The Impact of Vitamin D Status on COVID-19 Severity among Hospitalized Patients in the Western Region of Saudi Arabia: A Retrospective Cross-Sectional Study
et al., International Journal of Environmental Research and Public Health, doi:10.3390/ijerph19031901, Feb 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 197 hospitalized patients in Saudi Arabia, showing no significant differences based on vitamin D levels. Adjusted results are provided only for vitamin D as a continuous variable.
This is the 117th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
|
risk of mechanical ventilation, 32.1% lower, RR 0.68, p = 0.27, high D levels (≥20ng/mL) 10 of 53 (18.9%), low D levels (<20ng/mL) 40 of 144 (27.8%), NNT 11, unadjusted.
|
|
risk of ICU admission, 3.9% lower, RR 0.96, p = 0.87, high D levels (≥20ng/mL) 23 of 53 (43.4%), low D levels (<20ng/mL) 65 of 144 (45.1%), NNT 57, unadjusted.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Bushnaq et al., 8 Feb 2022, retrospective, Saudi Arabia, peer-reviewed, 7 authors.
The Impact of Vitamin D Status on COVID-19 Severity among Hospitalized Patients in the Western Region of Saudi Arabia: A Retrospective Cross-Sectional Study
International Journal of Environmental Research and Public Health, doi:10.3390/ijerph19031901
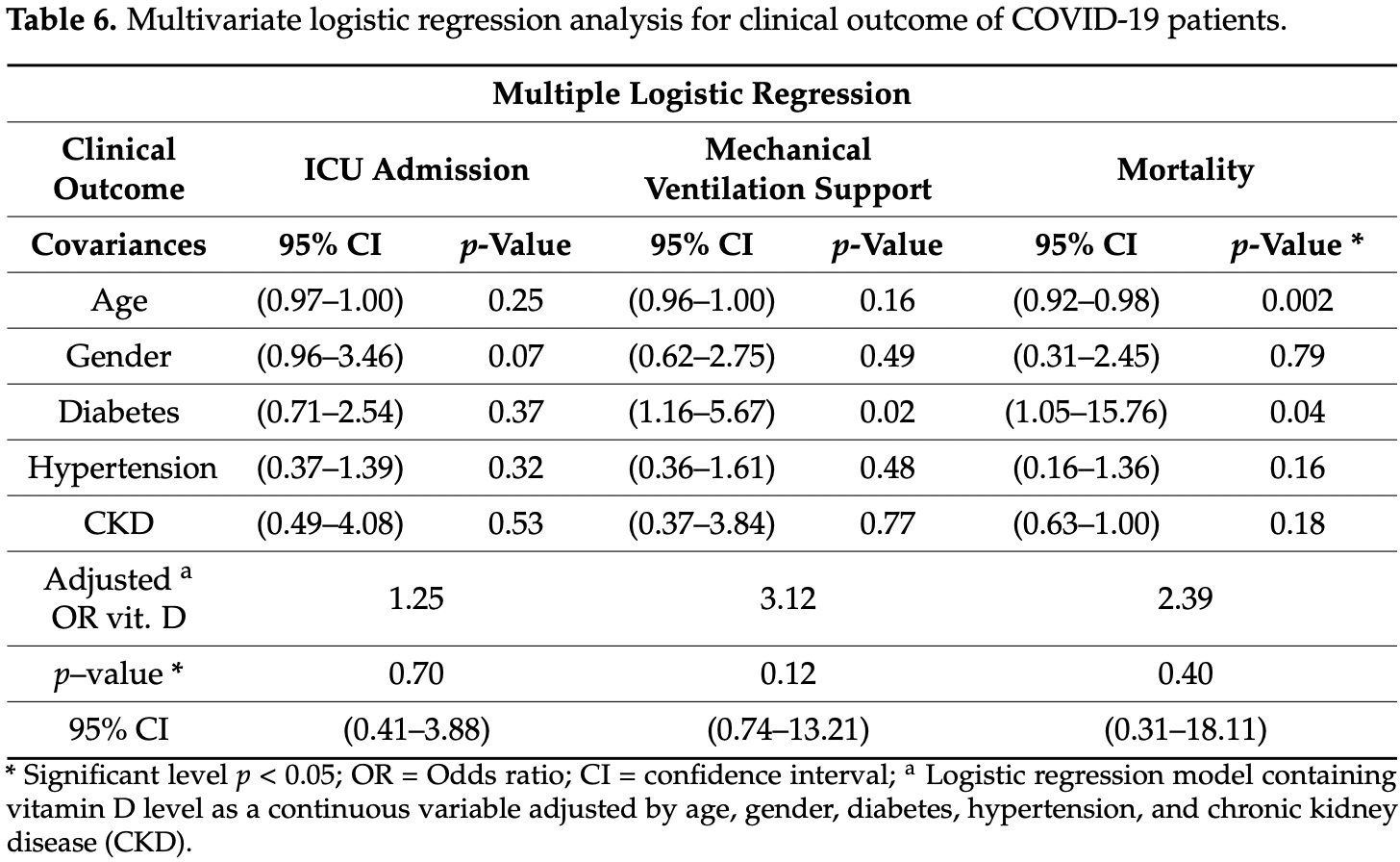
The coronaviruses disease 2019 (COVID-19) spreads continuously worldwide. The new vaccines and drugs have been approved. The prevention of disease is crucial, and some studies reveal the promising effect of alternative therapies such as vitamin D supplementations on COVID-19 prevention, but they still require sufficient evidence. Therefore, the current retrospective multicenter cross-sectional study aims to determine the primary association between the vitamin D status of hospitalized COVID-19 and its severity as well as mortality. A total of 197 COVID-19 were admitted at King Faisal Hospital, Al Noor Specialist Hospital in Makkah, and at Complex King Faisal Hospital in Taif in the Westering region of Saudi Arabia (SA) between June and August 2020. The demographic and clinical characteristics, laboratory tests included serum 25(OH)D and admission for intensive care unit (ICU), length of stay in the hospital, mechanical ventilation (MV) support, and mortality were recorded and analyzed. Vitamin D deficiency (25(OH)D < 20 ng/mL) was found in 73.10% of all study population. Multiple logistic regression was used after adjusted covariances such as age, gender, diabetes, hypertension, and chronic kidney disease (CKD). No statistically significant was shown for ICU admission [Odd Ratio, OR 1.25 (95% confidence interval,) p = 0.70], MV support [Odd Ratio, OR 3.12 (95% confidence interval, CI 0.74-13.21) p = 0.12] and mortality [Odd Ratio, OR 2.39 (95% confidence interval, CI 0.31-18.11), p = 0.40]. These data didn't support the association between serum 25(OH)D and the severity of the disease among hospitalized COVID-19 patients.
Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Data Availability Statement: The data that support the findings of this study are available from [King Faisal Hospital, Al Noor Specialist Hospital, and from Complex King Faisal Hospital] but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.
Conflicts of Interest: The authors declare no conflict of interest. The funders had no role in the design of the study, in the collection, analyses, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
References
Al-Daghri, Al-Saleh, Aljohani, Sulimani, Al-Othman et al., Vitamin D status correction in Saudi Arabia: An experts' consensus under the auspices of the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis, and Musculoskeletal Diseases (ESCEO), Arch. Osteoporos, doi:10.1007/s11657-016-0295-y
Al-Daghri, Vitamin D in Saudi Arabia: Prevalence, distribution and disease associations, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2016.12.017
Alguwaihes, Al-Sofiani, Megdad, Albader, Alsari et al., Diabetes and Covid-19 among hospitalized patients in Saudi Arabia: A single-centre retrospective study, Cardiovasc. Diabetol, doi:10.1186/s12933-020-01184-4
Alguwaihes, Sabico, Hasanato, Al-Sofiani, Megdad et al., Severe vitamin D deficiency is not related to SARS-CoV-2 infection but may increase mortality risk in hospitalized adults: A retrospective case-control study in an Arab Gulf country, Aging Clin. Exp. Res, doi:10.1007/s40520-021-01831-0
Annweiler, Corvaisier, Gautier, Dubée, Legrand et al., Vitamin D Supplementation Associated to Better Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study, Nutrients, doi:10.3390/nu12113377
Anwar, Hamdy, Taher, Fawzy, Abdulattif et al., Burden and Outcome of Vitamin D Deficiency Among Critically Ill Patients: A Prospective Study, Nutr. Clin. Pract, doi:10.1177/0884533616671741
Boonstra, Barrat, Crain, Heath, Savelkoul et al., 25-Dihydroxyvitamin D3 Has a Direct Effect on Naive CD4+ T Cells to Enhance the Development of Th2 Cells, J. Immunol, doi:10.4049/jimmunol.167.9.4974
Carpagnano, Di Lecce, Quaranta, Zito, Buonamico et al., Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J. Endocrinol. Investig, doi:10.1007/s40618-020-01370-x
Castillo, Manuel, Costa, Bouillon, Francisco, Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J. Steroid Biochem. Mol. Biol
Chen, Zhou, Dong, Qu, Gong et al., Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study, Lancet
Cui, Xu, Li, Qiao, Han et al., Vitamin D receptor activation regulates microglia polarization and oxidative stress in spontaneously hypertensive rats and angiotensin II-exposed microglial cells: Role of renin-angiotensin system, Redox Biol, doi:10.1016/j.redox.2019.101295
Demir, Demir, Aygun, Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease, J. Med. Virol, doi:10.1002/jmv.26832
Francis, Ghany, Gilkes, Umakanthan, Review of COVID-19 vaccine subtypes, efficacy and geographical distributions, Postgrad. Med. J, doi:10.1136/postgradmedj-2021-140654
Gombart, Pierre, Maggini, A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection, Nutrients, doi:10.3390/nu12010236
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Hernández, Nan, Fernandez-Ayala, García-Unzueta, Hernández-Hernández et al., Vitamin D Status in Hospitalized Patients with SARS-CoV-2
Honardoost, Ghavideldarestani, Khamseh, Role of vitamin D in pathogenesis and severity of COVID-19 infection, Arch. Physiol. Biochem, doi:10.1080/13813455.2020.1792505
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01570-8
Kostoglou-Athanassiou, Athanassiou, Chronaiou, Michou, Dadiras et al., Vitamin D deficiency and comorbid conditions, Bone, doi:10.1016/j.bone.2010.04.578
Lemire, Adams, Kermani-Arab, Bakke, Sakai et al., 1,25-Dihydroxyvitamin D3 suppresses human T helper/inducer lymphocyte activity in vitro, J. Immunol
Madden, Feldman, Chun, Smith, Sullivan et al., Critically ill children have low vitamin D-binding protein, influencing bioavailability of vitamin D, Ann. Am. Thorac. Soc, doi:10.1513/AnnalsATS.201503-160OC
Maruotti, Cantatore, Vitamin D and the Immune System, J. Rheumatol, doi:10.3899/jrheum.090797
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: An Israeli population-based study, FEBS J, doi:10.1111/febs.15495
Ong, Saw, Sahabdeen, Tey, Ho et al., Current 25-hydroxyvitamin D assays: Do they pass the test?, Clin. Chim. Acta, doi:10.1016/j.cca.2012.03.009
Orchard, Baldry, Nasim-Mohi, Monck, Saeed et al., Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients, Clin. Chem. Lab. Med, doi:10.1515/cclm-2020-1567
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity: Results of a local audit of practice, Clin. Endocrinol, doi:10.1111/cen.14276
Pos, Deficieincy in 25-Hydroxyvitamin D and 30-Day Mortality In Patients with Severe Sepsis and Septic Shock, Am. J. Crit. Care
Prietl, Treiber, Pieber, Amrein, Vitamin D and Immune Function, Nutrients, doi:10.3390/nu5072502
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger et al., Vitamin D Deficiency and Outcome of COVID-19 Patients, Nutrients, doi:10.3390/nu12092757
Rhodes, Subramanian, Laird, Griffin, Kenny, Perspective: Vitamin D deficiency and COVID-19 severity-Plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis, J. Intern. Med, doi:10.1111/joim.13149
Szeto, Zucker, Lasota, Rubin, Walker et al., Vitamin D Status and COVID-19 Clinical Outcomes in Hospitalized Patients, Endocr. Res, doi:10.1080/07435800.2020.1867162
Wang, Hu, Hu, Zhu, Liu et al., Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China, JAMA, doi:10.1001/jama.2020.1585
Wang, Wang, Ye, Liu, Review of the 2019 novel coronavirus (SARS-CoV-2) based on current evidence, Int. J. Antimicrob. Agents, doi:10.1016/j.ijantimicag.2020.105948
Who, Naming the Coronavirus Disease (COVID-19) and the Virus Tthat Causes It
Who, WHO Director-General's Opening Remarks at the Media Briefing on COVID-19-11
Wu, Chen, Cai, Xia, Zhou et al., Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China, JAMA Intern. Med, doi:10.1001/jamainternmed.2020.0994
Yang, Peng, Wang, Guan, Jiang et al., The deadly coronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China, J. Autoimmun, doi:10.1016/j.jaut.2020.102434
Zarooni, Al Marzouqi, Al Darmaki, Prinsloo, Nagelkerke, Prevalence of vitamin D deficiency and associated comorbidities among Abu Dhabi Emirates population, BMC Res. Notes, doi:10.1186/s13104-019-4536-1
Zdrenghea, Makrinioti, Bagacean, Bush, Johnston et al., Vitamin D modulation of innate immune responses to respiratory viral infections, Rev. Med. Virol, doi:10.1002/rmv.1909
Zheng, Peng, Xu, Zhao, Liu et al., Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis, J. Infect, doi:10.1016/j.jinf.2020.04.021
DOI record:
{
"DOI": "10.3390/ijerph19031901",
"ISSN": [
"1660-4601"
],
"URL": "http://dx.doi.org/10.3390/ijerph19031901",
"abstract": "<jats:p>The coronaviruses disease 2019 (COVID-19) spreads continuously worldwide. The new vaccines and drugs have been approved. The prevention of disease is crucial, and some studies reveal the promising effect of alternative therapies such as vitamin D supplementations on COVID-19 prevention, but they still require sufficient evidence. Therefore, the current retrospective multicenter cross-sectional study aims to determine the primary association between the vitamin D status of hospitalized COVID-19 and its severity as well as mortality. A total of 197 COVID-19 were admitted at King Faisal Hospital, Al Noor Specialist Hospital in Makkah, and at Complex King Faisal Hospital in Taif in the Westering region of Saudi Arabia (SA) between June and August 2020. The demographic and clinical characteristics, laboratory tests included serum 25(OH)D and admission for intensive care unit (ICU), length of stay in the hospital, mechanical ventilation (MV) support, and mortality were recorded and analyzed. Vitamin D deficiency (25(OH)D < 20 ng/mL) was found in 73.10% of all study population. Multiple logistic regression was used after adjusted covariances such as age, gender, diabetes, hypertension, and chronic kidney disease (CKD). No statistically significant was shown for ICU admission [Odd Ratio, OR 1.25 (95% confidence interval, CI 0.41–3.88) p = 0.70], MV support [Odd Ratio, OR 3.12 (95% confidence interval, CI 0.74–13.21) p = 0.12] and mortality [Odd Ratio, OR 2.39 (95% confidence interval, CI 0.31–18.11), p = 0.40]. These data didn’t support the association between serum 25(OH)D and the severity of the disease among hospitalized COVID-19 patients.</jats:p>",
"alternative-id": [
"ijerph19031901"
],
"author": [
{
"affiliation": [],
"family": "Bushnaq",
"given": "Taqwa",
"sequence": "first"
},
{
"affiliation": [],
"family": "Algethami",
"given": "Fadiyah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Qadhi",
"given": "Alaa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mustafa",
"given": "Reham",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9420-3666",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ghafouri",
"given": "Khloud",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Azhar",
"given": "Wedad",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4753-8938",
"affiliation": [],
"authenticated-orcid": false,
"family": "Malki",
"given": "Asma Al",
"sequence": "additional"
}
],
"container-title": [
"International Journal of Environmental Research and Public Health"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
2,
9
]
],
"date-time": "2022-02-09T04:37:48Z",
"timestamp": 1644381468000
},
"deposited": {
"date-parts": [
[
2022,
2,
9
]
],
"date-time": "2022-02-09T04:56:51Z",
"timestamp": 1644382611000
},
"indexed": {
"date-parts": [
[
2022,
2,
10
]
],
"date-time": "2022-02-10T21:42:58Z",
"timestamp": 1644529378026
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "1660-4601"
}
],
"issue": "3",
"issued": {
"date-parts": [
[
2022,
2,
8
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2022,
2
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
2,
8
]
],
"date-time": "2022-02-08T00:00:00Z",
"timestamp": 1644278400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1660-4601/19/3/1901/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1901",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
2,
8
]
]
},
"published-online": {
"date-parts": [
[
2022,
2,
8
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105948",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"key": "ref3"
},
{
"key": "ref4"
},
{
"DOI": "10.1016/j.jaut.2020.102434",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1016/S0140-6736(20)30211-7",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1001/jama.2020.1585",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1136/postgradmedj-2021-140654",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1080/13813455.2020.1792505",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1002/rmv.1909",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.3390/nu12010236",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"article-title": "1,25-Dihydroxyvitamin D3 suppresses human T helper/inducer lymphocyte activity in vitro",
"author": "Lemire",
"first-page": "3032",
"journal-title": "J. Immunol.",
"key": "ref14",
"volume": "134",
"year": "1985"
},
{
"DOI": "10.4049/jimmunol.167.9.4974",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1016/j.redox.2019.101295",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1111/joim.13149",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1111/febs.15495",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1007/s40618-020-01370-x",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1111/cen.14276",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1007/s40520-021-01831-0",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1016/j.jsbmb.2016.12.017",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1016/j.cca.2012.03.009",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1007/s11657-016-0295-y",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1186/s12933-020-01184-4",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1016/j.bone.2010.04.578",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1186/s13104-019-4536-1",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1016/j.jinf.2020.04.021",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1080/07435800.2020.1867162",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1210/clinem/dgaa733",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"article-title": "Deficieincy in 25-Hydroxyvitamin D and 30-Day Mortality In Patients with Severe Sepsis and Septic Shock",
"author": "Pos",
"first-page": "1",
"journal-title": "Am. J. Crit. Care",
"key": "ref32",
"volume": "23",
"year": "1978"
},
{
"DOI": "10.1177/0884533616671741",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.3390/nu12092757",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1515/cclm-2020-1567",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1002/jmv.26832",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"article-title": "Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study",
"author": "Castillo",
"first-page": "2",
"journal-title": "J. Steroid Biochem. Mol. Biol.",
"key": "ref37",
"volume": "203",
"year": "2020"
},
{
"DOI": "10.3390/nu12113377",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.3899/jrheum.090797",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.3390/nu5072502",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1513/AnnalsATS.201503-160OC",
"doi-asserted-by": "publisher",
"key": "ref41"
}
],
"reference-count": 41,
"references-count": 41,
"relation": {},
"score": 1,
"short-container-title": [
"IJERPH"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Health, Toxicology and Mutagenesis",
"Public Health, Environmental and Occupational Health"
],
"subtitle": [],
"title": [
"The Impact of Vitamin D Status on COVID-19 Severity among Hospitalized Patients in the Western Region of Saudi Arabia: A Retrospective Cross-Sectional Study"
],
"type": "journal-article",
"volume": "19"
}
