Correlation between Serum Vitamin D3 levels and severity of COVID-19, experience from a COVID-19-dedicated tertiary care hospital from Western India
et al., Indian Journal of Endocrinology and Metabolism, doi:10.4103/ijem.ijem_383_22, Apr 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective analysis of 200 hospitalized COVID-19 patients in India, showing no significant differences in outcomes with vitamin D deficiency.
This is the 178th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
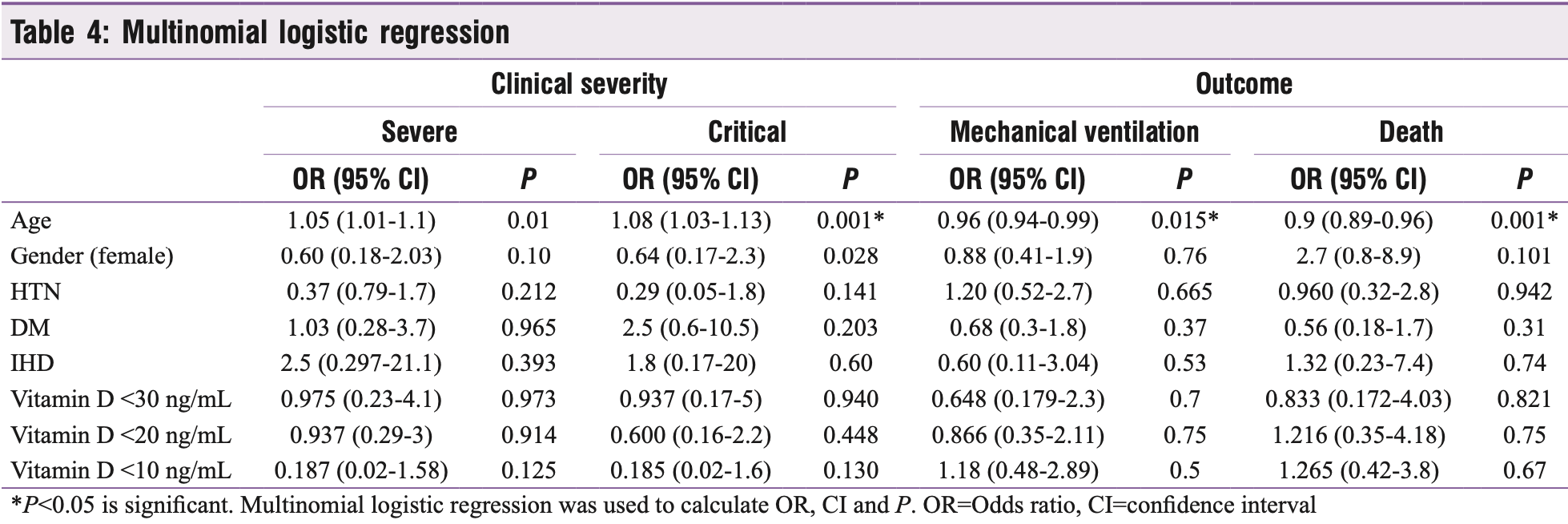
risk of death, 20.9% lower, OR 0.79, p = 0.67, high D levels (≥10ng/mL) 155, low D levels (<10ng/mL) 45, inverted to make OR<1 favor high D levels (≥10ng/mL), RR approximated with OR.
|
|
risk of mechanical ventilation, 15.3% lower, OR 0.85, p = 0.73, high D levels (≥10ng/mL) 155, low D levels (<10ng/mL) 45, inverted to make OR<1 favor high D levels (≥10ng/mL), RR approximated with OR.
|
|
risk of severe case, 434.8% higher, OR 5.35, p = 0.12, high D levels (≥10ng/mL) 155, low D levels (<10ng/mL) 45, inverted to make OR<1 favor high D levels (≥10ng/mL), RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Sanamandra et al., 30 Apr 2023, prospective, India, peer-reviewed, 6 authors, study period August 2020 - March 2021.
Contact: sukirtimisra09@gmail.com.
Correlation between Serum Vitamin D3 levels and severity of COVID-19, experience from a COVID-19-dedicated tertiary care hospital from Western India
Indian Journal of Endocrinology and Metabolism, doi:10.4103/ijem.ijem_383_22
The COVID-19 pandemic caused by a novel coronavirus (SARS-CoV-2) is characterized by significant morbidity and mortality with no current specific treatment. Preclinical research suggests that the SARS-CoV-2 virus enters cells via the angiotensin-converting enzyme 2 (ACE2). [1] Coronavirus replication downregulates ACE2, causing the renin-angiotensin system (RAS) to become dysfunctional and producing a cytokine storm with increased production of pro-inflammatory cytokines. This increases the risk of pneumonia, sepsis, acute respiratory distress syndrome and heart failure. [2] Research shows that vitamin D plays a role in balancing RAS, in reducing lung damage through the anti-inflammatory effect which is seen with higher vitamin D levels ranging from 20 to 60 ng/mL. [3] [4] [5] Vitamin D deficiency is one of India's most underdiagnosed and undertreated nutritional deficiencies. [6] Many studies have found that lacking vitamin D or vitamin D receptors causes altered innate and adaptive immune functions. [7, 8] Vitamin D supplementation is a potentially exciting treatment for COVID-19 infection but scientifically, with a low level of evidence until now. [9] Some studies have confirmed the Context: It is postulated that 25(OH)D deficiency is associated with a worse prognosis of COVID-19. Aims: We aimed to find out whether baseline serum 25-hydroxy vitamin D levels were correlated with COVID-19 disease severity or not in Indian population. Settings and Design: It is a prospective observational study. Methods and Material: We prospectively recruited 200 COVID-19-positive adult patients and measured their baseline vitamin D levels on admission and prospectively followed their clinical course for their outcome and correlated the association.
Statistical Analysis Used: The continuous data were represented as mean (±SD) or median (IQR), while the categorical data were represented as proportions. Parametric data were analysed using unpaired T-test and ANOVA for two and more than two groups, and for categorical, nonparametric data, Chi-square test were applied. A two-sided P value of <0.05 was considered as statistically significant with 95% confidence interval. Results: Eighty-six per cent (172/200) of patients had hypovitaminosis D (<30 ng/mL). The prevalence of 25(OH) severe deficiency, deficiency and vitamin D insufficiency was 23%, 41% and 22%, respectively. Clinical severity was graded as asymptomatic (11%), mild (14%), moderate (14.5%), severe (37.5%) and critical (22%). Sixty per cent of patients had clinically severe or critical disease requiring oxygen support with eleven per cent (n = 22) mortality overall. Age (P: 0.001), HTN (P: 0.049) and DM (P: 0.018) were negatively associated with clinical severity. No linear association was found between vitamin D levels and clinical severity. Low vitamin D levels had a significant inverse association with inflammatory markers like neutrophil-lymphocyte ratio (NLR, P: 0.012) and IL-6 (P:..
Conflicts of interest There are no conflicts of interest.
references
References
Akbas, Gungor, Ozcicek, Akbas, Askin et al., Vitamin D and inflammation: Evaluation with neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio, Arch Med Sci
Al Kiyumi, Kalra, Davies, Kalhan, The impact of vitamin D deficiency on the severity of symptoms and mortality rate among adult patients with Covid-19: A systematic review and meta-analysis, Indian J Endocrinol Metab
Alkhafaji, Al Argan, Albaker, Elq, Al-Hariri et al., The impact of vitamin D level on the severity and outcome of hospitalized patients with COVID-19 disease, Int J Gen Med
Aparna, Muthathal, Nongkynrih, Gupta, Vitamin D deficiency in India, J Family Med Prim Care
Avataneo, Manca, Cusato, Nicolò, Lucchini, 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients, Aging Clin Exp Res, doi:10.1007/S40520-020-01677-Y
Di Rosa, Malaguarnera, Nicoletti, Malaguarnera, Vitamin D3: A helpful immuno-modulator, Immunology
Dissanayake, Silva, Sumanatilleke, De Silva, Gamage et al., Prognostic and therapeutic role of vitamin D in COVID-19: Systematic review and meta-analysis, J Clin Endocrinol Metab
Gheblawi, Wang, Viveiros, Nguyen, Zhong et al., Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: Celebrating the 20 th anniversary of the discovery of ACE2, Circ Res
Hansdottir, Monick, Vitamin D effects on lung immunity and respiratory diseases, Vitam Horm
Hernández, Nan, Fernandez-Ayala, García-Unzueta, Hernández-Hernández et al., Vitamin D status in hospitalized patients with SARS-CoV-2 infection, J Clin Endocrinol Metab
Holick, Binkley, Bischoff-Ferrari, Gordon, Hanley et al., Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline, J Clin Endocrinol Metab
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci Rep
Jevalikar, Mithal, Singh, Sharma, Farooqui et al., Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19, Sci Rep, doi:10.1038/s41598-021-85809-y
Khazai, Judd, Tangpricha, Calcium and vitamin D: Skeletal and extraskeletal health, Curr Rheumatol Rep
Labudzynskyi, Shymanskyy, Veliky, Role of vitamin D3 in regulation of interleukin-6 and osteopontin expression in liver of diabetic mice, Eur Rev Med Pharmacol Sci
Liu, Zhou, The cytokine storm of severe influenza and development of immunomodulatory therapy, Cell Mol Immunol
Maghbooli, Sahraian, Ebrahimi, Pazoki, Kafan et al., Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection, PLoS One, doi:10.1371/journal.pone.0239799
Mardani, Alamdary, Nasab, Gholami, Ahmadi et al., Association of vitamin D with the modulation of the disease severity in COVID-19, Virus Res, doi:10.1016/J.VIRUSRES.2020.198148
Munger, Levin, Hollis, Howard, Ascherio, Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis, JAMA
Nasiri, Khodadadi, Molaei, Does vitamin D serum level affect prognosis of COVID-19 patients?, Int J Infect Dis
Ni, Yang, Yang, Bao, Li et al., Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19, Crit Care, doi:10.1186/S13054-020-03120-0
Pizzini, Aichner, Sahanic, Böhm, Egger et al., Impact of vitamin D deficiency on COVID-19-A prospective analysis from the CovILD registry, Nutrients, doi:10.3390/NU12092775
Radujkovic, Hippchen, Tiwari-Heckler, Dreher, Boxberger, Vitamin D deficiency and outcome of COVID-19 patients, Nutrients
Shi, Liu, Yao, Xing, Zhao et al., Chronic vitamin D deficiency induces lung fibrosis through activation of the renin-angiotensin system, Sci Rep, doi:10.1038/s41598-017-03474-6
Tabatabaeizadeh, Avan, Bahrami, Khodashenas, Esmaeili et al., High dose supplementation of vitamin D affects measures of systemic inflammation: Reductions in high sensitivity C-reactive protein level and neutrophil to lymphocyte ratio (NLR) distribution, J Cell Biochem
Vitamin, COVID-19 Treatment Guidelines
Walk, Dofferhoff, Van Den Ouweland, Van Daal, Janssen, Vitamin D -contrary to vitamin K -does not associate with clinical outcome in hospitalized COVID-19 patients, medRxiv, doi:10.1101/2020.11.07.20227512
Wang, Shen, Xi, Shen, Zhang, Vitamin D affects the neutrophil-to-lymphocyte ratio in patients with type 2 diabetes mellitus, J Diabetes Investig
Ye, Tang, Liao, Shaw, Deng et al., Does serum vitamin D level affect COVID-19 infection and its severity?-A case-control study, J Am Coll Nutr
DOI record:
{
"DOI": "10.4103/ijem.ijem_383_22",
"ISSN": [
"2230-8210"
],
"URL": "http://dx.doi.org/10.4103/ijem.ijem_383_22",
"alternative-id": [
"374149"
],
"author": [
{
"affiliation": [],
"family": "Misra",
"given": "Sukirti",
"sequence": "first"
},
{
"affiliation": [],
"family": "Sanamandra",
"given": "Prudwiraj",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gada",
"given": "JugalV",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Barasara",
"given": "SagarA",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Varthakavi",
"given": "PremlataK",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bhagwat",
"given": "NikhilM",
"sequence": "additional"
}
],
"container-title": "Indian Journal of Endocrinology and Metabolism",
"container-title-short": "Indian J Endocr Metab",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
4,
13
]
],
"date-time": "2023-04-13T11:45:39Z",
"timestamp": 1681386339000
},
"deposited": {
"date-parts": [
[
2023,
4,
13
]
],
"date-time": "2023-04-13T11:56:23Z",
"timestamp": 1681386983000
},
"indexed": {
"date-parts": [
[
2023,
4,
14
]
],
"date-time": "2023-04-14T04:56:36Z",
"timestamp": 1681448196553
},
"is-referenced-by-count": 0,
"issue": "2",
"issued": {
"date-parts": [
[
2023
]
]
},
"journal-issue": {
"issue": "2",
"published-print": {
"date-parts": [
[
2023
]
]
}
},
"language": "en",
"member": "2581",
"original-title": [],
"page": "170",
"prefix": "10.4103",
"published": {
"date-parts": [
[
2023
]
]
},
"published-print": {
"date-parts": [
[
2023
]
]
},
"publisher": "Medknow",
"reference": [
{
"author": "Gheblawi",
"first-page": "1456",
"journal-title": "Circ Res",
"key": "key-10.4103/2230-8210.374149-1",
"volume-title": "Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: Celebrating the 20th anniversary of the discovery of ACE2",
"year": "2020"
},
{
"author": "Ni",
"first-page": "422",
"journal-title": "Crit Care",
"key": "key-10.4103/2230-8210.374149-2",
"volume-title": "Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19?",
"year": "2020"
},
{
"author": "Shi",
"first-page": "3312",
"journal-title": "Sci Rep",
"key": "key-10.4103/2230-8210.374149-3",
"volume-title": "Chronic vitamin D deficiency induces lung fibrosis through activation of the renin-angiotensin system?",
"year": "2017"
},
{
"author": "Munger",
"first-page": "2832",
"journal-title": "JAMA",
"key": "key-10.4103/2230-8210.374149-4",
"volume-title": "Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis",
"year": "2006"
},
{
"author": "Khazai",
"first-page": "110",
"journal-title": "Curr Rheumatol Rep",
"key": "key-10.4103/2230-8210.374149-5",
"volume-title": "Calcium and vitamin D: Skeletal and extraskeletal health",
"year": "2008"
},
{
"ISSN": "http://id.crossref.org/issn/2249-4863",
"author": "Aparna",
"first-page": "324",
"issn-type": "print",
"journal-title": "J Family Med Prim Care",
"key": "key-10.4103/2230-8210.374149-6",
"volume-title": "Vitamin D deficiency in India",
"year": "2018"
},
{
"author": "Hansdottir",
"first-page": "217",
"journal-title": "Vitam Horm",
"key": "key-10.4103/2230-8210.374149-7",
"volume-title": "Vitamin D effects on lung immunity and respiratory diseases",
"year": "2011"
},
{
"author": "di",
"first-page": "123",
"journal-title": "Immunology",
"key": "key-10.4103/2230-8210.374149-8",
"volume-title": "Vitamin D3: A helpful immuno-modulator",
"year": "2011"
},
{
"key": "key-10.4103/2230-8210.374149-9",
"unstructured": "Vitamin D | COVID-19 Treatment Guidelines. Available from: https://www.covid19treatmentguidelines.nih.gov/therapies/supplements/vitamin-d/. [Last accessed on 2022 Apr 04]."
},
{
"author": "D'avolio",
"first-page": "1359",
"journal-title": "Nutrients",
"key": "key-10.4103/2230-8210.374149-10",
"volume-title": "25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2?",
"year": "2020"
},
{
"author": "Hernández",
"first-page": "E1343",
"journal-title": "J Clin Endocrinol Metab",
"key": "key-10.4103/2230-8210.374149-11",
"volume-title": "Vitamin D status in hospitalized patients with SARS-CoV-2 infection",
"year": "2021"
},
{
"key": "key-10.4103/2230-8210.374149-12",
"unstructured": "Clinical Spectrum | COVID-19 Treatment Guidelines. Available from: https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/. [Last accessed on 2022 Oct 01]."
},
{
"author": "Holick",
"first-page": "1911",
"journal-title": "J Clin Endocrinol Metab",
"key": "key-10.4103/2230-8210.374149-13",
"volume-title": "Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline",
"year": "2011"
},
{
"author": "Ye",
"first-page": "724",
"journal-title": "J Am Coll Nutr",
"key": "key-10.4103/2230-8210.374149-14",
"volume-title": "Does serum vitamin D level affect COVID-19 infection and its severity.-A case-control study?",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0239799",
"doi-asserted-by": "crossref",
"key": "key-10.4103/2230-8210.374149-15",
"unstructured": "Maghbooli Z, Sahraian MA, Ebrahimi M, Pazoki M, Kafan S, Tabriz HM, et al. Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PLoS One 15:e0239799. doi: 10.1371/journal.pone.0239799."
},
{
"author": "Mardani",
"first-page": "198148",
"journal-title": "Virus Res",
"key": "key-10.4103/2230-8210.374149-16",
"volume-title": "Association of vitamin D with the modulation of the disease severity in COVID-19?",
"year": "2020"
},
{
"author": "Radujkovic",
"first-page": "1",
"journal-title": "Nutrients",
"key": "key-10.4103/2230-8210.374149-17",
"volume-title": "Vitamin D deficiency and outcome of COVID-19 patients",
"year": "2020"
},
{
"author": "Jain",
"first-page": "1",
"journal-title": "Sci Rep",
"key": "key-10.4103/2230-8210.374149-18",
"volume-title": "Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers",
"year": "2020"
},
{
"author": "Alkhafaji",
"first-page": "343",
"journal-title": "Int J Gen Med",
"key": "key-10.4103/2230-8210.374149-19",
"volume-title": "The impact of vitamin D level on the severity and outcome of hospitalized patients with COVID-19 disease",
"year": "2022"
},
{
"author": "Nasiri",
"first-page": "264",
"journal-title": "Int J Infect Dis",
"key": "key-10.4103/2230-8210.374149-20",
"volume-title": "Does vitamin D serum level affect prognosis of COVID-19 patients?",
"year": "2021"
},
{
"DOI": "10.1101/2020.11.07.20227512",
"doi-asserted-by": "crossref",
"key": "key-10.4103/2230-8210.374149-21",
"unstructured": "Walk J, Dofferhoff ASM, van den Ouweland JMW, van Daal H, Janssen R. Vitamin D – contrary to vitamin K – does not associate with clinical outcome in hospitalized COVID-19 patients. medRxiv 2020;2020.11.07.20227512. doi: 10.1101/2020.11.07.20227512."
},
{
"author": "Pizzini",
"first-page": "1",
"journal-title": "Nutrients",
"key": "key-10.4103/2230-8210.374149-22",
"volume-title": "Impact of vitamin D deficiency on COVID-19-A prospective analysis from the CovILD registry?",
"year": "2020"
},
{
"author": "Dissanayake",
"first-page": "1484",
"journal-title": "J Clin Endocrinol Metab",
"key": "key-10.4103/2230-8210.374149-23",
"volume-title": "Prognostic and therapeutic role of vitamin D in COVID-19: Systematic review and meta-analysis",
"year": "2022"
},
{
"author": "al",
"first-page": "261",
"journal-title": "Indian J Endocrinol Metab",
"key": "key-10.4103/2230-8210.374149-24",
"volume-title": "The impact of vitamin D deficiency on the severity of symptoms and mortality rate among adult patients with Covid-19: A systematic review and meta-analysis",
"year": "2021"
},
{
"author": "Jevalikar",
"first-page": "1",
"journal-title": "Sci Rep",
"key": "key-10.4103/2230-8210.374149-25",
"volume-title": "Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19?",
"year": "2021"
},
{
"author": "Liu",
"first-page": "3",
"journal-title": "Cell Mol Immunol",
"key": "key-10.4103/2230-8210.374149-26",
"volume-title": "The cytokine storm of severe influenza and development of immunomodulatory therapy",
"year": "2016"
},
{
"author": "Labudzynskyi",
"first-page": "2916",
"journal-title": "Eur Rev Med Pharmacol Sci",
"key": "key-10.4103/2230-8210.374149-27",
"volume-title": "Role of vitamin D3 in regulation of interleukin-6 and osteopontin expression in liver of diabetic mice",
"year": "2016"
},
{
"author": "Wang",
"first-page": "254",
"journal-title": "J Diabetes Investig",
"key": "key-10.4103/2230-8210.374149-28",
"volume-title": "Vitamin D affects the neutrophil-to-lymphocyte ratio in patients with type 2 diabetes mellitus",
"year": "2021"
},
{
"author": "Akbas",
"first-page": "721",
"journal-title": "Arch Med Sci",
"key": "key-10.4103/2230-8210.374149-29",
"volume-title": "Vitamin D and inflammation: Evaluation with neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio",
"year": "2016"
},
{
"author": "Tabatabaeizadeh",
"first-page": "4317",
"journal-title": "J Cell Biochem",
"key": "key-10.4103/2230-8210.374149-30",
"volume-title": "High dose supplementation of vitamin D affects measures of systemic inflammation: Reductions in high sensitivity C-reactive protein level and neutrophil to lymphocyte ratio (NLR) distribution",
"year": "2017"
},
{
"author": "Daneshkhah",
"first-page": "2141",
"journal-title": "Aging Clin Exp Res",
"key": "key-10.4103/2230-8210.374149-31",
"volume-title": "Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients?",
"year": "2020"
}
],
"reference-count": 31,
"references-count": 31,
"relation": {},
"resource": {
"primary": {
"URL": "http://www.ijem.in/text.asp?2023/27/2/170/374149"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Correlation between Serum Vitamin D3 levels and severity of COVID-19, experience from a COVID-19-dedicated tertiary care hospital from Western India",
"type": "journal-article",
"volume": "27"
}
