Vitamin D levels and mortality with SARS-COV-2 infection: a retrospective two-centre cohort study
et al., Postgraduate Medical Journal, doi:10.1136/postgradmedj-2021-140564, Sep 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
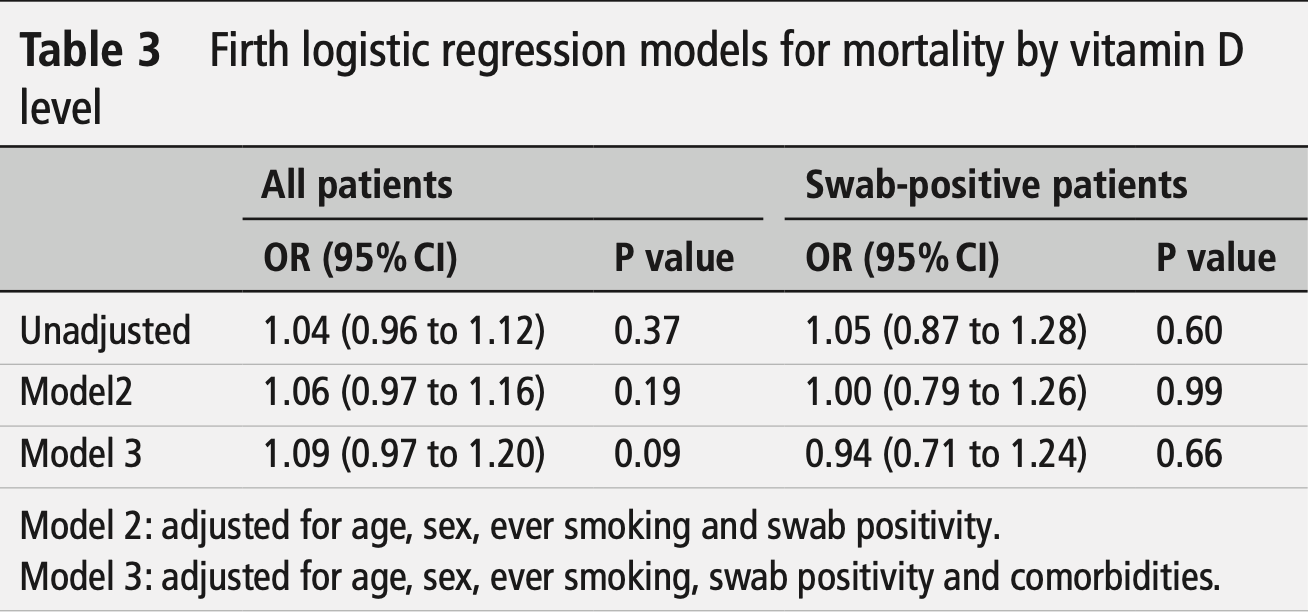
Retrospective 433 patients in the UK, 52 positive for COVID-19, showing no significant difference in mortality based on vitamin D levels. Authors also include results for all 433 patients, however given the expected test false negative rate compared with the very high number of COVID- patients, and the large difference in outcomes, it is likely that many of those patients did not have COVID-19. The adjusted results are only provided for vitamin D as a continuous value, where the most adjusted model for COVID+ patients shows lower mortality for higher vitamin D levels (not statistically significant).
This is the 95th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 42.9% higher, RR 1.43, p = 0.71, high D levels (≥25nmol/L) 12 of 42 (28.6%), low D levels (<25nmol/L) 2 of 10 (20.0%), COVID+ patients.
|
|
risk of death, 6.0% lower, OR 0.94, p = 0.68, high D levels 42, low D levels 10, COVID+ patients, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Zafar et al., 6 Sep 2021, retrospective, United Kingdom, peer-reviewed, median age 68.0, 37 authors.
Contact: 1mansoorzafar@gmail.com.
Vitamin D levels and mortality with SARS-COV-2 infection: a retrospective two-centre cohort study
Postgraduate Medical Journal, doi:10.1136/postgradmedj-2021-140564
Background The role of vitamin D in increased mortality with SARS-COV-2 virus, namely, COVID-19, remains uncertain. We analysed all the patients who were treated as COVID-19-positive with or without a positive swab and were tested for vitamin D levels. Methods This was a retrospective, study involving 1226 patients swabbed for SARS-CoV-2 between the 10 February 2020 and 1 May 2020 at two hospitals of East Sussex Healthcare NHS Trust. Patients who were swabpositive for COVID-19 or treated as COVID-19-positive on clinical grounds even though swab results were negative were included in this study. We analysed the association of vitamin D levels and mortality, assessing linear and non-linear associations. Results A total of 1226 patients had SARS-CoV-2 RNA swabs in this period with age range from 1 year to 101 years. A cohort of 433 of these patients had swabs and recent vitamin D levels anytime in the previous 3 months. Mortality rates were not found to be associated with vitamin D levels (OR=1.04, 95% CI 0.96 to 1.12). Conclusion Our findings suggest similar mortality risk from COVID-19 irrespective of the levels of vitamin D. Larger prospective studies will be needed to confirm these findings.
Collaborators Information is entered in the paper as coauthors in the main paper as previously advised by the journal. Contributors MZ designed the study and formed the steering group, which was responsible for ongoing evaluation for study design development, and led the methodological data collection from hospital electronic system towards comorbidities and access to blood test results. SM and WO assisted with electronic record for COVID-19 swab results for all patients from Conquest Hospital and Eastbourne District General Hospital. MZ, MK, MS, AK, LB, SA, KL, BP, RE, OM, DS, MF, HN, FC, KS, RSR, JH, OO, AE, BA, MP, MA, ZM, BK, AEM, GC, MJZ, NZ, MP, RG, AH and TM contributed with data acquisition and data entry. MZ, MK, MS, RSR, RE, SA and BP were responsible for the ongoing evaluation for study design development. SA, JH, DS, BP, ZM, BK, MK, JH and MP assisted with data assimilation, assisted by all other contributors. MJZ and NZ proofread the entire data for any errors. MZ and SA verified the data. MZ acted as guarantor. Statistical analysis was led by MZ, with intellectual review and support by Ms Jackie Cooper. MZ wrote the manuscript, which was reviewed by UD, MW and PM. All authors and UD approved the final version of the manuscript. Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared. Patient consent for publication Not required...
References
Baktash, Hosack, Patel, Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad Med J, doi:10.1136/postgradmedj-2020-138712
Bosworth, Levin, Robinson-Cohen, The serum 24,25-dihydroxyvitamin D concentration, a marker of vitamin D catabolism, is reduced in chronic kidney disease, Kidney Int, doi:10.1038/ki.2012.193
Bucak, Ozturk, Almis, Is there a relationship between low vitamin D and rotaviral diarrhea?, Pediatr Int, doi:10.1111/ped.12809
Carpagnano, Lecce, Quaranta, Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J Endocrinol Invest, doi:10.1007/s40618-020-01370-x
Cui, Xu, Li, Vitamin D receptor activation regulates microglia polarization and oxidative stress in spontaneously hypertensive rats and angiotensin II-exposed microglial cells: role of renin-angiotensin system, Redox Biol, doi:10.1016/j.redox.2019.101295
D'avolio, Avataneo, Manca, 25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Diagnostics, Elecsys® vitamin D total II
Draak, De Greef, Faber, The minimum clinically important difference: which direction to take, Eur J Neurol, doi:10.1111/ene.13941
Fasano, Cereda, Barichella, COVID-19 in Parkinson's disease patients living in Lombardy, Italy, Mov Disord, doi:10.1002/mds.28176
Grädel, Merker, Mueller, Schuetz, Screening and treatment of vitamin D deficiency on hospital admission: is there a benefit for medical inpatients?, Am J Med, doi:10.1016/j.amjmed.2015.06.034
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, Eur J Nutr, doi:10.1007/s00394-020-02372-4
Holick, Vitamin D deficiency, N Engl J Med, doi:10.1056/NEJMra070553
Holick, Vitamin D: the underappreciated D-lightful hormone that is important for skeletal and cellular health, Curr Opin Endocrinol Diabetes, doi:10.1097/00060793-200202000-00011
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res, doi:10.1007/s40520-020-01570-8
Isaia, Giorgino, Rini, Prevalence of hypovitaminosis D in elderly women in Italy: clinical consequences and risk factors, Osteoporos Int, doi:10.1007/s00198-003-1390-7
Laird, Rhodes, Kenny, Vitamin D and inflammation: potential implications for severity of Covid-19, Ir Med J
Maclaughlin, Holick, Aging decreases the capacity of human skin to produce vitamin D3, J Clin Invest, doi:10.1172/JCI112134
Palacios, Gonzalez, Is vitamin D deficiency a major global public health problem?, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2013.11.003
Pinzon, Pradana, Vitamin D deficiency among patients with COVID-19: case series and recent literature review, Trop Med Health, doi:10.1186/s41182-020-00277-w
Torjesen, Covid-19: public health agencies review whether vitamin D supplements could reduce risk, BMJ, doi:10.1136/bmj.m2475
Webmd, Vitamin, overview, uses, side effects, precautions, interactions, dosing and reviews
Woloshin, Patel, Kesselheim, False Negative Tests for SARS-CoV-2 Infection -Challenges and Implications, N Engl J Med, doi:10.1056/NEJMp2015897
Zafar, Ewnetu, Ahmed, COVID-19 vaccination-induced rash: does the choice of vaccine matter?, Cureus, doi:10.7759/cureus.15490
Zafar, Randhawa, Hegner, Can HbA1c levels be used as an independent marker of mortality and morbidity risk in patients with COVID19 positive swabs? -a retrospective observational study, University of Toronto Medical Journal
Zafar, Shahbaz, Karkhanis, A retrospective observational study: is absolute lymphocyte count a prognostic marker in COVID-19?, Cureus, doi:10.7759/cureus.16554
DOI record:
{
"DOI": "10.1136/postgradmedj-2021-140564",
"ISSN": [
"0032-5473",
"1469-0756"
],
"URL": "http://dx.doi.org/10.1136/postgradmedj-2021-140564",
"abstract": "<jats:title>Abstract</jats:title><jats:sec><jats:title>Background</jats:title><jats:p>The role of vitamin D in increased mortality with SARS-COV-2 virus, namely, COVID-19, remains uncertain. We analysed all the patients who were treated as COVID-19-positive with or without a positive swab and were tested for vitamin D levels.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>This was a retrospective, study involving 1226 patients swabbed for SARS-CoV-2 between the 10 February 2020 and 1 May 2020 at two hospitals of East Sussex Healthcare NHS Trust. Patients who were swab-positive for COVID-19 or treated as COVID-19-positive on clinical grounds even though swab results were negative were included in this study. We analysed the association of vitamin D levels and mortality, assessing linear and non-linear associations.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>A total of 1226 patients had SARS-CoV-2 RNA swabs in this period with age range from 1 year to 101 years. A cohort of 433 of these patients had swabs and recent vitamin D levels anytime in the previous 3 months. Mortality rates were not found to be associated with vitamin D levels (OR=1.04, 95% CI 0.96 to 1.12).</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>Our findings suggest similar mortality risk from COVID-19 irrespective of the levels of vitamin D. Larger prospective studies will be needed to confirm these findings.</jats:p></jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0001-8220-1014",
"affiliation": [
{
"name": "Gastroenterology, GIM, Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"authenticated-orcid": false,
"family": "Zafar",
"given": "Mansoor",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Karkhanis",
"given": "Mangala",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Shahbaz",
"given": "Muhammad",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Khanna",
"given": "Alisha",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Barry",
"given": "Lucinda",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Alam",
"given": "Saba",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Lawrence",
"given": "Kamal",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Pun",
"given": "Bipin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Eldebri",
"given": "Reem",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Makanjuola",
"given": "Opeyemi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Safarova",
"given": "Dana",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Farooq",
"given": "Mariya",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Nooredinavand",
"given": "Hesam",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Cuison",
"given": "Frderic",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Medicine, Conquest Hospital , Cardiff, UK"
}
],
"family": "Subba",
"given": "Karuna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Singh Randhawa",
"given": "Ratan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Hegner",
"given": "Johannes",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Oluwamayowa",
"given": "Ojofeitimi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Geriatric, Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Elyasaky",
"given": "Amr",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Adekunle",
"given": "Bolurin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Periasamy",
"given": "Manivannan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Abdelbagi",
"given": "Mohamed",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Maryam",
"given": "Zahra",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "General Internal Medicine, Conquest Hospital, East Sussex healthcare NHS Trust , St. Leonards-on-sea, UK"
}
],
"family": "Khuu",
"given": "Bao",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Esteves Morete",
"given": "Andreia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "General Internal Medicine, Conquest Hospital, East Sussex healthcare NHS Trust , St. Leonards-on-sea, UK"
}
],
"family": "Ciroi",
"given": "Giulio",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Microbiology, Eastbourne District General Hospital, East Sussex Healthcare NHS Trust , Eastbourne, UK"
}
],
"family": "Moran",
"given": "Steve",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Microbiology, Eastbourne District General Hospital , Eastbourne, UK"
}
],
"family": "O'Neill",
"given": "William",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine and Pharmacy, University of Oradea , Oradea, Romania"
}
],
"family": "Zafar",
"given": "Maaryah J",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Faculty of Medicine and Pharmacy, University of Oradea , Oradea, Romania"
}
],
"family": "Zafar",
"given": "Nadiyah",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Medical School and Health Science Center, University of Debrecen , Debrecen, Hungary"
}
],
"family": "Patel",
"given": "Mirej",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Geriatric, Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Golez",
"given": "Raphael",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "General Internal Medicine, Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Hadid",
"given": "Abubakr",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Gastroenterology, East Sussex Hospitals NHS Trust , Saint Leonards-on-Sea, UK"
}
],
"family": "Muhammad",
"given": "Tila",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Gastroenterology, Eastbourne District General Hospital. East Sussex Healthcare NHS Trust , Eastbourne, UK"
}
],
"family": "Mayhead",
"given": "Philip",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Consultant Physician and Gastroenterologist, Conquest Hospital , Saint Leonards on Sea, East Sussex, UK"
}
],
"family": "Whitehead",
"given": "Mark",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Diabetes and Endocrinology and General Internal Medicine, Conquest Hospital , Saint Leonards on Sea, UK"
}
],
"family": "Dashora",
"given": "Umesh",
"sequence": "additional"
}
],
"container-title": "Postgraduate Medical Journal",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
9,
6
]
],
"date-time": "2021-09-06T17:59:48Z",
"timestamp": 1630951188000
},
"deposited": {
"date-parts": [
[
2023,
1,
8
]
],
"date-time": "2023-01-08T18:28:54Z",
"timestamp": 1673202534000
},
"indexed": {
"date-parts": [
[
2023,
4,
17
]
],
"date-time": "2023-04-17T13:54:58Z",
"timestamp": 1681739698471
},
"is-referenced-by-count": 8,
"issue": "1161",
"issued": {
"date-parts": [
[
2021,
9,
6
]
]
},
"journal-issue": {
"issue": "1161",
"published-online": {
"date-parts": [
[
2021,
9,
6
]
]
},
"published-print": {
"date-parts": [
[
2022,
7,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 489,
"start": {
"date-parts": [
[
2023,
1,
8
]
],
"date-time": "2023-01-08T00:00:00Z",
"timestamp": 1673136000000
}
},
{
"URL": "https://bmj.com/coronavirus/usage",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
6
]
],
"date-time": "2021-09-06T00:00:00Z",
"timestamp": 1630886400000
}
}
],
"link": [
{
"URL": "https://academic.oup.com/pmj/article-pdf/98/1161/523/48387641/postgradmedj-98-523.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/pmj/article-pdf/98/1161/523/48387641/postgradmedj-98-523.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "286",
"original-title": [],
"page": "523-528",
"prefix": "10.1093",
"published": {
"date-parts": [
[
2021,
9,
6
]
]
},
"published-online": {
"date-parts": [
[
2021,
9,
6
]
]
},
"published-other": {
"date-parts": [
[
2022,
7
]
]
},
"published-print": {
"date-parts": [
[
2022,
7,
1
]
]
},
"publisher": "Oxford University Press (OUP)",
"reference": [
{
"DOI": "10.1016/j.jsbmb.2013.11.003",
"article-title": "Is vitamin D deficiency a major global public health problem?",
"author": "Palacios",
"doi-asserted-by": "crossref",
"first-page": "138",
"journal-title": "J Steroid Biochem Mol Biol",
"key": "2023010813412315400_bib1",
"volume": "144 Pt A",
"year": "2014"
},
{
"DOI": "10.1172/JCI112134",
"article-title": "Aging decreases the capacity of human skin to produce vitamin D3",
"author": "MacLaughlin",
"doi-asserted-by": "crossref",
"first-page": "1536",
"journal-title": "J Clin Invest",
"key": "2023010813412315400_bib2",
"volume": "76",
"year": "1985"
},
{
"DOI": "10.1097/00060793-200202000-00011",
"article-title": "Vitamin D: the underappreciated D-lightful hormone that is important for skeletal and cellular health",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "87",
"journal-title": "Curr Opin Endocrinol Diabetes",
"key": "2023010813412315400_bib3",
"volume": "9",
"year": "2002"
},
{
"DOI": "10.1038/ki.2012.193",
"article-title": "The serum 24,25-dihydroxyvitamin D concentration, a marker of vitamin D catabolism, is reduced in chronic kidney disease",
"author": "Bosworth",
"doi-asserted-by": "crossref",
"first-page": "693",
"journal-title": "Kidney Int",
"key": "2023010813412315400_bib4",
"volume": "82",
"year": "2012"
},
{
"DOI": "10.1056/NEJMra070553",
"article-title": "Vitamin D deficiency",
"author": "Holick",
"doi-asserted-by": "crossref",
"first-page": "266",
"journal-title": "N Engl J Med",
"key": "2023010813412315400_bib5",
"volume": "357",
"year": "2007"
},
{
"article-title": "25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2",
"author": "D'Avolio",
"journal-title": "Nutrients",
"key": "2023010813412315400_bib6",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1007/s00394-020-02372-4",
"article-title": "Vitamin D and COVID-19 infection and mortality in UK Biobank",
"author": "Hastie",
"doi-asserted-by": "crossref",
"first-page": "545",
"journal-title": "Eur J Nutr",
"key": "2023010813412315400_bib7",
"volume": "60",
"year": "2021"
},
{
"article-title": "Vitamin D and inflammation: potential implications for severity of Covid-19",
"author": "Laird",
"first-page": "81",
"journal-title": "Ir Med J",
"key": "2023010813412315400_bib8",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.1056/NEJMp2015897",
"article-title": "False Negative Tests for SARS-CoV-2 Infection - Challenges and Implications",
"author": "Woloshin",
"doi-asserted-by": "crossref",
"first-page": "e38",
"journal-title": "N Engl J Med",
"key": "2023010813412315400_bib9",
"volume": "383",
"year": "2020"
},
{
"author": "NHS England",
"key": "2023010813412315400_bib10",
"volume-title": "Guidance and standard operating procedure. COVID-19 virus testing in NHS laboratories",
"year": "2020"
},
{
"author": "Roche Diagnostics",
"key": "2023010813412315400_bib11",
"volume-title": "Elecsys® vitamin D total II",
"year": "2021"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"article-title": "The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality",
"author": "Ilie",
"doi-asserted-by": "crossref",
"first-page": "1195",
"journal-title": "Aging Clin Exp Res",
"key": "2023010813412315400_bib12",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1002/mds.28176",
"article-title": "COVID-19 in Parkinson's disease patients living in Lombardy, Italy",
"author": "Fasano",
"doi-asserted-by": "crossref",
"first-page": "1089",
"journal-title": "Mov Disord",
"key": "2023010813412315400_bib13",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1016/j.redox.2019.101295",
"article-title": "Vitamin D receptor activation regulates microglia polarization and oxidative stress in spontaneously hypertensive rats and angiotensin II-exposed microglial cells: role of renin-angiotensin system",
"author": "Cui",
"doi-asserted-by": "crossref",
"first-page": "101295",
"journal-title": "Redox Biol",
"key": "2023010813412315400_bib14",
"volume": "26",
"year": "2019"
},
{
"DOI": "10.1136/bmj.m2475",
"article-title": "Covid-19: public health agencies review whether vitamin D supplements could reduce risk",
"author": "Torjesen",
"doi-asserted-by": "crossref",
"first-page": "m2475",
"journal-title": "BMJ",
"key": "2023010813412315400_bib15",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1007/s00198-003-1390-7",
"article-title": "Prevalence of hypovitaminosis D in elderly women in Italy: clinical consequences and risk factors",
"author": "Isaia",
"doi-asserted-by": "crossref",
"first-page": "577",
"journal-title": "Osteoporos Int",
"key": "2023010813412315400_bib16",
"volume": "14",
"year": "2003"
},
{
"DOI": "10.1007/s40618-020-01370-x",
"article-title": "Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19",
"author": "Carpagnano",
"doi-asserted-by": "crossref",
"first-page": "765",
"journal-title": "J Endocrinol Invest",
"key": "2023010813412315400_bib17",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"article-title": "Vitamin D status and outcomes for hospitalised older patients with COVID-19",
"author": "Baktash",
"doi-asserted-by": "crossref",
"first-page": "442-447",
"journal-title": "Postgrad Med J",
"key": "2023010813412315400_bib18",
"volume": "97",
"year": "2021"
},
{
"DOI": "10.1016/j.amjmed.2015.06.034",
"article-title": "Screening and treatment of vitamin D deficiency on hospital admission: is there a benefit for medical inpatients?",
"author": "Grädel",
"doi-asserted-by": "crossref",
"first-page": "116.e1",
"journal-title": "Am J Med",
"key": "2023010813412315400_bib19",
"volume": "129",
"year": "2016"
},
{
"author": "Webmd",
"key": "2023010813412315400_bib20",
"volume-title": "Vitamin D: overview, uses, side effects, precautions, interactions, dosing and reviews",
"year": "2021"
},
{
"DOI": "10.1186/s41182-020-00277-w",
"article-title": "Vitamin D deficiency among patients with COVID-19: case series and recent literature review",
"author": "Pinzon",
"doi-asserted-by": "crossref",
"first-page": "102",
"journal-title": "Trop Med Health",
"key": "2023010813412315400_bib21",
"volume": "48",
"year": "2020"
},
{
"DOI": "10.1111/ped.12809",
"article-title": "Is there a relationship between low vitamin D and rotaviral diarrhea?",
"author": "Bucak",
"doi-asserted-by": "crossref",
"first-page": "270",
"journal-title": "Pediatr Int",
"key": "2023010813412315400_bib22",
"volume": "58",
"year": "2016"
},
{
"author": "Gastrointestinal Society",
"key": "2023010813412315400_bib23",
"volume-title": "Vitamin D might play a role in the prevention of disease",
"year": "2021"
},
{
"DOI": "10.1111/ene.13941",
"article-title": "The minimum clinically important difference: which direction to take",
"author": "Draak",
"doi-asserted-by": "crossref",
"first-page": "850",
"journal-title": "Eur J Neurol",
"key": "2023010813412315400_bib24",
"volume": "26",
"year": "2019"
},
{
"article-title": "A retrospective observational study: is absolute lymphocyte count a prognostic marker in COVID-19?",
"author": "Zafar",
"first-page": "e16554",
"journal-title": "Cureus",
"key": "2023010813412315400_bib25",
"volume": "13",
"year": "2021"
},
{
"article-title": "Can HbA1c levels be used as an independent marker of mortality and morbidity risk in patients with COVID19 positive swabs? - a retrospective observational study",
"author": "Zafar",
"first-page": "45",
"journal-title": "University of Toronto Medical Journal",
"key": "2023010813412315400_bib26",
"volume": "98",
"year": "2021"
},
{
"article-title": "COVID-19 vaccination-induced rash: does the choice of vaccine matter?",
"author": "Zafar",
"first-page": "e15490",
"journal-title": "Cureus",
"key": "2023010813412315400_bib27",
"volume": "13",
"year": "2021"
}
],
"reference-count": 27,
"references-count": 27,
"relation": {},
"resource": {
"primary": {
"URL": "https://academic.oup.com/pmj/article/98/1161/523/6959101"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Vitamin D levels and mortality with SARS-COV-2 infection: a retrospective two-centre cohort study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "98"
}
