Vitamin D status in hospitalized COVID‑19 patients is associated with disease severity and IL-5 production
et al., Virology Journal, doi:10.1186/s12985-023-02165-1, Sep 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 399 hospitalized patients in China, showing that lower vitamin D levels and higher IL-5 levels were independent risk factors for COVID-19 severity.
Qiu et al., 13 Sep 2023, retrospective, China, preprint, 10 authors, study period 19 December, 2022 - 1 February, 2023.
Contact: zhouyan790304@163.com.
Vitamin D status in hospitalized COVID‑19 patients is associated with disease severity and IL-5 production
doi:10.21203/rs.3.rs-3058788/v1
Background There are many studies on relationship between vitamin D and coronavirus disease 2019 (COVID-19), while the results are matters of debate and the mechanisms remain unknown. The present study to assess the impact of serum 25-hydroxyvitamin D [25(OH)D] levels on the severity of disease in hospitalized COVID-19 patients and identify potential mechanisms.
Methods A total of 399 hospitalized COVID-19 patients were recruited from three centers between December 19, 2022, and February 1, 2023.
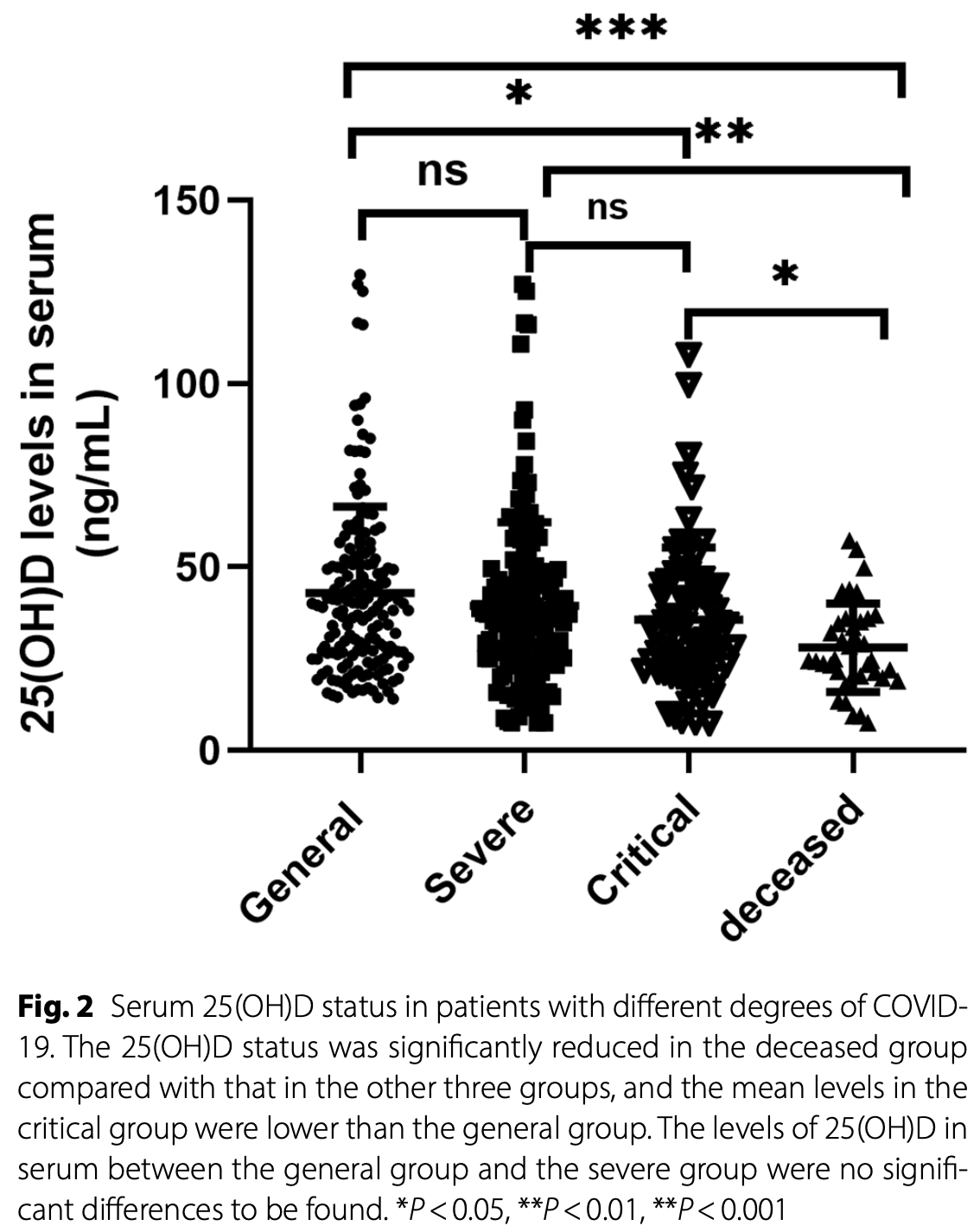
Results Levels of 25(OH)D were signi cantly lower in the deceased group than other three groups (P < 0.05). The levels of 25(OH)D (odds ratio = 0.986, 95% con dence interval: 0.973-0.998, P = 0.024) and IL-5 (odds ratio = 1.239, 95% con dence interval: 1.104-1.391, P = 0.04) were independent risk factors for the severity of COVID-19 disease upon admission. Serum 25(OH)D levels combined with IL-5 levels and eosinophil (Eos) counts were able to predict the mortality of patients with COVID-19. Circulating 25(OH)D status correlated negatively with the expression of IL-5 (r=-0.262, P < 0.001) and was positively linked with CD8 + T cell counts (r=-0.121, P < 0.05) in patients with COVID-19.
Conclusions Most COVID-19 patients have vitamin D de ciency and a severe de ciency is associated with fatal outcomes. This study found that the serum 25(OH)D status in COVID-19 patients correlated negatively with the expression of IL-5. The speci c mechanism for this relationship is worth further exploration.
Most COVID-19 patients have evidence of vitamin D de ciency and severe de ciency is associated with an increased risk of severe disease and mortality. The current study found that 25(OH)D levels combined with IL-5 levels and Eos counts could serve as predictors of early COVID-19-related lung injury and mortality. This study found that the levels of 25(OH)D in the serum of patients with COVID-19 correlated negatively with the expression of IL-5, however, the speci c mechanism requires further exploration.
Supplementary Material Supplementary Material is not available with this version Figures
References
Aglipay, Birken, Parkin, Loeb, Thorpe et al., Effect of High-Dose vs Standard-Dose Wintertime Vitamin D Supplementation on Viral Upper Respiratory Tract Infections in Young Healthy Children, doi:10.1001/jama.2017.8708
Alpcan, Tursun, Kandur, Vitamin D levels in children with COVID-19: a report from Turkey, Epidemiol Infect, doi:10.1017/S0950268821001825
Azkur, Akdis, Azkur, Sokolowska, Van De Veen et al., Immune response to SARS-CoV-2 and mechanisms of immunopathological changes in COVID-19, Allergy, doi:10.1111/all.14364
Benskin, A Basic Review of the Preliminary Evidence That COVID-19 Risk and Severity Is Increased in Vitamin D De ciency, Front Public Health, doi:10.3389/fpubh.2020.00513
Bilezikian, Bikle, Hewison, Lazaretti-Castro, Formenti et al., MECHANISMS IN ENDOCRINOLOGY: Vitamin D and COVID-19, Eur J Endocrinol, doi:10.1530/EJE-20-0665
Chen, Sang, Jiang, Yang, Jia et al., Medical Treatment Expert Group for, Longitudinal hematologic and immunologic variations associated with the progression of COVID-19 patients in China, J Allergy Clin Immunol, doi:10.1016/j.jaci.2020.05.003
Chen, Wu, Chen, Yan, Yang et al., Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study, BMJ, doi:10.1136/bmj.m1091
Chiodini, Gatti, Soranna, Merlotti, Mingiano et al., Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes, Front Public Health, doi:10.3389/fpubh.2021.736665
Dong, Zhai, Fang, Liu, Yuan et al., A retrospective study of Pupingqinghua prescription versus Lianhuaqingwen in Chinese participants infected with SARS-CoV-2 Omicron variants, Front Pharmacol, doi:10.3389/fphar.2022.988524
Favaloro, Lippi, Recommendations for Minimal Laboratory Testing Panels in Patients with COVID-19: Potential for Prognostic Monitoring, Semin Thromb Hemost, doi:10.1055/s-0040-1709498
Han, Zhang, Mu, Wei, Jin et al., Lactate dehydrogenase, an independent risk factor of severe COVID-19 patients: a retrospective and observational study, Aging (Albany NY), doi:10.18632/aging.103372
Holick, Binkley, Bischoff-Ferrari, Gordon, Hanley et al., Evaluation, treatment, and prevention of vitamin D de ciency: an Endocrine Society clinical practice guideline, J Clin Endocrinol Metab
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res, doi:10.1007/s40520-020-01570-8
Karonova, Andreeva, Golovatuk, Bykova, Simanenkova et al., Low 25(OH)D Level Is Associated with Severe Course and Poor Prognosis in COVID-19, Nutrients, doi:10.3390/nu13093021
Kuba, Imai, Rao, Gao, Guo et al., A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury, Nat Med, doi:10.1038/nm1267
Laires, Nunes, Population-based Estimates for High Risk of Severe COVID-19 Disease due to Age and Underlying Health Conditions, Acta Med Port, doi:10.20344/amp.14222
Ling, Broad, Murphy, Pappachan, Pardesi-Newton et al., High-Dose Cholecalciferol Booster Therapy is Associated with a Reduced Risk of Mortality in Patients with COVID-19: A Cross-Sectional Multi-Centre Observational Study, Nutrients, doi:10.3390/nu12123799
Lohia, Kapur, Patel, Seyoum, Letter to the editor: Vitamin D levels in acute illness and clinical severity in COVID-19 patients, Respir Res, doi:10.1186/s12931-021-01703-1
Lucas, Wong, Klein, Castro, Silva et al., Longitudinal analyses reveal immunological mis ring in severe COVID-19, Nature, doi:10.1038/s41586-020-2588-y
Oh, D status in patients with different degrees of COVID-19. The 25(OH)D status were signi cantly reduced in the deceased group compared with those in the other three groups, and the levels in the critical group were lower than that in the general group. The levels of 25(OH)D between the general group and the severe group was no signi cant difference to be found
Pala, Pistis, Anti-IL5 Drugs in COVID-19 Patients: Role of Eosinophils in SARS-CoV-2-Induced Immunopathology, doi:10.3389/fphar.2021.622554
Poddighe, Kovzel, Impact of Anti-Type 2 In ammation Biologic Therapy on COVID-19 Clinical Course and Outcome, J In amm Res, doi:10.2147/JIR.S345665
Sabico, Enani, Sheshah, Aljohani, Aldisi et al., Effects of a 2-Week 5000 IU versus 1000 IU Vitamin D3 Supplementation on Recovery of Symptoms in Patients with Mild to Moderate Covid-19: A Randomized Clinical Trial, Nutrients, doi:10.3390/nu13072170
Solis, Salas, Luesma Bartolome, Santander Ballestin, The Effects of Vitamin D Supplementation in COVID-19 Patients: A Systematic Review, Int J Mol Sci, doi:10.3390/ijms232012424
Sun, Dong, Wang, Xie, Li et al., Characteristics and prognostic factors of disease severity in patients with COVID-19: The Beijing experience, J Autoimmun, doi:10.1016/j.jaut.2020.102473
Wang, Tumes, Hercus, Yip, Aloe et al., Blocking the human common beta subunit of the GM-CSF, IL-5 and IL-3 receptors markedly reduces hyperin ammation in ARDS models, Cell Death Dis, doi:10.1038/s41419-022-04589-z
Wang, Wang, Chen, Zhang, Yu et al., E cacy of vitamin D supplementation on COPD and asthma control: A systematic review and meta-analysis, J Glob Health, doi:10.7189/jogh.12.04100
Yilmaz, Sen, Is vitamin D de ciency a risk factor for COVID-19 in children?, Pediatr Pulmonol, doi:10.1002/ppul.25106
Zdrenghea, Makrinioti, Bagacean, Bush, Johnston et al., Vitamin D modulation of innate immune responses to respiratory viral infections, Rev Med Virol, doi:10.1002/rmv.1909
Zheng, Gao, Wang, Song, Liu et al., Functional exhaustion of antiviral lymphocytes in COVID-19 patients, Cell Mol Immunol
