Vitamin D status in patients with COVID-19 – sex differences associated with severity of the disease
et al., Medical Journal MEDICUS, 28:1, May 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 115 COVID-19 patients in North Macedonia, showing lower vitamin D levels associated with hospitalization.
Pop-Kostova et al., 12 May 2023, retrospective, North Macedonia, peer-reviewed, 2 authors, study period September 2020 - December 2020.
Original scientific paper ЛИПИДНИОТ МАРКЕР АПОЛИПОПРОТЕИН Б КАКО ПРЕДИКТОР ЗА КОРОНАРНАТА АРТЕРИСКА БОЛЕСТ КАЈ ДИЈАБЕТЕС МЕЛИТУС ТИП 2 ПАЦИЕНТИ СО И БЕЗ ДИЈАБЕТИЧНА НЕФРОПАТИЈА
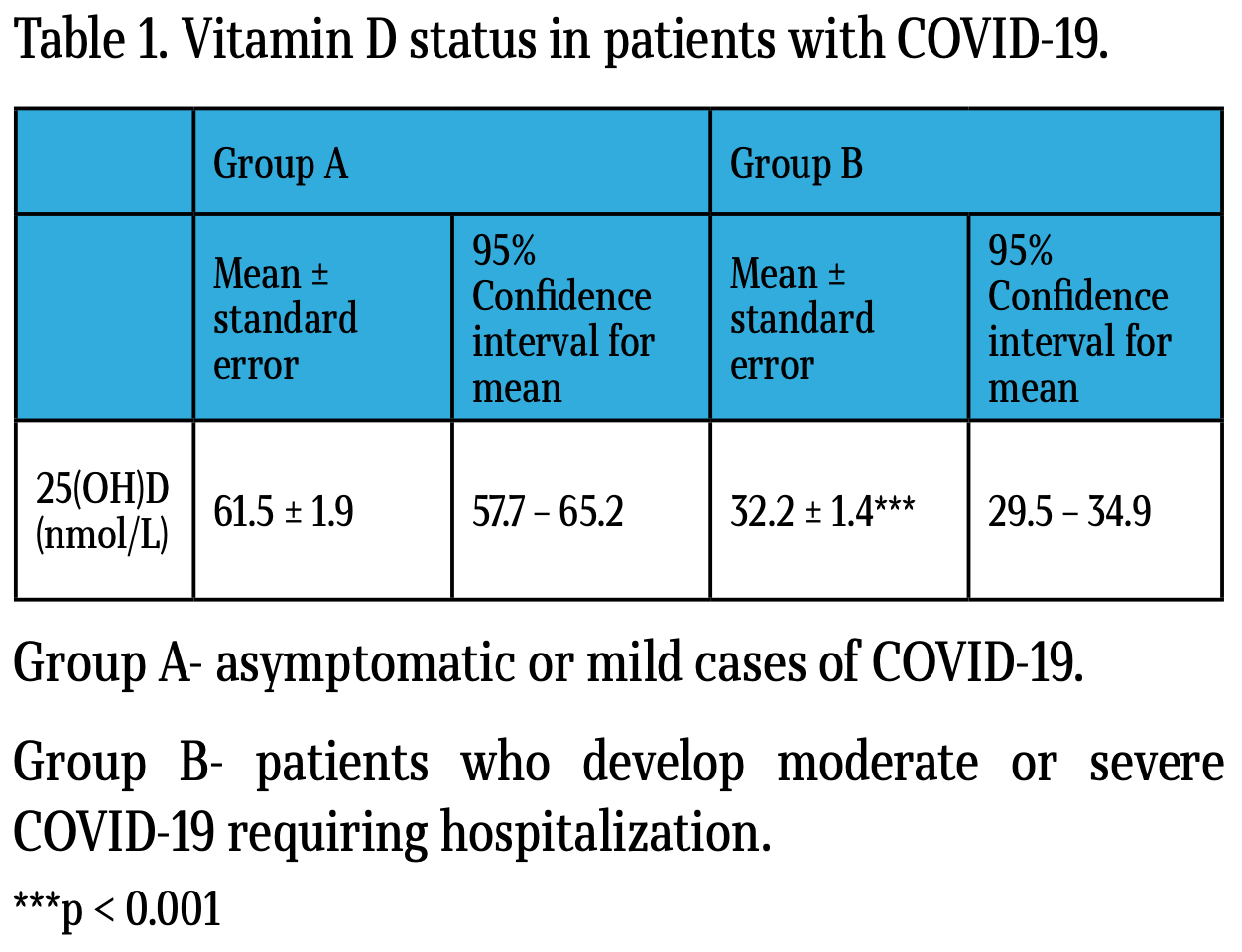
Background: Patients with COVID-19 can develop abnormal inflammatory response, which can progress to multiorgan failure and death, with a higher prevalence observed in men. Besides, recent research suggests a complex interaction between viral infections and vitamin D. Aims: This study evaluates sex differences of vitamin D status, circulating enzymes and biomarkers of inflammatory response at the time of diagnosis of COVID-19, depending on severity of disease the patients develop. Methods: This retrospective observational study was conducted from September to December 2020. Patients (n = 115) were divided in two groups: Group A-asymptomatic or mild cases (36 men and 19 women; mean age 53.3 ± 1.4 y.) and Group B-patients who develop moderate or severe COVID-19 requiring hospitalization (38 men and 22 women; mean age 56.1 ± 1.3 y.). Results: Patients of Group B had almost two-fold lower circulating 25(OH)D concentrations than patients of Group A (Group A: 61.6 ± 1.9 nmol/L; Group B: 32.2 ± 1.4 nmol/L; p < 0.001). Within Group A, the only parameter with a statistically significant sex difference was ferritin (p < 0.01). Within Group B, in addition to ferritin (p < 0.05), we observed a pronounced and statistically highly significant sex difference in circulating 25(OH)D concentrations (men: 35.8 ± 1.7 nmol/L; women: 26.0 ± 1.7; p < 0.001). Conclusions: Our results demonstrate that inadequate vitamin D status is associated with the development of moderate or severe COVID-19 and indicate that circulating 25(OH)D might be associated to sex differences in disease outcome.
VITAMIN D STATUS IN PATIENTS WITH COVID-19 -SEX DIFFERENCES ASSOCIATED WITH SEVERITY OF THE DISEASE.
Conflict of interest The authors declare that they have no conflict of interest.
References
Arsenault, Gage, Kim, Kapoor, Akweongo et al., COVID-19 and resilience of healthcare systems in ten countries, Nat Med, doi:10.1038/s41591-022-01750-
Aslan, Aslan, Özdemir, Letter to the Editor: Is Vitamin D One of the Key Elements in COVID-19 Days?, J Nutr Health Aging, doi:10.1007/s12603-020-1413-5
Autier, Mullie, Macacu, Dragomir, Boniol et al., Effect of vitamin D supplementation on non-skeletal disorders: a systematic review of meta-analyses and randomised trials, Lancet Diabetes Endocrinol, doi:10.1016/s2213-8587(17)30357-1
Ben-Eltriki, Hopefl, Wright, Association between Vitamin D Status and Risk of Developing Severe COVID-19 Infection: A Meta-Analysis of Observational Studies, J Am Nutr Assoc, doi:10.1080/07315724.2021.1951891
Chiodini, Gatti, Soranna, Merlotti, Mingiano et al., Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes, Front Public Health, doi:10.3389/fpubh.2021.736665
Correale, Ysrraelit, Gaitán, Gender differences in 1,25 dihydroxyvitamin D3 immunomodulatory effects in multiple sclerosis patients and healthy subjects, J Immunol, doi:10.4049/jimmunol.1000588
Cucinotta, Vanelli, WHO Declares COVID-19 a Pandemic, Acta Biomed, doi:10.23750/abm.v91i1.9397
Cullis, Fitzsimons, Griffiths, Tsochatzis, Thomas, Investigation and management of a raised serum ferritin, Br J Haematol, doi:10.1111/bjh.15166
Dror, Morozov, Daoud, Namir, Yakir et al., Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness, PLoS One, doi:10.1371/journal.pone.0263069
Gandini, Criniti, Gagliardi, Ballesio, Giglio et al., Sexdisaggregated data confirm serum ferritin as an independent predictor of disease severity both in male and female COVID-19 patients, J Infect, doi:10.1016/j.jinf.2020.10.012
Getachew, Tizabi, Vitamin D and COVID-19: Role of ACE2, age, gender, and ethnicity, J Med Virol, doi:10.1002/jmv.27075
Ghosh, Klein, Sex Drives Dimorphic Immune Responses to Viral Infections, J Immunol, doi:10.4049/jimmunol.1601166
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Hamid, Abid, Amir, Rehman, Akram et al., Current burden on healthcare systems in low-and middle-income countries: recommendations for emergency care of COVID-19, Drugs Ther Perspect, doi:10.1007/s40267-020-00766-2
Hars, Mendes, Serratrice, Herrmann, Gold et al., Sex-specific association between vitamin D deficiency and COVID-19 mortality in older patients, Osteoporos Int, doi:10.1007/s00198-020-05677-6
Hopefl, Ben-Eltriki, Association Between Vitamin D Levels and Inflammatory Markers in COVID-19 Patients: A Meta-Analysis of Observational Studies, J Pharm Pharm Sci, doi:10.18433/jpps32518
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci Rep, doi:10.1038/s41598-020-77093-z
Jakovac, COVID-19 and vitamin D-Is there a link and an opportunity for intervention?, Am J Physiol Endocrinol Metab, doi:10.1152/ajpen-do.00138
Kato, Kurzrock, Repurposing Interleukin-6 Inhibitors to Combat COVID-19, J Immunother Precis Oncol, doi:10.36401/jipo-20-11
Kaushal, Kaur, Sarma, Bhattacharyya, Sharma et al., Serum ferritin as a predictive biomarker in COVID-19. A systematic review, meta-analysis and meta-regression analysis, J Crit Care, doi:10.1016/j.jcrc.2021.09.023
Knovich, Storey, Coffman, Torti, Torti, Ferritin for the clinician, Blood Rev, doi:10.1016/j.blre.2008.08.001
Laird, Rhodes, Kenny, Vitamin D and Inflammation: Potential Implications for Severity of Covid-19, Ir Med J
Lundqvist, Norlin, Wikvall, 1α,25-Dihydroxyvitamin D3 exerts tissue-specific effects on estrogen and androgen metabolism, Biochim Biophys Acta, doi:10.1016/j.bba-lip.2011.01.004
Martineau, Jolliffe, Hooper, Greenberg, Aloia et al., Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, Bmj, doi:10.1136/bmj.i6583
Mendelsohn, Protective effects of estrogen on the cardiovascular system, Am J Cardiol
Mjaess, Karam, Aoun, Albisinni, Roumeguère, COVID-19 and the male susceptibility: the role of ACE2, TMPRSS2 and the androgen receptor, Prog Urol, doi:10.1016/j.purol.2020.05.007
Mogharab, Ostovar, Ruszkowski, Hussain, Shrestha et al., Global burden of the COVID-19 associated patient-related delay in emergency healthcare: a panel of systematic review and meta-analyses, Global Health, doi:10.1186/s12992-022-00836-2
Pagano, Peruzzu, Ruggieri, Ortona, Gagliardi, None
Peckham, De Gruijter, Raine, Radziszewska, Ciurtin et al., Male sex identified by global COVID-19 metaanalysis as a risk factor for death and ITU admission, Nat Commun, doi:10.1038/s41467-020-19741-6
Pop-Kostova, Ruskovska, Clinical significance of circulating enzymes in patients with COVID-19, Knowledge -International Journal
Pop-Kostova, Ruskovska, Inflammatory biomarkers in patients with COVID-19, Knowledge -International Journal
Prof, Omer Xhemaili, Zurich, Prof, Dr et al., None
Saponaro, Franzini, Okoye, Antognoli, Campi et al., Is There a Crucial Link Between Vitamin D Status and Inflammatory Response in Patients With COVID-19?, Front Immunol, doi:10.3389/fimmu.2021.745713
Spanier, Nashold, Mayne, Nelson, Hayes, Vitamin D and estrogen synergy in Vdr-expressing CD4(+) T cells is essential to induce Helios(+)FoxP3(+) T cells and prevent autoimmune demyelinating disease, J Neuroimmunol, doi:10.1016/j.jneuroim.2015.06.015
Takase, Tsugawa, Sugiyama, Ikesue, Eto et al., Association between 25-hydroxyvitamin D levels and COVID-19 severity, Clin Nutr ESPEN, doi:10.1016/j.clne-sp.2022.04.003
Teymoori-Rad, Shokri, Salimi, Marashi, The interplay between vitamin D and viral infections, Rev Med Virol, doi:10.1002/rmv.2032
