Incidence of COVID-19 Hospitalisation in Patients with Systemic Lupus Erythematosus: A Nationwide Cohort Study from Denmark
et al., Journal of Clinical Medicine, doi:10.3390/jcm10173842, Aug 2021
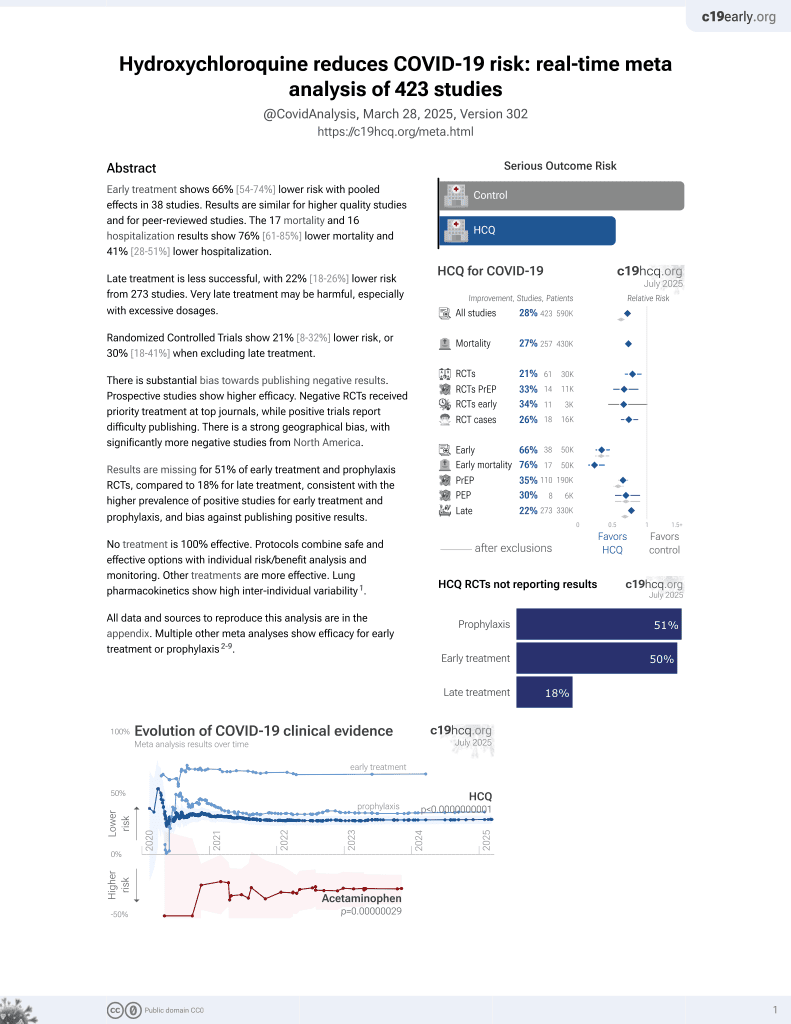
HCQ for COVID-19
1st treatment shown to reduce risk in
March 2020, now with p < 0.00000000001 from 424 studies, used in 59 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 2,533 SLE patients in Denmark showing no significant difference in hospitalization risk for COVID-19 cases with HCQ treatment.
|
risk of hospitalization, 40.0% lower, HR 0.60, p = 0.39, treatment 1,170, control 1,363, adjusted per study.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Cordtz et al., 27 Aug 2021, retrospective, population-based cohort, Denmark, peer-reviewed, 8 authors, study period 1 March, 2020 - 2 February, 2021.
Incidence of COVID-19 Hospitalisation in Patients with Systemic Lupus Erythematosus: A Nationwide Cohort Study from Denmark
Journal of Clinical Medicine, doi:10.3390/jcm10173842
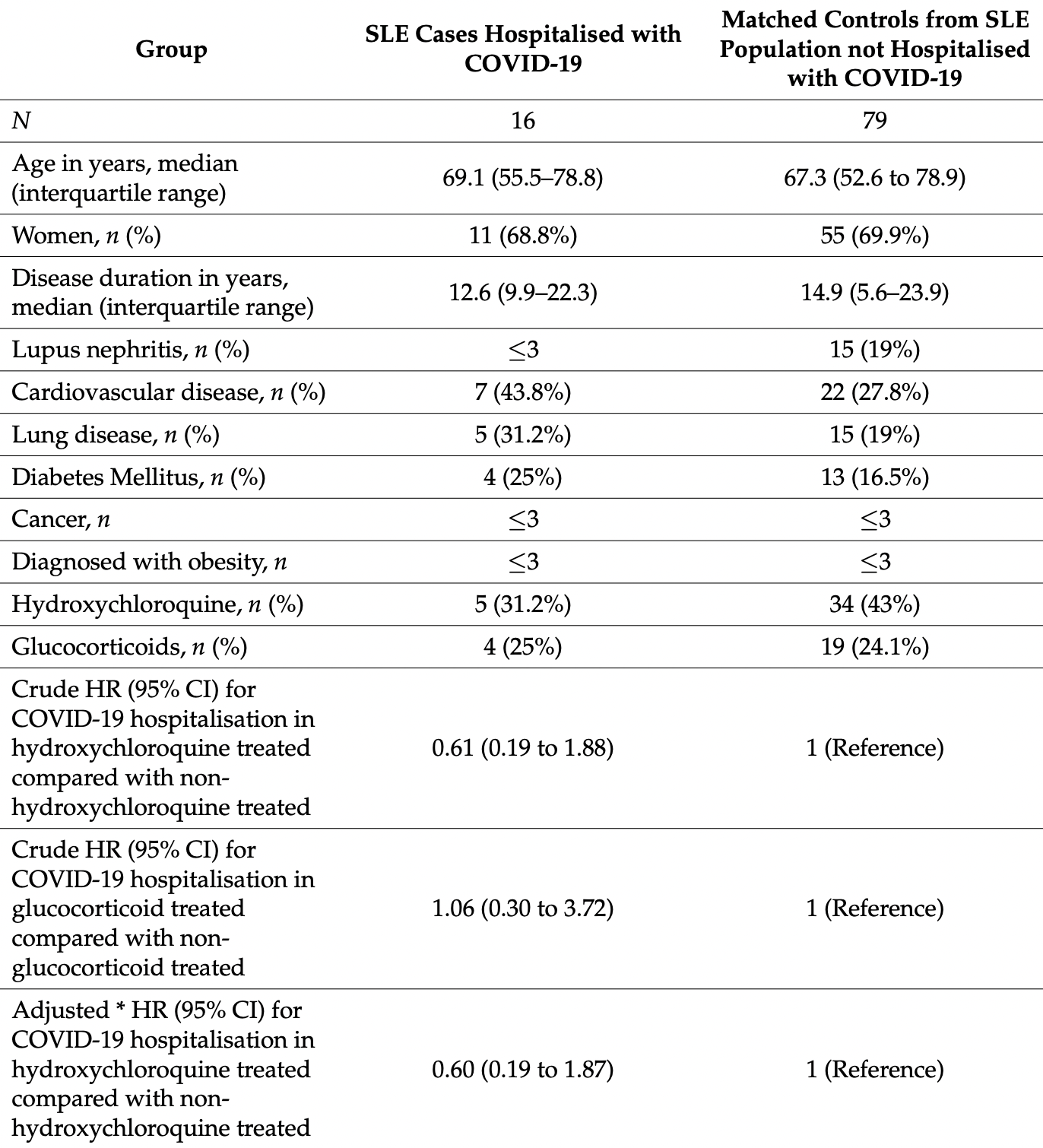
Background: Patients with systemic lupus erythematosus (SLE) have an increased risk of infections due to impaired immune functions, disease activity, and treatment. This study investigated the impact of having SLE on the incidence of hospitalisation with COVID-19 infection. Methods: This was a nationwide cohort study from Denmark between 1 March 2020 to 2 February 2021, based on the linkage of several nationwide registers. The adjusted incidence of COVID-19 hospitalisation was estimated for patients with SLE compared with the general population in Cox-regression models. Among SLE patients, the hazard ratio (HR) for hospitalisation was analysed as nested case-control study. Results: Sixteen of the 2533 SLE patients were hospitalised with COVID-19 infection. The age-sex adjusted rate per 1000 person years was 6.16 (95% CI 3.76-10.08) in SLE patients, and the corresponding hazard ratio was 2.54 (95% CI 1.55-4.16) compared with the matched general population group after adjustment for comorbidities. Among SLE patients, hydroxychloroquine treatment was associated with a HR for hospitalisation of 0.61 (95% CI 0.19-1.88), and 1.06 (95% CI 0.3-3.72) for glucocorticoid treatment. Conclusion: Patients with SLE were at increased risk of hospitalisation with COVID-19.
References
Bodilsen, Leth, Nielsen, Holler, Benfield et al., Positive Predictive Value of ICD-10 Diagnosis Codes for COVID-19, Clin. Epidemiol, doi:10.2147/CLEP.S309840
Cassione, Zanframundo, Biglia, Codullo, Montecucco et al., COVID-19 infection in a northern-Italian cohort of systemic lupus erythematosus assessed by telemedicine, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2020-217717
Chuah, Teh, Akbar, Cheong, Singh, Impact of COVID-19 pandemic on hospitalisation of patients with systemic lupus erythematosus (SLE): Report from a tertiary hospital during the peak of the pandemic, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2020-218475
Cordtz, Lindhardsen, Soussi, Vela, Uhrenholt et al., Incidence and severeness of COVID-19 hospitalization in patients with inflammatory rheumatic disease: A nationwide cohort study from Denmark, Rheumatology, doi:10.1093/rheumatology/keaa897
Danza, Ruiz-Irastorza, Infection risk in systemic lupus erythematosus patients: Susceptibility factors and preventive strategies, Lupus, doi:10.1177/0961203313493032
Fosbøl, Butt, Østergaard, Andersson, Selmer et al., Association of Angiotensin-Converting Enzyme Inhibitor or Angiotensin Receptor Blocker Use With COVID-19 Diagnosis and Mortality, JAMA-J. Am. Med. Assoc, doi:10.1001/jama.2020.11301
Geleris, Sun, Platt, Zucker, Baldwin et al., Observational Study of Hydroxychloroquine in Hospitalized Patients with Covid-19, N. Engl. J. Med
Gianfrancesco, Hyrich, Al-Adely, Carmona, Danila et al., Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: Data from the COVID-19 Global Rheumatology Alliance physician-reported registry, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2020-217871
Glintborg, Jensen, Engel, Terslev, Jensen et al., Self-protection strategies and health behaviour in patients with inflammatory rheumatic diseases during the COVID-19 pandemic: Results and predictors in more than 12 000 patients with inflammatory rheumatic diseases followed in the Danish DANBIO registry, RMD Open, doi:10.1136/rmdopen-2020-001505
Goyal, SLE patients are not immune to covid-19: Importance of sending the right message across, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2020-217658
Hermansen, Lindhardsen, Torp-Pedersen, Faurschou, Jacobsen, Incidence of Systemic Lupus Erythematosus and Lupus Nephritis in Denmark: A Nationwide Cohort Study, J. Rheumatol, doi:10.3899/jrheum.151221
Horisberger, Moi, Ribi, Comte, Impact of COVID-19 pandemic on SLE: Beyond the risk of infection, Lupus Sci. Med, doi:10.1136/lupus-2020-000408
Johannesdottir, Horváth-Puhó, Ehrenstein, Schmidt, Pedersen et al., Existing data sources for clinical epidemiology: The Danish National Database of Reimbursed Prescriptions, Clin. Epidemiol, doi:10.2147/CLEP.S37587
Konig, Kim, Scheetz, Graef, Liew et al., Baseline use of hydroxychloroquine in systemic lupus erythematosus does not preclude SARS-CoV-2 infection and severe COVID-19, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2020-217690
Liu, Cao, Xu, Wang, Zhang et al., Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro, Cell Discov, doi:10.1038/s41421-019-0132-8
Mageau, Aldebert, Van Gysel, Papo, Timsit et al., SARS-CoV-2 infection among inpatients with systemic lupus erythematosus in France: A nationwide epidemiological study, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2021-220010
Manzano, Fernández-Bello, Sanz, Marhuenda, López-Longo et al., Insights into the Procoagulant Profile of Patients with Systemic Lupus Erythematosus without Antiphospholipid Antibodies, J. Clin. Med, doi:10.3390/jcm9103297
Mathian, Mahevas, Rohmer, Roumier, Cohen-Aubart et al., Clinical course of coronavirus disease 2019 (COVID-19) in a series of 17 patients with systemic lupus erythematosus under long-term treatment with hydroxychloroquine, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2020-217566
Ning, Meng, Tang, Yu, Xu et al., A case of SLE with COVID-19 and multiple infections, Open Med, doi:10.1515/med-2020-0238
Ramirez, Gerosa, Beretta, Bellocchi, Argolini et al., COVID-19 in systemic lupus erythematosus: Data from a survey on 417 patients, Semin. Arthritis Rheum, doi:10.1016/j.semarthrit.2020.06.012
Rosenberg, Dufort, Udo, Wilberschied, Kumar et al., Association of Treatment With Hydroxychloroquine or Azithromycin With In-Hospital Mortality in Patients With COVID-19 in New York State, JAMA, doi:10.1001/jama.2020.8630
Schmidt, Pedersen, Sørensen, The Danish Civil Registration System as a tool in epidemiology, Eur. J. Epidemiol, doi:10.1007/s10654-014-9930-3
Schmidt, Schmidt, Sandegaard, Ehrenstein, Pedersen et al., The Danish National Patient Registry: A review of content, data quality, and research potential, Clin. Epidemiol, doi:10.2147/CLEP.S91125
Smeele, Perez-Garcia, Grimminck, Schoenmakers, Mulders et al., Systemic lupus erythematosus and COVID-19 during pregnancy, Lupus, doi:10.1177/09612033211002270
Sookaromdee, Wiwanitkit, Hydroxychloroquine, Turk, COVID-19, and SLE, J. Hematol, doi:10.4274/tjh.galenos.2021.2020.0770
Thanou, Sawalha, SARS-CoV-2 and Systemic Lupus Erythematosus, Curr. Rheumatol. Rep, doi:10.1007/s11926-020-00973-w
Wallace, Washer, Marder, Kahlenberg, Patients with lupus with COVID-19: University of Michigan experience, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2020-217794
Zurita, Arreaga, Chavez, Zurita, SARS-CoV-2 Infection and COVID-19 in 5 Patients in Ecuador after Prior Treatment with Hydroxychloroquine for Systemic Lupus Erythematosus, Am. J. Case Rep, doi:10.12659/AJCR.927304
DOI record:
{
"DOI": "10.3390/jcm10173842",
"ISSN": [
"2077-0383"
],
"URL": "http://dx.doi.org/10.3390/jcm10173842",
"abstract": "<jats:p>Background: Patients with systemic lupus erythematosus (SLE) have an increased risk of infections due to impaired immune functions, disease activity, and treatment. This study investigated the impact of having SLE on the incidence of hospitalisation with COVID-19 infection. Methods: This was a nationwide cohort study from Denmark between 1 March 2020 to 2 February 2021, based on the linkage of several nationwide registers. The adjusted incidence of COVID-19 hospitalisation was estimated for patients with SLE compared with the general population in Cox-regression models. Among SLE patients, the hazard ratio (HR) for hospitalisation was analysed as nested case-control study. Results: Sixteen of the 2533 SLE patients were hospitalised with COVID-19 infection. The age-sex adjusted rate per 1000 person years was 6.16 (95% CI 3.76–10.08) in SLE patients, and the corresponding hazard ratio was 2.54 (95% CI 1.55–4.16) compared with the matched general population group after adjustment for comorbidities. Among SLE patients, hydroxychloroquine treatment was associated with a HR for hospitalisation of 0.61 (95% CI 0.19–1.88), and 1.06 (95% CI 0.3–3.72) for glucocorticoid treatment. Conclusion: Patients with SLE were at increased risk of hospitalisation with COVID-19.</jats:p>",
"alternative-id": [
"jcm10173842"
],
"author": [
{
"affiliation": [],
"family": "Cordtz",
"given": "René",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-5812-5234",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kristensen",
"given": "Salome",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dalgaard",
"given": "Louise Plank Holm",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8148-9658",
"affiliation": [],
"authenticated-orcid": false,
"family": "Westermann",
"given": "Rasmus",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Duch",
"given": "Kirsten",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lindhardsen",
"given": "Jesper",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Torp-Pedersen",
"given": "Christian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dreyer",
"given": "Lene",
"sequence": "additional"
}
],
"container-title": [
"Journal of Clinical Medicine"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
8,
30
]
],
"date-time": "2021-08-30T15:01:37Z",
"timestamp": 1630335697000
},
"deposited": {
"date-parts": [
[
2021,
8,
30
]
],
"date-time": "2021-08-30T16:02:39Z",
"timestamp": 1630339359000
},
"indexed": {
"date-parts": [
[
2022,
2,
16
]
],
"date-time": "2022-02-16T18:49:09Z",
"timestamp": 1645037349732
},
"is-referenced-by-count": 4,
"issn-type": [
{
"type": "electronic",
"value": "2077-0383"
}
],
"issue": "17",
"issued": {
"date-parts": [
[
2021,
8,
27
]
]
},
"journal-issue": {
"issue": "17",
"published-online": {
"date-parts": [
[
2021,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
8,
27
]
],
"date-time": "2021-08-27T00:00:00Z",
"timestamp": 1630022400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2077-0383/10/17/3842/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "3842",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
8,
27
]
]
},
"published-online": {
"date-parts": [
[
2021,
8,
27
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1177/0961203313493032",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1136/annrheumdis-2020-217717",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1093/rheumatology/keaa897",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1016/j.semarthrit.2020.06.012",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1515/med-2020-0238",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1136/lupus-2020-000408",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.4274/tjh.galenos.2021.2020.0770",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1136/annrheumdis-2020-217658",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.12659/AJCR.927304",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1136/annrheumdis-2020-217690",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1136/annrheumdis-2020-217794",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1136/annrheumdis-2020-217566",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1136/annrheumdis-2020-218475",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1177/09612033211002270",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1007/s11926-020-00973-w",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1007/s10654-014-9930-3",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.3899/jrheum.151221",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.2147/CLEP.S91125",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.2147/CLEP.S37587",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.2147/CLEP.S309840",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1001/jama.2020.11301",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1136/annrheumdis-2020-217871",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1136/annrheumdis-2021-220010",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1038/s41421-019-0132-8",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1056/NEJMoa2012410",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1001/jama.2020.8630",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1136/rmdopen-2020-001505",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.3390/jcm9103297",
"doi-asserted-by": "publisher",
"key": "ref28"
}
],
"reference-count": 28,
"references-count": 28,
"relation": {},
"score": 1,
"short-container-title": [
"JCM"
],
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": [
"Incidence of COVID-19 Hospitalisation in Patients with Systemic Lupus Erythematosus: A Nationwide Cohort Study from Denmark"
],
"type": "journal-article",
"volume": "10"
}