Prognostic Factors for Predicting Post-COVID-19 Condition in Patients With COVID-19 in an Outpatient Setting
et al., Journal of Korean Medical Science, doi:10.3346/jkms.2024.39.e23, Jan 2024
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 257 outpatients with mild COVID-19 in South Korea showing vitamin D deficiency (<20 ng/mL) associated with post-COVID condition and longer symptom duration.
This is the 192nd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
risk of no recovery, 48.9% lower, HR 0.51, p = 0.002, high D levels (≥20ng/mL) 99, low D levels (<20ng/mL) 67, adjusted per study, multivariable.
|
|
risk of long COVID, 68.4% lower, HR 0.32, p = 0.001, high D levels (≥20ng/mL) 99, low D levels (<20ng/mL) 67, adjusted per study, inverted to make HR<1 favor high D levels (≥20ng/mL), multivariable.
|
|
risk of hospitalization, 25.6% lower, RR 0.74, p = 0.48, high D levels (≥20ng/mL) 11 of 99 (11.1%), low D levels (<20ng/mL) 10 of 67 (14.9%), NNT 26, unadjusted.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Choi et al., 2 Jan 2024, retrospective, South Korea, peer-reviewed, mean age 55.7, 6 authors, study period April 2022 - December 2022.
Contact: cem@ewha.ac.kr.
Prognostic Factors for Predicting Post-COVID-19 Condition in Patients With COVID-19 in an Outpatient Setting
Journal of Korean Medical Science, doi:10.3346/jkms.2024.39.e23
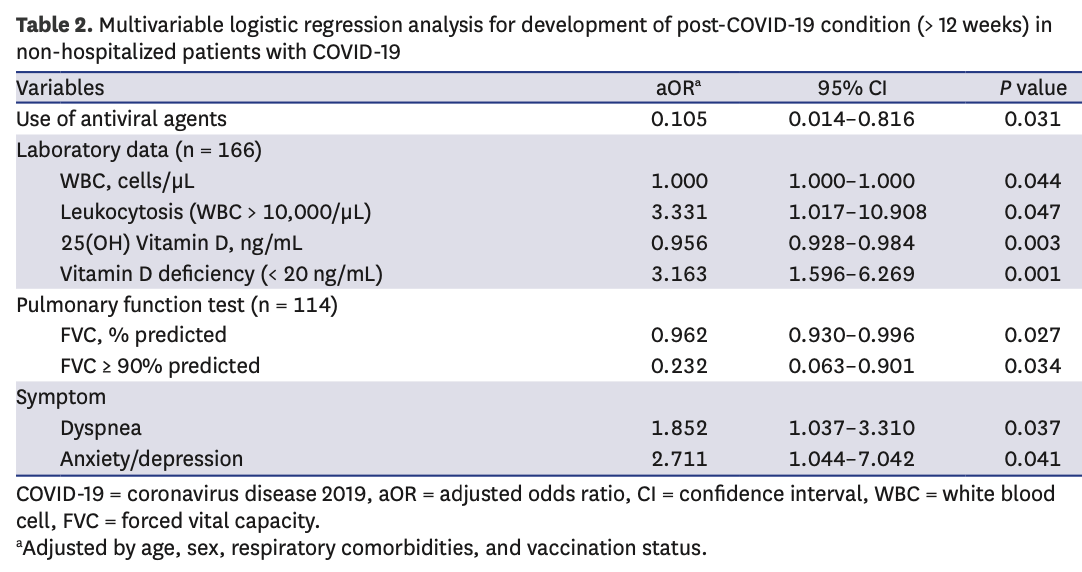
Background: Although data on post-coronavirus disease 2019 (COVID-19) conditions are extensive, the prognostic factors affecting symptom duration in non-hospitalized patients with COVID-19 are currently not well known. We aimed to investigate the various prognostic factors affecting symptom duration among outpatients with COVID-19. Methods: Data were analyzed from 257 patients who were diagnosed with mild COVID-19 and visited the 'post-COVID-19 outpatient clinic' between April and December 2022 after a mandatory isolation period. The symptom duration was measured from diagnosis to symptom resolution. Laboratory and pulmonary function test results from their first visit were collected. Results: The mean age of patients was 55.7 years, and the median symptom duration was 57 days. The development of post-COVID-19 conditions (> 12 weeks) were significantly correlated with not using antiviral drugs, leukocytosis (white blood cell > 10,000/µL), lower 25(OH)D 3 levels, forced vital capacity (FVC) < 90% predicted, and presence of dyspnea and anxiety/depression. Additionally, in multivariable Cox regression analysis, not using antiviral drugs, lower 25(OH)D 3 levels, and having dyspnea were poor prognostic factors for longer symptom duration. Particularly, vitamin D deficiency (< 20 ng/mL) and not using antivirals during the acute phase were independent poor prognostic factors for both post-COVID-19 condition and longer symptom duration.
Conclusion: The non-use of antivirals, lower 25(OH)D 3 levels, leukocytosis, FVC < 90% predicted, and the presence of dyspnea and anxiety/depression symptoms could be useful prognostic factors for predicting post-COVID-19 condition in outpatients with COVID-19. We suggest that the use of antiviral agents during the acute phase and vitamin D supplements might help reduce COVID-19 symptom duration.
SUPPLEMENTARY MATERIALS Supplementary Table 1 The incidence of clinical symptoms of patients with COVID- 4 Baseline characteristics of the study population at the time of their first visit to the outpatient department according to Vit D deficiency Click here to view Supplementary Table 5 Baseline characteristics of the study population at the time of their first visit to the outpatient department according to use of antiviral agent at acute phase of COVID-19
Click here to view
References
Amin, Kakamad, Ahmed, Ahmed, Abdulla et al., Post COVID-19 pulmonary fibrosis; a meta-analysis study, Ann Med Surg (Lond), doi:10.1016/j.amsu.2022.103590
Aminian, Bena, Pantalone, Burguera, Association of obesity with postacute sequelae of COVID-19, Diabetes Obes Metab, doi:10.1111/dom.14454
Augustin, Schommers, Stecher, Dewald, Gieselmann et al., Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study, Lancet Reg Health Eur, doi:10.1016/j.lanepe.2021.100122
Beigel, Tomashek, Dodd, Mehta, Zingman et al., Remdesivir for the treatment of COVID-19 -final report, N Engl J Med, doi:10.1056/NEJMoa2007764
Bilezikian, Bikle, Hewison, Lazaretti-Castro, Formenti et al., Mechanisms in endocrinology: vitamin D and COVID-19, Eur J Endocrinol, doi:10.1530/EJE-20-0665
Butt, Dargham, Coyle, Yassine, Al-Khal et al., COVID-19 disease severity in persons infected with Omicron BA.1 and BA.2 sublineages and association with vaccination status, JAMA Intern Med, doi:10.1001/jamainternmed.2022.3351
Carfì, Bernabei, Landi, Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19, JAMA, doi:10.1001/jama.2020.12603
Chen, Haupert, Zimmermann, Shi, Fritsche et al., Global prevalence of postcoronavirus disease 2019 (COVID-19) condition or long COVID: a meta-analysis and systematic review, J Infect Dis, doi:10.1093/infdis/jiac136
Daines, Zheng, Elneima, Harrison, Lone et al., Characteristics and risk factors for post-COVID-19 breathlessness after hospitalisation for COVID-19, ERJ Open Res, doi:10.1183/23120541.00274-2022
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients, Aging Clin Exp Res, doi:10.1007/s40520-020-01677-y
Dhawan, Gopalan, Howard, Vicente, Park et al., Beyond the clot: perfusion imaging of the pulmonary vasculature after COVID-19, Lancet Respir Med, doi:10.1016/S2213-2600(20)30407-0
Dissanayake, Silva, Sumanatilleke, De Silva, Gamage et al., Prognostic and therapeutic role of vitamin D in COVID-19: systematic review and meta-analysis, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab892
Dror, Morozov, Daoud, Namir, Yakir et al., Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness, PLoS One, doi:10.1371/journal.pone.0263069
Fernández-De-Las-Peñas, Palacios-Ceña, Gómez-Mayordomo, Florencio, Cuadrado et al., Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: a systematic review and meta-analysis, Eur J Intern Med, doi:10.1016/j.ejim.2021.06.009
Fernández-De-Las-Peñas, Pellicer-Valero, Navarro-Pardo, Palacios-Ceña, Florencio et al., Symptoms experienced at the acute phase of SARS-CoV-2 infection as risk factor of long-term post-COVID symptoms: the LONG-COVID-EXP-CM multicenter study, Int J Infect Dis, doi:10.1016/j.ijid.2022.01.007
Gao, Piernas, Astbury, Hippisley-Cox, 'rahilly et al., Associations between bodymass index and COVID-19 severity in 6•9 million people in England: a prospective, community-based, cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00089-9
Gottlieb, Vaca, Paredes, Mera, Webb et al., Early remdesivir to prevent progression to severe COVID-19 in outpatients, N Engl J Med, doi:10.1056/NEJMoa2116846
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths, Nutrients, doi:10.3390/nu12040988
Grein, Ohmagari, Shin, Diaz, Asperges et al., Compassionate use of remdesivir for patients with severe COVID-19, N Engl J Med, doi:10.1056/NEJMoa2007016
Hammond, Leister-Tebbe, Gardner, Abreu, Wisemandle, Oral nirmatrelvir for high-risk, nonhospitalized adults with COVID-19, N Engl J Med, doi:10.1056/NEJMoa2118542
Holick, Vitamin D deficiency, N Engl J Med, doi:10.1056/NEJMra070553
Huang, Huang, Wang, Li, Ren et al., 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study, Lancet, doi:10.1016/S0140-6736(20)32656-8
Huang, Kovalic, Graber, Prognostic value of leukocytosis and lymphopenia for coronavirus disease severity, Emerg Infect Dis, doi:10.3201/eid2608.201160
Jung, Ha, Choe, Lee, Jo et al., Persistent symptoms after acute COVID-19 infection in Omicron era, J Korean Med Sci, doi:10.3346/jkms.2022.37.e213
Kamal, Omirah, Hussein, Saeed, Assessment and characterisation of post-COVID-19 manifestations, Int J Clin Pract, doi:10.1111/ijcp.13746
Lopez-Leon, Wegman-Ostrosky, Perelman, Sepulveda, Rebolledo et al., More than 50 long-term effects of COVID-19: a systematic review and meta-analysis, Sci Rep, doi:10.1038/s41598-021-95565-8
Macintyre, Crapo, Viegi, Johnson, Van Der Grinten et al., Standardisation of the single-breath determination of carbon monoxide uptake in the lung, Eur Respir J, doi:10.1183/09031936.05.00034905
Magnúsdóttir, Lovik, Unnarsdóttir, Mccartney, Ask et al., Acute COVID-19 severity and mental health morbidity trajectories in patient populations of six nations: an observational study, Lancet Public Health, doi:10.1016/S2468-2667(22)00042-1
Michelen, Manoharan, Elkheir, Cheng, Dagens et al., Characterising long COVID: a living systematic review, BMJ Glob Health, doi:10.1136/bmjgh-2021-005427
Miller, Hankinson, Brusasco, Burgos, Casaburi et al., Standardisation of spirometry, Eur Respir J, doi:10.1183/09031936.05.00034805
Munker, Veit, Barton, Mertsch, Mümmler et al., Pulmonary function impairment of asymptomatic and persistently symptomatic patients 4 months after COVID-19 according to disease severity, Infection, doi:10.1007/s15010-021-01669-8
Nalbandian, Sehgal, Gupta, Madhavan, Mcgroder et al., Post-acute COVID-19 syndrome, Nat Med, doi:10.1038/s41591-021-01283-z
Nielsen, Junker, Boelt, Cohen, Munger et al., Vitamin D status and severity of COVID-19, Sci Rep, doi:10.1038/s41598-022-21513-9
Oscanoa, Amado, Vidal, Laird, Ghashut et al., The relationship between the severity and mortality of SARS-CoV-2 infection and 25-hydroxyvitamin D concentration -a metaanalysis, Adv Respir Med, doi:10.5603/ARM.a2021.0037
Pizzini, Aichner, Sahanic, Böhm, Egger et al., Impact of vitamin D deficiency on COVID-19-a prospective analysis from the CovILD registry, Nutrients, doi:10.3390/nu12092775
Renaud-Charest, Lui, Eskander, Ceban, Ho et al., Onset and frequency of depression in post-COVID-19 syndrome: a systematic review, J Psychiatr Res, doi:10.1016/j.jpsychires.2021.09.054
Song, Hui, Hull, Birring, Mcgarvey et al., Confronting COVID-19-associated cough and the post-COVID syndrome: role of viral neurotropism, neuroinflammation, and neuroimmune responses, Lancet Respir Med, doi:10.1016/S2213-2600(21)00125-9
Stavem, Ghanima, Olsen, Gilboe, Einvik, Persistent symptoms 1.5-6 months after COVID-19 in non-hospitalised subjects: a population-based cohort study, Thorax, doi:10.1136/thoraxjnl-2020-216377
Subramanian, Nirantharakumar, Hughes, Myles, Williams et al., Symptoms and risk factors for long COVID in non-hospitalized adults, Nat Med, doi:10.1038/s41591-022-01909-w
Sudre, Murray, Varsavsky, Graham, Penfold et al., Attributes and predictors of long COVID, Nat Med, doi:10.1038/s41591-021-01292-y
Tenforde, Kim, Lindsell, Rose, Shapiro et al., Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network -United States, March-June 2020, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6930e1
Townsend, Dyer, Mccluskey, 'brien, Dowds et al., Investigating the relationship between vitamin D and persistent symptoms following SARS-CoV-2 infection, Nutrients, doi:10.3390/nu13072430
Tsampasian, Elghazaly, Chattopadhyay, Debski, Naing et al., Risk factors associated with post-COVID-19 condition: a systematic review and meta-analysis, JAMA Intern Med, doi:10.1001/jamainternmed.2023.0750
Ulloa, Buchan, Daneman, Brown, Estimates of SARS-CoV-2 Omicron variant severity in Ontario, Canada, JAMA, doi:10.1001/jama.2022.2274
Wolter, Jassat, Walaza, Welch, Moultrie et al., Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: a data linkage study, Lancet, doi:10.1016/S0140-6736(22)00017-4
Yang, Luo, Gan, Chen, Li, Risk factors for predicting mortality of COVID-19 patients: a systematic review and meta-analysis, PLoS One, doi:10.1371/journal.pone.0243124
Ye, Pang, Li, Li, Liu et al., Both underweight and obesity are associated with an increased risk of coronavirus disease 2019 (COVID-19) severity, Front Nutr, doi:10.3389/fnut.2021.649422
Zhang, Bai, Yue, Qin, Zhang et al., Eight months follow-up study on pulmonary function, lung radiographic, and related physiological characteristics in COVID-19 survivors, Sci Rep, doi:10.1038/s41598-021-93191-y
Zhu, Feng, Jiang, Mi, Yang et al., Correlation between white blood cell count at admission and mortality in COVID-19 patients: a retrospective study, BMC Infect Dis, doi:10.1186/s12879-021-06277-3
DOI record:
{
"DOI": "10.3346/jkms.2024.39.e23",
"ISSN": [
"1011-8934",
"1598-6357"
],
"URL": "http://dx.doi.org/10.3346/jkms.2024.39.e23",
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"value": "2023-07-13"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"value": "2023-10-26"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published online",
"name": "published_online",
"value": "2024-01-02"
},
{
"group": {
"label": "Copyright and Licensing",
"name": "Copyright_and_licensing"
},
"label": "Copyright",
"name": "copyright",
"value": "© 2024 The Korean Academy of Medical Sciences."
},
{
"explanation": {
"URL": "https://creativecommons.org/licenses/by-nc/4.0/"
},
"group": {
"label": "Copyright and Licensing",
"name": "Copyright_and_licensing"
},
"label": "License",
"name": "license",
"value": "This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3538-1993",
"affiliation": [
{
"name": "Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Korea."
}
],
"authenticated-orcid": false,
"family": "Choi",
"given": "Myeong Geun",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0009-0005-6980-8838",
"affiliation": [
{
"name": "Department of Internal Medicine, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Korea."
}
],
"authenticated-orcid": false,
"family": "Joo",
"given": "Young Woong",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4909-2308",
"affiliation": [
{
"name": "Informatization Department, Ewha Womans University Seoul Hospital, Ewha Womans University College of Medicine, Seoul, Korea."
}
],
"authenticated-orcid": false,
"family": "Kim",
"given": "Min-Ho",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2731-8188",
"affiliation": [
{
"name": "Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Korea."
}
],
"authenticated-orcid": false,
"family": "Park",
"given": "Sojung",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0009-0004-9454-8401",
"affiliation": [
{
"name": "Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Korea."
}
],
"authenticated-orcid": false,
"family": "Shin",
"given": "Yune-Young",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9616-2722",
"affiliation": [
{
"name": "Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Korea."
}
],
"authenticated-orcid": false,
"family": "Chun",
"given": "Eun Mi",
"sequence": "additional"
}
],
"container-title": "Journal of Korean Medical Science",
"container-title-short": "J Korean Med Sci",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"jkms.org"
]
},
"created": {
"date-parts": [
[
2023,
12,
26
]
],
"date-time": "2023-12-26T21:54:16Z",
"timestamp": 1703627656000
},
"deposited": {
"date-parts": [
[
2024,
1,
14
]
],
"date-time": "2024-01-14T19:00:51Z",
"timestamp": 1705258851000
},
"indexed": {
"date-parts": [
[
2024,
1,
15
]
],
"date-time": "2024-01-15T05:13:08Z",
"timestamp": 1705295588450
},
"is-referenced-by-count": 0,
"issue": "2",
"issued": {
"date-parts": [
[
2024
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2024
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
1,
1
]
],
"date-time": "2024-01-01T00:00:00Z",
"timestamp": 1704067200000
}
}
],
"link": [
{
"URL": "https://jkms.org/pdf/10.3346/jkms.2024.39.e23",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://jkms.org/DOIx.php?id=10.3346/jkms.2024.39.e23",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://jkms.org/DOIx.php?id=10.3346/jkms.2024.39.e23",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "18617",
"original-title": [],
"prefix": "10.3346",
"published": {
"date-parts": [
[
2024
]
]
},
"published-online": {
"date-parts": [
[
2024
]
]
},
"publisher": "XMLink",
"reference": [
{
"DOI": "10.1038/s41591-021-01283-z",
"author": "Nalbandian",
"doi-asserted-by": "crossref",
"first-page": "601",
"issue": "4",
"journal-title": "Nat Med",
"key": "10.3346/jkms.2024.39.e23_ref1",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(20)32656-8",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "220",
"issue": "10270",
"journal-title": "Lancet",
"key": "10.3346/jkms.2024.39.e23_ref2",
"volume": "397",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.12603",
"author": "Carfì",
"doi-asserted-by": "crossref",
"first-page": "603",
"issue": "6",
"journal-title": "JAMA",
"key": "10.3346/jkms.2024.39.e23_ref3",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-95565-8",
"author": "Lopez-Leon",
"doi-asserted-by": "crossref",
"first-page": "16144",
"issue": "1",
"journal-title": "Sci Rep",
"key": "10.3346/jkms.2024.39.e23_ref4",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1136/bmjgh-2021-005427",
"author": "Michelen",
"doi-asserted-by": "crossref",
"first-page": "e005427",
"issue": "9",
"journal-title": "BMJ Glob Health",
"key": "10.3346/jkms.2024.39.e23_ref5",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1016/j.ejim.2021.06.009",
"author": "Fernández-de-Las-Peñas",
"doi-asserted-by": "crossref",
"first-page": "55",
"journal-title": "Eur J Intern Med",
"key": "10.3346/jkms.2024.39.e23_ref6",
"volume": "92",
"year": "2021"
},
{
"author": "World Health Organization",
"key": "10.3346/jkms.2024.39.e23_ref7",
"volume-title": "A Clinical Case Definition of Post COVID-19 Condition by a Delphi Consensus, 6 October 2021",
"year": "2021"
},
{
"key": "10.3346/jkms.2024.39.e23_ref8",
"unstructured": "Centers for Disease Control and Prevention. Post-COVID conditions: information for healthcare providers. Updated 2023. Accessed June 15, 2023. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html"
},
{
"DOI": "10.1001/jamainternmed.2022.3351",
"author": "Butt",
"doi-asserted-by": "crossref",
"first-page": "1097",
"issue": "10",
"journal-title": "JAMA Intern Med",
"key": "10.3346/jkms.2024.39.e23_ref9",
"volume": "182",
"year": "2022"
},
{
"DOI": "10.1016/S0140-6736(22)00017-4",
"author": "Wolter",
"doi-asserted-by": "crossref",
"first-page": "437",
"issue": "10323",
"journal-title": "Lancet",
"key": "10.3346/jkms.2024.39.e23_ref10",
"volume": "399",
"year": "2022"
},
{
"DOI": "10.1001/jama.2022.2274",
"author": "Ulloa",
"doi-asserted-by": "crossref",
"first-page": "1286",
"issue": "13",
"journal-title": "JAMA",
"key": "10.3346/jkms.2024.39.e23_ref11",
"volume": "327",
"year": "2022"
},
{
"DOI": "10.1038/s41591-022-01909-w",
"author": "Subramanian",
"doi-asserted-by": "crossref",
"first-page": "1706",
"issue": "8",
"journal-title": "Nat Med",
"key": "10.3346/jkms.2024.39.e23_ref12",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1016/j.lanepe.2021.100122",
"author": "Augustin",
"doi-asserted-by": "crossref",
"first-page": "100122",
"journal-title": "Lancet Reg Health Eur",
"key": "10.3346/jkms.2024.39.e23_ref13",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1136/thoraxjnl-2020-216377",
"author": "Stavem",
"doi-asserted-by": "crossref",
"first-page": "405",
"issue": "4",
"journal-title": "Thorax",
"key": "10.3346/jkms.2024.39.e23_ref14",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1001/jamainternmed.2023.0750",
"author": "Tsampasian",
"doi-asserted-by": "crossref",
"first-page": "566",
"issue": "6",
"journal-title": "JAMA Intern Med",
"key": "10.3346/jkms.2024.39.e23_ref15",
"volume": "183",
"year": "2023"
},
{
"DOI": "10.1183/09031936.05.00034905",
"author": "Macintyre",
"doi-asserted-by": "crossref",
"first-page": "720",
"issue": "4",
"journal-title": "Eur Respir J",
"key": "10.3346/jkms.2024.39.e23_ref16",
"volume": "26",
"year": "2005"
},
{
"DOI": "10.1183/09031936.05.00034805",
"author": "Miller",
"doi-asserted-by": "crossref",
"first-page": "319",
"issue": "2",
"journal-title": "Eur Respir J",
"key": "10.3346/jkms.2024.39.e23_ref17",
"volume": "26",
"year": "2005"
},
{
"DOI": "10.1056/NEJMra070553",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "266",
"issue": "3",
"journal-title": "N Engl J Med",
"key": "10.3346/jkms.2024.39.e23_ref18",
"volume": "357",
"year": "2007"
},
{
"DOI": "10.15585/mmwr.mm6930e1",
"author": "Tenforde",
"doi-asserted-by": "crossref",
"first-page": "993",
"issue": "30",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "10.3346/jkms.2024.39.e23_ref19",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.5603/ARM.a2021.0037",
"author": "Oscanoa",
"doi-asserted-by": "crossref",
"first-page": "145",
"issue": "2",
"journal-title": "Adv Respir Med",
"key": "10.3346/jkms.2024.39.e23_ref20",
"volume": "89",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0263069",
"author": "Dror",
"doi-asserted-by": "crossref",
"first-page": "e0263069",
"issue": "2",
"journal-title": "PLoS One",
"key": "10.3346/jkms.2024.39.e23_ref21",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1038/s41598-022-21513-9",
"author": "Nielsen",
"doi-asserted-by": "crossref",
"first-page": "19823",
"issue": "1",
"journal-title": "Sci Rep",
"key": "10.3346/jkms.2024.39.e23_ref22",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1210/clinem/dgab892",
"author": "Dissanayake",
"doi-asserted-by": "crossref",
"first-page": "1484",
"issue": "5",
"journal-title": "J Clin Endocrinol Metab",
"key": "10.3346/jkms.2024.39.e23_ref23",
"volume": "107",
"year": "2022"
},
{
"DOI": "10.3390/nu12040988",
"author": "Grant",
"doi-asserted-by": "crossref",
"first-page": "988",
"issue": "4",
"journal-title": "Nutrients",
"key": "10.3346/jkms.2024.39.e23_ref24",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3390/nu13072430",
"author": "Townsend",
"doi-asserted-by": "crossref",
"first-page": "2430",
"issue": "7",
"journal-title": "Nutrients",
"key": "10.3346/jkms.2024.39.e23_ref25",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3390/nu12092775",
"author": "Pizzini",
"doi-asserted-by": "crossref",
"first-page": "2775",
"issue": "9",
"journal-title": "Nutrients",
"key": "10.3346/jkms.2024.39.e23_ref26",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3346/jkms.2022.37.e213",
"author": "Jung",
"doi-asserted-by": "crossref",
"first-page": "e213",
"issue": "27",
"journal-title": "J Korean Med Sci",
"key": "10.3346/jkms.2024.39.e23_ref27",
"volume": "37",
"year": "2022"
},
{
"DOI": "10.1016/S2213-2600(21)00125-9",
"author": "Song",
"doi-asserted-by": "crossref",
"first-page": "533",
"issue": "5",
"journal-title": "Lancet Respir Med",
"key": "10.3346/jkms.2024.39.e23_ref28",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1007/s40520-020-01677-y",
"author": "Daneshkhah",
"doi-asserted-by": "crossref",
"first-page": "2141",
"issue": "10",
"journal-title": "Aging Clin Exp Res",
"key": "10.3346/jkms.2024.39.e23_ref29",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1530/EJE-20-0665",
"author": "Bilezikian",
"doi-asserted-by": "crossref",
"first-page": "R133",
"issue": "5",
"journal-title": "Eur J Endocrinol",
"key": "10.3346/jkms.2024.39.e23_ref30",
"volume": "183",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2007764",
"author": "Beigel",
"doi-asserted-by": "crossref",
"first-page": "1813",
"issue": "19",
"journal-title": "N Engl J Med",
"key": "10.3346/jkms.2024.39.e23_ref31",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2007016",
"author": "Grein",
"doi-asserted-by": "crossref",
"first-page": "2327",
"issue": "24",
"journal-title": "N Engl J Med",
"key": "10.3346/jkms.2024.39.e23_ref32",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2116846",
"author": "Gottlieb",
"doi-asserted-by": "crossref",
"first-page": "305",
"issue": "4",
"journal-title": "N Engl J Med",
"key": "10.3346/jkms.2024.39.e23_ref33",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2118542",
"author": "Hammond",
"doi-asserted-by": "crossref",
"first-page": "1397",
"issue": "15",
"journal-title": "N Engl J Med",
"key": "10.3346/jkms.2024.39.e23_ref34",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.1111/ijcp.13746",
"author": "Kamal",
"doi-asserted-by": "crossref",
"first-page": "e13746",
"issue": "3",
"journal-title": "Int J Clin Pract",
"key": "10.3346/jkms.2024.39.e23_ref35",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.1093/infdis/jiac136",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "1593",
"issue": "9",
"journal-title": "J Infect Dis",
"key": "10.3346/jkms.2024.39.e23_ref36",
"volume": "226",
"year": "2022"
},
{
"DOI": "10.1038/s41591-021-01292-y",
"author": "Sudre",
"doi-asserted-by": "crossref",
"first-page": "626",
"issue": "4",
"journal-title": "Nat Med",
"key": "10.3346/jkms.2024.39.e23_ref37",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2022.01.007",
"author": "Fernández-de-Las-Peñas",
"doi-asserted-by": "crossref",
"first-page": "241",
"journal-title": "Int J Infect Dis",
"key": "10.3346/jkms.2024.39.e23_ref38",
"volume": "116",
"year": "2022"
},
{
"DOI": "10.1016/S2213-2600(20)30407-0",
"author": "Dhawan",
"doi-asserted-by": "crossref",
"first-page": "107",
"issue": "1",
"journal-title": "Lancet Respir Med",
"key": "10.3346/jkms.2024.39.e23_ref39",
"volume": "9",
"year": "2021"
},
{
"author": "Hama Amin",
"first-page": "103590",
"journal-title": "Ann Med Surg (Lond)",
"key": "10.3346/jkms.2024.39.e23_ref40",
"volume": "77",
"year": "2022"
},
{
"DOI": "10.1183/23120541.00274-2022",
"author": "Daines",
"doi-asserted-by": "crossref",
"first-page": "00274-2022",
"issue": "1",
"journal-title": "ERJ Open Res",
"key": "10.3346/jkms.2024.39.e23_ref41",
"volume": "9",
"year": "2023"
},
{
"DOI": "10.1111/dom.14454",
"author": "Aminian",
"doi-asserted-by": "crossref",
"first-page": "2183",
"issue": "9",
"journal-title": "Diabetes Obes Metab",
"key": "10.3346/jkms.2024.39.e23_ref42",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(21)00089-9",
"author": "Gao",
"doi-asserted-by": "crossref",
"first-page": "350",
"issue": "6",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "10.3346/jkms.2024.39.e23_ref43",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.3389/fnut.2021.649422",
"author": "Ye",
"doi-asserted-by": "crossref",
"first-page": "649422",
"journal-title": "Front Nutr",
"key": "10.3346/jkms.2024.39.e23_ref44",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1186/s12879-021-06277-3",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "574",
"issue": "1",
"journal-title": "BMC Infect Dis",
"key": "10.3346/jkms.2024.39.e23_ref45",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0243124",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "e0243124",
"issue": "11",
"journal-title": "PLoS One",
"key": "10.3346/jkms.2024.39.e23_ref46",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.3201/eid2608.201160",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "1839",
"issue": "8",
"journal-title": "Emerg Infect Dis",
"key": "10.3346/jkms.2024.39.e23_ref47",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-93191-y",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "13854",
"issue": "1",
"journal-title": "Sci Rep",
"key": "10.3346/jkms.2024.39.e23_ref48",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1007/s15010-021-01669-8",
"author": "Munker",
"doi-asserted-by": "crossref",
"first-page": "157",
"issue": "1",
"journal-title": "Infection",
"key": "10.3346/jkms.2024.39.e23_ref49",
"volume": "50",
"year": "2022"
},
{
"DOI": "10.1016/S2468-2667(22)00042-1",
"author": "Magnúsdóttir",
"doi-asserted-by": "crossref",
"first-page": "e406",
"issue": "5",
"journal-title": "Lancet Public Health",
"key": "10.3346/jkms.2024.39.e23_ref50",
"volume": "7",
"year": "2022"
},
{
"DOI": "10.1016/j.jpsychires.2021.09.054",
"author": "Renaud-Charest",
"doi-asserted-by": "crossref",
"first-page": "129",
"journal-title": "J Psychiatr Res",
"key": "10.3346/jkms.2024.39.e23_ref51",
"volume": "144",
"year": "2021"
}
],
"reference-count": 51,
"references-count": 51,
"relation": {},
"resource": {
"primary": {
"URL": "https://jkms.org/DOIx.php?id=10.3346/jkms.2024.39.e23"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Prognostic Factors for Predicting Post-COVID-19 Condition in Patients With COVID-19 in an Outpatient Setting",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3346/crossmark_policy",
"volume": "39"
}
