COVID-19 Illness Severity in the Elderly in Relation to Vegetarian and Non-vegetarian Diets: A Single-Center Experience
et al., Frontiers in Nutrition, doi:10.3389/fnut.2022.837458, Apr 2022
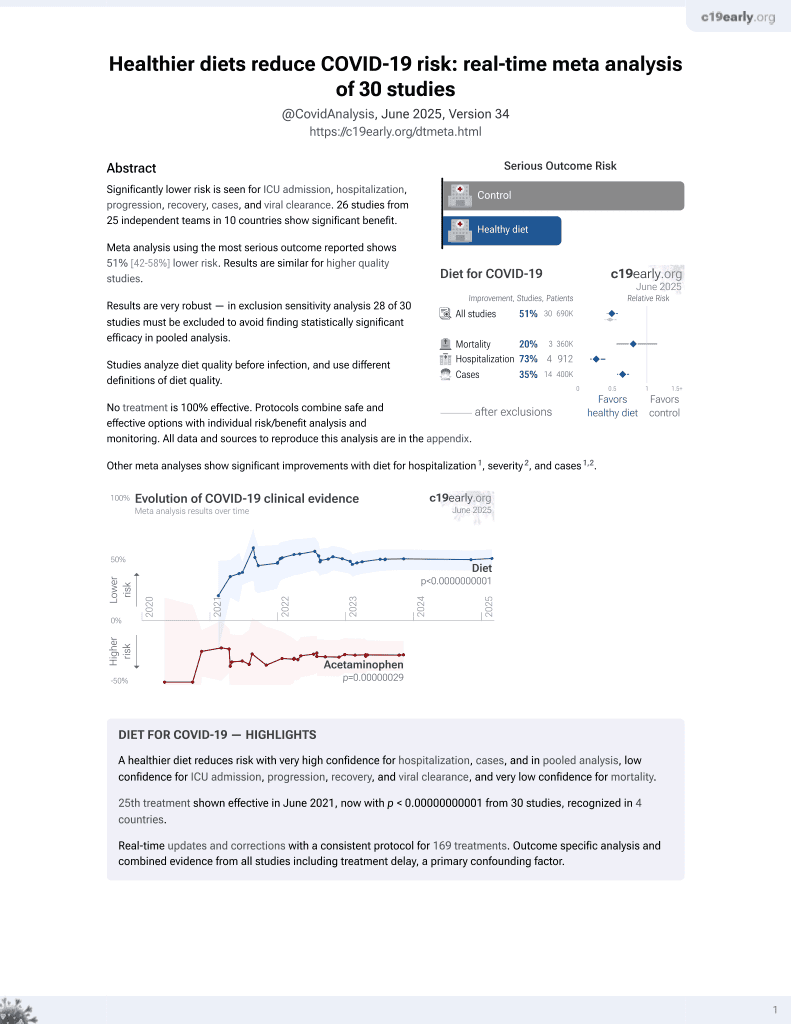
Diet for COVID-19
26th treatment shown to reduce risk in
June 2021, now with p < 0.00000000001 from 30 studies, recognized in 4 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 509 COVID-19 patients in Taiwan, showing higher risk of critical COVID-19 cases with non-vegetarian diets.
|
risk of critical case, 71.6% lower, RR 0.28, p = 0.23, higher quality diet 1 of 22 (4.5%), lower quality diet 78 of 487 (16.0%), NNT 8.7, excluded in exclusion analyses:
unadjusted results with no group details.
|
|
risk of moderate to critical case, 10.8% lower, RR 0.89, p = 0.66, higher quality diet 11 of 22 (50.0%), lower quality diet 273 of 487 (56.1%), NNT 17, excluded in exclusion analyses:
unadjusted results with no group details.
|
|
risk of critical case, 73.6% lower, RR 0.26, p = 0.005, higher quality diet 0 of 9 (0.0%), lower quality diet 47 of 127 (37.0%), NNT 2.7, adjusted per study, inverted to make RR<1 favor higher quality diet, odds ratio converted to relative risk, multivariable, age >65.
|
|
risk of moderate to critical case, 34.7% lower, RR 0.65, p = 0.04, higher quality diet 5 of 9 (55.6%), lower quality diet 108 of 127 (85.0%), NNT 3.4, age >65, excluded in exclusion analyses:
unadjusted results with no group details.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Hou et al., 29 Apr 2022, retrospective, Taiwan, peer-reviewed, survey, 3 authors, study period May 2021 - August 2021.
Contact: chaoycmd@yahoo.com.tw, williamsu2007@gmail.com.
COVID-19 Illness Severity in the Elderly in Relation to Vegetarian and Non-vegetarian Diets: A Single-Center Experience
Frontiers in Nutrition, doi:10.3389/fnut.2022.837458
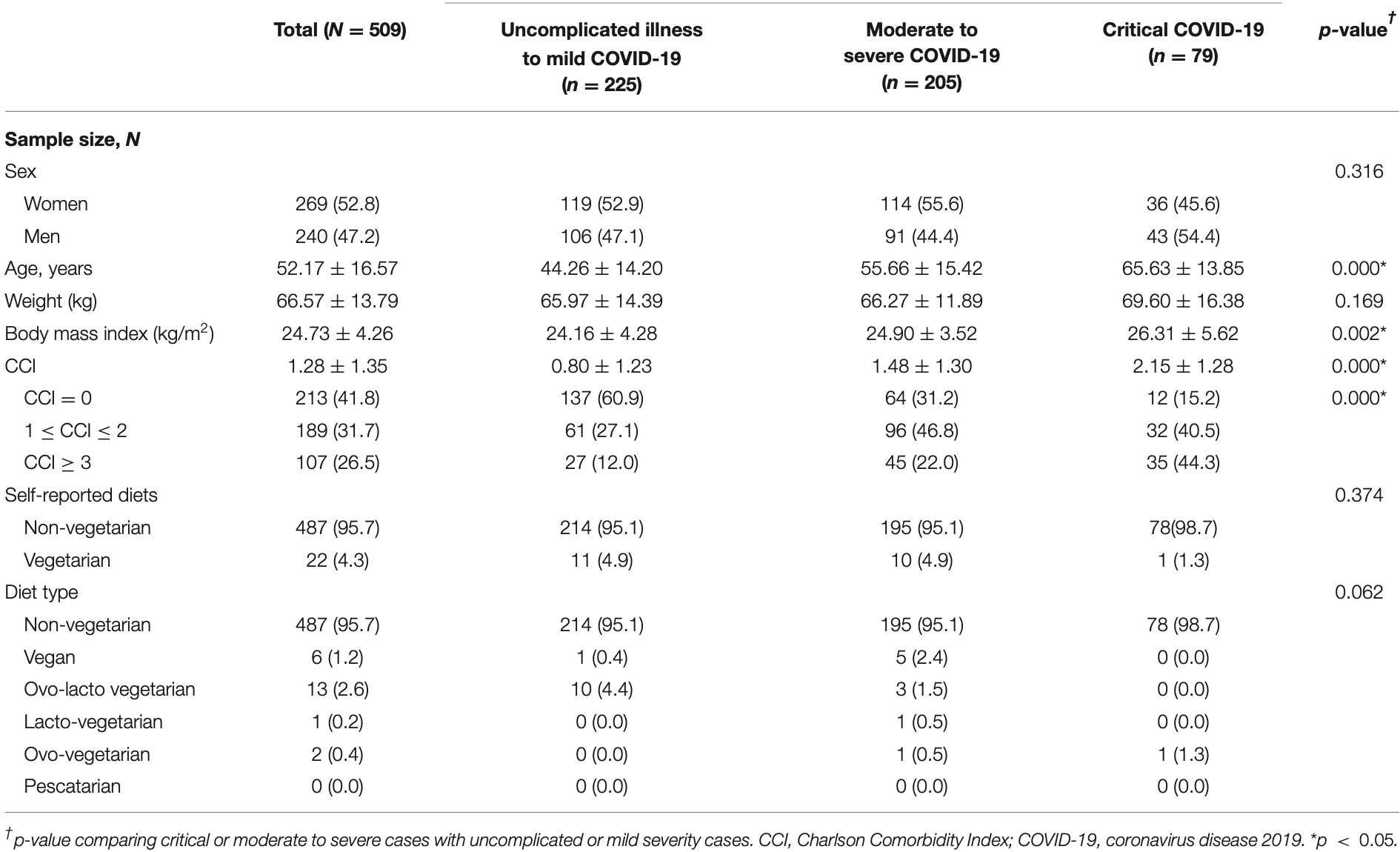
The first wave of the coronavirus disease 2019 (COVID-19) outbreak in Taiwan occurred in May 2021. The risk for and severity of this disease vary and are highly dependent on personal habits and comorbidities. Moreover, the gut microbiome, which may be affected by diet, is highly susceptible with regard to the risk and severity of infectious diseases such as COVID-19. The relationship between dietary habits, nutritional status, and the effects of these factors on the immune system in the context of a global pandemic is an extremely important topic of immediate concern. Hence, the aim of this study was to explore the effect of vegetarian and non-vegetarian diets on COVID-19 severity during the pandemic. We conducted a retrospective evaluation of 509 patients who had been diagnosed with COVID-19 at a single medical center between May 2021 and August 2021. Patients were divided into three groups according to disease severity. For patients aged ≥65 years, COVID-19 symptom severity was statistically significantly and inversely associated with the adherence to a vegetarian diet (p = 0.013). Moreover, subgroup analysis results showed that older COVID-19 patients and those with a non-vegetarian diet had a higher risk of contracting critically severe COVID-19 [adjusted odds ratio (OR) = 5.434, p = 0.005]. Further research is needed to determine the effects of dietary habits on COVID-19 risk and severity during the global pandemic.
ETHICS STATEMENT For this retrospective study, informed consent was waived by the IRB, and the privacy rights of patients, which cover any individual's data in any form (including individual details, images, or videos), were upheld. This study was approved by the Institutional Review Board of Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (approval number 10-X-141) and conducted according to the amended Declaration of Helsinki. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
AUTHOR CONTRIBUTIONS Y-CH and Y-CC conceived the study, designed the trial, obtained the research funding, analyzed and interpreted the data, and contributed to manuscript preparation. Y-CH and W-LS supervised the conduct of the trial, as well as data collection, and revised the manuscript for critical content. W-LS provided statistical advice with regard to the study design, and analyzed the data. Y-CH drafted the manuscript, and all authors contributed substantially to its revision. All authors take responsibility for the article as a whole. All authors contributed to the article and approved the submitted version.
SUPPLEMENTARY MATERIAL The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.
837458/full#supplementary-material
Conflict of Interest: The authors declare that the research was conducted in the..
References
Andarwulan, Kurniasih, Apriady, Rahmat, Roto et al., Polyphenols, carotenoids, and ascorbic acid in underutilized medicinal vegetables, J Funct Foods, doi:10.1016/j.jff.2012.01.003
Bajaj, Gadi, Spihlman, Wu, Choi et al., Aging, immunity, and Covid-19: how age influences the host immune response to coronavirus infections?, Front Physiol, doi:10.3389/fphys.2020.571416
Butler, Barrientos, The impact of nutrition on Covid-19 susceptibility and long-term consequences, Brain Behav Immun, doi:10.1016/j.bbi.2020.04.040
Calder, Nutrition, immunity and Covid-19, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000085
Charlson, Pompei, Ales, Mackenzie, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis, doi:10.1016/0021-9681(87)90171-8
Christensen, Strange, Gislason, Torp-Pedersen, Gerds et al., Charlson comorbidity index score and risk of severe outcome and death in danish Covid-19 patients, J Gen Intern Med, doi:10.1007/s11606-020-05991-z
Iddir, Brito, Dingeo, Del Campo, Samouda et al., Strengthening the immune system and reducing inflammation and oxidative stress through diet and nutrition: considerations during the Covid-19 crisis, Nutrients, doi:10.3390/nu12061562
Kim, Caulfield, Garcia-Larsen, Steffen, Grams et al., Plant-based diets and incident Ckd and kidney function, Clin J Am Soc Nephrol, doi:10.2215/CJN.12391018
Kim, Rebholz, Garcia-Larsen, Steffen, Coresh et al., Operational differences in plant-based diet indices affect the ability to detect associations with incident hypertension in middle-aged Us adults, J Nutr, doi:10.1093/jn/nxz275
Kim, Rebholz, Hegde, Lafiura, Raghavan et al., Plant-based diets, pescatarian diets and Covid-19 severity: a populationbased case-control study in six countries, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2021-000272
Kuswardhani, Henrina, Pranata, Lim, Lawrensia et al., Charlson comorbidity index and a composite of poor outcomes in Covid-19 patients: a systematic review and meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.10.022
Lim, Van Der Eerden, Laing, Boersma, Karalus et al., Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study, Thorax, doi:10.1136/thorax.58.5.377
Martinez-Ferran, De La Guia-Galipienso, Sanchis-Gomar, Pareja-Galeano, Metabolic impacts of confinement during the Covid-19 pandemic due to modified diet and physical activity habits, Nutrients, doi:10.3390/nu12061549
Merino, Joshi, Nguyen, Leeming, Mazidi et al., Diet quality and risk and severity of Covid-19: a prospective cohort study, Gut, doi:10.1136/gutjnl-2021-325353
Morais, Aquino, Da Silva-Maia, Vale, Maciel et al., Nutritional status, diet and viral respiratory infections: perspectives for severe acute respiratory syndrome Coronavirus 2, Br J Nutr, doi:10.1017/S0007114520003311
Satija, Hu, Plant-based diets and cardiovascular health, Trends Cardiovasc Med, doi:10.1016/j.tcm.2018.02.004
Segovia-Siapco, Burkholder-Cooley, Tabrizi, Sabate, Beyond meat: a comparison of the dietary intakes of vegetarian and non-vegetarian adolescents, Front Nutr, doi:10.3389/fnut.2019.00086
Silverio, Goncalves, Andrade, Seelaender, Coronavirus disease 2019 (Covid-19) and nutritional status: the missing link?, Adv Nutr, doi:10.1093/advances/nmaa125
Tavakol, Ghannadi, Tabesh, Halabchi, Noormohammadpour et al., Relationship between physical activity, healthy lifestyle and Covid-19 disease severity; a cross-sectional study, Z Gesundh Wiss, doi:10.1007/s10389-020-01468-9
Zabetakis, Lordan, Norton, Tsoupras, Covid-19: the inflammation link and the role of nutrition in potential mitigation, Nutrients, doi:10.3390/nu12051466
DOI record:
{
"DOI": "10.3389/fnut.2022.837458",
"ISSN": [
"2296-861X"
],
"URL": "http://dx.doi.org/10.3389/fnut.2022.837458",
"abstract": "<jats:p>The first wave of the coronavirus disease 2019 (COVID-19) outbreak in Taiwan occurred in May 2021. The risk for and severity of this disease vary and are highly dependent on personal habits and comorbidities. Moreover, the gut microbiome, which may be affected by diet, is highly susceptible with regard to the risk and severity of infectious diseases such as COVID-19. The relationship between dietary habits, nutritional status, and the effects of these factors on the immune system in the context of a global pandemic is an extremely important topic of immediate concern. Hence, the aim of this study was to explore the effect of vegetarian and non-vegetarian diets on COVID-19 severity during the pandemic. We conducted a retrospective evaluation of 509 patients who had been diagnosed with COVID-19 at a single medical center between May 2021 and August 2021. Patients were divided into three groups according to disease severity. For patients aged ≥65 years, COVID-19 symptom severity was statistically significantly and inversely associated with the adherence to a vegetarian diet (<jats:italic>p</jats:italic> = 0.013). Moreover, subgroup analysis results showed that older COVID-19 patients and those with a non-vegetarian diet had a higher risk of contracting critically severe COVID-19 [adjusted odds ratio (OR) = 5.434, <jats:italic>p</jats:italic> = 0.005]. Further research is needed to determine the effects of dietary habits on COVID-19 risk and severity during the global pandemic.</jats:p>",
"alternative-id": [
"10.3389/fnut.2022.837458"
],
"author": [
{
"affiliation": [],
"family": "Hou",
"given": "Yi-Cheng",
"sequence": "first"
},
{
"affiliation": [],
"family": "Su",
"given": "Wen-Lin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chao",
"given": "You-Chen",
"sequence": "additional"
}
],
"container-title": "Frontiers in Nutrition",
"container-title-short": "Front. Nutr.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2022,
4,
29
]
],
"date-time": "2022-04-29T09:19:57Z",
"timestamp": 1651223997000
},
"deposited": {
"date-parts": [
[
2022,
4,
29
]
],
"date-time": "2022-04-29T09:20:00Z",
"timestamp": 1651224000000
},
"funder": [
{
"DOI": "10.13039/501100008108",
"doi-asserted-by": "publisher",
"name": "Taipei Tzu Chi Hospital"
}
],
"indexed": {
"date-parts": [
[
2022,
4,
30
]
],
"date-time": "2022-04-30T16:15:12Z",
"timestamp": 1651335312460
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
4,
29
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
4,
29
]
],
"date-time": "2022-04-29T00:00:00Z",
"timestamp": 1651190400000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fnut.2022.837458/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2022,
4,
29
]
]
},
"published-online": {
"date-parts": [
[
2022,
4,
29
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1136/gutjnl-2021-325353",
"article-title": "Diet quality and risk and severity of Covid-19: a prospective cohort study",
"author": "Merino",
"doi-asserted-by": "publisher",
"first-page": "2096",
"journal-title": "Gut.",
"key": "B1",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.1136/bmjnph-2021-000272",
"article-title": "Plant-based diets, pescatarian diets and Covid-19 severity: a population-based case-control study in six countries",
"author": "Kim",
"doi-asserted-by": "publisher",
"first-page": "257",
"journal-title": "BMJ Nutr Prev Health.",
"key": "B2",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1017/S0007114520003311",
"article-title": "Nutritional status, diet and viral respiratory infections: perspectives for severe acute respiratory syndrome Coronavirus 2",
"author": "Morais",
"doi-asserted-by": "publisher",
"first-page": "851",
"journal-title": "Br J Nutr.",
"key": "B3",
"volume": "125",
"year": "2021"
},
{
"DOI": "10.3390/nu12051466",
"article-title": "Covid-19: the inflammation link and the role of nutrition in potential mitigation",
"author": "Zabetakis",
"doi-asserted-by": "publisher",
"first-page": "1466",
"journal-title": "Nutrients.",
"key": "B4",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1136/bmjnph-2020-000085",
"article-title": "Nutrition, immunity and Covid-19",
"author": "Calder",
"doi-asserted-by": "publisher",
"first-page": "74",
"journal-title": "BMJ Nutr Prev Health.",
"key": "B5",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1093/advances/nmaa125",
"article-title": "Coronavirus disease 2019 (Covid-19) and nutritional status: the missing link?",
"author": "Silverio",
"doi-asserted-by": "publisher",
"first-page": "682",
"journal-title": "Adv Nutr.",
"key": "B6",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1007/s10389-020-01468-9",
"article-title": "Relationship between physical activity, healthy lifestyle and Covid-19 disease severity; a cross-sectional study",
"author": "Tavakol",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Z Gesundh Wiss.",
"key": "B7",
"year": "2021"
},
{
"key": "B8",
"unstructured": ""
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"article-title": "A new method of classifying prognostic comorbidity in longitudinal studies: development and validation",
"author": "Charlson",
"doi-asserted-by": "publisher",
"first-page": "373",
"journal-title": "J Chronic Dis.",
"key": "B9",
"volume": "40",
"year": "1987"
},
{
"DOI": "10.1136/thorax.58.5.377",
"article-title": "Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study",
"author": "Lim",
"doi-asserted-by": "publisher",
"first-page": "377",
"journal-title": "Thorax.",
"key": "B10",
"volume": "58",
"year": "2003"
},
{
"DOI": "10.3389/fphys.2020.571416",
"article-title": "Aging, immunity, and Covid-19: how age influences the host immune response to coronavirus infections?",
"author": "Bajaj",
"doi-asserted-by": "publisher",
"first-page": "571416",
"journal-title": "Front Physiol.",
"key": "B11",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.10.022",
"article-title": "Charlson comorbidity index and a composite of poor outcomes in Covid-19 patients: a systematic review and meta-analysis",
"author": "Tuty Kuswardhani",
"doi-asserted-by": "publisher",
"first-page": "2103",
"journal-title": "Diabetes Metab Syndr.",
"key": "B12",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1007/s11606-020-05991-z",
"article-title": "Charlson comorbidity index score and risk of severe outcome and death in danish Covid-19 patients",
"author": "Christensen",
"doi-asserted-by": "publisher",
"first-page": "2801",
"journal-title": "J Gen Intern Med.",
"key": "B13",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.3390/nu12061562",
"article-title": "Strengthening the immune system and reducing inflammation and oxidative stress through diet and nutrition: considerations during the Covid-19 crisis",
"author": "Iddir",
"doi-asserted-by": "publisher",
"first-page": "1562",
"journal-title": "Nutrients.",
"key": "B14",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2020.04.040",
"article-title": "The impact of nutrition on Covid-19 susceptibility and long-term consequences",
"author": "Butler",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "Brain Behav Immun.",
"key": "B15",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.3390/nu12061549",
"article-title": "Metabolic impacts of confinement during the Covid-19 pandemic due to modified diet and physical activity habits",
"author": "Martinez-Ferran",
"doi-asserted-by": "publisher",
"first-page": "1549",
"journal-title": "Nutrients.",
"key": "B16",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/j.jff.2012.01.003",
"article-title": "Polyphenols, carotenoids, and ascorbic acid in underutilized medicinal vegetables",
"author": "Andarwulan",
"doi-asserted-by": "publisher",
"first-page": "339",
"journal-title": "J Funct Foods.",
"key": "B17",
"volume": "4",
"year": "2012"
},
{
"DOI": "10.3389/fnut.2019.00086",
"article-title": "Beyond meat: a comparison of the dietary intakes of vegetarian and non-vegetarian adolescents",
"author": "Segovia-Siapco",
"doi-asserted-by": "publisher",
"first-page": "86",
"journal-title": "Front Nutr.",
"key": "B18",
"volume": "6",
"year": "2019"
},
{
"DOI": "10.1093/jn/nxz275",
"article-title": "Operational differences in plant-based diet indices affect the ability to detect associations with incident hypertension in middle-aged Us adults",
"author": "Kim",
"doi-asserted-by": "publisher",
"first-page": "842",
"journal-title": "J Nutr.",
"key": "B19",
"volume": "150",
"year": "2020"
},
{
"DOI": "10.1016/j.tcm.2018.02.004",
"article-title": "Plant-based diets and cardiovascular health",
"author": "Satija",
"doi-asserted-by": "publisher",
"first-page": "437",
"journal-title": "Trends Cardiovasc Med.",
"key": "B20",
"volume": "28",
"year": "2018"
},
{
"DOI": "10.2215/CJN.12391018",
"article-title": "Plant-based diets and incident Ckd and kidney function",
"author": "Kim",
"doi-asserted-by": "publisher",
"first-page": "682",
"journal-title": "Clin J Am Soc Nephrol.",
"key": "B21",
"volume": "14",
"year": "2019"
}
],
"reference-count": 21,
"references-count": 21,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fnut.2022.837458/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Nutrition and Dietetics",
"Endocrinology, Diabetes and Metabolism",
"Food Science"
],
"subtitle": [],
"title": "COVID-19 Illness Severity in the Elderly in Relation to Vegetarian and Non-vegetarian Diets: A Single-Center Experience",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "9"
}