title": "Circ. Res.",
"key": "ref61",
"volume": "122",
"year": "2018 May 25"
},
{
"DOI": "10.4049/jimmunol.134.5.3032",
"article-title": "1,25-Dihydroxyvitamin D3 suppresses human T helper/inducer lymphocyte activity in vitro.",
"author": "J Lemire",
"doi-asserted-by": "publisher",
"first-page": "3032-3035",
"journal-title": "J. Immunol.",
"key": "ref62",
"volume": "134",
"year": "1985 May"
},
{
"DOI": "10.3390/nu7043011",
"article-title": "Vitamin D and 1,25(OH)2D Regulation of T cells.",
"author": "M Cantorna",
"doi-asserted-by": "publisher",
"first-page": "3011-3021",
"journal-title": "Nutrients.",
"key": "ref63",
"volume": "7",
"year": "2015 Apr 22"
},
{
"DOI": "10.4049/jimmunol.0803217",
"article-title": "1,25-Dihydroxyvitamin D3 and IL-2 Combine to Inhibit T Cell Production of Inflammatory Cytokines and Promote Development of Regulatory T Cells Expressing CTLA-4 and FoxP3.",
"author": "L Jeffery",
"doi-asserted-by": "publisher",
"first-page": "5458-5467",
"journal-title": "J. Immunol.",
"key": "ref64",
"volume": "183",
"year": "2009 Nov 1"
},
{
"article-title": "Toll-Like Receptor Triggering of a Vitamin D-Mediated Human Antimicrobial Response.",
"author": "P Liu",
"first-page": "1770-1773",
"journal-title": "Science (1979).",
"key": "ref65",
"volume": "311",
"year": "2006 Mar 24"
},
{
"DOI": "10.4049/jimmunol.0803736",
"article-title": "Vitamin D-Directed Rheostatic Regulation of Monocyte Antibacterial Responses.",
"author": "J Adams",
"doi-asserted-by": "publisher",
"first-page": "4289-4295",
"journal-title": "J. Immunol.",
"key": "ref66",
"volume": "182",
"year": "2009 Apr 1"
},
{
"DOI": "10.3389/fnut.2021.664940",
"article-title": "The Effect of Vitamin D Supplementation on Clinical Outcomes for Critically Ill Patients: A Systemic Review and Meta-Analysis of Randomized Clinical Trials.",
"author": "H Shen",
"doi-asserted-by": "publisher",
"journal-title": "Front. Nutr.",
"key": "ref67",
"volume": "8",
"year": "2021 May 4"
},
{
"DOI": "10.4049/jimmunol.173.5.2909",
"article-title": "Cutting Edge: 1,25-Dihydroxyvitamin D3 Is a Direct Inducer of Antimicrobial Peptide Gene Expression.",
"author": "T Wang",
"doi-asserted-by": "publisher",
"first-page": "2909-2912",
"journal-title": "J. Immunol.",
"key": "ref68",
"volume": "173",
"year": "2004 Sep 1"
},
{
"DOI": "10.1097/CCM.0000000000001148",
"article-title": "Effect of Cholecalciferol Supplementation on Vitamin D Status and Cathelicidin Levels in Sepsis.",
"author": "S Quraishi",
"doi-asserted-by": "publisher",
"first-page": "1928-1937",
"journal-title": "Crit. Care Med.",
"key": "ref69",
"volume": "43",
"year": "2015 Sep"
},
{
"DOI": "10.1016/j.bbamem.2006.03.030",
"article-title": "LL-37, the only human member of the cathelicidin family of antimicrobial peptides. Biochimica et Biophysica Acta (BBA).",
"author": "U Dürr",
"doi-asserted-by": "publisher",
"first-page": "1408-1425",
"journal-title": "Biomembranes.",
"key": "ref70",
"volume": "1758",
"year": "2006 Sep"
},
{
"DOI": "10.1038/nri2378",
"article-title": "Vitamin effects on the immune system: vitamins A and D take centre stage.",
"author": "J Mora",
"doi-asserted-by": "publisher",
"first-page": "685-698",
"journal-title": "Nat. Rev. Immunol.",
"key": "ref71",
"volume": "8",
"year": "2008 Sep"
},
{
"DOI": "10.1016/0192-0561(91)90315-X",
"article-title": "Inhibition of cytokine production by vitamin D3 deficiency.",
"author": "M Kankova",
"doi-asserted-by": "publisher",
"first-page": "773",
"journal-title": "Int. J. Immunopharmacol.",
"key": "ref72",
"volume": "13",
"year": "1991 Jan"
},
{
"DOI": "10.1038/s41533-021-00244-w",
"article-title": "A predictive score for progression of COVID-19 in hospitalized persons: a cohort study.",
"author": "J Xu",
"doi-asserted-by": "publisher",
"first-page": "33",
"journal-title": "NPJ Prim. Care Respir. Med.",
"key": "ref84",
"volume": "31",
"year": "2021 Jun 3"
},
{
"DOI": "10.1136/bmj.m1328",
"article-title": "Prediction models for diagnosis and prognosis of covid-19: systematic review and critical appraisal.",
"author": "L Wynants",
"doi-asserted-by": "publisher",
"journal-title": "BMJ.",
"key": "ref85",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1056/NEJMcp2009249",
"article-title": "Mild or Moderate Covid-19.",
"author": "R Gandhi",
"doi-asserted-by": "publisher",
"first-page": "1757-66",
"journal-title": "N. Engl. J. Med.",
"key": "ref86",
"volume": "383",
"year": "2020 Oct 29"
},
{
"DOI": "10.1016/j.jinf.2020.05.064",
"article-title": "A clinical risk score to identify patients with COVID-19 at high risk of critical care admission or death: An observational cohort study.",
"author": "J Galloway",
"doi-asserted-by": "publisher",
"first-page": "282-8",
"journal-title": "J. Infect.",
"key": "ref87",
"volume": "81",
"year": "2020 Aug"
},
{
"DOI": "10.1002/dmrr.3354",
"article-title": "Neck circumference as reliable predictor of mechanical ventilation support in adult inpatients with COVID-19: A multicentric prospective evaluation.",
"author": "S Di Bella",
"doi-asserted-by": "publisher",
"first-page": "e3354",
"journal-title": "Diabetes Metab. Res. Rev.",
"key": "ref88",
"volume": "37",
"year": "2021 Jan 14"
},
{
"DOI": "10.1016/j.jaci.2020.04.006",
"article-title": "Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan.",
"author": "X Li",
"doi-asserted-by": "publisher",
"first-page": "110-118",
"journal-title": "J. Allergy Clin. Immunol.",
"key": "ref89",
"volume": "146",
"year": "2020 Jul"
},
{
"DOI": "10.1183/13993003.00562-2020",
"article-title": "Clinical characteristics and outcomes of hospitalised patients with COVID-19 treated in Hubei (epicentre) and outside Hubei (non-epicentre): a nationwide analysis of China.",
"author": "W Liang",
"doi-asserted-by": "publisher",
"journal-title": "Eur. Respir. J.",
"key": "ref90",
"volume": "55",
"year": "2020 Jun"
},
{
"DOI": "10.15585/mmwr.mm6915e4",
"article-title": "Geographic Differences in COVID-19 Cases, Deaths, and Incidence — United States, February 12–April 7, 2020.",
"author": "S Bialek",
"doi-asserted-by": "publisher",
"first-page": "465-471",
"journal-title": "MMWR Morb. Mortal. Wkly. Rep.",
"key": "ref91",
"volume": "69",
"year": "2020 Apr 17"
},
{
"DOI": "10.1093/cid/ciaa443",
"article-title": "A Tool for Early Prediction of Severe Coronavirus Disease 2019 (COVID-19): A Multicenter Study Using the Risk Nomogram in Wuhan and Guangdong, China.",
"author": "J Gong",
"doi-asserted-by": "publisher",
"first-page": "833-40",
"journal-title": "Clin. Infect. Dis.",
"key": "ref92",
"volume": "71",
"year": "2020 Jul 28"
},
{
"DOI": "10.1016/S1473-3099(20)30243-7",
"article-title": "Estimates of the severity of coronavirus disease 2019: a model-based analysis.",
"author": "R Verity",
"doi-asserted-by": "publisher",
"first-page": "669-677",
"journal-title": "Lancet Infect. Dis.",
"key": "ref93",
"volume": "20",
"year": "2020 Jun"
},
{
"DOI": "10.1038/s41591-020-0822-7",
"article-title": "Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China.",
"author": "J Wu",
"doi-asserted-by": "publisher",
"first-page": "506-510",
"journal-title": "Nat. Med.",
"key": "ref94",
"volume": "26",
"year": "2020 Apr 1"
},
{
"DOI": "10.15585/mmwr.mm6912e2",
"article-title": "Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) — United States, February 12–March 16, 2020.",
"author": "S Bialek",
"doi-asserted-by": "publisher",
"first-page": "343-346",
"journal-title": "MMWR Morb. Mortal. Wkly. Rep.",
"key": "ref95",
"volume": "69",
"year": "2020 Mar 27"
},
{
"DOI": "10.1016/j.jsbmb.2018.12.010",
"article-title": "Daily oral dosing of vitamin D3 using 5000 TO 50,000 international units a day in long-term hospitalized patients: Insights from a seven year experience.",
"author": "P McCullough",
"doi-asserted-by": "publisher",
"first-page": "228-239",
"journal-title": "J. Steroid Biochem. Mol. Biol.",
"key": "ref73",
"volume": "189",
"year": "2019 May"
},
{
"DOI": "10.1007/s40618-021-01614-4",
"article-title": "Vitamin D supplementation and clinical outcomes in COVID-19: a systematic review and meta-analysis.",
"author": "R Pal",
"doi-asserted-by": "publisher",
"first-page": "53-68",
"journal-title": "J. Endocrinol. Investig.",
"key": "ref74",
"volume": "45",
"year": "2022 Jan 24"
},
{
"DOI": "10.1098/rsos.201912",
"article-title": "Vitamin D and COVID-19: evidence and recommendations for supplementation.",
"author": "G Griffin",
"doi-asserted-by": "publisher",
"first-page": "201912",
"journal-title": "R. Soc. Open Sci.",
"key": "ref75",
"volume": "7",
"year": "2020 Dec"
},
{
"DOI": "10.6084/m9.figshare.22145768.v2",
"article-title": "Raw Data - Impact of Vitamin D Deficiency in Relation to the Clinical Outcomes of Hospitalized COVID-19 Patients. figshare.",
"author": "A Rachman",
"doi-asserted-by": "publisher",
"journal-title": "Journal Contribution.",
"key": "ref76",
"year": "2023"
}
],
"reference-count": 99,
"references-count": 99,
"relation": {
"has-review": [
{
"asserted-by": "subject",
"id": "10.5256/f1000research.162135.r243971",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "https://f1000research.com/articles/12-394/v4"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "The association between vitamin D deficiency and the clinical outcomes of hospitalized COVID-19 patients",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.12688/f1000research.crossmark-policy",
"update-to": [
{
"DOI": "10.12688/f1000research.132214.1",
"label": "New version",
"type": "new_version",
"updated": {
"date-parts": [
[
2024,
2,
5
]
],
"date-time": "2024-02-05T00:00:00Z",
"timestamp": 1707091200000
}
},
{
"DOI": "10.12688/f1000research.132214.2",
"label": "New version",
"type": "new_version",
"updated": {
"date-parts": [
[
2024,
2,
5
]
],
"date-time": "2024-02-05T00:00:00Z",
"timestamp": 1707091200000
}
},
{
"DOI": "10.12688/f1000research.132214.3",
"label": "New version",
"type": "new_version",
"updated": {
"date-parts": [
[
2024,
2,
5
]
],
"date-time": "2024-02-05T00:00:00Z",
"timestamp": 1707091200000
}
}
],
"volume": "12"
}
