Association Between the Use of Psychotropic Medications and the Risk of COVID-19 Infection Among Long-term Inpatients With Serious Mental Illness in a New York State–wide Psychiatric Hospital System
et al., JAMA Network Open, doi:10.1001/jamanetworkopen.2022.10743, May 2022
31st treatment shown to reduce risk in
November 2021, now with p = 0.00014 from 21 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 1,958 consecutive psychiatric patients in the USA, showing higher cases and lower mortality with fluvoxamine, without statistical significance. There was only 25 fluvoxamine patients.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 97.5% lower, RR 0.03, p = 1.00, treatment 0 of 16 (0.0%), control 38 of 953 (4.0%), NNT 25, relative risk is not 0 because of continuity correction due to zero events (with reciprocal of the contrasting arm).
|
|
risk of case, 29.8% higher, RR 1.30, p = 0.16, treatment 16 of 25 (64.0%), control 953 of 1,933 (49.3%).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Nemani et al., 6 May 2022, retrospective, USA, peer-reviewed, 12 authors, study period 8 March, 2020 - 1 July, 2020.
Association Between the Use of Psychotropic Medications and the Risk of COVID-19 Infection Among Long-term Inpatients With Serious Mental Illness in a New York State–wide Psychiatric Hospital System
JAMA Network Open, doi:10.1001/jamanetworkopen.2022.10743
IMPORTANCE Individuals with serious mental illness are at increased risk of severe COVID-19 infection. Several psychotropic medications have been identified as potential therapeutic agents to prevent or treat COVID-19 but have not been systematically examined in this population. OBJECTIVE To evaluate the associations between the use of psychotropic medications and the risk of COVID-19 infection among adults with serious mental illness receiving long-term inpatient psychiatric treatment. DESIGN, SETTING, AND PARTICIPANTS This retrospective cohort study assessed adults with serious mental illness hospitalized in a statewide psychiatric hospital system in New York between March 8 and July 1, 2020. The final date of follow-up was December 1, 2020. The study included 1958 consecutive adult inpatients with serious mental illness (affective or nonaffective psychoses) who received testing for SARS-CoV-2 by reverse transcriptase-polymerase chain reaction or antinucleocapsid antibodies and were continuously hospitalized from March 8 until medical discharge or July 1, 2020. EXPOSURES Psychotropic medications prescribed prior to COVID-19 testing. MAIN OUTCOMES AND MEASURES COVID-19 infection was the primary outcome, defined by a positive SARS-CoV-2 reverse transcriptase-polymerase chain reaction or antibody test result. The secondary outcome was COVID-19-related death among patients with laboratory-confirmed infection.
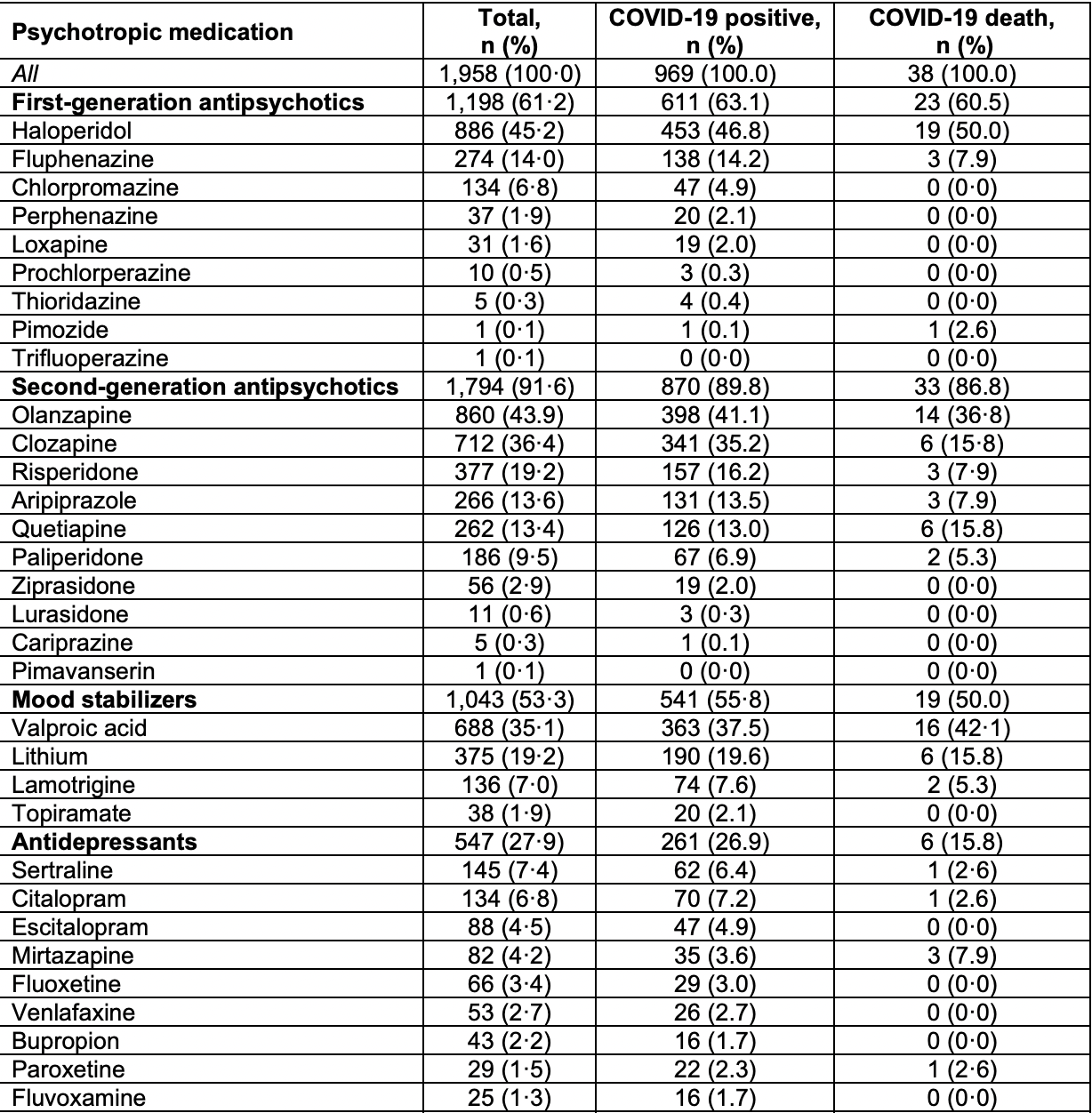
RESULTS Of the 2087 adult inpatients with serious mental illness continuously hospitalized during the study period, 1958 (93.8%) underwent testing and were included in the study; 1442 (73.6%) were men, and the mean (SD) age was 51.4 (14.3) years. A total of 969 patients (49.5%) had laboratory-confirmed COVID-19 infection that occurred while they were hospitalized; of those, 38 (3.9%) died. The use of second-generation antipsychotic medications, as a class, was associated with decreased odds of infection (odds ratio [OR], 0.62; 95% CI, 0.45-0.86), whereas the use of mood stabilizers was associated with increased odds of infection (OR, 1.23; 95% CI, 1.03-1.47). In a multivariable model of individual medications, the use of paliperidone was associated with decreased odds of infection (OR, 0.59; 95% CI, 0.41-0.84), and the use of valproic acid was associated with increased odds of infection (OR, 1.39; 95% CI, 1.10-1.76). Clozapine use was associated with reduced odds of mortality in unadjusted analyses (unadjusted OR, 0.25; 95% CI, 0.10-0.62; fully adjusted OR, 0.43; 95% CI, 0.17-1.12). (continued) Key Points Question Is psychotropic medication use associated with differences in the risk of COVID-19 infection among adults with serious mental illness? Findings In this cohort study of 1958 inpatients with serious mental illness in a statewide psychiatric hospital system, the use of second-generation antipsychotic medications was associated with a decreased risk of COVID-19 infection; the largest association was observed with the use of..
Author Contributions: Drs Nemani and Goff had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Nemani, Williams, Olfson, Finnerty, Clelland, Goff. Acquisition, analysis, or interpretation of data: Nemani, Williams, Leckman-Westin, Finnerty, Kammer, Smith, Silverman, Lindenmayer, Capichioni, Goff. Drafting of the manuscript: Nemani, Williams, Capichioni, Goff. Critical revision of the manuscript for important intellectual content: Nemani, Williams, Olfson, Leckman-Westin, Finnerty, Kammer, Smith, Silverman, Lindenmayer, Clelland, Goff.
Statistical analysis: Williams. Administrative, technical, or material support: Finnerty, Smith, Silverman, Lindenmayer, Capichioni, Goff. Supervision: Leckman-Westin, Finnerty, Smith, Goff.
Conflict of Interest Disclosures: Dr Lindenmayer reported receiving grants from Roche, Takeda, Lundbeck, Avanir, GW/Jazz, Neurocrine, and the National Institute of Mental Health outside the submitted work; and having a patent for the Structured Clinical Interview for the Positive and Negative Syndrome Scale (SCI-PANSS) with royalties paid. No other disclosures were reported.
References
Dotson, Hartvigsen, Wesner, Carbary, Fricchione et al., Clozapine toxicity in the setting of COVID-19, Psychosomatics, doi:10.1016/j.psym.2020.05.025
Druss, Addressing the COVID-19 pandemic in populations with serious mental illness, JAMA Psychiatry, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamapsychiatry.2020.0894&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2022.10743
Fond, Nemani, Etchecopar-Etchart, Association between mental health disorders and mortality among patients with COVID-19 in 7 countries: a systematic review and meta-analysis, JAMA Psychiatry, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamapsychiatry.2021.2274&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2022.10743
Gordon, Hiatt, Bouhaddou, Comparative host-coronavirus protein interaction networks reveal pan-viral disease mechanisms, Science, doi:10.1126/science.abe9403
Govind, Fonseca De Freitas, Pritchard, Hayes, Maccabe, Clozapine treatment and risk of COVID-19 infection: retrospective cohort, Br J Psychiatry, doi:10.1192/bjp.2020.151
Gul, Ozcan, Asar, Okyar, Barıs et al., In silico identification of widely used and well-tolerated drugs as potential SARS-CoV-2 3C-like protease and viral RNA-dependent RNA polymerase inhibitors for direct use in clinical trials, J Biomol Struct Dyn, doi:10.1080/07391102.2020.1802346
Hoertel, Sánchez-Rico, Gulbins, Entrepôt de Données de Santé" AP-HP Consortium. Association between FIASMAs and reduced risk of intubation or death in individuals hospitalized for severe COVID-19: an observational multicenter study, Clin Pharmacol Ther, doi:10.1002/cpt.2317
Hoertel, Sánchez-Rico, Vernet, /Universities/INSERM COVID-19 research collaboration and AP-HP COVID CDR Initiative. Observational study of haloperidol in hospitalized patients with COVID-19, PLoS One, doi:10.1371/journal.pone.0247122
Hoertel, Sánchez-Rico, Vernet, AP-HP/Universities/INSERM COVID-19 Research Collaboration and AP-HP COVID CDR Initiative. Observational study of chlorpromazine in hospitalized patients with COVID-19, Clin Drug Investig, doi:10.1007/s40261-021-01001-0
Hoertel, Sánchez-Rico, Vernet, Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study, Mol Psychiatry, doi:10.1038/s41380-021-01021-4
Hosmer, Lemeshow, Sturdivant, Applied Logistic Regression
Kennedy, Richeson, Houde, Psychiatry Association Between Psychotropic Medication Use and COVID-19 Risk, N Engl J Med, doi:10.1056/NEJMc2029354
Li, Li, Fortunati, Krystal, Association of a prior psychiatric diagnosis with mortality among hospitalized patients with coronavirus disease 2019 (COVID-19) infection, JAMA Netw Open, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamanetworkopen.2020.23282&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2022.10743
Maine, Lao, Krishnan, Longitudinal characterization of the IgM and IgG humoral response in symptomatic COVID-19 patients using the Abbott Architect, J Clin Virol, doi:10.1016/j.jcv.2020.104663
Mcmichael, Currie, Clark, Public Health-Seattle and King County, EvergreenHealth, and CDC COVID-19 Investigation Team. Epidemiology of Covid-19 in a long-term care facility in King County, Washington, N Engl J Med, doi:10.1056/NEJMoa2005412
Nemani, Conderino, Marx, Thorpe, Goff, Association between antipsychotic use and COVID-19 mortality among people with serious mental illness, JAMA Psychiatry, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamapsychiatry.2021.2503&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2022.10743
Nemani, Li, Olfson, Association of psychiatric disorders with mortality among patients with COVID-19, JAMA Psychiatry, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamapsychiatry.2020.4442&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2022.10743
Okusaga, Mitchell, Bernard, Walder, Clozapine is associated with higher COVID-19 infection rate in veterans with schizophrenia or schizoaffective disorder, J Clin Psychiatry
Oskotsky, Maric, Tang, Mortality risk among patients with COVID-19 prescribed selective serotonin reuptake inhibitor antidepressants, JAMA Netw Open, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamanetworkopen.2021.33090&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2022.10743
Pandurangi, Buckley, Inflammation, antipsychotic drugs, and evidence for effectiveness of antiinflammatory agents in schizophrenia, Curr Top Behav Neurosci, doi:10.1007/7854_2019_91
Pitt, Sutton, Wang, Goonewardena, Holinstat, Potential repurposing of the HDAC inhibitor valproic acid for patients with COVID-19, Eur J Pharmacol, doi:10.1016/j.ejphar.2021.173988
Plaze, Attali, Petit, Repurposing chlorpromazine to treat COVID-19: the reCoVery study, Encephale, doi:10.1016/j.encep.2020.05.006
Prokopez, Farinola, Vallejos, Olanzapine, risperidone and quetiapine: do these atypical antipsychotics have a protective effect for SARS-CoV-2?, Schizophr Res, doi:10.1016/j.schres.2022.01.035
Prokopez, Vallejos, Lopredo, An analysis of the possible protective effect of antipsychotics for SARS-CoV-2 in patients under treatment for severe mental illnesses, Schizophr Res, doi:10.1016/j.schres.2021.06.019
Reis, Santos Moreira-Silva, Silva, Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial, Lancet Glob Health, doi:10.1016/S2214-109X(21)00448-4
Singh, Singh, Valproic acid in prevention and treatment of COVID-19, Int J Respir Pulm Med, doi:10.23937/2378-3516/1410138
Smith, Rodgers, Silverman, COVID-19 case rates after surveillance and vaccinations in a statewide psychiatric hospital system, Am J Public Health, doi:10.2105/AJPH.2021.306444
Stip, Arnone, Aziz, Javaid, Diversity of mechanism of action of psychotropic drugs in their anti-COVID-19 properties, Mol Psychiatry, doi:10.1038/s41380-021-01222-x
Sukhatme, Reiersen, Vayttaden, Sukhatme, Fluvoxamine: a review of its mechanism of action and its role in COVID-19, Front Pharmacol, doi:10.3389/fphar.2021.652688
Supplement, Efigure, Study Profile eTable 1. Psychotropic Medications Exposure in Full Cohort and by Infection and Death eTable 2. ICD-9/10 Category Codes Used to Identify Medical Conditions and Psychiatric Diagnoses eTable 3. Incidence and Adjusted Odds Ratios of COVID-19 Infection by Psychotropic Medication Exposure in Patients with PCR Testing
Teixeira, Krause, Ghosh, Analysis of COVID-19 infection and mortality among patients with psychiatric disorders, JAMA Netw Open, doi:https://jama.jamanetwork.com/article.aspx?doi=10.1001/jamanetworkopen.2021.34969&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamanetworkopen.2022.10743
Tzur Bitan, Krieger, Kridin, COVID-19 prevalence and mortality among schizophrenia patients: a largescale retrospective cohort study, Schizophr Bull, doi:10.1093/schbul/sbab012
Vai, Mazza, Colli, Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis, Lancet Psychiatry, doi:10.1016/S2215-0366(21)00232-7
Vieira, Nery, Martins, Jabour, Dias et al., Downregulation of membrane-bound angiotensin converting enzyme 2 (ACE2) receptor has a pivotal role in COVID-19 immunopathology, Curr Drug Targets, doi:10.2174/1389450121666201020154033
Wang, Xu, Volkow, Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States, World Psychiatry, doi:10.1002/wps.20806
Yang, Kandula, Huynh, Estimating the infection-fatality risk of SARS-CoV-2 in New York City during the spring 2020 pandemic wave: a model-based analysis, Lancet Infect Dis, doi:10.1016/S1473-3099(20)30769-6
DOI record:
{
"DOI": "10.1001/jamanetworkopen.2022.10743",
"ISSN": [
"2574-3805"
],
"URL": "http://dx.doi.org/10.1001/jamanetworkopen.2022.10743",
"author": [
{
"affiliation": [
{
"name": "Nathan S. Kline Institute for Psychiatric Research, Orangeburg, New York"
},
{
"name": "Department of Psychiatry, New York University Langone Medical Center, New York"
}
],
"family": "Nemani",
"given": "Katlyn",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Nathan S. Kline Institute for Psychiatric Research, Orangeburg, New York"
}
],
"family": "Williams",
"given": "Sharifa Z.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Psychiatry, Columbia University Irving Medical Center, New York, New York"
}
],
"family": "Olfson",
"given": "Mark",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "New York State Office of Mental Health, New York"
}
],
"family": "Leckman-Westin",
"given": "Emily",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "New York State Office of Mental Health, New York"
}
],
"family": "Finnerty",
"given": "Molly",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "New York State Office of Mental Health, New York"
}
],
"family": "Kammer",
"given": "Jammie",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "New York State Office of Mental Health, New York"
}
],
"family": "Smith",
"given": "Thomas E.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "New York State Office of Mental Health, New York"
}
],
"family": "Silverman",
"given": "Daniel J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Nathan S. Kline Institute for Psychiatric Research, Orangeburg, New York"
},
{
"name": "Department of Psychiatry, New York University Langone Medical Center, New York"
}
],
"family": "Lindenmayer",
"given": "Jean-Pierre",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Psychiatry, New York University Langone Medical Center, New York"
}
],
"family": "Capichioni",
"given": "Gillian",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Nathan S. Kline Institute for Psychiatric Research, Orangeburg, New York"
}
],
"family": "Clelland",
"given": "James",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Nathan S. Kline Institute for Psychiatric Research, Orangeburg, New York"
},
{
"name": "Department of Psychiatry, New York University Langone Medical Center, New York"
}
],
"family": "Goff",
"given": "Donald C.",
"sequence": "additional"
}
],
"container-title": "JAMA Network Open",
"container-title-short": "JAMA Netw Open",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
5,
6
]
],
"date-time": "2022-05-06T15:33:36Z",
"timestamp": 1651851216000
},
"deposited": {
"date-parts": [
[
2022,
5,
6
]
],
"date-time": "2022-05-06T15:33:40Z",
"timestamp": 1651851220000
},
"indexed": {
"date-parts": [
[
2022,
6,
3
]
],
"date-time": "2022-06-03T13:32:32Z",
"timestamp": 1654263152211
},
"is-referenced-by-count": 1,
"issue": "5",
"issued": {
"date-parts": [
[
2022,
5,
6
]
]
},
"journal-issue": {
"issue": "5",
"published-print": {
"date-parts": [
[
2022,
5,
2
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://jamanetwork.com/journals/jamanetworkopen/articlepdf/2791969/nemani_2022_oi_220321_1651174051.2345.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "10",
"original-title": [],
"page": "e2210743",
"prefix": "10.1001",
"published": {
"date-parts": [
[
2022,
5,
6
]
]
},
"published-online": {
"date-parts": [
[
2022,
5,
6
]
]
},
"publisher": "American Medical Association (AMA)",
"reference": [
{
"DOI": "10.1016/S2215-0366(21)00232-7",
"article-title": "Mental disorders and risk of COVID-19–related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis.",
"author": "Vai",
"doi-asserted-by": "publisher",
"first-page": "797",
"issue": "9",
"journal-title": "Lancet Psychiatry",
"key": "zoi220321r1",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2020.23282",
"article-title": "Association of a prior psychiatric diagnosis with mortality among hospitalized patients with coronavirus disease 2019 (COVID-19) infection.",
"author": "Li",
"doi-asserted-by": "publisher",
"issue": "9",
"journal-title": "JAMA Netw Open",
"key": "zoi220321r2",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1001/jamanetworkopen.2021.34969",
"article-title": "Analysis of COVID-19 infection and mortality among patients with psychiatric disorders, 2020.",
"author": "Teixeira",
"doi-asserted-by": "publisher",
"issue": "11",
"journal-title": "JAMA Netw Open",
"key": "zoi220321r3",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1002/wps.v20.1",
"article-title": "Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States.",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "124",
"issue": "1",
"journal-title": "World Psychiatry",
"key": "zoi220321r4",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1001/jamapsychiatry.2021.2274",
"article-title": "Association between mental health disorders and mortality among patients with COVID-19 in 7 countries: a systematic review and meta-analysis.",
"author": "Fond",
"doi-asserted-by": "publisher",
"first-page": "1208",
"issue": "11",
"journal-title": "JAMA Psychiatry",
"key": "zoi220321r5",
"volume": "78",
"year": "2021"
},
{
"DOI": "10.1001/jamapsychiatry.2020.4442",
"article-title": "Association of psychiatric disorders with mortality among patients with COVID-19.",
"author": "Nemani",
"doi-asserted-by": "publisher",
"first-page": "380",
"issue": "4",
"journal-title": "JAMA Psychiatry",
"key": "zoi220321r6",
"volume": "78",
"year": "2021"
},
{
"DOI": "10.1093/schbul/sbab012",
"article-title": "COVID-19 prevalence and mortality among schizophrenia patients: a large-scale retrospective cohort study.",
"author": "Tzur Bitan",
"doi-asserted-by": "publisher",
"first-page": "1211",
"issue": "5",
"journal-title": "Schizophr Bull",
"key": "zoi220321r7",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1001/jamapsychiatry.2020.0894",
"article-title": "Addressing the COVID-19 pandemic in populations with serious mental illness.",
"author": "Druss",
"doi-asserted-by": "publisher",
"first-page": "891",
"issue": "9",
"journal-title": "JAMA Psychiatry",
"key": "zoi220321r8",
"volume": "77",
"year": "2020"
},
{
"DOI": "10.1001/jamapsychiatry.2021.2503",
"article-title": "Association between antipsychotic use and COVID-19 mortality among people with serious mental illness.",
"author": "Nemani",
"doi-asserted-by": "publisher",
"first-page": "1391",
"issue": "12",
"journal-title": "JAMA Psychiatry",
"key": "zoi220321r9",
"volume": "78",
"year": "2021"
},
{
"DOI": "10.1126/science.abe9403",
"author": "Gordon",
"doi-asserted-by": "publisher",
"journal-title": "Science",
"key": "zoi220321r10",
"year": "2020"
},
{
"DOI": "10.1016/j.encep.2020.05.006",
"article-title": "Repurposing chlorpromazine to treat COVID-19: the reCoVery study.",
"author": "Plaze",
"doi-asserted-by": "publisher",
"first-page": "169",
"issue": "3",
"journal-title": "Encephale",
"key": "zoi220321r11",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.3389/fphar.2021.652688",
"article-title": "Fluvoxamine: a review of its mechanism of action and its role in COVID-19.",
"author": "Sukhatme",
"doi-asserted-by": "publisher",
"journal-title": "Front Pharmacol",
"key": "zoi220321r12",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/S2214-109X(21)00448-4",
"article-title": "Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial.",
"author": "Reis",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Glob Health",
"key": "zoi220321r13",
"year": "2022"
},
{
"DOI": "10.1001/jamanetworkopen.2021.33090",
"article-title": "Mortality risk among patients with COVID-19 prescribed selective serotonin reuptake inhibitor antidepressants.",
"author": "Oskotsky",
"doi-asserted-by": "publisher",
"issue": "11",
"journal-title": "JAMA Netw Open",
"key": "zoi220321r14",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1038/s41380-021-01021-4",
"article-title": "Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study.",
"author": "Hoertel",
"doi-asserted-by": "publisher",
"first-page": "5199",
"issue": "9",
"journal-title": "Mol Psychiatry",
"key": "zoi220321r15",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0247122",
"article-title": "Observational study of haloperidol in hospitalized patients with COVID-19.",
"author": "Hoertel",
"doi-asserted-by": "publisher",
"issue": "2",
"journal-title": "PLoS One",
"key": "zoi220321r16",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1007/s40261-021-01001-0",
"article-title": "Observational study of chlorpromazine in hospitalized patients with COVID-19.",
"author": "Hoertel",
"doi-asserted-by": "publisher",
"first-page": "221",
"issue": "3",
"journal-title": "Clin Drug Investig",
"key": "zoi220321r17",
"volume": "41",
"year": "2021"
},
{
"DOI": "10.1016/j.schres.2022.01.035",
"article-title": "Olanzapine, risperidone and quetiapine: do these atypical antipsychotics have a protective effect for SARS-CoV-2?",
"author": "Prokopez",
"doi-asserted-by": "publisher",
"first-page": "140",
"journal-title": "Schizophr Res",
"key": "zoi220321r18",
"volume": "241",
"year": "2022"
},
{
"DOI": "10.1038/s41380-021-01222-x",
"article-title": "Diversity of mechanism of action of psychotropic drugs in their anti-COVID-19 properties.",
"author": "Stip",
"doi-asserted-by": "publisher",
"first-page": "7093",
"issue": "12",
"journal-title": "Mol Psychiatry",
"key": "zoi220321r19",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1016/j.jcv.2020.104663",
"article-title": "Longitudinal characterization of the IgM and IgG humoral response in symptomatic COVID-19 patients using the Abbott Architect.",
"author": "Maine",
"doi-asserted-by": "publisher",
"journal-title": "J Clin Virol",
"key": "zoi220321r21",
"volume": "133",
"year": "2020"
},
{
"DOI": "10.1016/S1473-3099(20)30769-6",
"article-title": "Estimating the infection-fatality risk of SARS-CoV-2 in New York City during the spring 2020 pandemic wave: a model-based analysis.",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "203",
"issue": "2",
"journal-title": "Lancet Infect Dis",
"key": "zoi220321r23",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1056/NEJMc2029354",
"article-title": "Risk factors for SARS-CoV-2 in a statewide correctional system.",
"author": "Kennedy",
"doi-asserted-by": "publisher",
"first-page": "2479",
"issue": "25",
"journal-title": "N Engl J Med",
"key": "zoi220321r24",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2005412",
"article-title": "Epidemiology of Covid-19 in a long-term care facility in King County, Washington.",
"author": "McMichael",
"doi-asserted-by": "publisher",
"first-page": "2005",
"issue": "21",
"journal-title": "N Engl J Med",
"key": "zoi220321r25",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1080/07391102.2020.1802346",
"article-title": "In silico identification of widely used and well-tolerated drugs as potential SARS-CoV-2 3C-like protease and viral RNA-dependent RNA polymerase inhibitors for direct use in clinical trials.",
"author": "Gul",
"doi-asserted-by": "publisher",
"first-page": "6772",
"issue": "17",
"journal-title": "J Biomol Struct Dyn",
"key": "zoi220321r26",
"volume": "39",
"year": "2021"
},
{
"DOI": "10.1016/j.psym.2020.05.025",
"article-title": "Clozapine toxicity in the setting of COVID-19.",
"author": "Dotson",
"doi-asserted-by": "publisher",
"first-page": "577",
"issue": "5",
"journal-title": "Psychosomatics",
"key": "zoi220321r27",
"volume": "61",
"year": "2020"
},
{
"DOI": "10.1192/bjp.2020.151",
"article-title": "Clozapine treatment and risk of COVID-19 infection: retrospective cohort study.",
"author": "Govind",
"doi-asserted-by": "publisher",
"first-page": "368",
"issue": "1",
"journal-title": "Br J Psychiatry",
"key": "zoi220321r28",
"volume": "219",
"year": "2021"
},
{
"author": "Okusaga",
"journal-title": "J Clin Psychiatry",
"key": "zoi220321r29",
"year": "2021"
},
{
"DOI": "10.1016/j.schres.2021.06.019",
"article-title": "An analysis of the possible protective effect of antipsychotics for SARS-CoV-2 in patients under treatment for severe mental illnesses.",
"author": "Prokopez",
"doi-asserted-by": "publisher",
"first-page": "99",
"journal-title": "Schizophr Res",
"key": "zoi220321r30",
"volume": "233",
"year": "2021"
},
{
"DOI": "10.1007/978-3-030-39141-6",
"article-title": "Inflammation, antipsychotic drugs, and evidence for effectiveness of anti-inflammatory agents in schizophrenia.",
"author": "Pandurangi",
"doi-asserted-by": "publisher",
"first-page": "227",
"journal-title": "Curr Top Behav Neurosci",
"key": "zoi220321r31",
"volume": "44",
"year": "2020"
},
{
"DOI": "10.1016/j.ejphar.2021.173988",
"article-title": "Potential repurposing of the HDAC inhibitor valproic acid for patients with COVID-19.",
"author": "Pitt",
"doi-asserted-by": "publisher",
"journal-title": "Eur J Pharmacol",
"key": "zoi220321r32",
"volume": "898",
"year": "2021"
},
{
"DOI": "10.23937/2378-3516",
"article-title": "Valproic acid in prevention and treatment of COVID-19.",
"author": "Singh",
"doi-asserted-by": "publisher",
"first-page": "138",
"journal-title": "Int J Respir Pulm Med",
"key": "zoi220321r33",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.2174/1389450121666201020154033",
"article-title": "Downregulation of membrane-bound angiotensin converting enzyme 2 (ACE2) receptor has a pivotal role in COVID-19 immunopathology.",
"author": "Vieira",
"doi-asserted-by": "publisher",
"first-page": "254",
"issue": "3",
"journal-title": "Curr Drug Targets",
"key": "zoi220321r34",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1002/cpt.v110.6",
"article-title": "Association between FIASMAs and reduced risk of intubation or death in individuals hospitalized for severe COVID-19: an observational multicenter study.",
"author": "Hoertel",
"doi-asserted-by": "publisher",
"first-page": "1498",
"issue": "6",
"journal-title": "Clin Pharmacol Ther",
"key": "zoi220321r35",
"volume": "110",
"year": "2021"
},
{
"DOI": "10.2105/AJPH.2021.306444",
"article-title": "COVID-19 case rates after surveillance and vaccinations in a statewide psychiatric hospital system.",
"author": "Smith",
"doi-asserted-by": "publisher",
"first-page": "1780",
"issue": "10",
"journal-title": "Am J Public Health",
"key": "zoi220321r36",
"volume": "111",
"year": "2021"
},
{
"DOI": "10.1002/9781118548387",
"author": "Hosmer",
"doi-asserted-by": "crossref",
"edition": "3rd ed",
"key": "zoi220321r22",
"volume-title": "Applied Logistic Regression",
"year": "2013"
},
{
"key": "zoi220321r20",
"unstructured": "US Food and Drug Administration. EUA authorized serology test performance. Accessed October 3, 2021. https://www.fda.gov/medical-devices/coronavirus-disease-2019-covid-19-emergency-use-authorizations-medical-devices/eua-authorized-serology-test-performance"
}
],
"reference-count": 36,
"references-count": 36,
"relation": {},
"resource": {
"primary": {
"URL": "https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2791969"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Association Between the Use of Psychotropic Medications and the Risk of COVID-19 Infection Among Long-term Inpatients With Serious Mental Illness in a New York State–wide Psychiatric Hospital System",
"type": "journal-article",
"volume": "5"
}
