Minerals and Antioxidant Micronutrients Levels and Clinical Outcome in Older Patients Hospitalized for COVID-19 during the First Wave of the Pandemic
et al., Nutrients, doi:10.3390/nu15061516, Mar 2023
Retrospective 235 hospitalized COVID-19 patients in France, showing higher mortality with lower selenium levels, without statistical significance. Results are provided for selenium levels as a continuous value.
|
risk of death, 33.6% lower, OR 0.66, p = 0.14, adjusted per study, inverted to make OR<1 favor high selenium levels, per 10 unit change, multivariable, RR approximated with OR, per 10 units.
|
|
risk of severe case, 13.6% lower, OR 0.86, p = 0.51, adjusted per study, inverted to make OR<1 favor high selenium levels, per 10 unit change, multivariable, RR approximated with OR, per 10 units.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Lahaye et al., 21 Mar 2023, retrospective, France, peer-reviewed, 13 authors.
Minerals and Antioxidant Micronutrients Levels and Clinical Outcome in Older Patients Hospitalized for COVID-19 during the First Wave of the Pandemic
Nutrients, doi:10.3390/nu15061516
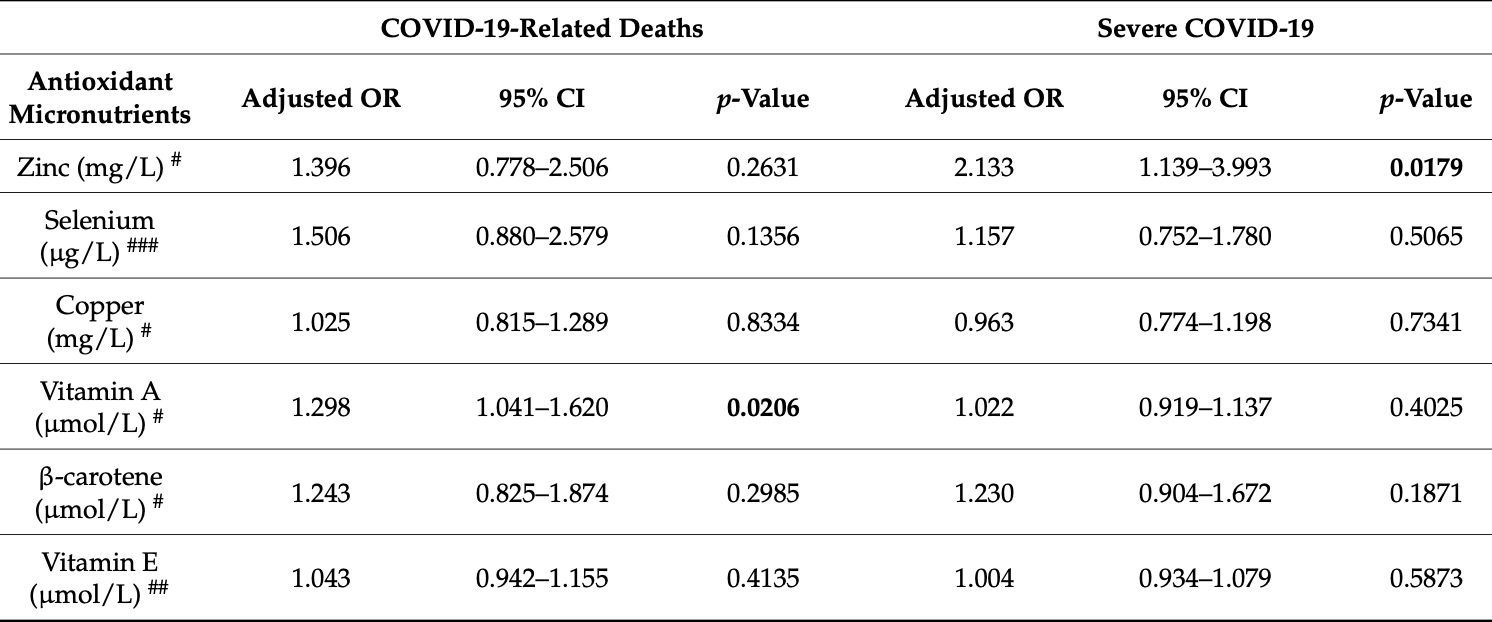
Excessive inflammatory response has been implicated in severe respiratory forms of coronavirus disease 2019 . Trace elements such as zinc, selenium, and copper are known to modulate inflammation and immunity. This study aimed to assess the relationships between antioxidant vitamins and mineral trace elements levels as well as COVID-19 severity in older adults hospitalized. In this observational retrospective cohort study, the levels of zinc, selenium, copper, vitamin A, β-carotene, and vitamin E were measured in 94 patients within the first 15 days of hospitalization. The outcomes were in-hospital mortality secondary to COVID-19 or severe COVID-19. A logistic regression analysis was conducted to test whether the levels of vitamins and minerals were independently associated with severity. In this cohort (average age of 78 years), severe forms (46%) were associated with lower zinc (p = 0.012) and β-carotene (p < 0.001) concentrations, and in-hospital mortality (15%) was associated with lower zinc (p = 0.009), selenium (p = 0.014), vitamin A (p = 0.001), and β-carotene (p = 0.002) concentrations. In regression analysis, severe forms remained independently associated with lower zinc (aOR 2.13, p = 0.018) concentrations, and death was associated with lower vitamin A (aOR = 0.165, p = 0.021) concentrations. Low plasma concentrations of zinc and vitamin A were associated with poor prognosis in older people hospitalized with COVID-19.
Supplementary Materials: The following supporting information can be downloaded at: https:// www.mdpi.com/article/10.3390/nu15061516/s1, Table S1 : Logistic regression analysis of association between the 41 severe COVID-19 and serum antioxidant micronutrients levels. Funding: This research received financial support from the Hospices Civils de Lyon (Lyon, France) within the framework of the Clinical Biology Department Call for Proposal (grant number NCT04877509) and the APC was funded by Hospices Civils de Lyon (Lyon, France).
Author
Institutional Review Board Statement: The study was conducted in accordance with the Declaration of Helsinki and approved by the ethical committee of the Hospices Civils de Lyon (protocol code 21_5067, the 30 December 2021). Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Data Availability Statement: The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical considerations, regarding personal information and respecting what was written in the generic information sheet dedicated to COVID-19 research at the Hospices Civils de Lyon (Lyon, France).
Conflicts of Interest: The authors declare no conflict of interest.
References
Akbaraly, Arnaud, Hininger-Favier, Gourlet, Roussel et al., Selenium and Mortality in the Elderly: Results from the EVA Study, Clin. Chem, doi:10.1373/clinchem.2005.055301
Bajaj, Gadi, Spihlman, Wu, Choi et al., Immunity, and COVID-19: How Age Influences the Host Immune Response to Coronavirus Infections?, Front. Physiol, doi:10.3389/fphys.2020.571416
Baudry, Kopp, Boeing, Kipp, Schwerdtle et al., Changes of Trace Element Status during Aging: Results of the EPIC-Potsdam Cohort Study, Eur. J. Nutr, doi:10.1007/s00394-019-02143-w
Beran, Mhanna, Srour, Ayesh, Stewart et al., Clinical Significance of Micronutrient Supplements in Patients with Coronavirus Disease 2019: A Comprehensive Systematic Review and Meta-Analysis, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2021.12.033
Calder, Carr, Gombart, Eggersdorfer, Optimal Nutritional Status for a Well-Functioning Immune System is an Important Factor to Protect against Viral Infections, Nutrients, doi:10.3390/nu12041181
Casaer, Bellomo, Micronutrient Deficiency in Critical Illness: An Invisible Foe?, Intensive Care Med
Chan, Cheng, Martin, Impact of COVID-19 on Excess Mortality, Life Expectancy, and Years of Life Lost in the United States, PLoS ONE, doi:10.1371/journal.pone.0256835
Cortes-Telles, Gutiérrez-Solis, Álvarez-Sánchez, González-Garay, Lugo et al., Dynamic Inflammatory Response among Routine Laboratory Biomarkers and Their Predictive Ability for Mortality in Patients with Severe COVID-19, Front. Med, doi:10.3389/fmed.2022.1047304
Culbertson, Culotta, Copper in Infectious Disease: Using Both Sides of the Penny, Semin. Cell Dev. Biol, doi:10.1016/j.semcdb.2020.12.003
Damayanthi, Prabani, Nutritional Determinants and COVID-19 Outcomes of Older Patients with COVID-19: A Systematic Review, Arch. Gerontol. Geriatr, doi:10.1016/j.archger.2021.104411
De Faria Coelho-Ravagnani, Corgosinho, Sanches, Prado, Laviano et al., Dietary Recommendations during the COVID-19 Pandemic, Nutr. Rev, doi:10.1093/nutrit/nuaa067
Demetriou, Achilleos, Quattrocchi, Gabel, Critselis et al., Impact of the COVID-19 Pandemic on Total, Sex-and Age-Specific All-Cause Mortality in 20 Countries Worldwide during 2020: Results from the C-MOR Project, Int. J. Epidemiol, doi:10.1093/ije/dyac170
Dessie, Zewotir, Mortality-Related Risk Factors of COVID-19: A Systematic Review and Meta-Analysis of 42 Studies and 423,117 Patients, BMC Infect. Dis, doi:10.1186/s12879-021-06536-3
El Sabbagh, El-Sayed, Elbaz, Vitamins and Minerals: A Means for Surviving the COVID-19 Pandemic or Just a Myth?, J. Infect. Dev. Ctries, doi:10.3855/jidc.14692
Elham, Azam, Azam, Mostafa, Nasrin et al., Serum Vitamin D, Calcium, and Zinc Levels in Patients with COVID-19, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2021.03.040
Fischer Walker, Black, Zinc and the Risk for Infectious Disease, Annu. Rev. Nutr, doi:10.1146/annurev.nutr.23.011702.073054
Fitero, Bungau, Tit, Endres, Khan et al., Associated Diseases, and Risk Assessment in COVID-19-A Systematic Review, Int. J. Clin. Pract, doi:10.1155/2022/1571826
Gombart, Pierre, Maggini, A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection, Nutrients, doi:10.3390/nu12010236
Heller, Sun, Hackler, Seelig, Seibert et al., Prediction of Survival Odds in COVID-19 by Zinc, Age and Selenoprotein P as Composite Biomarker, Redox Biol
Homem, Moreira, Da Silva, Barni, Da Rosa et al., Relationship between Oropharyngeal Dysphagia, Nutritional Status, Antioxidant Vitamins and the Inflammatory Response in Adults and Elderly: A Cross-Sectional Study, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2020.04.011
Huang, Liu, Qi, Brand, Zheng, Role of Vitamin A in the Immune System, J. Clin. Med, doi:10.3390/jcm7090258
Im, Je, Baek, Chung, Kwon et al., Nutritional Status of Patients with COVID-19, Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis, doi:10.1016/j.ijid.2020.08.018
Kabir, Uddin, Hossain, Abdulhakim, Alam et al., NCOVID-19 Pandemic: From Molecular Pathogenesis to Potential Investigational Therapeutics, Front. Cell Dev. Biol, doi:10.3389/fcell.2020.00616
Katona, Katona-Apte, The Interaction between Nutrition and Infection, Clin. Infect. Dis, doi:10.1086/587658
Kaur, Behl, Sehgal, Singh, Sharma et al., A Motley of Possible Therapies of the COVID-19: Reminiscing the Origin of the Pandemic, Environ. Sci. Pollut. Res, doi:10.1007/s11356-022-22345-w
Koekkoek, Hettinga, De Vries, Zanten, Van, Micronutrient Deficiencies in Critical Illness, Clin. Nutr, doi:10.1016/j.clnu.2021.05.003
Koekkoek, Van Zanten, Antioxidant Vitamins and Trace Elements in Critical Illness, Nutr. Clin. Pract, doi:10.1177/0884533616653832
Krinsky, Johnson, Carotenoid Actions and Their Relation to Health and Disease, Mol. Asp. Med
Lambermont, Rousseau, Seidel, Thys, Cavalleri et al., Outcome Improvement Between the First Two Waves of the Coronavirus Disease 2019 Pandemic in a Single Tertiary-Care Hospital in Belgium, Crit. Care Explor, doi:10.1097/CCE.0000000000000438
Lanham-New, Webb, Cashman, Buttriss, Fallowfield et al., Vitamin D and SARS-CoV-2 Virus/COVID-19 Disease, BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2020-000089
Majeed, Nagabhushanam, Gowda, Mundkur, An Exploratory Study of Selenium Status in Healthy Individuals and in Patients with COVID-19 in a South Indian Population: The Case for Adequate Selenium Status, Nutrition
Martinez, Huang, Acuna, Laverde, Trujillo et al., Role of Selenium in Viral Infections with a Major Focus on SARS-CoV-2, Int. J. Mol. Sci, doi:10.3390/ijms23010280
Moghaddam, Heller, Sun, Seelig, Cherkezov et al., Selenium Deficiency is Associated with Mortality Risk from COVID-19, Nutrients, doi:10.3390/nu12072098
Mueller, Mcnamara, Sinclair, Why Does COVID-19 Disproportionately Affect Older People?, Aging, doi:10.18632/aging.103344
Munteanu, Schwartz, The Relationship between Nutrition and the Immune System, Front. Nutr, doi:10.3389/fnut.2022.1082500
Muthuvattur Pallath, Ahirwar, Chandra Tripathi, Asia, Sakarde et al., COVID-19 and Nutritional Deficiency: A Review of Existing Knowledge, Horm. Mol. Biol. Clin. Investig, doi:10.1515/hmbci-2020-0074
Notz, Herrmann, Schlesinger, Helmer, Sudowe et al., Clinical Significance of Micronutrient Supplementation in Critically Ill COVID-19 Patients with Severe ARDS, Nutrients, doi:10.3390/nu13062113
Ostermann, Summers, Lei, Card, Harrington et al., Micronutrients in Critically Ill Patients with Severe Acute Kidney Injury-A Prospective Study, Sci. Rep, doi:10.1038/s41598-020-58115-2
Parant, Bouloy, Haesebaert, Bendim'red, Goldet et al., Vitamin D and COVID-19 Severity in Hospitalized Older Patients: Potential Benefit of Prehospital Vitamin D Supplementation, Nutrients, doi:10.3390/nu14081641
Pechlivanidou, Vlachakis, Tsarouhas, Panidis, Tsitsimpikou et al., The Prognostic Role of Micronutrient Status and Supplements in COVID-19 Outcomes: A Systematic Review, Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc, doi:10.1016/j.fct.2022.112901
Pouw, Van De Maat, Veerman, Ten Oever, Janssen et al., Clinical Characteristics and Outcomes of 952 Hospitalized COVID-19 Patients in The Netherlands: A Retrospective Cohort Study, PLoS ONE, doi:10.1371/journal.pone.0248713
Read, Obeid, Ahlenstiel, Ahlenstiel, The Role of Zinc in Antiviral Immunity, Adv. Nutr
Rederstorff, Krol, Lescure, Understanding the Importance of Selenium and Selenoproteins in Muscle Function, Cell. Mol. Life Sci, doi:10.1007/s00018-005-5313-y
Renata, Arely, Gabriela, Esther, Immunomodulatory Role of Microelements in COVID-19 Outcome: A Relationship with Nutritional Status, Biol. Trace Elem. Res, doi:10.1007/s12011-022-03290-8
Richardson, Lovegrove, Nutritional Status of Micronutrients as a Possible and Modifiable Risk Factor for COVID-19: A UK Perspective, Br. J. Nutr, doi:10.1017/S000711452000330X
Rockwood, Song, Macknight, Bergman, Hogan et al., A Global Clinical Measure of Fitness and Frailty in Elderly People, CMAJ, doi:10.1503/cmaj.050051
Rosa, Franca, Lanes, Vieira, Carvalho et al., Reduction of Serum Concentrations and Synergy between Retinol, β-Carotene, and Zinc According to Cancer Staging and Different Treatment Modalities Prior to Radiation Therapy in Women with Breast Cancer, Nutrients, doi:10.3390/nu11122953
Saadatian-Elahi, Picot, Hénaff, Pradel, Escuret et al., Protocol for a Prospective, Observational, Hospital-Based Multicentre Study of Nosocomial SARS-CoV-2 Transmission: NOSO-COR Project, BMJ Open, doi:10.1136/bmjopen-2020-039088
Salahshoori, Mobaraki-Asl, Seyfaee, Mirzaei Nasirabad, Dehghan et al., Overview of COVID-19 Disease: Virology, Epidemiology, Prevention Diagnosis, Treatment, and Vaccines, Biologics, doi:10.3390/biologics1010002
Salo, Mendy, Wilkerson, Molsberry, Feinstein et al., Serum Antioxidant Vitamins and Respiratory Morbidity and Mortality: A Pooled Analysis, Respir. Res, doi:10.1186/s12931-022-02059-w
Skalny, Rink, Ajsuvakova, Aschner, Gritsenko et al., Zinc and Respiratory Tract Infections: Perspectives for COVID-19 (Review), Int. J. Mol. Med, doi:10.3892/ijmm.2020.4575
Tomasa-Irriguible, Bielsa-Berrocal, Bordejé-Laguna, Tural-Llàcher, Barallat et al., Low Levels of Few Micronutrients May Impact COVID-19 Disease Progression: An Observational Study on the First Wave, Metabolites, doi:10.3390/metabo11090565
Tourkochristou, Triantos, Mouzaki, The Influence of Nutritional Factors on Immunological Outcomes, Front. Immunol, doi:10.3389/fimmu.2021.665968
Trujillo-Mayol, Guerra-Valle, Casas-Forero, Sobral, Viegas et al., Western Dietary Pattern Antioxidant Intakes and Oxidative Stress: Importance During the SARS-CoV-2/COVID-19 Pandemic, Adv. Nutr, doi:10.1093/advances/nmaa171
Voelkle, Gregoriano, Neyer, Koch, Kutz et al., Prevalence of Micronutrient Deficiencies in Patients Hospitalized with COVID-19: An Observational Cohort Study, Nutrients
Vogel-González, Talló-Parra, Herrera-Fernández, Pérez-Vilaró, Chillón et al., Low Zinc Levels at Admission Associates with Poor Clinical Outcomes in SARS-CoV-2 Infection, Nutrients, doi:10.3390/nu13020562
Vural, Avery, Kalogiros, Coneyworth, Welham, Trace Mineral Intake and Deficiencies in Older Adults Living in the Community and Institutions: A Systematic Review, Nutrients, doi:10.3390/nu12041072
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors Associated with COVID-19-Related Death Using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Wong, Rinaldi, Ho, Zinc Deficiency Enhanced Inflammatory Response by Increasing Immune Cell Activation and Inducing IL6 Promoter Demethylation, Mol. Nutr. Food Res, doi:10.1002/mnfr.201400761
Younesian, Khodabakhshi, Abdolahi, Norouzi, Behnampour et al., Decreased Serum Selenium Levels of COVID-19 Patients in Comparison with Healthy Individuals, Biol. Trace Elem. Res, doi:10.1007/s12011-021-02797-w
lahaye