Higher Adherence to the Mediterranean Dietary Pattern Is Inversely Associated With Severity of COVID-19 and Related Symptoms: A Cross-Sectional Study
et al., Frontiers in Medicine, doi:10.3389/fmed.2022.911273, Jul 2022
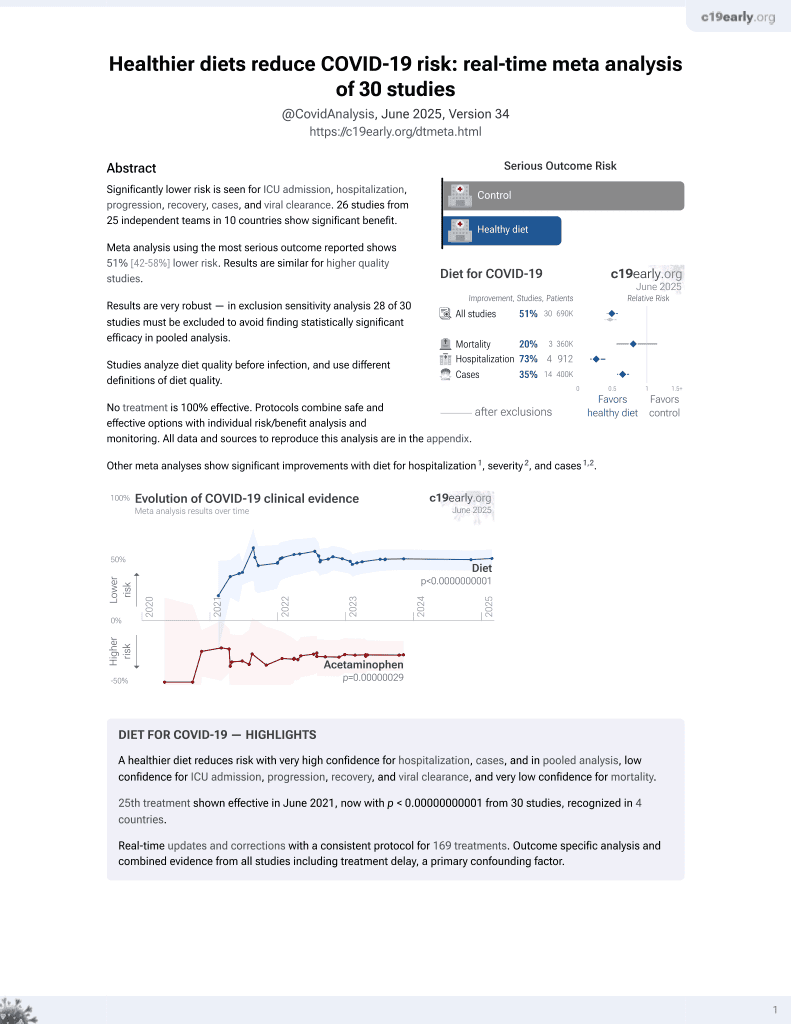
Diet for COVID-19
26th treatment shown to reduce risk in
June 2021, now with p < 0.00000000001 from 30 studies, recognized in 4 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 250 COVID-19 patients in Iran, showing lower risk of severe disease with greater adherence to a Mediterranean diet.
|
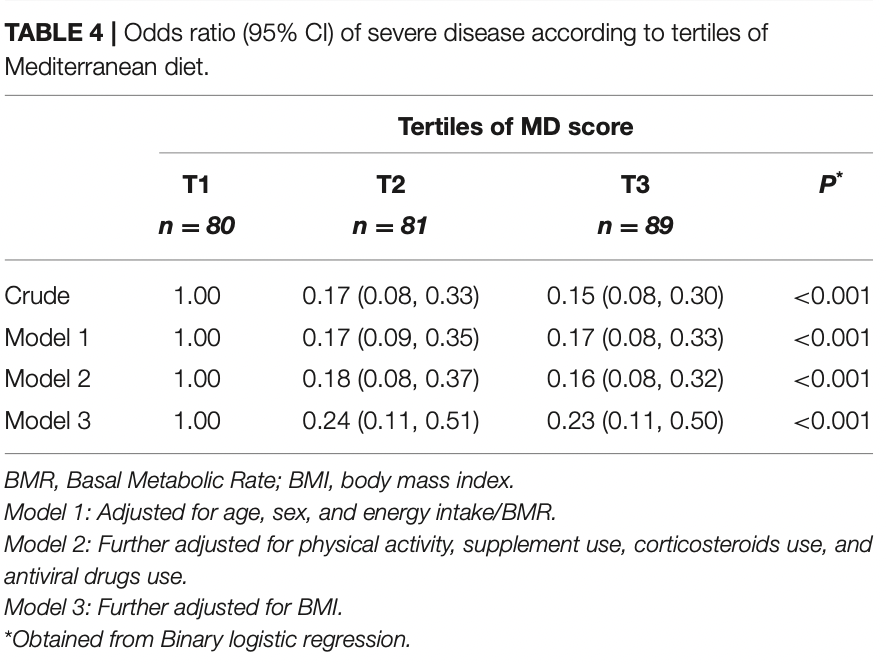
risk of severe case, 77.0% lower, OR 0.23, p < 0.001, higher quality diet 89, lower quality diet 80, adjusted per study, top tertile vs. lowest tertile, MD score, model 3, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Zargarzadeh et al., 19 Jul 2022, retrospective, Iran, peer-reviewed, mean age 44.1, 11 authors, study period June 2021 - September 2021.
Contact: amkhv@yahoo.com.
Higher Adherence to the Mediterranean Dietary Pattern Is Inversely Associated With Severity of COVID-19 and Related Symptoms: A Cross-Sectional Study
Frontiers in Medicine, doi:10.3389/fmed.2022.911273
Background and Aims: Adherence to the Mediterranean diet (MD) has been associated with a decreased risk of developing a variety of chronic diseases that are comorbidities in COVID-19 patients. However, its association to the severity and symptoms of COVID-19 are still unknown. This study aimed to examine the association between adherence to the MD pattern and COVID-19 severity and symptoms in Iranian hospitalized patients. Methods: In this cross-sectional study, 250 COVID-19 patients aged 18 to 65 were examined. We employed a food frequency questionnaire (FFQ) to obtain data on dietary intake of participants in the year prior to their COVID-19 diagnosis. COVID-19 severity was determined using the National Institutes of Health's Coronavirus Disease 2019 report. Additionally, symptoms associated with COVID-19, inflammatory markers, and other variables were evaluated. The scoring method proposed by Trichopoulou et al. was used to assess adherence to the MD.
Results: The participants' mean age was 44.1 ± 12.1 years, and 46% of them had severe COVID-19. Patients who adhered more closely to the MD had lower serum C-reactive protein levels (7.80 vs. 37.36 mg/l) and erythrocyte sedimentation rate (14.08 vs. 42.65 mm/h). Those with the highest MD score were 77% less likely to have severe COVID-19 after controlling for confounding variables. The MD score was also found to be inversely associated with COVID-19 symptoms, including dyspnea, cough, fever, chills, weakness, myalgia, nausea and vomiting, and sore throat.
Conclusion: Higher adherence to the MD was associated with a decreased likelihood of COVID-19 severity and symptoms, as well as a shorter duration of hospitalization and convalescence, and inflammatory biomarkers.
ETHICS STATEMENT The studies involving human participants were reviewed and approved by Kashan University of Medical Sciences, IR.KAUMS.MEDNT.REC.1400.048. The patients/participants provided their written informed consent to participate in this study.
AUTHOR CONTRIBUTIONS NZ and SM: conceptualization, formal analysis, writing original draft, and writing review and editing. AE, MT, HK, and CA: data collection. AM: supervision, conceptualization, methodology, investigation, funding acquisition, formal analysis, writing original draft, and writing review and editing. HS, FT, HC, and KV: writing review and editing. All authors contributed to the article and approved the submitted version.
SUPPLEMENTARY MATERIAL The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed. 2022.911273/full#supplementary-material
Conflict of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Publisher's Note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Andrade, Jorge, García-Conesa, Philippou, Massaro et al., Mediterranean diet adherence and subjective well-being in a sample of Portuguese adults, Nutrients, doi:10.3390/nu12123837
Angelidi, Kokkinos, Katechaki, Mantzoros, Mediterranean diet as a nutritional approach for COVID-19, Metabolism, doi:10.1016/j.metabol.2020.154407
Antwi, Appiah, Oluwakuse, Abu, The nutrition-COVID-19 interplay: a review, Curr Nutr Rep, doi:10.1007/s13668-021-00380-2
Aronis, Vamvini, Chamberland, Sweeney, Brennan et al., Short-term walnut consumption increases circulating total adiponectin and apolipoprotein A concentrations, but does not affect markers of inflammation or vascular injury in obese humans with the metabolic syndrome: data from a double-blinded, randomized, placebo-controlled study, Metabolism, doi:10.1016/j.metabol.2011.09.008
Billingsley, Carbone, The antioxidant potential of the Mediterranean diet in patients at high cardiovascular risk: an in-depth review of the PREDIMED, Nutr Diabetes, doi:10.1038/s41387-018-0025-1
Bray, Bell, Liang, Haykal, Kaiksow et al., Erythrocyte sedimentation rate and C-reactive protein measurements and their relevance in clinical medicine, WMJ
Caldera-Crespo, Paidas, Roy, Schulman, Kenyon et al., Experimental models of COVID-19, Front Cell Infect Microbiol, doi:10.3389/fcimb.2021.792584
Canales, Sánchez-Muniz, Bastida, Librelotto, Nus et al., Effect of walnut-enriched meat on the relationship between VCAM, ICAM, and LTB4 levels and PON-1 activity in ApoA4 360 and PON-1 allele carriers at increased cardiovascular risk, Eur J Clin Nutr, doi:10.1038/ejcn.2011.20
Cascella, Rajnik, Aleem, Dulebohn, Napoli, Features, Evaluation, and Treatment of Coronavirus (COVID-19)
Cruz, Cervantes, Juárez, COVID-19, a worldwide public health emergency, Rev Clin Esp, doi:10.1016/j.rceng.2020.03.001
Dahle, Ostendorf, Zaman, Pan, Melanson et al., Underreporting of energy intake in weight loss maintainers, Am J Clin Nutr, doi:10.1093/ajcn/nqab012
De Souza, Schincaglia, Pimentel, Mota, Nuts and human health outcomes: a systematic review, Nutrients, doi:10.3390/nu9121311
Detopoulou, Al-Khelefawi, Kalonarchi, Papamikos, Formulation of the menu of a general hospital after its conversion to a "COVID Hospital": a nutrient analysis of 28-day menus, Front Nutr, doi:10.3389/fnut.2022.833628
Detopoulou, Demopoulos, Antonopoulou, Micronutrients, phytochemicals and Mediterranean diet: a potential protective role against COVID-19 through Modulation of PAF actions and metabolism, Nutrients, doi:10.3390/nu13020462
Dos, Quadros, Weschenfelder, Garofallo, Marcadenti, Oxidative stress biomarkers, nut-related antioxidants, and cardiovascular disease, Nutrients, doi:10.3390/nu12030682
Estruch, Martínez-González, Salas-Salvadó, Ruiz-Gutiérrez, Covas, Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial, Ann Intern Med, doi:10.7326/0003-4819-145-1-200607040-00004
Estruch, Salas-Salvadó, Covas, Corella, Arós, Primary prevention of cardiovascular disease with a mediterranean diet supplemented with extra-virgin olive oil or nuts, N Engl J Med, doi:10.1056/NEJMoa1800389
Ferro, Pujia, Maurotti, Boragina, Mirarchi et al., Mediterranean diet a potential strategy against SARS-CoV-2 infection: a narrative review, Medicina, doi:10.3390/medicina57121389
Fitó, Guxens, Corella, Sáez, Estruch et al., Effect of a traditional Mediterranean diet on lipoprotein oxidation: a randomized controlled trial, Arch Intern Med, doi:10.1001/archinte.167.11.1195
Fritsche, The science of fatty acids and inflammation, Adv Nutr, doi:10.3945/an.114.006940
Gotsis, Anagnostis, Mariolis, Vlachou, Katsiki et al., Health benefits of the Mediterranean diet: an update of research over the last 5 years, Angiology, doi:10.1177/0003319714532169
Guasch-Ferré, Salas-Salvadó, Estruch, Corella, Fitó, The PREDIMED trial, Mediterranean diet and health outcomes: how strong is the evidence?, Nutr Metab Cardiovasc Dis, doi:10.1016/j.numecd.2017.05.004
Hidalgo-Mora, García-Vigara, Sánchez-Sánchez, García-Pérez, Tarín et al., The mediterranean diet: a historical perspective on food for health, Maturitas, doi:10.1016/j.maturitas.2019.12.002
Hou, Su, Chao, COVID-19 illness severity in the elderly in relation to vegetarian and non-vegetarian diets: a single-center experience, Front Nutr, doi:10.3389/fnut.2022.837458
Hu, Huang, Yin, The cytokine storm and COVID-19, J Med Virol, doi:10.1002/jmv.26232
Kaye, Okeagu, Pham, Silva, Hurley et al., Economic impact of COVID-19 pandemic on healthcare facilities and systems: international perspectives, Best Pract Res Clin Anaesthesiol, doi:10.1016/j.bpa.2020.11.009
Kim, Rebholz, Hegde, Lafiura, Raghavan et al., Plant-based diets, pescatarian diets and COVID-19 severity: a populationbased case-control study in six countries, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2021-000272
Kris-Etherton, Krauss, Public health guidelines should recommend reducing saturated fat consumption as much as possible: YES, Am J Clin Nutr, doi:10.1093/ajcn/nqaa110
Lee, Sohn, Rhee, Hwang, Saturated fatty acids, but not unsaturated fatty acids, induce the expression of cyclooxygenase-2 mediated through toll-like receptor 4, J Biol Chem, doi:10.1074/jbc.M011695200
Ling, Zabetakis, The role of an anti-inflammatory diet in conjunction to COVID-19, Diseases, doi:10.3390/diseases9040076
Logue, Franko, Mcculloch, Mcdonald, Magedson et al., Sequelae in adults at 6 months after COVID-19 infection, JAMA Network Open, doi:10.1001/jamanetworkopen.2021.0830
Lozano, Perez-Martinez, Marin, Tinahones, Delgado-Lista et al., An acute intake of a walnut-enriched meal improves postprandial adiponectin response in healthy young adults, Nutr Res, doi:10.1016/j.nutres.2013.08.010
Martínez-González, Salas-Salvadó, Estruch, Corella, Fitó, Benefits of the mediterranean diet: insights from the PREDIMED study, Prog Cardiovasc Dis, doi:10.1016/j.pcad.2015.04.003
Medina-Remón, Casas, Tressserra-Rimbau, Martínez-González, Fitó, Polyphenol intake from a Mediterranean diet decreases inflammatory biomarkers related to atherosclerosis: a substudy of the PREDIMED trial, Br J Clin Pharmacol, doi:10.1111/bcp.12986
Mirmiran, Esfahani, Mehrabi, Hedayati, Azizi, Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study, Public Health Nutr, doi:10.1017/S1368980009991698
Mousavi, Djafarian, Mojtahed, Varkaneh, Shab-Bidar, The effect of zinc supplementation on plasma C-reactive protein concentrations: A systematic review and meta-analysis of randomized controlled trials, Eur J Pharmacol, doi:10.1016/j.ejphar.2018.07.019
Murai, Fernandes, Sales, Pinto, Goessler et al., Effect of a single high dose of Vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial, JAMA, doi:10.1001/jama.2020.26848
Nalbandian, Sehgal, Gupta, Madhavan, Mcgroder et al., Post-acute COVID-19 syndrome, Nat Med, doi:10.1038/s41591-021-01283-z
Panossian, Brendler, The role of adaptogens in prophylaxis and treatment of viral respiratory infections, Pharmaceuticals, doi:10.3390/ph13090236
Peramo-Álvarez, López-Zúñiga, López-Ruz, Medical sequels of COVID-19, Med Clin, doi:10.1016/j.medcle.2021.04.008
Rando, Wellhausen, Ghosh, Lee, Dattoli et al., Identification and development of therapeutics for COVID-19, Msystems, doi:10.1128/mSystems.00233-21
Ruiz-Núñez, Da, Muskiet, The relation of saturated fatty acids with low-grade inflammation and cardiovascular disease, J Nutr Biochem, doi:10.1016/j.jnutbio.2015.12.007
Ruiz-Roso, Knott-Torcal, Matilla-Escalante, Garcimartín, Sampedro-Nuñez et al., COVID-19 lockdown and changes of the dietary pattern and physical activity habits in a cohort of patients with type 2 diabetes mellitus, Nutrients, doi:10.3390/nu12082327
Sadighara, Ghanati, The aflatoxin B1 content of peanut-based foods in Iran: a systematic review, Rev Environ Health, doi:10.1515/reveh-2021-0065
Salas-Salvadó, Bulló, Pérez-Heras, Dietary fibre, nuts and cardiovascular diseases, Br J Nutr, doi:10.1017/BJN20061863
Santos, Genario, Gomes, Schoenfeld, Cherry intake as a dietary strategy in sport and diseases: a review of clinical applicability and mechanisms of action, Crit Rev Food Sci Nutr
Santos, Tinsley, Da Silva, Bueno, Pharmaconutrition in the clinical management of COVID-19: a lack of evidence-based research but clues to personalized prescription, J Pers Med, doi:10.3390/jpm10040145
Schofield, Predicting basal metabolic rate, new standards and review of previous work, Hum Nutr Clin Nutr
Sinha, Matthay, Calfee, Is a "Cytokine Storm" relevant to COVID-19?, JAMA Intern Med, doi:10.1001/jamainternmed.2020.3313
Slaats, Oever, Van De Veerdonk, Netea, IL-1β/IL-6/CRP and IL-18/ferritin: distinct inflammatory programs in infections, PLoS Pathog, doi:10.1371/journal.ppat.1005973
Sy, Nutraceuticals of anti-inflammatory activity as complementary therapy for rheumatoid arthritis, Toxicol Ind Health, doi:10.1177/0748233712462468
Thomas, Patel, Bittel, Wolski, Wang et al., Effect of high-dose zinc and ascorbic acid supplementation vs usual care on symptom length and reduction among ambulatory patients with SARS-CoV-2 infection: the COVID A to Z randomized clinical trial, JAMA Network Open, doi:10.1001/jamanetworkopen.2021.0369
Tresserra-Rimbau, Medina-Remón, Pérez-Jiménez, Martínez-González, Covas et al., Dietary intake and major food sources of polyphenols in a Spanish population at high cardiovascular risk: the PREDIMED study, Nutr Metab Cardiovasc Dis, doi:10.1016/j.numecd.2012.10.008
Trichopoulou, Costacou, Bamia, Trichopoulos, Adherence to a Mediterranean diet and survival in a Greek population, N Engl J Med, doi:10.1056/NEJMoa025039
Tuczyńska, Matthews-Kozanecka, Baum, Accessibility to non-COVID health services in the world during the COVID-19 pandemic: review, Front Public Health, doi:10.3389/fpubh.2021.760795
Urpi-Sarda, Casas, Chiva-Blanch, Romero-Mamani, Valderas-Martínez et al., Virgin olive oil and nuts as key foods of the Mediterranean diet effects on inflammatory biomakers related to atherosclerosis, Pharmacol Res, doi:10.1016/j.phrs.2012.03.006
Wang, Zhang, Hou, Liu, Wang et al., The effects of pomegranate supplementation on biomarkers of inflammation and endothelial dysfunction: A meta-analysis and systematic review, Complement Ther Med
Ye, Wang, Mao, The pathogenesis and treatment of the 'Cytokine Storm' in COVID-19, J Infect, doi:10.1016/j.jinf.2020.03.037
Zabetakis, Lordan, Norton, Tsoupras, COVID-19: The inflammation link and the role of nutrition in potential mitigation, Nutrients, doi:10.3390/nu12051466
Zargarzadeh, Severo, Pizarro, Persad, Mousavi, The effects of folic acid supplementation on pro-inflammatory mediators: a systematic review and dose-response meta-analysis of randomized controlled trials, Clin Ther, doi:10.1016/j.clinthera.2021.10.002
DOI record:
{
"DOI": "10.3389/fmed.2022.911273",
"ISSN": [
"2296-858X"
],
"URL": "http://dx.doi.org/10.3389/fmed.2022.911273",
"abstract": "<jats:sec><jats:title>Background and Aims</jats:title><jats:p>Adherence to the Mediterranean diet (MD) has been associated with a decreased risk of developing a variety of chronic diseases that are comorbidities in COVID-19 patients. However, its association to the severity and symptoms of COVID-19 are still unknown. This study aimed to examine the association between adherence to the MD pattern and COVID-19 severity and symptoms in Iranian hospitalized patients.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>In this cross-sectional study, 250 COVID-19 patients aged 18 to 65 were examined. We employed a food frequency questionnaire (FFQ) to obtain data on dietary intake of participants in the year prior to their COVID-19 diagnosis. COVID-19 severity was determined using the National Institutes of Health's Coronavirus Disease 2019 report. Additionally, symptoms associated with COVID-19, inflammatory markers, and other variables were evaluated. The scoring method proposed by Trichopoulou et al. was used to assess adherence to the MD.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>The participants' mean age was 44.1 ± 12.1 years, and 46% of them had severe COVID-19. Patients who adhered more closely to the MD had lower serum C-reactive protein levels (7.80 vs. 37.36 mg/l) and erythrocyte sedimentation rate (14.08 vs. 42.65 mm/h). Those with the highest MD score were 77% less likely to have severe COVID-19 after controlling for confounding variables. The MD score was also found to be inversely associated with COVID-19 symptoms, including dyspnea, cough, fever, chills, weakness, myalgia, nausea and vomiting, and sore throat.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>Higher adherence to the MD was associated with a decreased likelihood of COVID-19 severity and symptoms, as well as a shorter duration of hospitalization and convalescence, and inflammatory biomarkers.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fmed.2022.911273"
],
"author": [
{
"affiliation": [],
"family": "Zargarzadeh",
"given": "Nikan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Tadbir Vajargah",
"given": "Kiana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ebrahimzadeh",
"given": "Armin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mousavi",
"given": "Seyed Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Khodaveisi",
"given": "Hamidreza",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Akhgarjand",
"given": "Camellia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Toyos",
"given": "Fernando M. P.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cerqueira",
"given": "Henrique S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Santos",
"given": "Heitor O.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Taghizadeh",
"given": "Mohsen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Milajerdi",
"given": "Alireza",
"sequence": "additional"
}
],
"container-title": "Frontiers in Medicine",
"container-title-short": "Front. Med.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2022,
7,
19
]
],
"date-time": "2022-07-19T05:06:43Z",
"timestamp": 1658207203000
},
"deposited": {
"date-parts": [
[
2022,
7,
19
]
],
"date-time": "2022-07-19T05:06:51Z",
"timestamp": 1658207211000
},
"indexed": {
"date-parts": [
[
2022,
7,
19
]
],
"date-time": "2022-07-19T05:41:46Z",
"timestamp": 1658209306043
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
7,
19
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
7,
19
]
],
"date-time": "2022-07-19T00:00:00Z",
"timestamp": 1658188800000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2022.911273/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2022,
7,
19
]
]
},
"published-online": {
"date-parts": [
[
2022,
7,
19
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"author": "Cascella",
"key": "B1",
"volume-title": "Features, Evaluation, and Treatment of Coronavirus (COVID-19)",
"year": "2022"
},
{
"DOI": "10.3389/fcimb.2021.792584",
"article-title": "Experimental models of COVID-19",
"author": "Caldera-Crespo",
"doi-asserted-by": "publisher",
"first-page": "792584",
"journal-title": "Front Cell Infect Microbiol",
"key": "B2",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.3389/fpubh.2021.760795",
"article-title": "Accessibility to non-COVID health services in the world during the COVID-19 pandemic: review",
"author": "Tuczyńska",
"doi-asserted-by": "publisher",
"first-page": "760795",
"journal-title": "Front Public Health.",
"key": "B3",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.bpa.2020.11.009",
"article-title": "Economic impact of COVID-19 pandemic on healthcare facilities and systems: international perspectives",
"author": "Kaye",
"doi-asserted-by": "publisher",
"first-page": "293",
"journal-title": "Best Pract Res Clin Anaesthesiol.",
"key": "B4",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1016/j.rceng.2020.03.001",
"article-title": "COVID-19, a worldwide public health emergency",
"author": "Palacios Cruz",
"doi-asserted-by": "publisher",
"first-page": "55",
"journal-title": "Rev Clin Esp.",
"key": "B5",
"volume": "221",
"year": "2021"
},
{
"DOI": "10.1038/s41591-021-01283-z",
"article-title": "Post-acute COVID-19 syndrome",
"author": "Nalbandian",
"doi-asserted-by": "publisher",
"first-page": "601",
"journal-title": "Nat Med.",
"key": "B6",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/j.medcle.2021.04.008",
"article-title": "Medical sequels of COVID-19",
"author": "Peramo-Álvarez",
"doi-asserted-by": "publisher",
"first-page": "388",
"journal-title": "Med Clin.",
"key": "B7",
"volume": "157",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.0830",
"article-title": "Sequelae in adults at 6 months after COVID-19 infection",
"author": "Logue",
"doi-asserted-by": "crossref",
"key": "B8",
"volume-title": "JAMA Network Open",
"year": "2021"
},
{
"DOI": "10.1128/mSystems.00233-21",
"article-title": "Identification and development of therapeutics for COVID-19",
"author": "Rando",
"doi-asserted-by": "publisher",
"first-page": "e00233",
"journal-title": "Msystems.",
"key": "B9",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.3390/jpm10040145",
"article-title": "Pharmaconutrition in the clinical management of COVID-19: a lack of evidence-based research but clues to personalized prescription",
"author": "Santos",
"doi-asserted-by": "publisher",
"first-page": "145",
"journal-title": "J Pers Med.",
"key": "B10",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1007/s13668-021-00380-2",
"article-title": "The nutrition-COVID-19 interplay: a review",
"author": "Antwi",
"doi-asserted-by": "publisher",
"first-page": "364",
"journal-title": "Curr Nutr Rep.",
"key": "B11",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1001/jamainternmed.2020.3313",
"article-title": "Is a “Cytokine Storm” relevant to COVID-19?",
"author": "Sinha",
"doi-asserted-by": "publisher",
"first-page": "1152",
"journal-title": "JAMA Intern Med.",
"key": "B12",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26232",
"article-title": "The cytokine storm and COVID-19",
"author": "Hu",
"doi-asserted-by": "publisher",
"first-page": "250",
"journal-title": "J Med Virol.",
"key": "B13",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1177/0748233712462468",
"article-title": "Nutraceuticals of anti-inflammatory activity as complementary therapy for rheumatoid arthritis",
"author": "Al-Okbi",
"doi-asserted-by": "publisher",
"first-page": "738",
"journal-title": "Toxicol Ind Health.",
"key": "B14",
"volume": "30",
"year": "2014"
},
{
"DOI": "10.1016/j.ejphar.2018.07.019",
"article-title": "The effect of zinc supplementation on plasma C-reactive protein concentrations: A systematic review and meta-analysis of randomized controlled trials",
"author": "Mousavi",
"doi-asserted-by": "publisher",
"first-page": "10",
"journal-title": "Eur J Pharmacol.",
"key": "B15",
"volume": "834",
"year": "2018"
},
{
"DOI": "10.1016/j.clinthera.2021.10.002",
"article-title": "The effects of folic acid supplementation on pro-inflammatory mediators: a systematic review and dose–response meta-analysis of randomized controlled trials",
"author": "Zargarzadeh",
"doi-asserted-by": "publisher",
"first-page": "e346",
"journal-title": "Clin Ther.",
"key": "B16",
"volume": "43",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.0369",
"article-title": "Effect of high-dose zinc and ascorbic acid supplementation vs usual care on symptom length and reduction among ambulatory patients with SARS-CoV-2 infection: the COVID A to Z randomized clinical trial",
"author": "Thomas",
"doi-asserted-by": "crossref",
"key": "B17",
"volume-title": "JAMA Network Open",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.26848",
"article-title": "Effect of a single high dose of Vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial",
"author": "Murai",
"doi-asserted-by": "publisher",
"first-page": "1053",
"journal-title": "JAMA.",
"key": "B18",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.3390/nu12082327",
"article-title": "COVID-19 lockdown and changes of the dietary pattern and physical activity habits in a cohort of patients with type 2 diabetes mellitus",
"author": "Ruiz-Roso",
"doi-asserted-by": "publisher",
"first-page": "2327",
"journal-title": "Nutrients.",
"key": "B19",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1136/bmjnph-2021-000272",
"article-title": "Plant-based diets, pescatarian diets and COVID-19 severity: a population-based case–control study in six countries",
"author": "Kim",
"doi-asserted-by": "publisher",
"first-page": "257",
"journal-title": "BMJ Nutr Prev Health.",
"key": "B20",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.3389/fnut.2022.837458",
"article-title": "COVID-19 illness severity in the elderly in relation to vegetarian and non-vegetarian diets: a single-center experience",
"author": "Hou",
"doi-asserted-by": "publisher",
"first-page": "837458",
"journal-title": "Front Nutr",
"key": "B21",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.3390/medicina57121389",
"article-title": "Mediterranean diet a potential strategy against SARS-CoV-2 infection: a narrative review",
"author": "Ferro",
"doi-asserted-by": "publisher",
"first-page": "1389",
"journal-title": "Medicina.",
"key": "B22",
"volume": "57",
"year": "2021"
},
{
"DOI": "10.3390/nu12051466",
"article-title": "COVID-19: The inflammation link and the role of nutrition in potential mitigation",
"author": "Zabetakis",
"doi-asserted-by": "publisher",
"first-page": "1466",
"journal-title": "Nutrients.",
"key": "B23",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3390/diseases9040076",
"article-title": "The role of an anti-inflammatory diet in conjunction to COVID-19",
"author": "Ling",
"doi-asserted-by": "publisher",
"first-page": "76",
"journal-title": "Diseases.",
"key": "B24",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.maturitas.2019.12.002",
"article-title": "The mediterranean diet: a historical perspective on food for health",
"author": "Hidalgo-Mora",
"doi-asserted-by": "publisher",
"first-page": "65",
"journal-title": "Maturitas.",
"key": "B25",
"volume": "132",
"year": "2020"
},
{
"DOI": "10.3390/nu12123837",
"article-title": "Mediterranean diet adherence and subjective well-being in a sample of Portuguese adults",
"author": "Andrade",
"doi-asserted-by": "publisher",
"first-page": "3837",
"journal-title": "Nutrients.",
"key": "B26",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1177/0003319714532169",
"article-title": "Health benefits of the Mediterranean diet: an update of research over the last 5 years",
"author": "Gotsis",
"doi-asserted-by": "publisher",
"first-page": "304",
"journal-title": "Angiology.",
"key": "B27",
"volume": "66",
"year": "2015"
},
{
"DOI": "10.1016/j.metabol.2020.154407",
"article-title": "Mediterranean diet as a nutritional approach for COVID-19",
"author": "Angelidi",
"doi-asserted-by": "publisher",
"first-page": "154407",
"journal-title": "Metabolism.",
"key": "B28",
"volume": "114",
"year": "2021"
},
{
"DOI": "10.1017/S1368980009991698",
"article-title": "Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study",
"author": "Mirmiran",
"doi-asserted-by": "publisher",
"first-page": "654",
"journal-title": "Public Health Nutr.",
"key": "B29",
"volume": "13",
"year": "2010"
},
{
"DOI": "10.1056/NEJMoa025039",
"article-title": "Adherence to a Mediterranean diet and survival in a Greek population",
"author": "Trichopoulou",
"doi-asserted-by": "publisher",
"first-page": "2599",
"journal-title": "N Engl J Med.",
"key": "B30",
"volume": "348",
"year": "2003"
},
{
"key": "B31",
"unstructured": "2021"
},
{
"article-title": "Erythrocyte sedimentation rate and C-reactive protein measurements and their relevance in clinical medicine",
"author": "Bray",
"first-page": "317",
"journal-title": "WMJ.",
"key": "B32",
"volume": "115",
"year": "2016"
},
{
"DOI": "10.1016/j.jinf.2020.03.037",
"article-title": "The pathogenesis and treatment of the ‘Cytokine Storm' in COVID-19",
"author": "Ye",
"doi-asserted-by": "publisher",
"first-page": "607",
"journal-title": "J Infect.",
"key": "B33",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1001/archinte.167.11.1195",
"article-title": "Effect of a traditional Mediterranean diet on lipoprotein oxidation: a randomized controlled trial",
"author": "Fitó",
"doi-asserted-by": "publisher",
"first-page": "1195",
"journal-title": "Arch Intern Med.",
"key": "B34",
"volume": "167",
"year": "2007"
},
{
"DOI": "10.1016/j.phrs.2012.03.006",
"article-title": "Virgin olive oil and nuts as key foods of the Mediterranean diet effects on inflammatory biomakers related to atherosclerosis",
"author": "Urpi-Sarda",
"doi-asserted-by": "publisher",
"first-page": "577",
"journal-title": "Pharmacol Res.",
"key": "B35",
"volume": "65",
"year": "2012"
},
{
"DOI": "10.1016/j.pcad.2015.04.003",
"article-title": "Benefits of the mediterranean diet: insights from the PREDIMED study",
"author": "Martínez-González",
"doi-asserted-by": "publisher",
"first-page": "50",
"journal-title": "Prog Cardiovasc Dis.",
"key": "B36",
"volume": "58",
"year": "2015"
},
{
"DOI": "10.1016/j.numecd.2017.05.004",
"article-title": "The PREDIMED trial, Mediterranean diet and health outcomes: how strong is the evidence?",
"author": "Guasch-Ferré",
"doi-asserted-by": "publisher",
"first-page": "624",
"journal-title": "Nutr Metab Cardiovasc Dis.",
"key": "B37",
"volume": "27",
"year": "2017"
},
{
"DOI": "10.1056/NEJMoa1800389",
"article-title": "Primary prevention of cardiovascular disease with a mediterranean diet supplemented with extra-virgin olive oil or nuts",
"author": "Estruch",
"doi-asserted-by": "publisher",
"first-page": "e34",
"journal-title": "N Engl J Med.",
"key": "B38",
"volume": "378",
"year": "2018"
},
{
"DOI": "10.1038/s41387-018-0025-1",
"article-title": "The antioxidant potential of the Mediterranean diet in patients at high cardiovascular risk: an in-depth review of the PREDIMED",
"author": "Billingsley",
"doi-asserted-by": "publisher",
"first-page": "13",
"journal-title": "Nutr Diabetes.",
"key": "B39",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.7326/0003-4819-145-1-200607040-00004",
"article-title": "Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial",
"author": "Estruch",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Ann Intern Med.",
"key": "B40",
"volume": "145",
"year": "2006"
},
{
"DOI": "10.1111/bcp.12986",
"article-title": "Polyphenol intake from a Mediterranean diet decreases inflammatory biomarkers related to atherosclerosis: a substudy of the PREDIMED trial",
"author": "Medina-Remón",
"doi-asserted-by": "publisher",
"first-page": "114",
"journal-title": "Br J Clin Pharmacol.",
"key": "B41",
"volume": "83",
"year": "2017"
},
{
"DOI": "10.3390/nu13020462",
"article-title": "Micronutrients, phytochemicals and Mediterranean diet: a potential protective role against COVID-19 through Modulation of PAF actions and metabolism",
"author": "Detopoulou",
"doi-asserted-by": "publisher",
"first-page": "462",
"journal-title": "Nutrients",
"key": "B42",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3390/ph13090236",
"article-title": "The role of adaptogens in prophylaxis and treatment of viral respiratory infections",
"author": "Panossian",
"doi-asserted-by": "publisher",
"first-page": "236",
"journal-title": "Pharmaceuticals.",
"key": "B43",
"volume": "13",
"year": "2020"
},
{
"article-title": "Cherry intake as a dietary strategy in sport and diseases: a review of clinical applicability and mechanisms of action",
"author": "Santos",
"first-page": "1",
"key": "B44",
"volume-title": "Crit Rev Food Sci Nutr",
"year": "2020"
},
{
"DOI": "10.1016/j.ctim.2020.102358",
"article-title": "The effects of pomegranate supplementation on biomarkers of inflammation and endothelial dysfunction: A meta-analysis and systematic review",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "102358",
"journal-title": "Complement Ther Med",
"key": "B45",
"volume": "49",
"year": "2020"
},
{
"DOI": "10.1074/jbc.M011695200",
"article-title": "Saturated fatty acids, but not unsaturated fatty acids, induce the expression of cyclooxygenase-2 mediated through toll-like receptor 4",
"author": "Lee",
"doi-asserted-by": "publisher",
"first-page": "16683",
"journal-title": "J Biol Chem.",
"key": "B46",
"volume": "276",
"year": "2001"
},
{
"DOI": "10.3945/an.114.006940",
"article-title": "The science of fatty acids and inflammation",
"author": "Fritsche",
"doi-asserted-by": "crossref",
"key": "B47",
"volume-title": "Adv Nutr.",
"year": "2015"
},
{
"DOI": "10.1016/j.jnutbio.2015.12.007",
"article-title": "The relation of saturated fatty acids with low-grade inflammation and cardiovascular disease",
"author": "Ruiz-Núñez",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Nutr Biochem.",
"key": "B48",
"volume": "36",
"year": "2016"
},
{
"DOI": "10.1093/ajcn/nqaa110",
"article-title": "Public health guidelines should recommend reducing saturated fat consumption as much as possible: YES",
"author": "Kris-Etherton",
"doi-asserted-by": "publisher",
"first-page": "13",
"journal-title": "Am J Clin Nutr.",
"key": "B49",
"volume": "112",
"year": "2020"
},
{
"DOI": "10.3390/nu9121311",
"article-title": "Nuts and human health outcomes: a systematic review",
"author": "de Souza",
"doi-asserted-by": "publisher",
"first-page": "1311",
"journal-title": "Nutrients",
"key": "B50",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.1016/j.numecd.2012.10.008",
"article-title": "Dietary intake and major food sources of polyphenols in a Spanish population at high cardiovascular risk: the PREDIMED study",
"author": "Tresserra-Rimbau",
"doi-asserted-by": "publisher",
"first-page": "953",
"journal-title": "Nutr Metab Cardiovasc Dis.",
"key": "B51",
"volume": "23",
"year": "2013"
},
{
"DOI": "10.1515/reveh-2021-0065",
"article-title": "The aflatoxin B1 content of peanut-based foods in Iran: a systematic review",
"author": "Sadighara",
"doi-asserted-by": "publisher",
"first-page": "29",
"journal-title": "Rev Environ Health.",
"key": "B52",
"volume": "37",
"year": "2021"
},
{
"DOI": "10.1017/BJN20061863",
"article-title": "Dietary fibre, nuts and cardiovascular diseases",
"author": "Salas-Salvadó",
"doi-asserted-by": "publisher",
"first-page": "S45",
"journal-title": "Br J Nutr.",
"key": "B53",
"volume": "96",
"year": "2006"
},
{
"DOI": "10.1016/j.nutres.2013.08.010",
"article-title": "An acute intake of a walnut-enriched meal improves postprandial adiponectin response in healthy young adults",
"author": "Lozano",
"doi-asserted-by": "publisher",
"first-page": "1012",
"journal-title": "Nutr Res.",
"key": "B54",
"volume": "33",
"year": "2013"
},
{
"DOI": "10.1038/ejcn.2011.20",
"article-title": "Effect of walnut-enriched meat on the relationship between VCAM, ICAM, and LTB4 levels and PON-1 activity in ApoA4 360 and PON-1 allele carriers at increased cardiovascular risk",
"author": "Canales",
"doi-asserted-by": "publisher",
"first-page": "703",
"journal-title": "Eur J Clin Nutr.",
"key": "B55",
"volume": "65",
"year": "2011"
},
{
"DOI": "10.1016/j.metabol.2011.09.008",
"article-title": "Short-term walnut consumption increases circulating total adiponectin and apolipoprotein A concentrations, but does not affect markers of inflammation or vascular injury in obese humans with the metabolic syndrome: data from a double-blinded, randomized, placebo-controlled study",
"author": "Aronis",
"doi-asserted-by": "publisher",
"first-page": "577",
"journal-title": "Metabolism.",
"key": "B56",
"volume": "61",
"year": "2012"
},
{
"DOI": "10.3390/nu12030682",
"article-title": "Oxidative stress biomarkers, nut-related antioxidants, and cardiovascular disease",
"author": "Lorenzon Dos Santos",
"doi-asserted-by": "publisher",
"first-page": "682",
"journal-title": "Nutrients",
"key": "B57",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1093/ajcn/nqab012",
"article-title": "Underreporting of energy intake in weight loss maintainers",
"author": "Dahle",
"doi-asserted-by": "publisher",
"first-page": "257",
"journal-title": "Am J Clin Nutr.",
"key": "B58",
"volume": "114",
"year": "2021"
},
{
"article-title": "Predicting basal metabolic rate, new standards and review of previous work",
"author": "Schofield",
"first-page": "5",
"journal-title": "Hum Nutr Clin Nutr.",
"key": "B59",
"volume": "39",
"year": "1985"
},
{
"DOI": "10.3389/fnut.2022.833628",
"article-title": "Formulation of the menu of a general hospital after its conversion to a “COVID Hospital”: a nutrient analysis of 28-day menus",
"author": "Detopoulou",
"doi-asserted-by": "publisher",
"first-page": "833628",
"journal-title": "Front Nutr",
"key": "B60",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1371/journal.ppat.1005973",
"article-title": "IL-1β/IL-6/CRP and IL-18/ferritin: distinct inflammatory programs in infections",
"author": "Slaats",
"doi-asserted-by": "publisher",
"first-page": "e1005973",
"journal-title": "PLoS Pathog.",
"key": "B61",
"volume": "12",
"year": "2016"
}
],
"reference-count": 61,
"references-count": 61,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2022.911273/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Higher Adherence to the Mediterranean Dietary Pattern Is Inversely Associated With Severity of COVID-19 and Related Symptoms: A Cross-Sectional Study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "9"
}