The Effects of 10,000 IU Vitamin D Supplementation on Improvement of Clinical Outcomes, Inflammatory and Coagulation Markers in Moderate COVID-19 Patients: A Randomized-Controlled Trial
et al., Nutr. clín. diet. hosp., doi:10.12873/432taslim, NCT05126602, May 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
RCT 72 moderate COVID-19 patients with vitamin D deficiency or insufficiency in Indonesia, showing faster viral clearance and improved recovery with 10,000IU vitamin D vs. 1,000IU vitamin D. Higher vitamin D levels were associated with shorter length of stay (p = 0.009).
10,000IU vs. 1,000IU cholecalciferol daily for 2 weeks.
Cholecalciferol was used in this study.
Meta-analysis shows that late stage treatment with calcitriol / calcifediol (or
paricalcitol, alfacalcidol, etc.) is more effective than cholecalciferol: 66% [47‑78%] lower risk vs. 44% [33‑53%] lower risk.
Cholecalciferol requires two hydroxylation steps to become activated - first
in the liver to calcifediol, then in the kidney to calcitriol. Calcitriol,
paricalcitol, and alfacalcidol are active vitamin D analogs that do not
require conversion. This allows them to have more rapid onset of action
compared to cholecalciferol. The time delay for cholecalciferol to increase
serum calcifediol levels can be 2-3 days, and the delay for converting
calcifediol to active calcitriol can be up to 7 days.
This is the 35th of 40 COVID-19 RCTs for vitamin D, which collectively show efficacy with p=0.0000001.
This is the 119th of 136 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
|
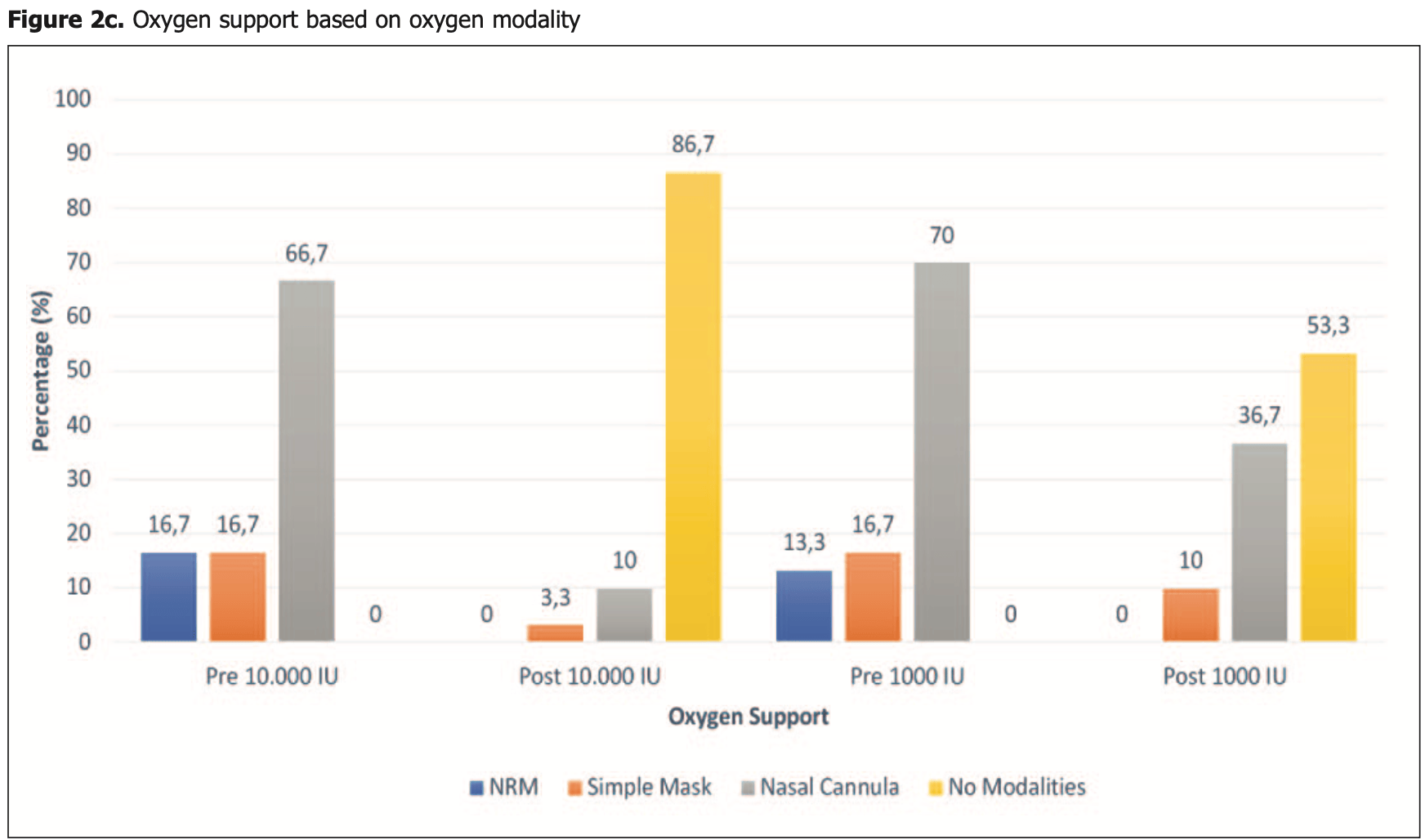
risk of oxygen therapy, 71.4% lower, RR 0.29, p = 0.01, treatment 4 of 30 (13.3%), control 14 of 30 (46.7%), NNT 3.0.
|
|
risk of oxygen therapy, 66.7% lower, RR 0.33, p = 0.61, treatment 1 of 30 (3.3%), control 3 of 30 (10.0%), NNT 15, mask.
|
|
risk of oxygen therapy, 72.7% lower, RR 0.27, p = 0.03, treatment 3 of 30 (10.0%), control 11 of 30 (36.7%), NNT 3.8, nasal cannula.
|
|
risk of no recovery, 60.0% lower, RR 0.40, p = 0.42, treatment 2 of 30 (6.7%), control 5 of 30 (16.7%), NNT 10.0, fever.
|
|
hospitalization time, 21.0% lower, relative time 0.79, p < 0.001, treatment mean 11.63 (±2.5) n=30, control mean 14.73 (±3.45) n=30.
|
|
time to viral-, 37.6% lower, relative time 0.62, p < 0.001, treatment mean 6.53 (±1.17) n=30, control mean 10.47 (±2.56) n=30, primary outcome.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Taslim et al., 1 May 2023, Single Blind Randomized Controlled Trial, Indonesia, peer-reviewed, 10 authors, study period 1 April, 2021 - 30 September, 2021, trial NCT05126602 (history).
Contact: pudji_taslim@yahoo.com.
The Effects of 10,000 IU Vitamin D Supplementation on Improvement of Clinical Outcomes, Inflammatory and Coagulation Markers in Moderate COVID-19 Patients: A Randomized-Controlled Trial
doi:10.12873/432taslim
Background & aims: Vitamin D supplementation as an immunomodulator has been identified as a potential strategy to prevent and treat Coronavirus disease 2019 (COVID-19). We aimed to analyze the effect of 10,000 IU vitamin D3 supplementation on 25(OH)D levels on primary clinical outcomes (conversion length), inflammatory markers (Total Lymphocyte Count (TLC), Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR)) and coagulation marker (D-Dimer
CONCLUSION The effects of 10,000 IU Vitamin D3 supplementation in moderate COVID-19 patients whom have low vitamin D status showed improvements in LOC, LOS, clinical manifestations, functional capacity, and positive correlation on inflammatory and coagulation markers, such as PLR.
References
Altaş, Tosun, Assessment of Vitamin D and inflammatory response relationship using neutrophil to lymphocyte ratio, platelet to lymphocyte ratio and mean platelet volume, Turk Osteoporoz Derg, doi:10.4274/tod.07108
Bennasrallah, Zemni, Dhouib, Factors associated with a prolonged negative conversion of viral RNA in patients with COVID-19, Int J Infect Dis, doi:10.1016/j.ijid.2021.02.089
Fiorindi, Campani, Rasero, Prevalence of nutritional risk and malnutrition during and after hospitalization for COVID-19 infection: Preliminary results of a single-centre experience, Clin Nutr ESPEN, doi:10.1016/j.clnesp.2021.07.020
Frassinette, Albuquerque, Xavier, Desfecho clínico e fatores associados em pacientes com COVID-19 internados em uma Unidade de Terapia Intensiva Clinical outcome and associated factors in patients with COVID-19 admitted to an Intensive Care Unit, doi:10.12873/424oliveira
Gotelli, Paolino, Soldano, Cutolo, Vitamin D Immune-Mediated Responses and SARS-CoV-2 Infection: Clinical Implications in COVID-19, Immuno, doi:10.3390/immuno2010001
Guan, Ni, Hu, Clinical Characteristics of Coronavirus Disease 2019 in China, N Engl J Med, doi:10.1056/nejmoa2002032
Indonesia, Pedoman Tatalaksana COVID-19
King, The Role of Vitamin D deficiency in COVID-19 related deaths in BAME, Obese and Other High-risk Categories, doi:10.31232/osf.io/73whx
Kollias, Kyriakoulis, Dimakakos, Poulakou, Stergiou et al., Thromboembolic risk and anticoagulant therapy in COVID-19 patients: emerging evidence and call for action, Br J Haematol, doi:10.1111/bjh.16727
Lechien, Chiesa-Estomba, Place, Clinical and epidemiological characteristics of 1420 European patients with mildto-moderate coronavirus disease 2019, J Intern Med, doi:10.1111/joim.13089
Li, Zhou, Ba, Nutritional risk and therapy for severe and critical COVID-19 patients: A multicenter retrospective observational study, Clin Nutr, doi:10.1016/j.clnu.2020.09.040
Liu, Zhang, Wu, Clinical outcomes of COVID-19 in Wuhan, China: a large cohort study, Ann Intensive Care, doi:10.1186/s13613-020-00706-3
Ludwig, Jacob, Basedow, Andersohn, Walker, Clinical outcomes and characteristics of patients hospitalized for Influenza or COVID-19 in Germany, Int J Infect Dis, doi:10.1016/j.ijid.2020.11.204
Merzon, Tworowski, Gorohovski, Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS J, doi:10.1111/febs.15495
Moriconi, Masi, Rebelos, Obesity prolongs the hospital stay in patients affected by COVID-19, and may impact on SARS-COV-2 shedding, Obes Res Clin Pract, doi:10.1016/j.orcp.2020.05.009
Murai, Fernandes, Sales, Effect of a Single High Dose of Vitamin D3on Hospital Length of Stay in Patients with Moderate to Severe COVID-19: A Randomized Clinical Trial, JAMA -J Am Med Assoc, doi:10.1001/jama.2020.26848
Musselwhite, Andrade, Ellenberg, Vitamin D, Ddimer, Interferon γ, and sCD14 Levels are Independently Associated with Immune Reconstitution Inflammatory Syndrome: A Prospective, International Study, EBioMedicine, doi:10.1016/j.ebiom.2016.01.016
Nicolau, Ayala, Sanchís, Influence of nutritional status on clinical outcomes among hospitalized patients with COVID-19, Clin Nutr ESPEN, doi:10.1016/j.clnesp.2021.04.013
Orchard, Baldry, Nasim-Mohi, Vitamin-D levels and intensive care unit outcomes of a cohort of critically ill COVID-19 patients, Clin Chem Lab Med, doi:10.1515/cclm-2020-1567
Pdgki, Panduan Praktis Penatalaksanaan Nutrisi COVID-19. Perhimpun Dr Spes Gizi Klin Indones
Pereira, Damascena, Azevedo, De Almeida Oliveira, Da et al., Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis, Crit Rev Food Sci Nutr, doi:10.1080/10408398.2020.1841090
Rastogi, Bhansali, Khare, Short term, high-dose vitamin D supplementation for COVID-19 disease: A randomised, placebocontrolled, study (SHADE study), Postgrad Med J. Published online, doi:10.1136/postgradmedj-2020-139065
Roth, Emmons-Bell, Alger, Trends in Patient Characteristics and COVID-19 In-Hospital Mortality in the United States During the COVID-19 Pandemic, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.8828
Sabico, Enani, Sheshah, Effects of a 2-week 5000 iu versus 1000 iu vitamin d3 supplementation on recovery of symptoms in patients with mild to moderate covid-19: A randomized clinical trial, Nutrients, doi:10.3390/nu13072170
Sepandi, Taghdir, Alimohamadi, Afrashteh, Hosamirudsari H. Factors associated with mortality in COVID-19 patients: A systematic review and meta-analysis, Iran J Public Health, doi:10.18502/ijph.v49i7.3574
Shareef, Zwain, Mahbuba, Superiority of lymphocyte ratio over total leukocyte count in detecting the severity of COVID-19 pneumonia, Heliyon, doi:10.1016/j.heliyon.2021.e08412
Song, Chen, Yuan, Wang, Wang, Total lymphocyte count, neutrophil-lymphocyte ratio, and platelet-lymphocyte ratio as prognostic factors in advanced non-small cell lung cancer with chemoradiotherapy, Cancer Manag Res, doi:10.2147/CMAR.S188578
Spagnolo, Manson, Joffe, Sex and Gender Differences in Health: What the COVID-19 Pandemic Can Teach Us, Ann Intern Med, doi:10.7326/M20-1941
Wang, Wang, Gu, Vitamin D is related to handgrip strength in adult men aged 50 years and over: A population study from the TCLSIH cohort study, Clin Endocrinol (Oxf), doi:10.1111/cen.13952
Wu, Chen, Chan, The outbreak of COVID-19: An overview, J Chinese Med Assoc, doi:10.1097/JCMA.0000000000000270
Yang, Liu, Tao W Qiang, Li, Ming, The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients, Int Immunopharmacol, doi:10.1016/j.intimp.2020.106504
Yue, Li, Wang, Nutritional Support and Clinical Outcome of Severe and Critical Patients With COVID-19 Pneumonia, Front Nutr, doi:10.3389/fnut.2020.581679
Zhao, Meng, Kumar, Lymphopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A systemic review and meta-analysis, Int J Infect Dis, doi:10.1016/j.ijid.2020.04.086
