The Impact of GLP-1 RAs and DPP-4is on Hospitalisation and Mortality in the COVID-19 Era: A Two-Year Observational Study
et al., Biomedicines, doi:10.3390/biomedicines11082292, Aug 2023
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
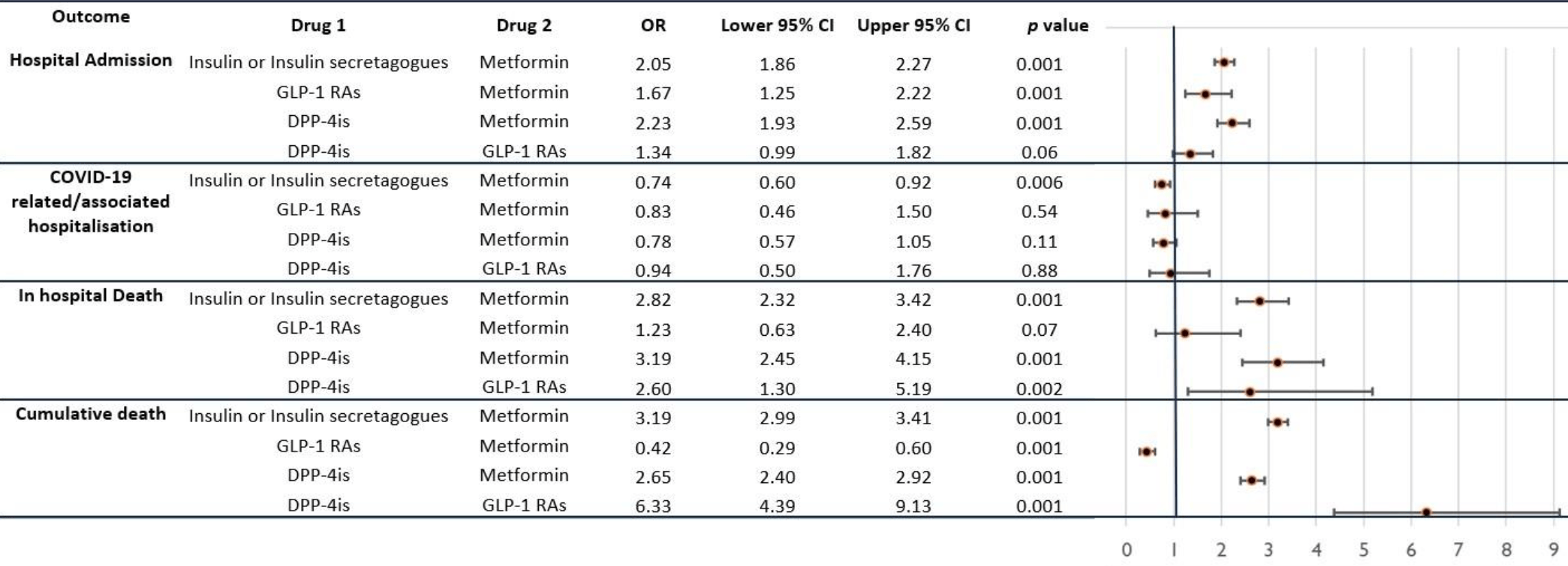
Retrospective 76,764 diabetes patients in Italy, showing that patients on metformin had lower rates of COVID-19 hospitalization compared to those on insulin/insulin secretagogues, GLP-1 receptor agonists, and DPP-4 inhibitors. Metformin vs. no metformin results are not provided. The most relevant result for COVID-19 and metformin may be the DPP-4i comparison, based on the DPP-4i group being the most similar to the metformin group in terms of baseline COVID-19 risk and confounders. Patients on insulin/secretagogues may have more severe or advanced diabetes.
|
risk of hospitalization, 22.0% lower, OR 0.78, p = 0.11, treatment 30,238, control 2,264, DPP-4is, RR approximated with OR.
|
|
risk of hospitalization, 26.0% lower, OR 0.74, p = 0.006, treatment 30,238, control 14,739, insulin or insulin secretagogues, RR approximated with OR.
|
|
risk of hospitalization, 17.0% lower, OR 0.83, p = 0.54, treatment 30,238, control 317, GLP-1 RAs, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Greco et al., 18 Aug 2023, retrospective, Italy, peer-reviewed, 8 authors, study period January 2020 - December 2021, this trial compares with another treatment - results may be better when compared to placebo.
Contact: angelina.passaro@unife.it (corresponding author), grcsvt@unife.it, v.monda@ausl.fe.it, giorgia.valpiani@unife.it, n.napoli@ospfe.it, c.crespini@ospfe.it, a.marra@ospfe.it, farmaciainterna.fo@auslromagna.it.
The Impact of GLP-1 RAs and DPP-4is on Hospitalisation and Mortality in the COVID-19 Era: A Two-Year Observational Study
Biomedicines, doi:10.3390/biomedicines11082292
Novel antidiabetic drugs have the ability to produce anti-inflammatory effects regardless of their glucose-lowering action. For this reason, these molecules (including GLP-1 RAs and DPP-4is) were hypothesized to be effective against COVID-19, which is characterized by cytokines hyperactivity and multiorgan inflammation. The aim of our work is to explore the potential protective role of GLP-1 RAs and DPP-4is in COVID-19 (with the disease intended to be a model of an acute stressor) and non-COVID-19 patients over a two-year observation period. Retrospective and one-versus-one analyses were conducted to assess the impact of antidiabetic drugs on the need for hospitalization (in both COVID-19-and non-COVID-19-related cases), in-hospital mortality, and two-year mortality. Logistic regression analyses were conducted to identify the variables associated with these outcomes. Additionally, log-rank tests were used to plot survival curves for each group of subjects, based on their antidiabetic treatment. The performed analyses revealed that despite similar hospitalization rates, subjects undergoing home therapy with GLP-1 RAs exhibited significantly lower mortality rates, even over a two-year period. These individuals demonstrated improved survival estimates both within hospital and non-hospital settings, even during a longer observation period.
Supplementary Materials: The following supporting information can be downloaded at: https:// www.mdpi.com/article/10.3390/biomedicines11082292/s1, Figure S1 : Prevalence of diabetes in the overall adult subjects in the districts of Ferrara and Romagna (A), percentage of diabetic subjects in the districts of Ferrara and Romagna and overall average of diabetic subjects (B); Figure S2 : Evaluation of the length of stay in terms of days in the subgroup of patients treated with the four main antidiabetic treatments (A); length of stay among the same four subgroups of inpatients and comparison between COVID-19 and non-COVID-19 subjects (B); Table S1 : The institutions serving the districts of Ferrara and Romagna participating in the study; Table S2 : MACEs and antidiabetic drugs. Author Contributions: S.G.: acquisition, analysis and interpretation of data, drafting the article; V.M.M.: the conception and design of the study, drafting the article and revising it critically for important intellectual content; G.V. and N.N.: collection and processing of data; C.C., F.P. and A.M.: acquisition of information concerning drug prescriptions and dispensation, processing data relating to local pharmacies; A.P.: conception and design of the study; revising the article critically for important intellectual content; and final approval of the version to be submitted. All authors have read and agreed to the published version of the manuscript. Informed Consent Statement: Not applicable.
..
References
Asakura, Ogawa, COVID-19-associated coagulopathy and disseminated intravascular coagulation, Int. J. Hematol, doi:10.1007/s12185-020-03029-y
Becker, COVID-19 update: COVID-19-associated coagulopathy, J. Thromb. Thrombolysis, doi:10.1007/s11239-020-02134-3
Bonnet, Scheen, Effects of SGLT2 inhibitors on systemic and tissue low-grade inflammation: The potential contribution to diabetes complications and cardiovascular disease, Diabetes Metab, doi:10.1016/j.diabet.2018.09.005
Bonora, Avogaro, Fadini, Disentangling conflicting evidence on DPP-4 inhibitors and outcomes of COVID-19: Narrative review and meta-analysis, J. Endocrinol. Investig, doi:10.1007/s40618-021-01515-6
Boye, Erdemir, Zimmerman, Reddy, Benneyworth et al., Risk Factors Associated with COVID-19 Hospitalization and Mortality: A Large Claims-Based Analysis Among People with Type 2 Diabetes Mellitus in the United States, Diabetes Ther, doi:10.1007/s13300-021-01110-1
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Metformin and risk of mortality in patients hospitalised with COVID-19: A retrospective cohort analysis, doi:10.1016/S2666-7568(20)30033-7
Chaudhry, Lavandero, Xie, Sabharwal, Zheng et al., Manipulation of ACE2 expression in COVID-19, doi:10.1136/openhrt-2020-001424
Chen, Lv, Lin, Arshad, Dai, The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients with Diabetes: A Bayesian Network Meta, Analysis. Front. Endocrinol, doi:10.3389/fendo.2022.895458
Corrao, Pinelli, Vacca, Raspanti, Argano, Type 2 Diabetes Mellitus and COVID-19: A Narrative Review, Front. Endocrinol. 2021, doi:10.3389/fendo.2021.609470
Dal Canto, Ceriello, Rydén, Ferrini, Hansen et al., Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications, Eur. J. Prev. Cardiol, doi:10.1177/2047487319878371
Fang, Stavrou, Schmaier, Grobe, Morris et al., Angiotensin 1-7 and Mas decrease thrombosis in Bdkrb2 -/-mice by increasing NO and prostacyclin to reduce platelet spreading and glycoprotein VI activation, Blood, doi:10.1182/blood-2012-09-459156
Feldman, Savelieff, Hayek, Pennathur, Kretzler et al., COVID-19 and Diabetes: A Collision and Collusion of Two Diseases, Diabetes, doi:10.2337/dbi20-0032
Fraga-Silva, Costa-Fraga, De Sousa, Alenina, Bader et al., An orally active formulation of angiotensin-(1-7) produces an antithrombotic effect, Clinics, doi:10.1590/S1807-59322011000500021
Gager, Lewinski, Sourij, Jilma, Eyileten et al., Effects of SGLT2 Inhibitors on Ion Homeostasis and Oxidative Stress associated Mechanisms in Heart Failure, Biomed. Pharmacother, doi:10.1016/j.biopha.2021.112169
Garvey, Van Gaal, Leiter, Vijapurkar, List et al., Effects of canagliflozin versus glimepiride on adipokines and inflammatory biomarkers in type 2 diabetes, doi:10.1016/j.metabol.2018.02.002
Ghany, Palacio, Dawkins, Chen, Mccarter et al., Metformin is associated with lower hospitalizations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA, Diabetes Metab. Syndr. Clin. Res. Rev. 2021, doi:10.1016/j.dsx.2021.02.022
Grotta, De Candia, Olivieri, Matacchione, Giuliani et al., Anti-inflammatory effect of SGLT-2 inhibitors via uric acid and insulin, Cell. Mol. Life Sci, doi:10.1007/s00018-022-04289-z
Hariyanto, Intan, Hananto, Putri, Kurniawan, Pre-admission glucagon-like peptide-1 receptor agonist (GLP-1RA) and mortality from coronavirus disease 2019 (COVID-19): A systematic review, meta-analysis, and meta-regression, Diabetes Res. Clin. Pract, doi:10.1016/j.diabres.2021.109031
Hariyanto, Kurniawan, Dipeptidyl peptidase 4 (DPP4) inhibitor and outcome from coronavirus disease 2019 (COVID-19) in diabetic patients: A systematic review, meta-analysis, and meta-regression, J. Diabetes Metab. Disord
He, Yuan, Cheng, Zhang, Guo et al., Mast Cell and M1 Macrophage Infiltration and Local Pro-Inflammatory Factors Were Attenuated with Incretin-Based Therapies in Obesity-Related Glomerulopathy, Metab. Syndr. Relat. Disord, doi:10.1089/met.2017.0057
Hedrington, Davis, Oral semaglutide for the treatment of type 2 diabetes, Expert Opin. Pharmacother
Helms, Tacquard, Severac, Leonard-Lorant, Ohana et al., High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study, Intensive Care Med, doi:10.1007/s00134-020-06062-x
Holman, Knighton, Kar, O'keefe, Curley et al., Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: A population-based cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30271-0
Iacobellis, Fricke, Effects of Semaglutide Versus Dulaglutide on Epicardial Fat Thickness in Subjects with Type 2 Diabetes and Obesity, J. Endocr. Soc, doi:10.1210/jendso/bvz042
Israelsen, Pottegård, Sandholdt, Madsbad, Thomsen et al., Comparable COVID-19 outcomes with current use of GLP-1 receptor agonists, DPP-4 inhibitors or SGLT-2 inhibitors among patients with diabetes who tested positive for SARS-CoV-2, Diabetes Obes. Metab, doi:10.1111/dom.14329
Kahkoska, Abrahamsen, Alexander, Bennett, Chute et al., Association Between Glucagon-Like Peptide 1 Receptor Agonist and Sodium-Glucose Cotransporter 2 Inhibitor Use and COVID-19 Outcomes, Diabetes Care, doi:10.2337/dc21-0065
Kan, Zhang, Han, Xu, Ye et al., Mortality Risk of Antidiabetic Agents for Type 2 Diabetes with COVID-19: A Systematic Review and Meta-Analysis, doi:10.3389/fendo.2021.708494
Khunti, Knighton, Zaccardi, Bakhai, Barron et al., Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: A nationwide observational study in England, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00050-4
Kim, Garg, O'halloran, Whitaker, Pham et al., Risk Factors for Intensive Care Unit Admission and In-hospital Mortality Among Hospitalized Adults Identified through the US Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET), Clin. Infect. Dis, doi:10.1093/cid/ciaa1012
Kow, Hasan, Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis, J. Med. Virol, doi:10.1002/jmv.26498
Kuba, Imai, Rao, Gao, Guo et al., A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury, Nat. Med, doi:10.1038/nm1267
Lee, Jun, Anti, Inflammatory Effects of GLP-1-Based Therapies beyond Glucose Control, Mediat. Inflamm, doi:10.1155/2016/3094642
Li, Wei, Li, Mccowen, Xiong et al., Metformin Use in Diabetes Prior to Hospitalization: Effects on Mortality in COVID-19, Endocr. Pract, doi:10.4158/EP-2020-0466
Lima-Martínez, Paoli, Rodney, Balladares, Contreras et al., Effect of sitagliptin on epicardial fat thickness in subjects with type 2 diabetes and obesity: A pilot study, Endocrine, doi:10.1007/s12020-015-0710-y
Lontchi-Yimagou, Sobngwi, Matsha, Kengne, None, Diabetes Mellitus and Inflammation. Curr. Diabetes Rep, doi:10.1007/s11892-013-0375-y
Lu, Zhao, Li, Niu, Yang et al., Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding, Lancet, doi:10.1016/S0140-6736(20)30251-8
Ma, Liu, Ilyas, Little, Kamato et al., GLP-1 receptor agonists (GLP-1RAs): Cardiovascular actions and therapeutic potential, Int. J. Biol. Sci, doi:10.7150/ijbs.59965
Martin, Deacon, Gorrell, Prins, Incretin-based therapies-Review of the physiology, pharmacology and emerging clinical experience, Intern. Med. J, doi:10.1111/j.1445-5994.2011.02439.x
Mirabelli, Chiefari, Puccio, Foti, Brunetti, Potential Benefits and Harms of Novel Antidiabetic Drugs During COVID-19 Crisis, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph17103664
Mirani, Favacchio, Carrone, Betella, Biamonte et al., Impact of Comorbidities and Glycemia at Admission and Dipeptidyl Peptidase 4 Inhibitors in Patients with Type 2 Diabetes with COVID-19: A Case Series from an Academic Hospital, Diabetes Care, doi:10.2337/dc20-1340
Monda, Porcellati, Strollo, Gentile, ACE2 and SARS-CoV-2 Infection: Might GLP-1 Receptor Agonists Play a Role? Diabetes Ther, doi:10.1007/s13300-020-00898-8
Nguyen, Ho, Nguyen, Ho, Li et al., Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis, Metabolism
Nyland, Raja-Khan, Bettermann, Haouzi, Leslie et al., Grigson, P.S. Diabetes, Drug Treatment, and Mortality in COVID-19: A Multinational Retrospective Cohort Study, doi:10.2337/db21-0385
Packer, Do sodium-glucose co-transporter-2 inhibitors prevent heart failure with a preserved ejection fraction by counterbalancing the effects of leptin? A novel hypothesis, Diabetes Obes. Metab, doi:10.1111/dom.13229
Pai, Lo, Hsu, Peng, Wang, Angiotensin-(1-7) Inhibits Thrombin-Induced Endothelial Phenotypic Changes and Reactive Oxygen Species Production via NADPH Oxidase 5 Downregulation, Front. Physiol, doi:10.3389/fphys.2017.00994
Pal, Banerjee, Mukherjee, Bhogal, Kaur et al., Dipeptidyl peptidase-4 inhibitor use and mortality in COVID-19 patients with diabetes mellitus: An updated systematic review and meta-analysis. Ther, Adv. Endocrinol. Metab, doi:10.1177/2042018821996482
Pal, Bhansali, COVID-19, diabetes mellitus and ACE2: The conundrum, Diabetes Res. Clin. Pract, doi:10.1016/j.diabres.2020.108132
Panchapakesan, Pegg, Gross, Komala, Mudaliar et al., Effects of SGLT2 Inhibition in Human Kidney Proximal Tubular Cells-Renoprotection in Diabetic Nephropathy?, PLoS ONE, doi:10.1371/journal.pone.0054442
Parker, Reimann, Gribble, Molecular mechanisms underlying nutrient-stimulated incretin secretion, Expert Rev. Mol. Med, doi:10.1017/S146239940900132X
Pérez-Belmonte, Torres-Peña, López-Carmona, Ayala-Gutiérrez, Fuentes-Jiménez et al., Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: A nationwide cohort study, BMC Med, doi:10.1186/s12916-020-01832-2
Raj, Mou, Smits, Dekkers, Müller et al., Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC, Nature, doi:10.1038/nature12005
Rakhmat, Kusmala, Handayani, Juliastuti, Nawangsih et al., Dipeptidyl peptidase-4 (DPP-4) inhibitor and mortality in coronavirus disease 2019 (COVID-19)-A systematic review, meta-analysis, and meta-regression, Diabetes Metab. Syndr. Clin. Res. Rev. 2021, doi:10.1016/j.dsx.2021.03.027
Rhee, Lee, Nam, Kyoung, Shin et al., Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19, Diabetes Metab. J, doi:10.4093/dmj.2020.0206
Romaní-Pérez, Outeiriño-Iglesias, Moya, Santisteban, González-Matías et al., Activation of the GLP-1 Receptor by Liraglutide Increases ACE2 Expression, Reversing Right Ventricle Hypertrophy, and Improving the Production of SP-A and SP-B in the Lungs of Type 1 Diabetes Rats, Endocrinology, doi:10.1210/en.2014-1685
Roussel, Darmon, Pichelin, Goronflot, Abouleka et al., Use of dipeptidyl peptidase-4 inhibitors and prognosis of COVID-19 in hospitalized patients with type 2 diabetes: A propensity score analysis from the CORONADO study, Diabetes Obes. Metab, doi:10.1111/dom.14324
Rowlands, Heng, Newsholme, Carlessi, Pleiotropic Effects of GLP-1 and Analogs on Cell Signaling, Metabolism, and Function. Front. Endocrinol, doi:10.3389/fendo.2018.00672
Scheen, Metformin and COVID-19: From cellular mechanisms to reduced mortality, Diabetes Metab, doi:10.1016/j.diabet.2020.07.006
Shajahan, Pepi, Rouhani, Heiss, Azadi, Glycosylation of SARS-CoV-2: Structural and functional insights, Anal. Bioanal. Chem, doi:10.1007/s00216-021-03499-x
Shukla, Banerjee, Angiotensin-Converting-Enzyme 2 and Renin-Angiotensin System Inhibitors in COVID-19: An Update, doi:10.1007/s40292-021-00439-9
Solerte, Di Sabatino, Galli, Fiorina, Dipeptidyl peptidase-4 (DPP4) inhibition in COVID-19, Acta Diabetol, doi:10.1007/s00592-020-01539-z
Solerte, Trevisan, Lovati, Rossi, Pastore et al., Sitagliptin Treatment at the Time of Hospitalization Was Associated with Reduced Mortality in Patients with Type 2 Diabetes and COVID-19: A Multicenter, Case-Control, Retrospective, Observational Study, Diabetes Care, doi:10.2337/dc20-1521
Vallon, Gerasimova, Rose, Masuda, Satriano et al., SGLT2 inhibitor empagliflozin reduces renal growth and albuminuria in proportion to hyperglycemia and prevents glomerular hyperfiltration in diabetic Akita mice, Am. J. Physiol. Physiol, doi:10.1152/ajprenal.00520.2013
Verdecchia, Cavallini, Spanevello, Angeli, The pivotal link between ACE2 deficiency and SARS-CoV-2 infection, Eur. J. Intern. Med, doi:10.1016/j.ejim.2020.04.037
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Xu, Nagata, Nagashimada, Zhuge, Ni et al., SGLT2 Inhibition by Empagliflozin Promotes Fat Utilization and Browning and Attenuates Inflammation and Insulin Resistance by Polarizing M2 Macrophages in Diet-induced Obese Mice, doi:10.1016/j.ebiom.2017.05.028
Xu, Ota, Emerging roles of SGLT2 inhibitors in obesity and insulin resistance: Focus on fat browning and macrophage polarization, doi:10.1080/21623945.2017.1413516
Zein, Raffaello, Dipeptidyl peptidase-4 (DPP-IV) inhibitor was associated with mortality reduction in COVID-19-A systematic review and meta-analysis, Prim. Care Diabetes, doi:10.1016/j.pcd.2021.12.008
DOI record:
{
"DOI": "10.3390/biomedicines11082292",
"ISSN": [
"2227-9059"
],
"URL": "http://dx.doi.org/10.3390/biomedicines11082292",
"abstract": "<jats:p>Novel antidiabetic drugs have the ability to produce anti-inflammatory effects regardless of their glucose-lowering action. For this reason, these molecules (including GLP-1 RAs and DPP-4is) were hypothesized to be effective against COVID-19, which is characterized by cytokines hyperactivity and multiorgan inflammation. The aim of our work is to explore the potential protective role of GLP-1 RAs and DPP-4is in COVID-19 (with the disease intended to be a model of an acute stressor) and non-COVID-19 patients over a two-year observation period. Retrospective and one-versus-one analyses were conducted to assess the impact of antidiabetic drugs on the need for hospitalization (in both COVID-19- and non-COVID-19-related cases), in-hospital mortality, and two-year mortality. Logistic regression analyses were conducted to identify the variables associated with these outcomes. Additionally, log-rank tests were used to plot survival curves for each group of subjects, based on their antidiabetic treatment. The performed analyses revealed that despite similar hospitalization rates, subjects undergoing home therapy with GLP-1 RAs exhibited significantly lower mortality rates, even over a two-year period. These individuals demonstrated improved survival estimates both within hospital and non-hospital settings, even during a longer observation period.</jats:p>",
"alternative-id": [
"biomedicines11082292"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-7334-0135",
"affiliation": [
{
"name": "Department of Translational Medicine, University of Ferrara, Via Luigi Borsari, 46, I-44121 Ferrara, FE, Italy"
},
{
"name": "Department of Internal Medicine, Ospedale del Delta, Via Valle Oppio, 2, I-44023 Lagosanto, FE, Italy"
}
],
"authenticated-orcid": false,
"family": "Greco",
"given": "Salvatore",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Primary Care Department, Diabetes Unit of “SS. Annunziata” Hospital, Via Giovanni Vicini 2, I-44042 Cento, FE, Italy"
}
],
"family": "Monda",
"given": "Vincenzo M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Research and Innovation Section, University Hospital of Ferrara Arcispedale Sant’Anna, Via Aldo Moro 8, I-44124 Cona, FE, Italy"
}
],
"family": "Valpiani",
"given": "Giorgia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Programming and Management Control Unit, University Hospital of Ferrara Arcispedale Sant’Anna, Via Aldo Moro 8, I-44124 Cona, FE, Italy"
}
],
"family": "Napoli",
"given": "Nicola",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Pharmaceutical Department, University Hospital of Ferrara Arcispedale Sant’Anna, Via Aldo Moro 8, I-44124 Cona, FE, Italy"
}
],
"family": "Crespini",
"given": "Carlo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Pharmaceutical Care Department, Azienda Unità Sanitaria Locale della Romagna, Via Carlo Forlanini 34, I-47121 Forlì, FC, Italy"
}
],
"family": "Pieraccini",
"given": "Fabio",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Pharmaceutical Department, University Hospital of Ferrara Arcispedale Sant’Anna, Via Aldo Moro 8, I-44124 Cona, FE, Italy"
}
],
"family": "Marra",
"given": "Anna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Translational Medicine, University of Ferrara, Via Luigi Borsari, 46, I-44121 Ferrara, FE, Italy"
},
{
"name": "Research and Innovation Section, University Hospital of Ferrara Arcispedale Sant’Anna, Via Aldo Moro 8, I-44124 Cona, FE, Italy"
},
{
"name": "Department of Internal Medicine, University Hospital of Ferrara Arcispedale Sant’Anna, Via Aldo Moro 8, I-44124 Cona, FE, Italy"
}
],
"family": "Passaro",
"given": "Angelina",
"sequence": "additional"
}
],
"container-title": "Biomedicines",
"container-title-short": "Biomedicines",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
8,
18
]
],
"date-time": "2023-08-18T14:14:38Z",
"timestamp": 1692368078000
},
"deposited": {
"date-parts": [
[
2023,
8,
18
]
],
"date-time": "2023-08-18T15:11:02Z",
"timestamp": 1692371462000
},
"indexed": {
"date-parts": [
[
2023,
8,
19
]
],
"date-time": "2023-08-19T04:54:12Z",
"timestamp": 1692420852537
},
"is-referenced-by-count": 0,
"issue": "8",
"issued": {
"date-parts": [
[
2023,
8,
18
]
]
},
"journal-issue": {
"issue": "8",
"published-online": {
"date-parts": [
[
2023,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
8,
18
]
],
"date-time": "2023-08-18T00:00:00Z",
"timestamp": 1692316800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2227-9059/11/8/2292/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "2292",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
8,
18
]
]
},
"published-online": {
"date-parts": [
[
2023,
8,
18
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1177/2047487319878371",
"article-title": "Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications",
"author": "Ceriello",
"doi-asserted-by": "publisher",
"first-page": "25",
"journal-title": "Eur. J. Prev. Cardiol.",
"key": "ref_1",
"volume": "26",
"year": "2019"
},
{
"DOI": "10.1093/cid/ciaa1012",
"article-title": "Risk Factors for Intensive Care Unit Admission and In-hospital Mortality Among Hospitalized Adults Identified through the US Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET)",
"author": "Kim",
"doi-asserted-by": "publisher",
"first-page": "e206",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_2",
"volume": "72",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"article-title": "Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: A population-based cohort study",
"author": "Holman",
"doi-asserted-by": "publisher",
"first-page": "823",
"journal-title": "Lancet Diabetes Endocrinol.",
"key": "ref_3",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.2337/dbi20-0032",
"article-title": "COVID-19 and Diabetes: A Collision and Collusion of Two Diseases",
"author": "Feldman",
"doi-asserted-by": "publisher",
"first-page": "2549",
"journal-title": "Diabetes",
"key": "ref_4",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.3389/fendo.2021.609470",
"article-title": "Type 2 Diabetes Mellitus and COVID-19: A Narrative Review",
"author": "Corrao",
"doi-asserted-by": "publisher",
"first-page": "609470",
"journal-title": "Front. Endocrinol.",
"key": "ref_5",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"article-title": "Factors associated with COVID-19-related death using OpenSAFELY",
"author": "Williamson",
"doi-asserted-by": "publisher",
"first-page": "430",
"journal-title": "Nature",
"key": "ref_6",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1007/s00592-020-01539-z",
"article-title": "Dipeptidyl peptidase-4 (DPP4) inhibition in COVID-19",
"author": "Solerte",
"doi-asserted-by": "publisher",
"first-page": "779",
"journal-title": "Acta Diabetol.",
"key": "ref_7",
"volume": "57",
"year": "2020"
},
{
"DOI": "10.3390/ijerph17103664",
"doi-asserted-by": "crossref",
"key": "ref_8",
"unstructured": "Mirabelli, M., Chiefari, E., Puccio, L., Foti, D.P., and Brunetti, A. (2020). Potential Benefits and Harms of Novel Antidiabetic Drugs During COVID-19 Crisis. Int. J. Environ. Res. Public Health, 17."
},
{
"DOI": "10.1007/s13300-020-00898-8",
"article-title": "ACE2 and SARS-CoV-2 Infection: Might GLP-1 Receptor Agonists Play a Role?",
"author": "Monda",
"doi-asserted-by": "publisher",
"first-page": "1909",
"journal-title": "Diabetes Ther.",
"key": "ref_9",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30251-8",
"article-title": "Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding",
"author": "Lu",
"doi-asserted-by": "publisher",
"first-page": "565",
"journal-title": "Lancet",
"key": "ref_10",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1038/nm1267",
"article-title": "A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus–induced lung injury",
"author": "Kuba",
"doi-asserted-by": "publisher",
"first-page": "875",
"journal-title": "Nat. Med.",
"key": "ref_11",
"volume": "11",
"year": "2005"
},
{
"DOI": "10.1038/nature12005",
"article-title": "Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC",
"author": "Raj",
"doi-asserted-by": "publisher",
"first-page": "251",
"journal-title": "Nature",
"key": "ref_12",
"volume": "495",
"year": "2013"
},
{
"DOI": "10.1017/S146239940900132X",
"article-title": "Molecular mechanisms underlying nutrient-stimulated incretin secretion",
"author": "Parker",
"doi-asserted-by": "publisher",
"first-page": "e1",
"journal-title": "Expert Rev. Mol. Med.",
"key": "ref_13",
"volume": "12",
"year": "2010"
},
{
"DOI": "10.3389/fendo.2018.00672",
"article-title": "Pleiotropic Effects of GLP-1 and Analogs on Cell Signaling, Metabolism, and Function",
"author": "Rowlands",
"doi-asserted-by": "publisher",
"first-page": "672",
"journal-title": "Front. Endocrinol.",
"key": "ref_14",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1155/2016/3094642",
"article-title": "Anti-Inflammatory Effects of GLP-1-Based Therapies beyond Glucose Control",
"author": "Lee",
"doi-asserted-by": "publisher",
"first-page": "3094642",
"journal-title": "Mediat. Inflamm.",
"key": "ref_15",
"volume": "2016",
"year": "2016"
},
{
"DOI": "10.1007/s11892-013-0375-y",
"article-title": "Diabetes Mellitus and Inflammation",
"author": "Sobngwi",
"doi-asserted-by": "publisher",
"first-page": "435",
"journal-title": "Curr. Diabetes Rep.",
"key": "ref_16",
"volume": "13",
"year": "2013"
},
{
"DOI": "10.1111/j.1445-5994.2011.02439.x",
"article-title": "Incretin-based therapies—Review of the physiology, pharmacology and emerging clinical experience",
"author": "Martin",
"doi-asserted-by": "publisher",
"first-page": "299",
"journal-title": "Intern. Med. J.",
"key": "ref_17",
"volume": "41",
"year": "2011"
},
{
"DOI": "10.1080/14656566.2018.1552258",
"article-title": "Oral semaglutide for the treatment of type 2 diabetes",
"author": "Hedrington",
"doi-asserted-by": "publisher",
"first-page": "133",
"journal-title": "Expert Opin. Pharmacother.",
"key": "ref_18",
"volume": "20",
"year": "2019"
},
{
"DOI": "10.1210/jendso/bvz042",
"article-title": "Effects of Semaglutide Versus Dulaglutide on Epicardial Fat Thickness in Subjects with Type 2 Diabetes and Obesity",
"author": "Iacobellis",
"doi-asserted-by": "publisher",
"first-page": "bvz042",
"journal-title": "J. Endocr. Soc.",
"key": "ref_19",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1007/s12020-015-0710-y",
"article-title": "Effect of sitagliptin on epicardial fat thickness in subjects with type 2 diabetes and obesity: A pilot study",
"author": "Paoli",
"doi-asserted-by": "publisher",
"first-page": "448",
"journal-title": "Endocrine",
"key": "ref_20",
"volume": "51",
"year": "2016"
},
{
"DOI": "10.7150/ijbs.59965",
"article-title": "GLP-1 receptor agonists (GLP-1RAs): Cardiovascular actions and therapeutic potential",
"author": "Ma",
"doi-asserted-by": "publisher",
"first-page": "2050",
"journal-title": "Int. J. Biol. Sci.",
"key": "ref_21",
"volume": "17",
"year": "2021"
},
{
"DOI": "10.1089/met.2017.0057",
"article-title": "Mast Cell and M1 Macrophage Infiltration and Local Pro-Inflammatory Factors Were Attenuated with Incretin-Based Therapies in Obesity-Related Glomerulopathy",
"author": "He",
"doi-asserted-by": "publisher",
"first-page": "344",
"journal-title": "Metab. Syndr. Relat. Disord.",
"key": "ref_22",
"volume": "15",
"year": "2017"
},
{
"DOI": "10.2337/dc20-1521",
"article-title": "Sitagliptin Treatment at the Time of Hospitalization Was Associated with Reduced Mortality in Patients with Type 2 Diabetes and COVID-19: A Multicenter, Case-Control, Retrospective, Observational Study",
"author": "Solerte",
"doi-asserted-by": "publisher",
"first-page": "2999",
"journal-title": "Diabetes Care",
"key": "ref_23",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1016/j.pcd.2021.12.008",
"article-title": "Dipeptidyl peptidase-4 (DPP-IV) inhibitor was associated with mortality reduction in COVID-19—A systematic review and meta-analysis",
"author": "Zein",
"doi-asserted-by": "publisher",
"first-page": "162",
"journal-title": "Prim. Care Diabetes",
"key": "ref_24",
"volume": "16",
"year": "2022"
},
{
"DOI": "10.1210/en.2014-1685",
"article-title": "Activation of the GLP-1 Receptor by Liraglutide Increases ACE2 Expression, Reversing Right Ventricle Hypertrophy, and Improving the Production of SP-A and SP-B in the Lungs of Type 1 Diabetes Rats",
"author": "Moya",
"doi-asserted-by": "publisher",
"first-page": "3559",
"journal-title": "Endocrinology",
"key": "ref_25",
"volume": "156",
"year": "2015"
},
{
"DOI": "10.1016/j.diabres.2020.108132",
"article-title": "COVID-19, diabetes mellitus and ACE2: The conundrum",
"author": "Pal",
"doi-asserted-by": "publisher",
"first-page": "108132",
"journal-title": "Diabetes Res. Clin. Pract.",
"key": "ref_26",
"volume": "162",
"year": "2020"
},
{
"DOI": "10.1136/openhrt-2020-001424",
"article-title": "Manipulation of ACE2 expression in COVID-19",
"author": "Chaudhry",
"doi-asserted-by": "publisher",
"first-page": "e001424",
"journal-title": "Open Heart",
"key": "ref_27",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1007/s00216-021-03499-x",
"article-title": "Glycosylation of SARS-CoV-2: Structural and functional insights",
"author": "Shajahan",
"doi-asserted-by": "publisher",
"first-page": "7179",
"journal-title": "Anal. Bioanal. Chem.",
"key": "ref_28",
"volume": "413",
"year": "2021"
},
{
"DOI": "10.3389/fphys.2017.00994",
"article-title": "Angiotensin-(1-7) Inhibits Thrombin-Induced Endothelial Phenotypic Changes and Reactive Oxygen Species Production via NADPH Oxidase 5 Downregulation",
"author": "Pai",
"doi-asserted-by": "publisher",
"first-page": "994",
"journal-title": "Front. Physiol.",
"key": "ref_29",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.1590/S1807-59322011000500021",
"article-title": "An orally active formulation of angiotensin-(1-7) produces an antithrombotic effect",
"author": "Alenina",
"doi-asserted-by": "publisher",
"first-page": "837",
"journal-title": "Clinics",
"key": "ref_30",
"volume": "66",
"year": "2011"
},
{
"DOI": "10.1182/blood-2012-09-459156",
"article-title": "Angiotensin 1-7 and Mas decrease thrombosis in Bdkrb2−/− mice by increasing NO and prostacyclin to reduce platelet spreading and glycoprotein VI activation",
"author": "Fang",
"doi-asserted-by": "publisher",
"first-page": "3023",
"journal-title": "Blood",
"key": "ref_31",
"volume": "121",
"year": "2013"
},
{
"DOI": "10.1007/s11239-020-02134-3",
"article-title": "COVID-19 update: COVID-19-associated coagulopathy",
"author": "Becker",
"doi-asserted-by": "publisher",
"first-page": "54",
"journal-title": "J. Thromb. Thrombolysis",
"key": "ref_32",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1016/j.ejim.2020.04.037",
"article-title": "The pivotal link between ACE2 deficiency and SARS-CoV-2 infection",
"author": "Verdecchia",
"doi-asserted-by": "publisher",
"first-page": "14",
"journal-title": "Eur. J. Intern. Med.",
"key": "ref_33",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1007/s12185-020-03029-y",
"article-title": "COVID-19-associated coagulopathy and disseminated intravascular coagulation",
"author": "Asakura",
"doi-asserted-by": "publisher",
"first-page": "45",
"journal-title": "Int. J. Hematol.",
"key": "ref_34",
"volume": "113",
"year": "2021"
},
{
"DOI": "10.1007/s00134-020-06062-x",
"article-title": "High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study",
"author": "Helms",
"doi-asserted-by": "publisher",
"first-page": "1089",
"journal-title": "Intensive Care Med.",
"key": "ref_35",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1007/s40292-021-00439-9",
"article-title": "Angiotensin-Converting-Enzyme 2 and Renin-Angiotensin System Inhibitors in COVID-19: An Update",
"author": "Shukla",
"doi-asserted-by": "publisher",
"first-page": "129",
"journal-title": "High Blood Press. Cardiovasc. Prev.",
"key": "ref_36",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.2337/dc21-0065",
"article-title": "Association Between Glucagon-Like Peptide 1 Receptor Agonist and Sodium–Glucose Cotransporter 2 Inhibitor Use and COVID-19 Outcomes",
"author": "Kahkoska",
"doi-asserted-by": "publisher",
"first-page": "1564",
"journal-title": "Diabetes Care",
"key": "ref_37",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1111/dom.14329",
"article-title": "Comparable COVID-19 outcomes with current use of GLP-1 receptor agonists, DPP-4 inhibitors or SGLT-2 inhibitors among patients with diabetes who tested positive for SARS-CoV-2",
"author": "Israelsen",
"doi-asserted-by": "publisher",
"first-page": "1397",
"journal-title": "Diabetes Obes. Metab.",
"key": "ref_38",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"article-title": "Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: A nationwide observational study in England",
"author": "Khunti",
"doi-asserted-by": "publisher",
"first-page": "293",
"journal-title": "Lancet Diabetes Endocrinol.",
"key": "ref_39",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.diabres.2021.109031",
"article-title": "Pre-admission glucagon-like peptide-1 receptor agonist (GLP-1RA) and mortality from coronavirus disease 2019 (COVID-19): A systematic review, meta-analysis, and meta-regression",
"author": "Hariyanto",
"doi-asserted-by": "publisher",
"first-page": "109031",
"journal-title": "Diabetes Res. Clin. Pract.",
"key": "ref_40",
"volume": "179",
"year": "2021"
},
{
"DOI": "10.1016/j.metabol.2022.155196",
"article-title": "Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis",
"author": "Nguyen",
"doi-asserted-by": "publisher",
"first-page": "155196",
"journal-title": "Metabolism",
"key": "ref_41",
"volume": "131",
"year": "2022"
},
{
"DOI": "10.3389/fendo.2022.895458",
"article-title": "The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients with Diabetes: A Bayesian Network Meta-Analysis",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "895458",
"journal-title": "Front. Endocrinol.",
"key": "ref_42",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1111/dom.14324",
"article-title": "Use of dipeptidyl peptidase-4 inhibitors and prognosis of COVID-19 in hospitalized patients with type 2 diabetes: A propensity score analysis from the CORONADO study",
"author": "Roussel",
"doi-asserted-by": "publisher",
"first-page": "1162",
"journal-title": "Diabetes Obes. Metab.",
"key": "ref_43",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1186/s12916-020-01832-2",
"doi-asserted-by": "crossref",
"key": "ref_44",
"unstructured": "Pérez-Belmonte, L.M., Torres-Peña, J.D., López-Carmona, M.D., Ayala-Gutiérrez, M.M., Fuentes-Jiménez, F., Huerta, L.J., Muñoz, J.A., Rubio-Rivas, M., Madrazo, M., and Garcia, M.G. (2020). Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: A nationwide cohort study. BMC Med., 18."
},
{
"DOI": "10.4093/dmj.2020.0206",
"article-title": "Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19",
"author": "Rhee",
"doi-asserted-by": "publisher",
"first-page": "251",
"journal-title": "Diabetes Metab. J.",
"key": "ref_45",
"volume": "45",
"year": "2021"
},
{
"DOI": "10.2337/dc20-1340",
"article-title": "Impact of Comorbidities and Glycemia at Admission and Dipeptidyl Peptidase 4 Inhibitors in Patients with Type 2 Diabetes with COVID-19: A Case Series from an Academic Hospital in Lombardy, Italy",
"author": "Mirani",
"doi-asserted-by": "publisher",
"first-page": "3042",
"journal-title": "Diabetes Care",
"key": "ref_46",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1007/s40200-021-00777-4",
"article-title": "Dipeptidyl peptidase 4 (DPP4) inhibitor and outcome from coronavirus disease 2019 (COVID-19) in diabetic patients: A systematic review, meta-analysis, and meta-regression",
"author": "Hariyanto",
"doi-asserted-by": "publisher",
"first-page": "543",
"journal-title": "J. Diabetes Metab. Disord.",
"key": "ref_47",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.2337/db21-0385",
"article-title": "Diabetes, Drug Treatment, and Mortality in COVID-19: A Multinational Retrospective Cohort Study",
"author": "Nyland",
"doi-asserted-by": "publisher",
"first-page": "2903",
"journal-title": "Diabetes",
"key": "ref_48",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2021.03.027",
"article-title": "Dipeptidyl peptidase-4 (DPP-4) inhibitor and mortality in coronavirus disease 2019 (COVID-19)—A systematic review, meta-analysis, and meta-regression",
"author": "Rakhmat",
"doi-asserted-by": "publisher",
"first-page": "777",
"journal-title": "Diabetes Metab. Syndr. Clin. Res. Rev.",
"key": "ref_49",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1177/2042018821996482",
"article-title": "Dipeptidyl peptidase-4 inhibitor use and mortality in COVID-19 patients with diabetes mellitus: An updated systematic review and meta-analysis",
"author": "Pal",
"doi-asserted-by": "publisher",
"first-page": "204201882199648",
"journal-title": "Ther. Adv. Endocrinol. Metab.",
"key": "ref_50",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1007/s40618-021-01515-6",
"article-title": "Disentangling conflicting evidence on DPP-4 inhibitors and outcomes of COVID-19: Narrative review and meta-analysis",
"author": "Bonora",
"doi-asserted-by": "publisher",
"first-page": "1379",
"journal-title": "J. Endocrinol. Investig.",
"key": "ref_51",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0054442",
"doi-asserted-by": "crossref",
"key": "ref_52",
"unstructured": "Panchapakesan, U., Pegg, K., Gross, S., Komala, M.G., Mudaliar, H., Forbes, J., Pollock, C., and Mather, A. (2013). Effects of SGLT2 Inhibition in Human Kidney Proximal Tubular Cells—Renoprotection in Diabetic Nephropathy?. PLoS ONE, 8."
},
{
"DOI": "10.1016/j.diabet.2018.09.005",
"article-title": "Effects of SGLT2 inhibitors on systemic and tissue low-grade inflammation: The potential contribution to diabetes complications and cardiovascular disease",
"author": "Bonnet",
"doi-asserted-by": "publisher",
"first-page": "457",
"journal-title": "Diabetes Metab.",
"key": "ref_53",
"volume": "44",
"year": "2018"
},
{
"DOI": "10.1152/ajprenal.00520.2013",
"article-title": "SGLT2 inhibitor empagliflozin reduces renal growth and albuminuria in proportion to hyperglycemia and prevents glomerular hyperfiltration in diabetic Akita mice",
"author": "Vallon",
"doi-asserted-by": "publisher",
"first-page": "F194",
"journal-title": "Am. J. Physiol. Physiol.",
"key": "ref_54",
"volume": "306",
"year": "2014"
},
{
"DOI": "10.1007/s00018-022-04289-z",
"article-title": "Anti-inflammatory effect of SGLT-2 inhibitors via uric acid and insulin",
"author": "Olivieri",
"doi-asserted-by": "publisher",
"first-page": "273",
"journal-title": "Cell. Mol. Life Sci.",
"key": "ref_55",
"volume": "79",
"year": "2022"
},
{
"DOI": "10.1016/j.metabol.2018.02.002",
"article-title": "Effects of canagliflozin versus glimepiride on adipokines and inflammatory biomarkers in type 2 diabetes",
"author": "Garvey",
"doi-asserted-by": "publisher",
"first-page": "32",
"journal-title": "Metabolism",
"key": "ref_56",
"volume": "85",
"year": "2018"
},
{
"DOI": "10.1111/dom.13229",
"article-title": "Do sodium-glucose co-transporter-2 inhibitors prevent heart failure with a preserved ejection fraction by counterbalancing the effects of leptin? A novel hypothesis",
"author": "Packer",
"doi-asserted-by": "publisher",
"first-page": "1361",
"journal-title": "Diabetes Obes. Metab.",
"key": "ref_57",
"volume": "20",
"year": "2018"
},
{
"DOI": "10.1016/j.biopha.2021.112169",
"article-title": "Effects of SGLT2 Inhibitors on Ion Homeostasis and Oxidative Stress associated Mechanisms in Heart Failure",
"author": "Gager",
"doi-asserted-by": "publisher",
"first-page": "112169",
"journal-title": "Biomed. Pharmacother.",
"key": "ref_58",
"volume": "143",
"year": "2021"
},
{
"DOI": "10.1016/j.ebiom.2017.05.028",
"article-title": "SGLT2 Inhibition by Empagliflozin Promotes Fat Utilization and Browning and Attenuates Inflammation and Insulin Resistance by Polarizing M2 Macrophages in Diet-induced Obese Mice",
"author": "Xu",
"doi-asserted-by": "publisher",
"first-page": "137",
"journal-title": "Ebiomedicine",
"key": "ref_59",
"volume": "20",
"year": "2017"
},
{
"DOI": "10.1080/21623945.2017.1413516",
"article-title": "Emerging roles of SGLT2 inhibitors in obesity and insulin resistance: Focus on fat browning and macrophage polarization",
"author": "Xu",
"doi-asserted-by": "publisher",
"first-page": "121",
"journal-title": "Adipocyte",
"key": "ref_60",
"volume": "7",
"year": "2017"
},
{
"DOI": "10.1007/s13300-021-01110-1",
"article-title": "Risk Factors Associated with COVID-19 Hospitalization and Mortality: A Large Claims-Based Analysis Among People with Type 2 Diabetes Mellitus in the United States",
"author": "Boye",
"doi-asserted-by": "publisher",
"first-page": "2223",
"journal-title": "Diabetes Ther.",
"key": "ref_61",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.3389/fendo.2021.708494",
"article-title": "Mortality Risk of Antidiabetic Agents for Type 2 Diabetes with COVID-19: A Systematic Review and Meta-Analysis",
"author": "Kan",
"doi-asserted-by": "publisher",
"first-page": "708494",
"journal-title": "Front. Endocrinol.",
"key": "ref_62",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1002/jmv.26498",
"article-title": "Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis",
"author": "Kow",
"doi-asserted-by": "publisher",
"first-page": "695",
"journal-title": "J. Med. Virol.",
"key": "ref_63",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.4158/EP-2020-0466",
"article-title": "Metformin Use in Diabetes Prior to Hospitalization: Effects on Mortality in COVID-19",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "1166",
"journal-title": "Endocr. Pract.",
"key": "ref_64",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2021.02.022",
"article-title": "Metformin is associated with lower hospitalizations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA",
"author": "Ghany",
"doi-asserted-by": "publisher",
"first-page": "513",
"journal-title": "Diabetes Metab. Syndr. Clin. Res. Rev.",
"key": "ref_65",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1016/j.diabet.2020.07.006",
"article-title": "Metformin and COVID-19: From cellular mechanisms to reduced mortality",
"author": "Scheen",
"doi-asserted-by": "publisher",
"first-page": "423",
"journal-title": "Diabetes Metab.",
"key": "ref_66",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/S2666-7568(20)30033-7",
"article-title": "Metformin and risk of mortality in patients hospitalised with COVID-19: A retrospective cohort analysis",
"author": "Bramante",
"doi-asserted-by": "publisher",
"first-page": "e34",
"journal-title": "Lancet Healthy Longev.",
"key": "ref_67",
"volume": "2",
"year": "2021"
}
],
"reference-count": 67,
"references-count": 67,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2227-9059/11/8/2292"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Biochemistry, Genetics and Molecular Biology",
"Medicine (miscellaneous)"
],
"subtitle": [],
"title": "The Impact of GLP-1 RAs and DPP-4is on Hospitalisation and Mortality in the COVID-19 Era: A Two-Year Observational Study",
"type": "journal-article",
"volume": "11"
}
