Vitamin D deficiency and COVID-19: A case-control study at a tertiary care hospital in India
et al., Annals of Medicine and Surgery, doi:10.1016/j.amsu.2021.102661, Aug 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
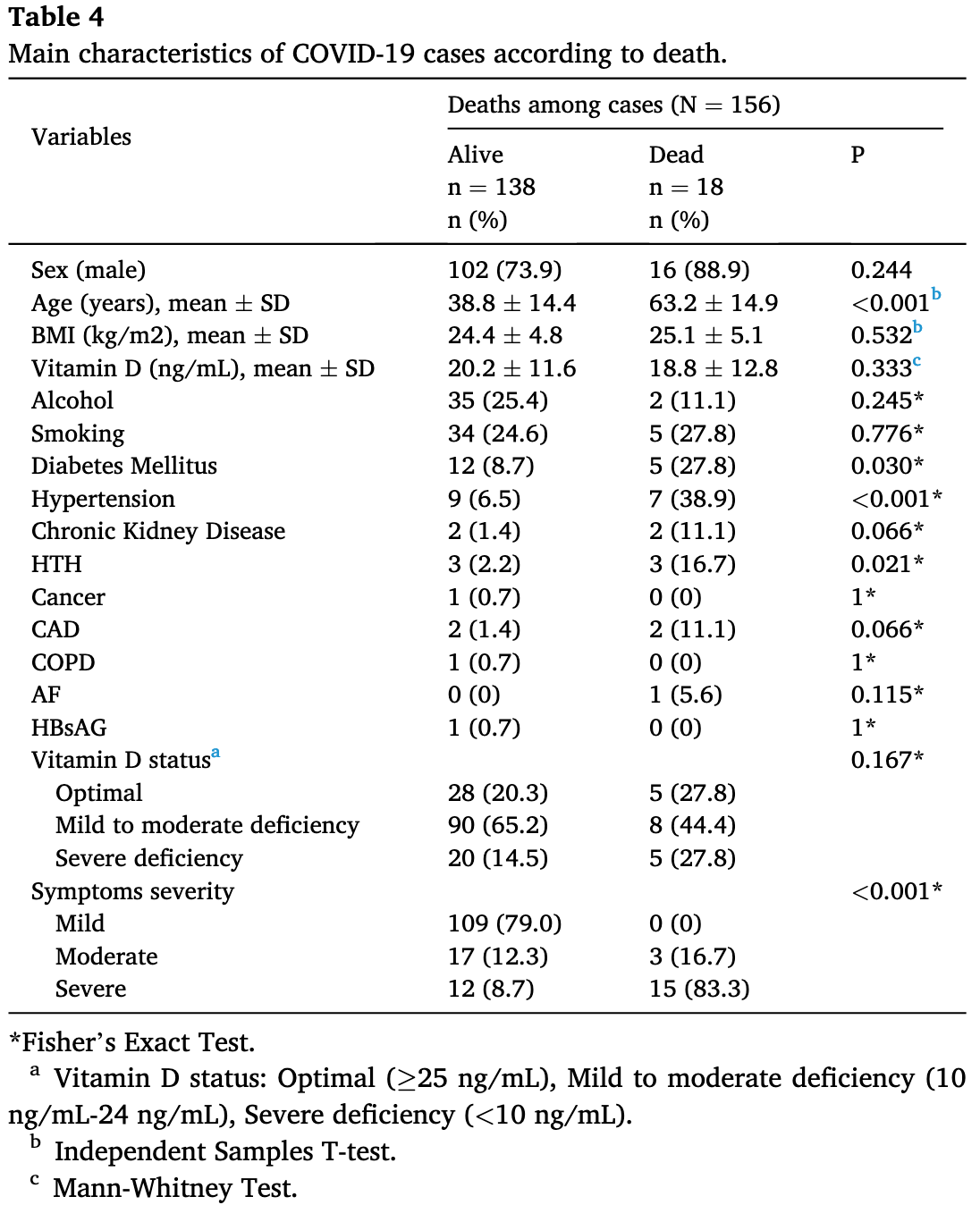
Case control study with 156 PCR+ cases in India and 204 controls, showing more frequent vitamin D deficiency in COVID-19 patients, and an association between lower vitamin D levels and COVID-19 severity.
This is the 83rd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of death, 50.4% lower, RR 0.50, p = 0.17, high D levels 13 of 131 (9.9%), low D levels 5 of 25 (20.0%), NNT 9.9, >10ng/mL, within cases.
|
|
risk of severe case, 67.6% lower, RR 0.32, p = 0.003, high D levels 17 of 131 (13.0%), low D levels 10 of 25 (40.0%), NNT 3.7, >10ng/mL, within cases.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Nimavat et al., 5 Aug 2021, retrospective, India, peer-reviewed, 5 authors.
Vitamin D deficiency and COVID-19: A case-control study at a tertiary care hospital in India
Annals of Medicine and Surgery, doi:10.1016/j.amsu.2021.102661
Background: As the pandemic COVID-19 affected developing and developed countries, there is no proven treatment options available yet. The anti-inflammatory, antiviral and immune modulator effect of Vitamin D could be beneficial to COVID-19. Aim: To find out the possible association between Vitamin D and COVID-19. Methods: The present case-control study was conducted at tertiary care hospital, AIIMS, Patna, Bihar, India. Total 156 cases and 204 controls were enrolled in the study after obtaining informed consent. Categorization of the patients were done based on clinical severity and level of Vitamin D. The association between these categories with different variables were analyzed using regression analysis and other statistical tests. Results: The status of Vitamin D (optimal, mild to moderate deficiency and severe deficiency) differed significantly among cases and controls. Diabetes and hypertension were most prevalent comorbidities among cases. On regression analysis, the difference in Vitamin D level was significant (aOR, 3.295; 95%CI,). The association between Vitamin D status and clinical severity group was statistically significant among cases. Among all variables, age, diabetes, hypertension and clinical severity were associated with worst outcome.
Conclusion: Vitamin D status appears to be strongly associated with COVID-19 clinical severity. After COVID-19 confirmation, Vitamin D level should be measured in all patients and curative plus preventive therapy should be initiated.
Author contribution All authors contributed significantly and in agreement with the content of the article. All authors were involved in project design, data collection, analysis, statistical analysis, data interpretation and writing the manuscript. All authors read and approved the final, submitted version.
Registration of research studies 1 Research Registry registration ID -researchregistry7001 Guarantor Shruti Singh.
Conflict of interest The authors declare that they have no conflict of interests.
Funding agency There was not any direct fund to carry out the research.
References
Agha, Abdall-Razak, Crossley, STROCSS 2019 Guideline: strengthening the reporting of cohort studies in surgery, Int. J. Surg, doi:10.1016/j.ijsu.2019.11.002
Arentz, Yim, Klaff, Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state, J. Am. Med. Assoc, doi:10.1001/jama.2020.4326
Bhatraju, Ghassemieh, Nichols, Covid-19 in critically ill patients in the seattle region -case series, N. Engl. J. Med, doi:10.1056/NEJMoa2004500
Bouillon, Marcocci, Carmeliet, Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions, Endocr. Rev, doi:10.1210/er.2018-00126
Cannell, Vieth, Umhau, Epidemic influenza and vitamin D, Epidemiol, Infect, doi:10.1017/S0950268806007175
Cannell, Vieth, Willett, Cod liver oil, vitamin A toxicity, frequent respiratory infections, and the vitamin D deficiency epidemic, Ann. Otol. Rhinol. Laryngol, doi:10.1177/000348940811701112
Carpagnano, Di Lecce, Quaranta, Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J. Endocrinol. Invest, doi:10.1007/s40618-020-01370-x
Clark, Mcdonagh, Mcmanus, Martin, COVID-19 and hypertension: risks and management. A scientific statement on behalf of the British and Irish Hypertension Society, J. Hum. Hypertens, doi:10.1038/s41371-020-00451-x
Dankers, Colin, Van Hamburg, Lubberts, Vitamin D in autoimmunity: molecular mechanisms and therapeutic potential, Front. Immunol, doi:10.3389/fimmu.2016.00697
Ginde, Mansbach, Camargo, Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the third national health and nutrition examination survey, Arch. Intern. Med, doi:10.1001/archinternmed.2008.560
Greiller, Martineau, Modulation of the immune response to respiratory viruses by vitamin D, Nutrients, doi:10.3390/nu7064240
Hoffmann, Kleine-Weber, Schroeder, SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01570-8
Infante, Ricordi, Sanchez, Influence of vitamin D on islet autoimmunity and beta-cell function in type 1 diabetes, Nutrients, doi:10.3390/nu11092185
Jakovac, COVID-19 and vitamin D-Is there a link and an opportunity for intervention?, Am. J. Physiol. Endocrinol. Metab, doi:10.1152/ajpendo.00138.2020
Khan, Chen, Geiger, Role of endolysosomes in severe acute respiratory syndrome coronavirus-2 infection and coronavirus disease 2019 pathogenesis: implications for potential treatments, Front. Pharmacol, doi:10.3389/fphar.2020.595888
Li, Zhang, Zhuo, The vasoprotective axes of the renin-angiotensin system: physiological relevance and therapeutic implications in cardiovascular, hypertensive and kidney diseases, Pharmacol. Res, doi:10.1016/j.phrs.2017.06.005
Lim, Bae, Kwon, Nauck, COVID-19 and diabetes mellitus: from pathophysiology to clinical management, Nat. Rev. Endocrinol, doi:10.1038/s41574-020-00435-4
Mahdavi, A brief review of interplay between vitamin D and angiotensinconverting enzyme 2: implications for a potential treatment for COVID-19, Rev. Med. Virol, doi:10.1002/rmv.2119
Mamani, Muceli, Ghasemi Basir, Vasheghani, Association between serum concentration of 25-hydroxyvitamin D and communityacquired pneumonia: a case-control study, Int. J. Gen. Med, doi:10.2147/IJGM.S149049
Martineau, Jolliffe, Greenberg, Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis, Health Technol. Assess, doi:10.3310/hta23020
Martineau, Jolliffe, Hooper, Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Mendy, Apewokin, Wells, Morrow, Factors associated with hospitalization and disease severity in a racially and ethnically diverse population of COVID-19 patients, MedRxiv Prepr. Serv. Heal. Sci, doi:10.1101/2020.06.25.20137323
Munshi, Hussein, Toraih, Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, J. Med. Virol, doi:10.1002/jmv.26360
Panagiotou, Tee, Ihsan, Low serum 25-hydroxyvitamin D (25[OH] D) levels in patients hospitalized with COVID-19 are associated with greater disease severity, Clin. Endocrinol, doi:10.1111/cen.14276
Pinzon, Pradana, Vitamin D deficiency among patients with COVID-19: case series and recent literature review, Trop. Med. Health, doi:10.1186/s41182-020-00277-w
Piroth, Cottenet, Mariet, Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30527-0
Rafiullah, Can a combination of AT1R antagonist and vitamin D treat the lung complication of COVID-19?, Am. J. Med. Sci, doi:10.1016/j.amjms.2020.07.018
Ricci, Pagliuca, D'ascanio, Circulating Vitamin D levels status and clinical prognostic indices in COVID-19 patients, Respir. Res, doi:10.1186/s12931-021-01666-3
Singh, Nimavat, Kumar, Singh, Ahmad et al., Prevalence of low level of vitamin D among COVID-19 patients and associated risk factors in India -a hospital-based study, Int. J. Gen. Med, doi:10.2147/IJGM.S309003
Talebi, Rasooli Nejad, Yaseri, Hadadi, Association of vitamin D status with the severity and mortality of community-acquired pneumonia in Iran during 2016-2017: a prospective cohort study, Reports Biochem. Mol. Biol
Tay, Poh, Rénia, Macary, Ng, The trinity of COVID-19: immunity, inflammation and intervention, Nat. Rev. Immunol, doi:10.1038/s41577-020-0311-8
Thacher, Clarke, Vitamin D insufficiency, Mayo Clin. Proc, doi:10.4065/mcp.2010.0567
Tramontana, Napoli, El-Hajj Fuleihan, Strollo, The D-side of COVID-19: musculoskeletal benefits of vitamin D and beyond, Endocrine, doi:10.1007/s12020-020-02407-0
Tsujino, Ushikoshi-Nakayama, Yamazaki, Matsumoto, Saito, Pulmonary activation of vitamin D3 and preventive effect against interstitial pneumonia, J. Clin. Biochem. Nutr, doi:10.3164/jcbn.19-48
Urashima, Segawa, Okazaki, Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren, Am. J. Clin. Nutr, doi:10.3945/ajcn.2009.29094
Vo, Koppel, Espinola, Vitamin D status at the time of hospitalization for bronchiolitis and its association with disease severity, J. Pediatr, doi:10.1016/j.jpeds.2018.07.097
Wan, Shang, Graham, Baric, Li, Receptor recognition by the novel coronavirus from wuhan: an analysis based on decade-long structural studies of SARS coronavirus, J. Virol, doi:10.1128/JVI.00127-20
Xiao, Li, Su, Mu, Qu, Could SARS-CoV-2-induced lung injury be attenuated by vitamin D?, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.10.059
Yang, Yu, Xu, Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30079-5
Ye, Tang, Liao, Does serum vitamin D level affect COVID-19 infection and its severity?-A case-control study, J. Am. Coll. Nutr, doi:10.1080/07315724.2020.1826005
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
DOI record:
{
"DOI": "10.1016/j.amsu.2021.102661",
"ISSN": [
"2049-0801"
],
"URL": "http://dx.doi.org/10.1016/j.amsu.2021.102661",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Vitamin D deficiency and COVID-19: A case-control study at a tertiary care hospital in India"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Annals of Medicine and Surgery"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.amsu.2021.102661"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 The Authors. Published by Elsevier Ltd on behalf of IJS Publishing Group Ltd."
}
],
"author": [
{
"affiliation": [],
"family": "Nimavat",
"given": "Nirav",
"sequence": "first"
},
{
"affiliation": [],
"family": "Singh",
"given": "Shruti",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Singh",
"given": "Pratibha",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Singh",
"given": "Sunil Kumar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sinha",
"given": "Nishi",
"sequence": "additional"
}
],
"container-title": "Annals of Medicine & Surgery",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.jp",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.fr",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
8,
5
]
],
"date-time": "2021-08-05T10:56:41Z",
"timestamp": 1628161001000
},
"deposited": {
"date-parts": [
[
2023,
3,
12
]
],
"date-time": "2023-03-12T23:05:24Z",
"timestamp": 1678662324000
},
"indexed": {
"date-parts": [
[
2024,
3,
28
]
],
"date-time": "2024-03-28T19:12:26Z",
"timestamp": 1711653146567
},
"is-referenced-by-count": 20,
"issued": {
"date-parts": [
[
2021,
8
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
8,
1
]
],
"date-time": "2021-08-01T00:00:00Z",
"timestamp": 1627776000000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 3,
"start": {
"date-parts": [
[
2021,
8,
4
]
],
"date-time": "2021-08-04T00:00:00Z",
"timestamp": 1628035200000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S2049080121006117?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S2049080121006117?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://journals.lww.com/10.1016/j.amsu.2021.102661",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "276",
"original-title": [],
"prefix": "10.1097",
"published": {
"date-parts": [
[
2021,
8
]
]
},
"published-print": {
"date-parts": [
[
2021,
8
]
]
},
"publisher": "Ovid Technologies (Wolters Kluwer Health)",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://journals.lww.com/10.1016/j.amsu.2021.102661"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine",
"Surgery"
],
"subtitle": [],
"title": "Vitamin D deficiency and COVID-19: A case-control study at a tertiary care hospital in India",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "68"
}
