Vitamin D insufficiency in COVID-19 and influenza A, and critical illness survivors: a cross-sectional study
et al., BMJ Open, doi:10.1136/bmjopen-2021-055435, Oct 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Analysis of 259 hospitalized COVID-19 patients in the UK, showing a majority of patients had vitamin D deficiency/insufficiency, which was associated with poor outcomes. Both free and total 25(OH)D were analyzed with consistent results. ISRCTN66726260.
This is the 100th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 68.4% lower, RR 0.32, p = 0.005, high D levels 68, low D levels 191, odds ratio converted to relative risk, >50nmol/l, multivariable, Supplementary Table 2, control prevalance approximated with overall prevalence.
|
|
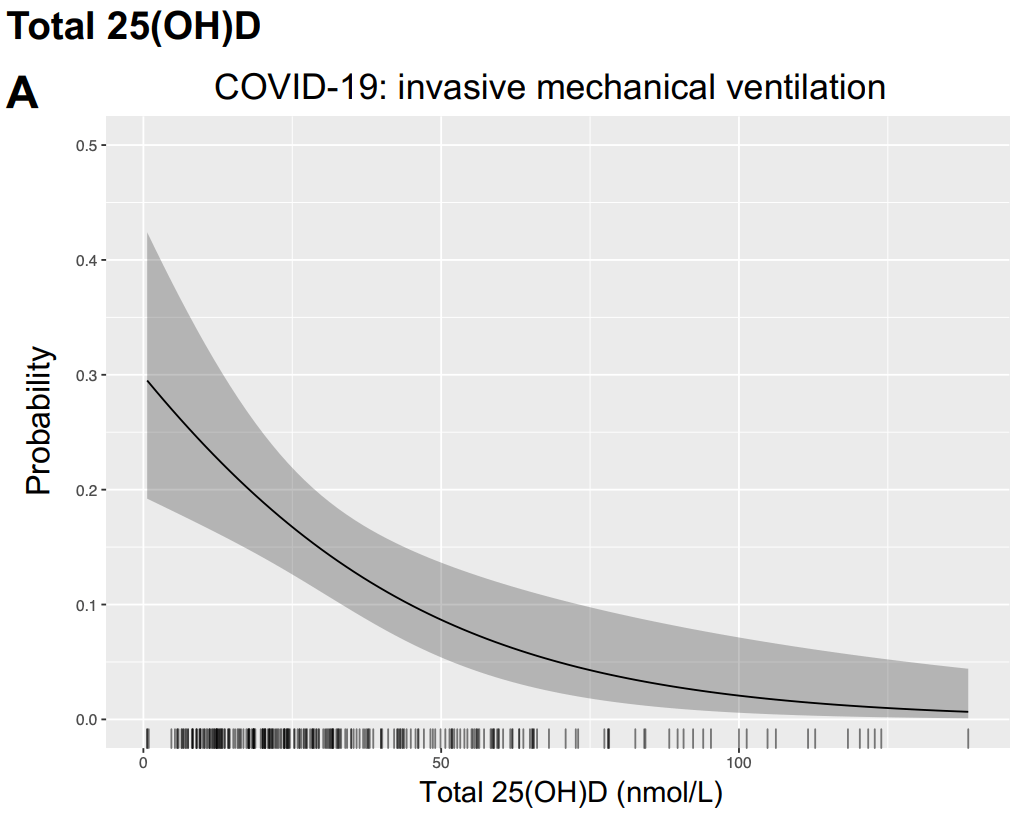
risk of mechanical ventilation, 66.0% lower, RR 0.34, p = 0.004, high D levels 6 of 68 (8.8%), low D levels 61 of 191 (31.9%), NNT 4.3, odds ratio converted to relative risk, >50nmol/l, multivariable, Supplementary Table 2.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Hurst et al., 22 Oct 2021, prospective, United Kingdom, peer-reviewed, 23 authors.
Vitamin D insufficiency in COVID-19 and influenza A, and critical illness survivors: a cross-sectional study
BMJ Open, doi:10.1136/bmjopen-2021-055435
Objectives The steroid hormone vitamin D has roles in immunomodulation and bone health. Insufficiency is associated with susceptibility to respiratory infections. We report 25-hydroxy vitamin D (25(OH)D) measurements in hospitalised people with COVID-19 and influenza A and in survivors of critical illness to test the hypotheses that vitamin D insufficiency scales with illness severity and persists in survivors. Design Cross-sectional study. Setting and participants Plasma was obtained from 295 hospitalised people with COVID-19 (International Severe Acute Respiratory and emerging Infections Consortium (ISARIC)/WHO Clinical Characterization Protocol for Severe Emerging Infections UK study), 93 with influenza A (Mechanisms of Severe Acute Influenza Consortium (MOSAIC) study, during the 2009-2010 H1N1 pandemic) and 139 survivors of non-selected critical illness (prior to the COVID-19 pandemic). Total 25(OH)D was measured by liquid chromatography-tandem mass spectrometry. Free 25(OH)D was measured by ELISA in COVID-19 samples. Outcome measures Receipt of invasive mechanical ventilation (IMV) and in-hospital mortality. Results Vitamin D insufficiency (total 25(OH)D 25-50 nmol/L) and deficiency (<25 nmol/L) were prevalent in COVID-19 (29.3% and 44.4%, respectively), influenza A (47.3% and 37.6%) and critical illness survivors (30.2% and 56.8%). In COVID-19 and influenza A, total 25(OH) D measured early in illness was lower in patients who received IMV (19.6 vs 31.9 nmol/L (p<0.0001) and 22.9 vs 31.1 nmol/L (p=0.0009), respectively). In COVID-19, biologically active free 25(OH)D correlated with total 25(OH)D and was lower in patients who received IMV, but was not associated with selected circulating inflammatory mediators. Conclusions Vitamin D deficiency/insufficiency was present in majority of hospitalised patients with COVID-19 or influenza A and correlated with severity and persisted in critical illness survivors at concentrations expected to disrupt bone metabolism. These findings support early supplementation trials to determine if insufficiency is causal in progression to severe disease, and investigation of longer-term bone health outcomes.
Ethics approval Ethical approval for the ISARIC/WHO CCP-UK study (COVID- 19) was given by the South Central Oxford C Research Ethics Committee in England (13/SC/0149), the Scotland A Research Ethics Committee (20/SS/0028), and the WHO Ethics Review Committee (RPC571 and RPC572, 25 April 2013). Ethical approval for the MOSAIC study (influenza A) was given by the NHS National Research Ethics Service, Outer West London Research Ethics Committee (09/ H0709/52, 09/MRE00/67). Provenance and peer review Not commissioned; externally peer reviewed. Data availability statement Data are available upon reasonable request. Data generated by the ISARIC4C consortium is available for collaborative analysis projects through an independent data and materials access committee at isaric4c. net/ sample_ access. Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and..
References
Amrein, Christopher, Mcnally, Understanding vitamin D deficiency in intensive care patients, Intensive Care Med, doi:10.1007/s00134-015-3937-4
Amrein, Schnedl, Holl, Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial, JAMA, doi:10.1001/jama.2014.13204
Arnson, Gringauz, Itzhaky, Vitamin D deficiency is associated with poor outcomes and increased mortality in severely ill patients, QJM, doi:10.1093/qjmed/hcs014
Baillie, Peter, Openshaw, Carson, Alex et al., Patient Engagement: Seán Keating. Outbreak Laboratory Staff and Volunteers, doi:10.1016/j.mce.2010.02.013
Bmj Open, None
Braun, Chang, Mahadevappa, Association of low serum 25-hydroxyvitamin D levels and mortality in the critically ill, Crit Care Med, doi:10.1097/CCM.0b013e318206ccdf
Braun, Litonjua, Moromizato, Association of low serum 25-hydroxyvitamin D levels and acute kidney injury in the critically ill, Crit Care Med, doi:10.1097/CCM.0b013e318260c928
Campbell, Spector, Hormonally active vitamin D3 (1alpha,25-dihydroxycholecalciferol) triggers autophagy in human macrophages that inhibits HIV-1 infection, J Biol Chem, doi:10.1074/jbc.M110.206110
Carpagnano, Lecce, Quaranta, Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J Endocrinol Invest, doi:10.1007/s40618-020-01370-x
Castillo, Costa, Barrios, Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2020.105751
Chun, Lauridsen, Suon, Vitamin D-binding protein directs monocyte responses to 25-hydroxy-and 1,25-dihydroxyvitamin D, J Clin Endocrinol Metab, doi:10.1210/jc.2010-0195
Chun, Peercy, Adams, Vitamin D binding protein and monocyte response to 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D: analysis by mathematical modeling, PLoS One, doi:10.1371/journal.pone.0030773
Czarnik, Czarnik, Gawda, Vitamin D kinetics in the acute phase of critical illness: a prospective observational study, J Crit Care, doi:10.1016/j.jcrc.2017.09.179
D'avolio, Avataneo, Manca, 25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Dancer, Parekh, Lax, Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS), Thorax, doi:10.1136/thoraxjnl-2014-206680
De Haan, Groeneveld, De Geus, Vitamin D deficiency as a risk factor for infection, sepsis and mortality in the critically ill: systematic review and meta-analysis, Crit Care, doi:10.1186/s13054-014-0660-4
Docherty, Harrison, Green, Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study, BMJ, doi:10.1136/bmj.m1985
Dunning, Blankley, Hoang, Progression of wholeblood transcriptional signatures from interferon-induced to neutrophil-associated patterns in severe influenza, Nat Immunol, doi:10.1038/s41590-018-0111-5
Francis, Aspray, Fraser, Vitamin D and Bone Health : A Practical Clinical Guideline for Patient Management, doi:10.1136/bmjopen-2021-055435:e055435.112021
Ganmaa, Uyanga, Zhou, Vitamin D supplements for prevention of tuberculosis infection and disease, N Engl J Med, doi:10.1056/NEJMoa1915176
Griffith, Lewis, Rossi, Systemic inflammation after critical illness: relationship with physical recovery and exploration of potential mechanisms, Thorax, doi:10.1136/thoraxjnl-2015-208114
Han, Alvarez, Jones, Impact of high-dose vitamin D 3 on plasma free 25-hydroxyvitamin D concentrations and antimicrobial peptides in critically ill mechanically ventilated adults, Nutrition, doi:10.1016/j.nut.2017.02.002
Heart, Lung ; Ginde, Brower, Early High-Dose Vitamin D 3 for Critically Ill, Vitamin D-Deficient Patients, N Engl J Med, doi:10.1056/NEJMoa1911124
Hurst, Homer, Gow, Vitamin D status is seasonally stable in northern European dogs, Vet Clin Pathol, doi:10.1111/vcp.12859
Kaufman, Niles, Kroll, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One, doi:10.1371/journal.pone.0239252
Khare, Godbole, Pawar, Calcitriol [1, 25[OH]2 D3] pre-and post-treatment suppresses inflammatory response to influenza A (H1N1) infection in human lung A549 epithelial cells, Eur J Nutr, doi:10.1007/s00394-012-0449-7
Larner, Jenkinson, Chun, Free versus total serum 25-hydroxyvitamin D in a murine model of colitis, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2019.01.015
Lee, Vitamin D metabolism and deficiency in critical illness, Best Pract Res Clin Endocrinol Metab, doi:10.1016/j.beem.2011.03.001
Lips, Vitamin, Deficiency and Secondary Hyperparathyroidism in the Elderly: Consequences for Bone Loss and Fractures and Therapeutic Implications, Endocr Rev, doi:10.1210/edrv.22.4.0437
Liu, Stenger, Li, Toll-Like receptor triggering of a vitamin D-mediated human antimicrobial response, Science, doi:10.1126/science.1123933
Lubin, Colt, Camann, Epidemiologic evaluation of measurement data in the presence of detection limits, Environ Health Perspect, doi:10.1289/ehp.7199
Lucidarme, Messai, Mazzoni, Incidence and risk factors of vitamin D deficiency in critically ill patients: results from a prospective observational study, Intensive Care Med, doi:10.1007/s00134-010-1875-8
Ma, Zhou, Heianza, Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank, Am J Clin Nutr, doi:10.1093/ajcn/nqaa381
Malabanan, Veronikis, Holick, Redefining vitamin D insufficiency, Lancet, doi:10.1016/S0140-6736(05)78933-9
Martineau, Jolliffe, Greenberg, Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis, Health Technol Assess, doi:10.3310/hta23020
Mathyssen, Gayan-Ramirez, Bouillon, Vitamin D supplementation in respiratory diseases: evidence from randomized controlled trials, Pol Arch Intern Med, doi:10.20452/pamw.4134
Meltzer, Best, Zhang, Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.19722
Monlezun, Bittner, Christopher, Vitamin D status and acute respiratory infection: cross sectional results from the United States National health and nutrition examination survey, 2001-2006, Nutrients, doi:10.3390/nu7031933
Murai, Fernandes, Sales, Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial, JAMA, doi:10.1001/jama.2020.26848
Ney, Heyland, Amrein, The relevance of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D concentration for postoperative infections and postoperative organ dysfunctions in cardiac surgery patients: the evidence study, Clin Nutr, doi:10.1016/j.clnu.2018.11.033
Nogues, Ovejero, Pineda-Moncusí, Calcifediol treatment and COVID-19-Related outcomes, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab405
Orford, Lane, Bailey, Changes in bone mineral density in the year after critical illness, Am J Respir Crit Care Med, doi:10.1164/rccm.201508-1514OC
Panagiotou, Tee, Ihsan, Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity, Clin Endocrinol, doi:10.1111/cen.14276
Papadimitriou, Vassaras, Holick, Association between population vitamin D status and SARS-CoV-2 related serious-critical illness and deaths: an ecological integrative approach, World J Virol, doi:10.5501/wjv.v10.i3.111
Quraishi, Camargo, Vitamin D in acute stress and critical illness, Curr Opin Clin Nutr Metab Care, doi:10.1097/MCO.0b013e328358fc2b
Quraishi, Pascale, Needleman, Effect of cholecalciferol supplementation on vitamin D status and cathelicidin levels in sepsis: a randomized, placebo-controlled trial, Crit Care Med, doi:10.1097/CCM.0000000000001148
Sabetta, Depetrillo, Cipriani, Serum 25-hydroxyvitamin D and the incidence of acute viral respiratory tract infections in healthy adults, PLoS One, doi:10.1371/journal.pone.0011088
Sai, Walters, Fang, Gallagher, Relationship between Vitamin D, Parathyroid Hormone, and Bone Health, J Clin Endocrinol Metab, doi:10.1210/jc.2010-1886
Sai, Walters, Fang, Relationship between vitamin D, parathyroid hormone, and bone health, J Clin Endocrinol Metab, doi:10.1210/jc.2010-1886
Thwaites, Sevilla Uruchurtu, Siggins, Inflammatory profiles across the spectrum of disease reveal a distinct role for GM-CSF in severe COVID-19, Sci Immunol, doi:10.1126/sciimmunol.abg9873
Walsh, Salisbury, Merriweather, Increased hospitalbased physical rehabilitation and information provision after intensive care unit discharge: the recover randomized clinical trial, JAMA Intern Med, doi:10.1001/jamainternmed.2015.0822
Wood, Fast stable restricted maximum likelihood and marginal likelihood estimation of semiparametric generalized linear models, Journal of the Royal Statistical Society: Series B, doi:10.1111/j.1467-9868.2010.00749.x
Wood, Thin plate regression splines, Journal of the Royal Statistical Society: Series B, doi:10.1111/1467-9868.00374
Yuk, Shin, Lee, Vitamin D3 induces autophagy in human monocytes/macrophages via cathelicidin, Cell Host Microbe, doi:10.1016/j.chom.2009.08.004
DOI record:
{
"DOI": "10.1136/bmjopen-2021-055435",
"ISSN": [
"2044-6055",
"2044-6055"
],
"URL": "http://dx.doi.org/10.1136/bmjopen-2021-055435",
"abstract": "<jats:sec><jats:title>Objectives</jats:title><jats:p>The steroid hormone vitamin D has roles in immunomodulation and bone health. Insufficiency is associated with susceptibility to respiratory infections. We report 25-hydroxy vitamin D (25(OH)D) measurements in hospitalised people with COVID-19 and influenza A and in survivors of critical illness to test the hypotheses that vitamin D insufficiency scales with illness severity and persists in survivors.</jats:p></jats:sec><jats:sec><jats:title>Design</jats:title><jats:p>Cross-sectional study.</jats:p></jats:sec><jats:sec><jats:title>Setting and participants</jats:title><jats:p>Plasma was obtained from 295 hospitalised people with COVID-19 (International Severe Acute Respiratory and emerging Infections Consortium (ISARIC)/WHO Clinical Characterization Protocol for Severe Emerging Infections UK study), 93 with influenza A (Mechanisms of Severe Acute Influenza Consortium (MOSAIC) study, during the 2009–2010 H1N1 pandemic) and 139 survivors of non-selected critical illness (prior to the COVID-19 pandemic). Total 25(OH)D was measured by liquid chromatography-tandem mass spectrometry. Free 25(OH)D was measured by ELISA in COVID-19 samples.</jats:p></jats:sec><jats:sec><jats:title>Outcome measures</jats:title><jats:p>Receipt of invasive mechanical ventilation (IMV) and in-hospital mortality.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Vitamin D insufficiency (total 25(OH)D 25–50 nmol/L) and deficiency (<25 nmol/L) were prevalent in COVID-19 (29.3% and 44.4%, respectively), influenza A (47.3% and 37.6%) and critical illness survivors (30.2% and 56.8%). In COVID-19 and influenza A, total 25(OH)D measured early in illness was lower in patients who received IMV (19.6 vs 31.9 nmol/L (p<0.0001) and 22.9 vs 31.1 nmol/L (p=0.0009), respectively). In COVID-19, biologically active free 25(OH)D correlated with total 25(OH)D and was lower in patients who received IMV, but was not associated with selected circulating inflammatory mediators.</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>Vitamin D deficiency/insufficiency was present in majority of hospitalised patients with COVID-19 or influenza A and correlated with severity and persisted in critical illness survivors at concentrations expected to disrupt bone metabolism. These findings support early supplementation trials to determine if insufficiency is causal in progression to severe disease, and investigation of longer-term bone health outcomes.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjopen-2021-055435"
],
"author": [
{
"affiliation": [],
"family": "Hurst",
"given": "Emma A",
"sequence": "first"
},
{
"affiliation": [],
"family": "Mellanby",
"given": "Richard J",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Handel",
"given": "Ian",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9500-241X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Griffith",
"given": "David M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rossi",
"given": "Adriano G",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Walsh",
"given": "Timothy S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shankar-Hari",
"given": "Manu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dunning",
"given": "Jake",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Homer",
"given": "Natalie Z",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Denham",
"given": "Scott G",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Devine",
"given": "Kerri",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Holloway",
"given": "Paul A",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moore",
"given": "Shona C",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Thwaites",
"given": "Ryan S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Samanta",
"given": "Romit J",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7269-2873",
"affiliation": [],
"authenticated-orcid": false,
"family": "Summers",
"given": "Charlotte",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hardwick",
"given": "Hayley E",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Oosthuyzen",
"given": "Wilna",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Turtle",
"given": "Lance",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Semple",
"given": "Malcolm G",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Openshaw",
"given": "Peter J M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Baillie",
"given": "J Kenneth",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9873-8243",
"affiliation": [],
"authenticated-orcid": false,
"family": "Russell",
"given": "Clark D",
"sequence": "additional"
}
],
"clinical-trial-number": [
{
"clinical-trial-number": "isrctn09412438",
"registry": "10.18810/isrctn"
}
],
"container-title": "BMJ Open",
"container-title-short": "BMJ Open",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
10,
22
]
],
"date-time": "2021-10-22T15:02:27Z",
"timestamp": 1634914947000
},
"deposited": {
"date-parts": [
[
2021,
10,
22
]
],
"date-time": "2021-10-22T15:03:00Z",
"timestamp": 1634914980000
},
"funder": [
{
"DOI": "10.13039/501100000265",
"award": [
"MC_PC_19059",
"MR/R005982/1"
],
"doi-asserted-by": "publisher",
"name": "Medical Research Council"
},
{
"DOI": "10.13039/501100000272",
"award": [
"CS-2016-16-011"
],
"doi-asserted-by": "publisher",
"name": "National Institute for Health Research"
},
{
"DOI": "10.13039/100010269",
"award": [
"205228/Z/16/Z",
"215091/Z/18/Z"
],
"doi-asserted-by": "publisher",
"name": "Wellcome"
},
{
"DOI": "10.13039/501100000272",
"award": [
"CO-CIN-01"
],
"doi-asserted-by": "crossref",
"name": "National Institute for Health Research"
}
],
"indexed": {
"date-parts": [
[
2024,
4,
2
]
],
"date-time": "2024-04-02T16:05:27Z",
"timestamp": 1712073927713
},
"is-referenced-by-count": 10,
"issue": "10",
"issued": {
"date-parts": [
[
2021,
10
]
]
},
"journal-issue": {
"issue": "10",
"published-online": {
"date-parts": [
[
2021,
10,
22
]
]
},
"published-print": {
"date-parts": [
[
2021,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 21,
"start": {
"date-parts": [
[
2021,
10,
22
]
],
"date-time": "2021-10-22T00:00:00Z",
"timestamp": 1634860800000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjopen-2021-055435",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e055435",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
10
]
]
},
"published-online": {
"date-parts": [
[
2021,
10,
22
]
]
},
"published-print": {
"date-parts": [
[
2021,
10
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1016/j.mce.2010.02.013",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.1"
},
{
"DOI": "10.1210/jc.2010-0195",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.2"
},
{
"DOI": "10.1371/journal.pone.0011088",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.3"
},
{
"DOI": "10.3390/nu7031933",
"article-title": "Vitamin D status and acute respiratory infection: cross sectional results from the United States National health and nutrition examination survey, 2001-2006",
"author": "Monlezun",
"doi-asserted-by": "crossref",
"first-page": "1933",
"journal-title": "Nutrients",
"key": "2021102207552340000_11.10.e055435.4",
"volume": "7",
"year": "2015"
},
{
"DOI": "10.1136/thoraxjnl-2014-206680",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.5"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"article-title": "Association of vitamin D status and other clinical characteristics with COVID-19 test results",
"author": "Meltzer",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw Open",
"key": "2021102207552340000_11.10.e055435.6",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0239252",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.7"
},
{
"DOI": "10.5501/wjv.v10.i3.111",
"article-title": "Association between population vitamin D status and SARS-CoV-2 related serious-critical illness and deaths: an ecological integrative approach",
"author": "Papadimitriou",
"doi-asserted-by": "crossref",
"first-page": "111",
"journal-title": "World J Virol",
"key": "2021102207552340000_11.10.e055435.8",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1097/MCO.0b013e328358fc2b",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.9"
},
{
"article-title": "Vitamin D supplementation in respiratory diseases: evidence from randomized controlled trials",
"author": "Mathyssen",
"first-page": "775",
"journal-title": "Pol Arch Intern Med",
"key": "2021102207552340000_11.10.e055435.10",
"volume": "127",
"year": "2017"
},
{
"DOI": "10.3310/hta23010",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.11"
},
{
"DOI": "10.1056/NEJMoa1915176",
"article-title": "Vitamin D supplements for prevention of tuberculosis infection and disease",
"author": "Ganmaa",
"doi-asserted-by": "crossref",
"first-page": "359",
"journal-title": "N Engl J Med",
"key": "2021102207552340000_11.10.e055435.12",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.26848",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.13"
},
{
"DOI": "10.1164/rccm.201508-1514OC",
"article-title": "Changes in bone mineral density in the year after critical illness",
"author": "Orford",
"doi-asserted-by": "crossref",
"first-page": "736",
"journal-title": "Am J Respir Crit Care Med",
"key": "2021102207552340000_11.10.e055435.14",
"volume": "193",
"year": "2016"
},
{
"DOI": "10.1136/bmj.m1985",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.15"
},
{
"DOI": "10.1038/s41590-018-0111-5",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.16"
},
{
"DOI": "10.1001/jamainternmed.2015.0822",
"article-title": "Increased hospital-based physical rehabilitation and information provision after intensive care unit discharge: the recover randomized clinical trial",
"author": "Walsh",
"doi-asserted-by": "crossref",
"first-page": "901",
"journal-title": "JAMA Intern Med",
"key": "2021102207552340000_11.10.e055435.17",
"volume": "175",
"year": "2015"
},
{
"DOI": "10.1136/thoraxjnl-2015-208114",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.18"
},
{
"DOI": "10.1111/vcp.12859",
"article-title": "Vitamin D status is seasonally stable in northern European dogs",
"author": "Hurst",
"doi-asserted-by": "crossref",
"first-page": "279",
"journal-title": "Vet Clin Pathol",
"key": "2021102207552340000_11.10.e055435.19",
"volume": "49",
"year": "2020"
},
{
"DOI": "10.1210/jc.2010-1886",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.20"
},
{
"DOI": "10.1111/1467-9868.00374",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.21"
},
{
"DOI": "10.1111/j.1467-9868.2010.00749.x",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.22"
},
{
"DOI": "10.1289/ehp.7199",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.23"
},
{
"DOI": "10.1126/sciimmunol.abg9873",
"article-title": "Inflammatory profiles across the spectrum of disease reveal a distinct role for GM-CSF in severe COVID-19",
"author": "Thwaites",
"doi-asserted-by": "crossref",
"journal-title": "Sci Immunol",
"key": "2021102207552340000_11.10.e055435.24",
"volume": "6",
"year": "2021"
},
{
"article-title": "25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2",
"author": "D'Avolio",
"journal-title": "Nutrients",
"key": "2021102207552340000_11.10.e055435.25",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1111/cen.14276",
"article-title": "Low serum 25‐hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID‐19 are associated with greater disease severity",
"author": "Panagiotou",
"doi-asserted-by": "crossref",
"first-page": "508",
"journal-title": "Clin Endocrinol",
"key": "2021102207552340000_11.10.e055435.26",
"volume": "93",
"year": "2020"
},
{
"DOI": "10.1007/s40618-020-01370-x",
"article-title": "Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19",
"author": "Carpagnano",
"doi-asserted-by": "crossref",
"first-page": "765",
"journal-title": "J Endocrinol Invest",
"key": "2021102207552340000_11.10.e055435.27",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1016/j.chom.2009.08.004",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.28"
},
{
"DOI": "10.1126/science.1123933",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.29"
},
{
"DOI": "10.1074/jbc.M110.206110",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.30"
},
{
"DOI": "10.1007/s00394-012-0449-7",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.31"
},
{
"DOI": "10.1371/journal.pone.0030773",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.32"
},
{
"DOI": "10.1016/j.jsbmb.2019.01.015",
"article-title": "Free versus total serum 25-hydroxyvitamin D in a murine model of colitis",
"author": "Larner",
"doi-asserted-by": "crossref",
"first-page": "204",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "2021102207552340000_11.10.e055435.33",
"volume": "189",
"year": "2019"
},
{
"DOI": "10.1016/j.nut.2017.02.002",
"article-title": "Impact of high-dose vitamin D\n 3\n on plasma free 25-hydroxyvitamin D concentrations and antimicrobial peptides in critically ill mechanically ventilated adults",
"author": "Han",
"doi-asserted-by": "crossref",
"first-page": "102",
"journal-title": "Nutrition",
"key": "2021102207552340000_11.10.e055435.34",
"volume": "38",
"year": "2017"
},
{
"DOI": "10.1097/CCM.0000000000001148",
"article-title": "Effect of cholecalciferol supplementation on vitamin D status and cathelicidin levels in sepsis: a randomized, placebo-controlled trial",
"author": "Quraishi",
"doi-asserted-by": "crossref",
"first-page": "1928",
"journal-title": "Crit Care Med",
"key": "2021102207552340000_11.10.e055435.35",
"volume": "43",
"year": "2015"
},
{
"DOI": "10.1097/CCM.0b013e318206ccdf",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.36"
},
{
"DOI": "10.1007/s00134-010-1875-8",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.37"
},
{
"DOI": "10.1016/j.jcrc.2017.09.179",
"article-title": "Vitamin D kinetics in the acute phase of critical illness: a prospective observational study",
"author": "Czarnik",
"doi-asserted-by": "crossref",
"first-page": "294",
"journal-title": "J Crit Care",
"key": "2021102207552340000_11.10.e055435.38",
"volume": "43",
"year": "2018"
},
{
"DOI": "10.1007/s00134-015-3937-4",
"article-title": "Understanding vitamin D deficiency in intensive care patients",
"author": "Amrein",
"doi-asserted-by": "crossref",
"first-page": "1961",
"journal-title": "Intensive Care Med",
"key": "2021102207552340000_11.10.e055435.39",
"volume": "41",
"year": "2015"
},
{
"DOI": "10.1016/j.beem.2011.03.001",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.40"
},
{
"DOI": "10.1097/CCM.0b013e318260c928",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.41"
},
{
"DOI": "10.1093/qjmed/hcs014",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.42"
},
{
"DOI": "10.1186/s13054-014-0660-4",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.43"
},
{
"DOI": "10.1016/S0140-6736(05)78933-9",
"article-title": "Redefining vitamin D insufficiency",
"author": "Malabanan",
"doi-asserted-by": "crossref",
"first-page": "805",
"journal-title": "Lancet",
"key": "2021102207552340000_11.10.e055435.44",
"volume": "351",
"year": "1998"
},
{
"DOI": "10.1001/jama.2014.13204",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.45"
},
{
"DOI": "10.1056/NEJMoa1911124",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.46"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "publisher",
"key": "2021102207552340000_11.10.e055435.47"
},
{
"DOI": "10.1210/clinem/dgab405",
"article-title": "Calcifediol treatment and COVID-19-Related outcomes",
"author": "Nogues",
"doi-asserted-by": "crossref",
"first-page": "e4017",
"journal-title": "J Clin Endocrinol Metab",
"key": "2021102207552340000_11.10.e055435.48",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1093/ajcn/nqaa381",
"article-title": "Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank",
"author": "Ma",
"doi-asserted-by": "crossref",
"first-page": "1275",
"journal-title": "Am J Clin Nutr",
"key": "2021102207552340000_11.10.e055435.49",
"volume": "113",
"year": "2021"
},
{
"DOI": "10.1016/j.clnu.2018.11.033",
"article-title": "The relevance of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D concentration for postoperative infections and postoperative organ dysfunctions in cardiac surgery patients: the evidence study",
"author": "Ney",
"doi-asserted-by": "crossref",
"first-page": "2756",
"journal-title": "Clin Nutr",
"key": "2021102207552340000_11.10.e055435.50",
"volume": "38",
"year": "2019"
}
],
"reference-count": 50,
"references-count": 50,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2021-055435"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Vitamin D insufficiency in COVID-19 and influenza A, and critical illness survivors: a cross-sectional study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "11"
}
