Relationship of anti-SARS-CoV-2 IgG antibodies with Vitamin D and inflammatory markers in COVID-19 patients
et al., Scientific Reports, doi:10.1038/s41598-022-09785-7, Apr 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
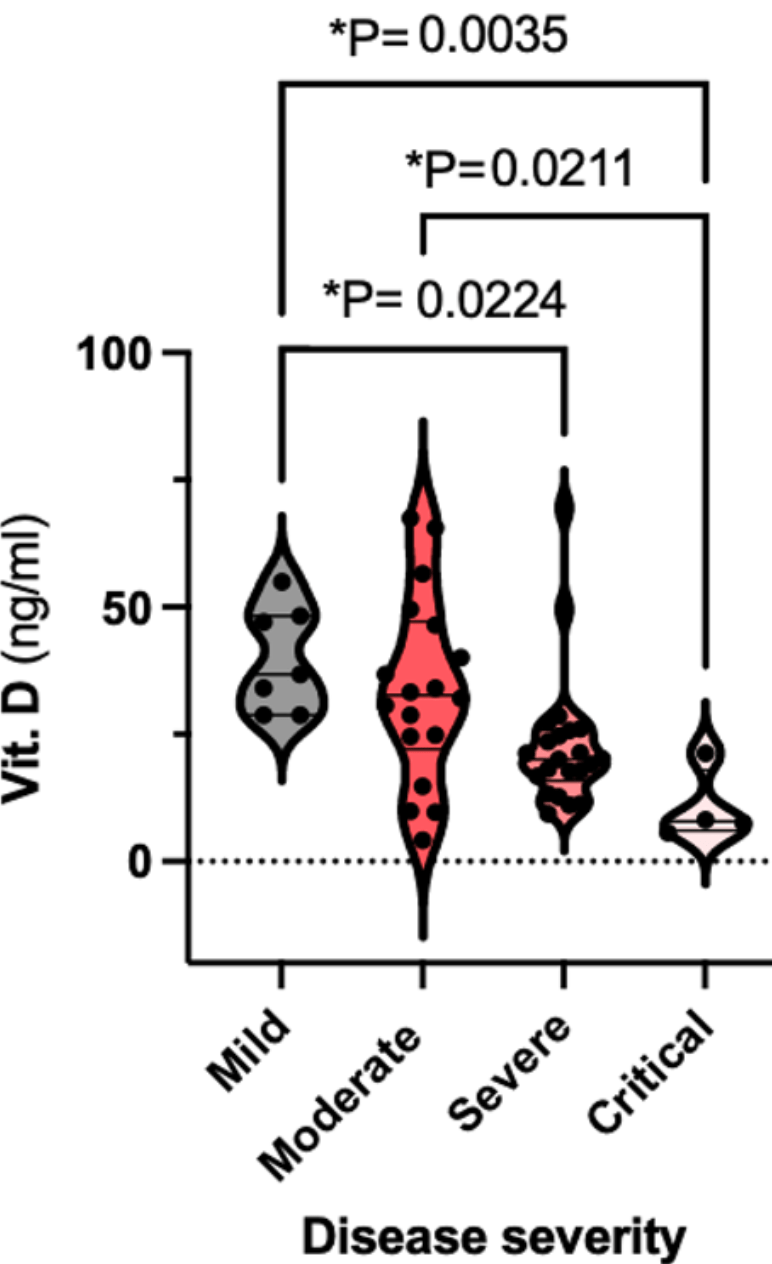
Prospective study of 69 COVID+ patients in Kosovo, showing lower vitamin D levels associated with COVID-19 severity.
Latifi-Pupovci et al., 5 Apr 2022, prospective, Kosovo, peer-reviewed, 9 authors.
Relationship of anti-SARS-CoV-2 IgG antibodies with Vitamin D and inflammatory markers in COVID-19 patients
Scientific Reports, doi:10.1038/s41598-022-09785-7
Several studies have found an association of COVID-19 disease severity with Vitamin D deficiency and higher levels of anti-SARS-CoV-2 IgGs. The aim of this study was to determine whether levels of Vitamin D and "inflammatory state" influence the magnitude of anti-SARS-CoV-2 IgGs levels in COVID-19 patients. For this purpose, in 67 patients levels of anti-SARS-CoV-2 IgG were measured in week 4 whereas in 52 patients levels of Vitamin D were measured in week 1 after symptom onset. We found that low Vitamin D levels were significantly associated with age and disease severity whereas there was a trend without significance, towards negative correlation of Vitamin D with anti-SARS-CoV-2 IgG. Anti-SARS-CoV-2 IgG were significantly higher in older ages, patients with severe disease, diabetes and those who received corticosteroid and antibiotic therapy. There was a positive correlation of anti-SARS-CoV-2 IgG with IL-6, CRP, LDH, ESR and with percentages of granulocytes. In conclusion, Vitamin D and anti-SARS-CoV-2 IgG share common parameters associated with inflammatory state. However, even though Vitamin D protects against severe forms of COVID-19 it could not directly affect anti-SARS-CoV-2 IgG production.
The coronavirus disease 2019 (COVID-19 ) is caused by a new coronavirus which in addition to acute respiratory failure is associated with systemic disorders such as hyperinflammation, hypercoagulation and vasculitis 1 . Although many people exhibit mild 'flu-like' symptoms, in severe responses systemic changes have been attributed to the cytokine storm accompanying severe inflammatory syndrome [2] [3] [4] . Severe forms of COVID-19 have been linked with low levels of circulating 25-hydroxy Vitamin D (25[OH]D) as an expression of Vitamin D (Vit. D) [5] [6] [7] [8] [9] [10] . Vit. D has immunomodulatory activity in response to invasion of bacterial and viral pathogens 11, 12 interacting with its receptor (VDR) in immune cells [13] [14] [15] . In several studies it was shown that severe inflammatory syndrome was accompanied with changes in hematological markers and increased several inflammatory markers such as CRP, LDH, ESR, ferritin etc. 2, [16] [17] [18] . A recent study has shown that in the presence of Vit. D, IL-6 induces higher production of IL-10, a known anti-inflammatory cytokine which is expected to lead to the reduction of inflammatory markers such as CRP 19 . Several studies have shown inverse association between Vit. D and CRP levels [20] [21] [22] . Additionally, high levels of CRP were associated with lowering levels of Vit. D 23 indicating that Vit. D is a negative acute phase reactant. Thus, Vit. D insufficiency could be the cause and effect of high CRP levels in COVID-19 patients. Humoral and cellular immune responses, two wings of adaptive immunity, are crucial in clearing a variety of viral infections 24 , and have been implicated in recovered COVID-19 patients 25, 26 . In several studies disease severity..
Ethics declaration. This study was approved by the Ethics Committee at University Clinical Centre of Kosova (reference no 2548/2020). Written informed consent was obtained from all participants, in accordance with the Declaration of Helsinki.
Author contributions
Competing interests The authors declare no competing interests.
References
Ahmed, A network-based analysis reveals the mechanism underlying vitamin D in suppressing cytokine storm and virus in SARS-CoV-2 infection, Front. Immunol, doi:10.3389/fimmu.2020.590459
Akter, Disease characteristics and serological responses in patients with differing severity of COVID-19 infection: A longitudinal cohort study in Dhaka, Bangladesh, PLoS Negl. Trop. Dis, doi:10.1371/journal.pntd.0010102
Ali, Elevated level of C-reactive protein may be an early marker to predict risk for severity of COVID-19, J. Med. Virol, doi:10.1002/jmv.26097
Ali, Role of vitamin D in preventing of COVID-19 infection, progression and severity, J. Infect. Public Health, doi:10.1016/j.jiph.2020.06.021
Almerighi, 1Alpha,25-dihydroxyvitamin D3 inhibits CD40L-induced pro-inflammatory and immunomodulatory activity in human monocytes, Cytokine, doi:10.1016/j.cyto.2008.12.009
Aoshi, Koyama, Kobiyama, Akira, Ishii, Innate and adaptive immune responses to viral infection and vaccination, Curr. Opin. Virol, doi:10.1016/j.coviro.2011.07.002
Baktash, Vitamin D status and outcomes for hospitalised older patients with COVID-19, Postgrad. Med. J, doi:10.1136/postgradmedj-2020-138712
Barassi, Vitamin D in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) patients with non-invasive ventilation support, Panminerva Med, doi:10.23736/S0031-0808.21.04277-4
Bellia, Serum 25-hydroxyvitamin D levels are inversely associated with systemic inflammation in severe obese subjects, Intern. Emerg. Med, doi:10.1007/s11739-011-0559-x
Bert, SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls, Nature, doi:10.1038/s41586-020-2550-z
Carpagnano, Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19, J. Endocrinol. Investig, doi:10.1007/s40618-020-01370-x
Chadha, Effect of 25-hydroxyvitamin D status on serological response to influenza vaccine in prostate cancer patients, Prostate, doi:10.1002/pros.21250
Charoenngam, Holick, Immunologic effects of vitamin D on human health and disease, Nutrients, doi:10.3390/nu12072097
Cruz, Interleukin-6 Is a biomarker for the development of fatal severe acute respiratory syndrome coronavirus 2 oxi, Front. Immunol, doi:10.3389/fimmu.2021.613422
Daneshkhah, Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01677-y
Darif, The pro-inflammatory cytokines in COVID-19 pathogenesis: What goes wrong?, Microb. Pathog, doi:10.1016/j.micpath.2021.104799
Demir, Demir, Aygun, Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease, J. Med. Virol, doi:10.1002/jmv.26832
Ebadi, Montano-Loza, Perspective: Improving vitamin D status in the management of COVID-19, Eur. J. Clin. Nutr, doi:10.1038/s41430-020-0661-0
Esperança-Martins, Humoral immune response of SARS-CoV-2-infected patients with cancer: Influencing factors and mechanisms, Oncologist, doi:10.1002/onco.13828
Faniyi, Vitamin D status and seroconversion for COVID-19 in UK healthcare workers, Eur. Respir. J, doi:10.1183/13993003.04234-2020
Figueiredo-Campos, Seroprevalence of anti-SARS-CoV-2 antibodies in COVID-19 patients and healthy volunteers up to 6 months post disease onset, Eur. J. Immunol, doi:10.1002/eji.202048970
Gao, The dichotomous and incomplete adaptive immunity in COVID-19 patients with different disease severity, Signal Transduct. Target Ther, doi:10.1038/s41392-021-00525-3
Ghasemian, The role of vitamin D in the age of COVID-19: A systematic review and meta-analysis, Int. J. Clin. Pract, doi:10.1111/ijcp.14675
Ghashut, Talwar, Kinsella, Duncan, Mcmillan, The effect of the systemic inflammatory response on plasma vitamin 25 (OH) D concentrations adjusted for albumin, PLoS One, doi:10.1371/journal.pone.0092614
Gozalbo-Rovira, SARS-CoV-2 antibodies, serum inflammatory biomarkers and clinical severity of hospitalized COVID-19 patients, J. Clin. Virol, doi:10.1016/j.jcv.2020.104611
Hastie, Pell, Sattar, Vitamin D and COVID-19 infection and mortality in UK Biobank, Eur. J. Nutr, doi:10.1007/s00394-020-02372-4
Hoepel, High titers and low fucosylation of early human anti-SARS-CoV-2 IgG promote inflammation by alveolar macrophages, Sci. Transl. Med, doi:10.1126/scitranslmed.abf8654
Honardoost, Ghavideldarestani, Khamseh, Role of Vitamin D in pathogenesis and severity of COVID-19 infection, Arch. Physiol. Biochem, doi:10.1080/13813455.2020.1792505
Ibarrondo, Rapid decay of anti-SARS-CoV-2 antibodies in persons with mild covid-19, N. Engl. J. Med, doi:10.1056/NEJMc2025179
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01570-8
Jain, Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers, Sci. Rep, doi:10.1038/s41598-020-77093-z
Jego, Plasmacytoid dendritic cells induce plasma cell differentiation through type I interferon and interleukin 6, Immunity, doi:10.1016/s1074-7613(03)00208-5
Kalia, Studzinski, Sarkar, Role of Vitamin D in regulating COVID-19 severity-An immunological perspective, J. Leukoc. Biol, doi:10.1002/JLB.4COVR1020-698R
Kaufman, Niles, Kroll, Bi, Holick, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One, doi:10.1371/journal.pone.0239252
Kebapcilar, Relationship between mean platelet volume and low-grade systemic coagulation with vitamin D deficiency in primary ovarian insufficiency, Arch. Gynecol. Obstet, doi:10.1007/s00404-013-2735-x
Kerget, Evaluation of the relationship of serum vitamin D levels in COVID-19 patients with clinical course and prognosis. COVID-19 hastalarında serum vitamin D düzeyinin klinik seyir ve prognozla ilişkisinin değerlendirilmesi, Tuberk Toraks, doi:10.5578/tt.70027
Kutsuna, Factors associated with anti-SARS-CoV-2 IgG antibody production in patients convalescing from COVID-19, J. Infect. Chemother, doi:10.1016/j.jiac.2021.01.006
Lee, Dynamics of anti-SARS-Cov-2 IgM and IgG antibodies among COVID-19 patients, J. Infect, doi:10.1016/j.jinf.2020.04.019
Li, Dynamic changes in anti-SARS-CoV-2 antibodies during SARS-CoV-2 infection and recovery from COVID-19, Nat. Commun, doi:10.1038/s41467-020-19943-y
Li, Patient and clinical factors at admission affect the levels of neutralizing antibodies six months after recovering from COVID-19, Viruses, doi:10.3390/v14010080
Li, Tong, Bare, Devlin, Assessment of the association of vitamin D level with SARS-CoV-2 seropositivity among working-age adults, JAMA Netw. Open, doi:10.1001/jamanetworkopen.2021.11634
Long, Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections, Nat. Med, doi:10.1038/s41591-020-0965-6
Ma, Decline of SARS-CoV-2-specific IgG, IgM and IgA in convalescent COVID-19 patients within 100 days after hospital discharge, Sci. China Life Sci, doi:10.1007/s11427-020-1805-0
Marklund, Serum-IgG responses to SARS-CoV-2 after mild and severe COVID-19 infection and analysis of IgG nonresponders, PLoS ONE, doi:10.1371/journal.pone.0241104
Mcgregor, An autocrine vitamin D-driven Th1 shutdown program can be exploited for COVID-19, doi:10.1101/2020.07.18.210161
Mellenthin, Association between serum vitamin D concentrations and inflammatory markers in the general adult population, Metabolism, doi:10.1016/j.metabol.2014.05.002
Moutchia, Clinical laboratory parameters associated with severe or critical novel coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis, PLoS One, doi:10.1371/journal.pone.0239802
Munshi, Vitamin D insufficiency as a potential culprit in critical COVID-19 patients, J. Med. Virol, doi:10.1002/jmv.26360
Ni, Detection of SARS-CoV-2-specific humoral and cellular immunity in COVID-19 convalescent individuals, Immunity, doi:10.1016/j.immuni.2020.04.023
Olbei, SARS-CoV-2 causes a different cytokine response compared to other cytokine storm-causing respiratory viruses in severely ill patients, Front. Immunol, doi:10.3389/fimmu.2021.629193
Palaniswamy, Could vitamin D reduce obesity-associated inflammation? Observational and Mendelian randomization study, Am. J. Clin. Nutr, doi:10.1093/ajcn/nqaa056
Robbiani, Convergent antibody responses to SARS-CoV-2 in convalescent individuals, Nature, doi:10.1038/s41586-020-2456-9
Sassi, Tamone, D' Amelio, Vitamin, nutrient, hormone, and immunomodulator, Nutrients, doi:10.3390/nu10111656
Sholukh, Evaluation of SARS-CoV-2 neutralization assays for antibody monitoring in natural infection and vaccine trials, doi:10.1101/2020.12.07.20245431
Terpos, Hematological findings and complications of COVID-19, Am. J. Hematol, doi:10.1002/ajh.25829
Thomson, Toscano-Guerra, Casis, Paciucci, C1 esterase inhibitor and the contact system in COVID-19, Br. J. Haematol, doi:10.1111/bjh.16938
Tjendra, Predicting disease severity and outcome in COVID-19 patients: A review of multiple biomarkers, Arch. Pathol. Lab. Med, doi:10.5858/arpa.2020-0471-SA
To, Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: An observational cohort study, Lancet Infect. Dis, doi:10.1016/S1473-3099(20)30196-1
Vinuesa, Linterman, Yu, Maclennan, Follicular helper T cells, Annu. Rev. Immunol, doi:10.1146/annurev-immunol-041015-055605
Wu, Clinical characteristics and immune injury mechanisms in 71 patients with COVID-19, mSphere, doi:10.1128/mSphere.00362-20
Yisak, Effects of Vitamin D on COVID-19 infection and prognosis: A systematic review, Risk Manag. Healthc. Policy, doi:10.2147/RMHP.S291584
Zhao, A comparative study of the laboratory features of COVID-19 and other viral pneumonias in the recovery stage, J. Clin. Lab. Anal, doi:10.1002/jcla.23483
Zhao, Antibody responses to SARS-CoV-2 in patients with novel coronavirus disease 2019, Clin. Infect. Dis, doi:10.1093/cid/ciaa344
DOI record:
{
"DOI": "10.1038/s41598-022-09785-7",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-022-09785-7",
"abstract": "<jats:title>Abstract</jats:title><jats:p>Several studies have found an association of COVID-19 disease severity with Vitamin D deficiency and higher levels of anti-SARS-CoV-2 IgGs. The aim of this study was to determine whether levels of Vitamin D and “inflammatory state” influence the magnitude of anti-SARS-CoV-2 IgGs levels in COVID-19 patients. For this purpose, in 67 patients levels of anti-SARS-CoV-2 IgG were measured in week 4 whereas in 52 patients levels of Vitamin D were measured in week 1 after symptom onset. We found that low Vitamin D levels were significantly associated with age and disease severity whereas there was a trend without significance, towards negative correlation of Vitamin D with anti-SARS-CoV-2 IgG. Anti-SARS-CoV-2 IgG were significantly higher in older ages, patients with severe disease, diabetes and those who received corticosteroid and antibiotic therapy. There was a positive correlation of anti-SARS-CoV-2 IgG with IL-6, CRP, LDH, ESR and with percentages of granulocytes. In conclusion, Vitamin D and anti-SARS-CoV-2 IgG share common parameters associated with inflammatory state. However, even though Vitamin D protects against severe forms of COVID-19 it could not directly affect anti-SARS-CoV-2 IgG production.</jats:p>",
"alternative-id": [
"9785"
],
"article-number": "5699",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "29 November 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "28 March 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "5 April 2022"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Latifi-Pupovci",
"given": "Hatixhe",
"sequence": "first"
},
{
"affiliation": [],
"family": "Namani",
"given": "Sadie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pajaziti",
"given": "Artina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ahmetaj-Shala",
"given": "Blerina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ajazaj",
"given": "Lindita",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kotori",
"given": "Afrim",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Haxhibeqiri",
"given": "Valdete",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gegaj",
"given": "Valentin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bunjaku",
"given": "Gramoz",
"sequence": "additional"
}
],
"container-title": [
"Scientific Reports"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
4,
5
]
],
"date-time": "2022-04-05T17:03:16Z",
"timestamp": 1649178196000
},
"deposited": {
"date-parts": [
[
2022,
4,
5
]
],
"date-time": "2022-04-05T17:16:52Z",
"timestamp": 1649179012000
},
"indexed": {
"date-parts": [
[
2022,
4,
5
]
],
"date-time": "2022-04-05T17:45:17Z",
"timestamp": 1649180717741
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "2045-2322"
}
],
"issue": "1",
"issued": {
"date-parts": [
[
2022,
4,
5
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2022,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
4,
5
]
],
"date-time": "2022-04-05T00:00:00Z",
"timestamp": 1649116800000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
4,
5
]
],
"date-time": "2022-04-05T00:00:00Z",
"timestamp": 1649116800000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-022-09785-7.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-022-09785-7",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-022-09785-7.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2022,
4,
5
]
]
},
"published-online": {
"date-parts": [
[
2022,
4,
5
]
]
},
"published-print": {
"date-parts": [
[
2022,
12
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1111/bjh.16938",
"author": "TM Thomson",
"doi-asserted-by": "publisher",
"first-page": "520",
"issue": "4",
"journal-title": "Br. J. Haematol.",
"key": "9785_CR1",
"unstructured": "Thomson, T. M., Toscano-Guerra, E., Casis, E. & Paciucci, R. C1 esterase inhibitor and the contact system in COVID-19. Br. J. Haematol. 190(4), 520–524. https://doi.org/10.1111/bjh.16938 (2020).",
"volume": "190",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2021.613422",
"author": "A Santa Cruz",
"doi-asserted-by": "publisher",
"journal-title": "Front. Immunol.",
"key": "9785_CR2",
"unstructured": "Santa Cruz, A. et al. Interleukin-6 Is a biomarker for the development of fatal severe acute respiratory syndrome coronavirus 2 oxi. Front. Immunol. 12, 613422. https://doi.org/10.3389/fimmu.2021.613422 (2021).",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2021.629193",
"author": "M Olbei",
"doi-asserted-by": "publisher",
"journal-title": "Front. Immunol.",
"key": "9785_CR3",
"unstructured": "Olbei, M. et al. SARS-CoV-2 causes a different cytokine response compared to other cytokine storm-causing respiratory viruses in severely ill patients. Front. Immunol. 12, 629193. https://doi.org/10.3389/fimmu.2021.629193 (2021).",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/j.micpath.2021.104799",
"author": "D Darif",
"doi-asserted-by": "publisher",
"journal-title": "Microb. Pathog.",
"key": "9785_CR4",
"unstructured": "Darif, D. et al. The pro-inflammatory cytokines in COVID-19 pathogenesis: What goes wrong?. Microb. Pathog. 153, 104799. https://doi.org/10.1016/j.micpath.2021.104799 (2021).",
"volume": "153",
"year": "2021"
},
{
"DOI": "10.1016/j.jiph.2020.06.021",
"author": "N Ali",
"doi-asserted-by": "publisher",
"first-page": "1373",
"issue": "10",
"journal-title": "J. Infect. Public Health.",
"key": "9785_CR5",
"unstructured": "Ali, N. Role of vitamin D in preventing of COVID-19 infection, progression and severity. J. Infect. Public Health. 13(10), 1373–1380. https://doi.org/10.1016/j.jiph.2020.06.021 (2020).",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2020.590459",
"author": "F Ahmed",
"doi-asserted-by": "publisher",
"journal-title": "Front. Immunol.",
"key": "9785_CR6",
"unstructured": "Ahmed, F. A network-based analysis reveals the mechanism underlying vitamin D in suppressing cytokine storm and virus in SARS-CoV-2 infection. Front. Immunol. 11, 590459. https://doi.org/10.3389/fimmu.2020.590459 (2020).",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1080/13813455.2020.1792505",
"author": "M Honardoost",
"doi-asserted-by": "publisher",
"journal-title": "Arch. Physiol. Biochem.",
"key": "9785_CR7",
"unstructured": "Honardoost, M., Ghavideldarestani, M. & Khamseh, M. E. Role of Vitamin D in pathogenesis and severity of COVID-19 infection. Arch. Physiol. Biochem. https://doi.org/10.1080/13813455.2020.1792505 (2020).",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"author": "PC Ilie",
"doi-asserted-by": "publisher",
"first-page": "1195",
"issue": "7",
"journal-title": "Aging Clin. Exp. Res.",
"key": "9785_CR8",
"unstructured": "Ilie, P. C., Stefanescu, S. & Smith, L. The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality. Aging Clin. Exp. Res. 32(7), 1195–1198. https://doi.org/10.1007/s40520-020-01570-8 (2020).",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1002/JLB.4COVR1020-698R",
"author": "V Kalia",
"doi-asserted-by": "publisher",
"first-page": "809",
"issue": "4",
"journal-title": "J. Leukoc. Biol.",
"key": "9785_CR9",
"unstructured": "Kalia, V., Studzinski, G. P. & Sarkar, S. Role of Vitamin D in regulating COVID-19 severity—An immunological perspective. J. Leukoc. Biol. 110(4), 809–819. https://doi.org/10.1002/JLB.4COVR1020-698R (2021).",
"volume": "110",
"year": "2021"
},
{
"DOI": "10.2147/RMHP.S291584",
"author": "H Yisak",
"doi-asserted-by": "publisher",
"first-page": "31",
"journal-title": "Risk Manag. Healthc. Policy.",
"key": "9785_CR10",
"unstructured": "Yisak, H. et al. Effects of Vitamin D on COVID-19 infection and prognosis: A systematic review. Risk Manag. Healthc. Policy. 14, 31–38. https://doi.org/10.2147/RMHP.S291584 (2021).",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.3390/nu12072097",
"author": "N Charoenngam",
"doi-asserted-by": "publisher",
"first-page": "2097",
"issue": "7",
"journal-title": "Nutrients",
"key": "9785_CR11",
"unstructured": "Charoenngam, N. & Holick, M. F. Immunologic effects of vitamin D on human health and disease. Nutrients 12(7), 2097. https://doi.org/10.3390/nu12072097 (2020).",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3390/nu10111656",
"author": "F Sassi",
"doi-asserted-by": "publisher",
"first-page": "1656",
"issue": "11",
"journal-title": "Nutrients",
"key": "9785_CR12",
"unstructured": "Sassi, F., Tamone, C. & D’Amelio, P. Vitamin D: nutrient, hormone, and immunomodulator. Nutrients 10(11), 1656. https://doi.org/10.3390/nu10111656 (2018).",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.1002/pros.21250",
"author": "MK Chadha",
"doi-asserted-by": "publisher",
"first-page": "368",
"issue": "4",
"journal-title": "Prostate",
"key": "9785_CR13",
"unstructured": "Chadha, M. K. et al. Effect of 25-hydroxyvitamin D status on serological response to influenza vaccine in prostate cancer patients. Prostate 71(4), 368–372. https://doi.org/10.1002/pros.21250 (2011).",
"volume": "71",
"year": "2011"
},
{
"DOI": "10.1007/s40520-020-01677-y",
"author": "A Daneshkhah",
"doi-asserted-by": "publisher",
"first-page": "2141",
"issue": "10",
"journal-title": "Aging Clin. Exp. Res.",
"key": "9785_CR14",
"unstructured": "Daneshkhah, A. et al. Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients. Aging Clin. Exp. Res. 32(10), 2141–2158. https://doi.org/10.1007/s40520-020-01677-y (2020).",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1038/s41430-020-0661-0",
"author": "M Ebadi",
"doi-asserted-by": "publisher",
"first-page": "856",
"issue": "6",
"journal-title": "Eur. J. Clin. Nutr.",
"key": "9785_CR15",
"unstructured": "Ebadi, M. & Montano-Loza, A. J. Perspective: Improving vitamin D status in the management of COVID-19. Eur. J. Clin. Nutr. 74(6), 856–859. https://doi.org/10.1038/s41430-020-0661-0 (2020).",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.1002/ajh.25829",
"author": "E Terpos",
"doi-asserted-by": "publisher",
"first-page": "834",
"issue": "7",
"journal-title": "Am. J. Hematol.",
"key": "9785_CR16",
"unstructured": "Terpos, E. et al. Hematological findings and complications of COVID-19. Am. J. Hematol. 95(7), 834–847. https://doi.org/10.1002/ajh.25829 (2020).",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0239802",
"author": "J Moutchia",
"doi-asserted-by": "publisher",
"issue": "10",
"journal-title": "PLoS One",
"key": "9785_CR17",
"unstructured": "Moutchia, J. et al. Clinical laboratory parameters associated with severe or critical novel coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. PLoS One 15(10), e0239802. https://doi.org/10.1371/journal.pone.0239802 (2020).",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1016/j.jcv.2020.104611",
"author": "R Gozalbo-Rovira",
"doi-asserted-by": "publisher",
"journal-title": "J. Clin. Virol.",
"key": "9785_CR18",
"unstructured": "Gozalbo-Rovira, R. et al. SARS-CoV-2 antibodies, serum inflammatory biomarkers and clinical severity of hospitalized COVID-19 patients. J. Clin. Virol. 131, 104611. https://doi.org/10.1016/j.jcv.2020.104611 (2020).",
"volume": "131",
"year": "2020"
},
{
"DOI": "10.1101/2020.07.18.210161",
"author": "R McGregor",
"doi-asserted-by": "publisher",
"journal-title": "bioRxiv",
"key": "9785_CR19",
"unstructured": "McGregor, R. et al. An autocrine vitamin D-driven Th1 shutdown program can be exploited for COVID-19. Preprint. bioRxiv https://doi.org/10.1101/2020.07.18.210161 (2020).",
"year": "2020"
},
{
"DOI": "10.1016/j.metabol.2014.05.002",
"author": "L Mellenthin",
"doi-asserted-by": "publisher",
"first-page": "1056",
"issue": "8",
"journal-title": "Metabolism",
"key": "9785_CR20",
"unstructured": "Mellenthin, L. et al. Association between serum vitamin D concentrations and inflammatory markers in the general adult population. Metabolism 63(8), 1056–1062. https://doi.org/10.1016/j.metabol.2014.05.002 (2014).",
"volume": "63",
"year": "2014"
},
{
"DOI": "10.1093/ajcn/nqaa056",
"author": "S Palaniswamy",
"doi-asserted-by": "publisher",
"first-page": "1036",
"issue": "5",
"journal-title": "Am. J. Clin. Nutr.",
"key": "9785_CR21",
"unstructured": "Palaniswamy, S. et al. Could vitamin D reduce obesity-associated inflammation? Observational and Mendelian randomization study. Am. J. Clin. Nutr. 111(5), 1036–1047. https://doi.org/10.1093/ajcn/nqaa056 (2020).",
"volume": "111",
"year": "2020"
},
{
"DOI": "10.1007/s11739-011-0559-x",
"author": "A Bellia",
"doi-asserted-by": "publisher",
"first-page": "33",
"issue": "1",
"journal-title": "Intern. Emerg. Med.",
"key": "9785_CR22",
"unstructured": "Bellia, A. et al. Serum 25-hydroxyvitamin D levels are inversely associated with systemic inflammation in severe obese subjects. Intern. Emerg. Med. 8(1), 33–40. https://doi.org/10.1007/s11739-011-0559-x (2013).",
"volume": "8",
"year": "2013"
},
{
"DOI": "10.1371/journal.pone.0092614",
"author": "RA Ghashut",
"doi-asserted-by": "publisher",
"issue": "3",
"journal-title": "PLoS One",
"key": "9785_CR23",
"unstructured": "Ghashut, R. A., Talwar, D., Kinsella, J., Duncan, A. & McMillan, D. C. The effect of the systemic inflammatory response on plasma vitamin 25 (OH) D concentrations adjusted for albumin. PLoS One 9(3), e92614. https://doi.org/10.1371/journal.pone.0092614 (2014).",
"volume": "9",
"year": "2014"
},
{
"DOI": "10.1016/j.coviro.2011.07.002",
"author": "T Aoshi",
"doi-asserted-by": "publisher",
"first-page": "226",
"issue": "4",
"journal-title": "Curr. Opin. Virol.",
"key": "9785_CR24",
"unstructured": "Aoshi, T., Koyama, S., Kobiyama, K., Akira, S. & Ishii, K. J. Innate and adaptive immune responses to viral infection and vaccination. Curr. Opin. Virol. 1(4), 226–232. https://doi.org/10.1016/j.coviro.2011.07.002 (2011).",
"volume": "1",
"year": "2011"
},
{
"DOI": "10.1038/s41586-020-2550-z",
"author": "N Le Bert",
"doi-asserted-by": "publisher",
"first-page": "457",
"issue": "7821",
"journal-title": "Nature",
"key": "9785_CR25",
"unstructured": "Le Bert, N. et al. SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls. Nature 584(7821), 457–462. https://doi.org/10.1038/s41586-020-2550-z (2020).",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1016/j.immuni.2020.04.023",
"author": "L Ni",
"doi-asserted-by": "publisher",
"first-page": "971",
"issue": "6",
"journal-title": "Immunity",
"key": "9785_CR26",
"unstructured": "Ni, L. et al. Detection of SARS-CoV-2-specific humoral and cellular immunity in COVID-19 convalescent individuals. Immunity 52(6), 971-977.e3. https://doi.org/10.1016/j.immuni.2020.04.023 (2020).",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa344",
"author": "J Zhao",
"doi-asserted-by": "publisher",
"first-page": "2027",
"issue": "16",
"journal-title": "Clin. Infect. Dis.",
"key": "9785_CR27",
"unstructured": "Zhao, J. et al. Antibody responses to SARS-CoV-2 in patients with novel coronavirus disease 2019. Clin. Infect. Dis. 71(16), 2027–2034. https://doi.org/10.1093/cid/ciaa344 (2020).",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.1038/s41591-020-0965-6",
"author": "QX Long",
"doi-asserted-by": "publisher",
"first-page": "1200",
"issue": "8",
"journal-title": "Nat. Med.",
"key": "9785_CR28",
"unstructured": "Long, Q. X. et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat. Med. 26(8), 1200–1204. https://doi.org/10.1038/s41591-020-0965-6 (2020).",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.04.019",
"author": "YL Lee",
"doi-asserted-by": "publisher",
"first-page": "e55",
"issue": "2",
"journal-title": "J. Infect.",
"key": "9785_CR29",
"unstructured": "Lee, Y. L. et al. Dynamics of anti-SARS-Cov-2 IgM and IgG antibodies among COVID-19 patients. J. Infect. 81(2), e55–e58. https://doi.org/10.1016/j.jinf.2020.04.019 (2020).",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2025179",
"author": "FJ Ibarrondo",
"doi-asserted-by": "publisher",
"first-page": "1085",
"issue": "11",
"journal-title": "N. Engl. J. Med.",
"key": "9785_CR30",
"unstructured": "Ibarrondo, F. J. et al. Rapid decay of anti-SARS-CoV-2 antibodies in persons with mild covid-19. N. Engl. J. Med. 383(11), 1085–1087. https://doi.org/10.1056/NEJMc2025179 (2020).",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1016/s1074-7613(03)00208-5",
"author": "G Jego",
"doi-asserted-by": "publisher",
"first-page": "225",
"issue": "2",
"journal-title": "Immunity",
"key": "9785_CR31",
"unstructured": "Jego, G. et al. Plasmacytoid dendritic cells induce plasma cell differentiation through type I interferon and interleukin 6. Immunity 19(2), 225–234. https://doi.org/10.1016/s1074-7613(03)00208-5 (2003).",
"volume": "19",
"year": "2003"
},
{
"DOI": "10.1016/j.jiac.2021.01.006",
"author": "S Kutsuna",
"doi-asserted-by": "publisher",
"first-page": "808",
"issue": "6",
"journal-title": "J. Infect. Chemother.",
"key": "9785_CR32",
"unstructured": "Kutsuna, S. et al. Factors associated with anti-SARS-CoV-2 IgG antibody production in patients convalescing from COVID-19. J. Infect. Chemother. 27(6), 808–813. https://doi.org/10.1016/j.jiac.2021.01.006 (2021).",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1146/annurev-immunol-041015-055605",
"author": "CG Vinuesa",
"doi-asserted-by": "publisher",
"first-page": "335",
"journal-title": "Annu. Rev. Immunol.",
"key": "9785_CR33",
"unstructured": "Vinuesa, C. G., Linterman, M. A., Yu, D. & MacLennan, I. C. Follicular helper T cells. Annu. Rev. Immunol. 34, 335–368. https://doi.org/10.1146/annurev-immunol-041015-055605 (2016).",
"volume": "34",
"year": "2016"
},
{
"DOI": "10.1183/13993003.04234-2020",
"author": "AA Faniyi",
"doi-asserted-by": "publisher",
"first-page": "2004234",
"issue": "4",
"journal-title": "Eur. Respir. J.",
"key": "9785_CR34",
"unstructured": "Faniyi, A. A. et al. Vitamin D status and seroconversion for COVID-19 in UK healthcare workers. Eur. Respir. J. 57(4), 2004234. https://doi.org/10.1183/13993003.04234-2020 (2021).",
"volume": "57",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0239252",
"author": "HW Kaufman",
"doi-asserted-by": "publisher",
"issue": "9",
"journal-title": "PLoS One",
"key": "9785_CR35",
"unstructured": "Kaufman, H. W., Niles, J. K., Kroll, M. H., Bi, C. & Holick, M. F. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLoS One 15(9), e0239252. https://doi.org/10.1371/journal.pone.0239252 (2020).",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26832",
"author": "M Demir",
"doi-asserted-by": "publisher",
"first-page": "2992",
"issue": "5",
"journal-title": "J. Med. Virol.",
"key": "9785_CR36",
"unstructured": "Demir, M., Demir, F. & Aygun, H. Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease. J. Med. Virol. 93(5), 2992–2999. https://doi.org/10.1002/jmv.26832 (2021).",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1007/s00404-013-2735-x",
"author": "AG Kebapcilar",
"doi-asserted-by": "publisher",
"first-page": "207",
"issue": "1",
"journal-title": "Arch. Gynecol. Obstet.",
"key": "9785_CR37",
"unstructured": "Kebapcilar, A. G. et al. Relationship between mean platelet volume and low-grade systemic coagulation with vitamin D deficiency in primary ovarian insufficiency. Arch. Gynecol. Obstet. 288(1), 207–212. https://doi.org/10.1007/s00404-013-2735-x (2013).",
"volume": "288",
"year": "2013"
},
{
"DOI": "10.1001/jamanetworkopen.2021.11634",
"author": "Y Li",
"doi-asserted-by": "publisher",
"issue": "5",
"journal-title": "JAMA Netw. Open.",
"key": "9785_CR38",
"unstructured": "Li, Y., Tong, C. H., Bare, L. A. & Devlin, J. J. Assessment of the association of vitamin D level with SARS-CoV-2 seropositivity among working-age adults. JAMA Netw. Open. 4(5), e2111634. https://doi.org/10.1001/jamanetworkopen.2021.11634 (2021).",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1111/ijcp.14675",
"author": "R Ghasemian",
"doi-asserted-by": "publisher",
"issue": "11",
"journal-title": "Int. J. Clin. Pract.",
"key": "9785_CR39",
"unstructured": "Ghasemian, R. et al. The role of vitamin D in the age of COVID-19: A systematic review and meta-analysis. Int. J. Clin. Pract. 75(11), e14675. https://doi.org/10.1111/ijcp.14675 (2021).",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"author": "A Jain",
"doi-asserted-by": "publisher",
"first-page": "20191",
"issue": "1",
"journal-title": "Sci. Rep.",
"key": "9785_CR40",
"unstructured": "Jain, A. et al. Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers. Sci. Rep. 10(1), 20191. https://doi.org/10.1038/s41598-020-77093-z (2020).",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.5578/tt.70027",
"author": "B Kerget",
"doi-asserted-by": "publisher",
"first-page": "227",
"issue": "3",
"journal-title": "Tuberk Toraks.",
"key": "9785_CR41",
"unstructured": "Kerget, B. et al. Evaluation of the relationship of serum vitamin D levels in COVID-19 patients with clinical course and prognosis. COVID-19 hastalarında serum vitamin D düzeyinin klinik seyir ve prognozla ilişkisinin değerlendirilmesi. Tuberk Toraks. 68(3), 227–235. https://doi.org/10.5578/tt.70027 (2020).",
"volume": "68",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26360",
"author": "R Munshi",
"doi-asserted-by": "publisher",
"first-page": "733",
"issue": "2",
"journal-title": "J. Med. Virol.",
"key": "9785_CR42",
"unstructured": "Munshi, R. et al. Vitamin D insufficiency as a potential culprit in critical COVID-19 patients. J. Med. Virol. 93(2), 733–740. https://doi.org/10.1002/jmv.26360 (2021).",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1007/s00394-020-02372-4",
"author": "CE Hastie",
"doi-asserted-by": "publisher",
"first-page": "545",
"issue": "1",
"journal-title": "Eur. J. Nutr.",
"key": "9785_CR43",
"unstructured": "Hastie, C. E., Pell, J. P. & Sattar, N. Vitamin D and COVID-19 infection and mortality in UK Biobank. Eur. J. Nutr. 60(1), 545–548. https://doi.org/10.1007/s00394-020-02372-4 (2021).",
"volume": "60",
"year": "2021"
},
{
"DOI": "10.1136/postgradmedj-2020-138712",
"author": "V Baktash",
"doi-asserted-by": "publisher",
"first-page": "442",
"issue": "1149",
"journal-title": "Postgrad. Med. J.",
"key": "9785_CR44",
"unstructured": "Baktash, V. et al. Vitamin D status and outcomes for hospitalised older patients with COVID-19. Postgrad. Med. J. 97(1149), 442–447. https://doi.org/10.1136/postgradmedj-2020-138712 (2021).",
"volume": "97",
"year": "2021"
},
{
"DOI": "10.1007/s40618-020-01370-x",
"author": "GE Carpagnano",
"doi-asserted-by": "publisher",
"first-page": "765",
"issue": "4",
"journal-title": "J. Endocrinol. Investig.",
"key": "9785_CR45",
"unstructured": "Carpagnano, G. E. et al. Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19. J. Endocrinol. Investig. 44(4), 765–771. https://doi.org/10.1007/s40618-020-01370-x (2021).",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1016/j.cyto.2008.12.009",
"author": "C Almerighi",
"doi-asserted-by": "publisher",
"first-page": "190",
"issue": "3",
"journal-title": "Cytokine",
"key": "9785_CR46",
"unstructured": "Almerighi, C. et al. 1Alpha,25-dihydroxyvitamin D3 inhibits CD40L-induced pro-inflammatory and immunomodulatory activity in human monocytes. Cytokine 45(3), 190–197. https://doi.org/10.1016/j.cyto.2008.12.009 (2009).",
"volume": "45",
"year": "2009"
},
{
"DOI": "10.1002/jmv.26097",
"author": "N Ali",
"doi-asserted-by": "publisher",
"first-page": "2409",
"issue": "11",
"journal-title": "J. Med. Virol.",
"key": "9785_CR47",
"unstructured": "Ali, N. Elevated level of C-reactive protein may be an early marker to predict risk for severity of COVID-19. J. Med. Virol. 92(11), 2409–2411. https://doi.org/10.1002/jmv.26097 (2020).",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.5858/arpa.2020-0471-SA",
"author": "Y Tjendra",
"doi-asserted-by": "publisher",
"first-page": "1465",
"issue": "12",
"journal-title": "Arch. Pathol. Lab. Med.",
"key": "9785_CR48",
"unstructured": "Tjendra, Y. et al. Predicting disease severity and outcome in COVID-19 patients: A review of multiple biomarkers. Arch. Pathol. Lab. Med. 144(12), 1465–1474. https://doi.org/10.5858/arpa.2020-0471-SA (2020).",
"volume": "144",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2456-9",
"author": "DF Robbiani",
"doi-asserted-by": "publisher",
"first-page": "437",
"issue": "7821",
"journal-title": "Nature",
"key": "9785_CR49",
"unstructured": "Robbiani, D. F. et al. Convergent antibody responses to SARS-CoV-2 in convalescent individuals. Nature 584(7821), 437–442. https://doi.org/10.1038/s41586-020-2456-9 (2020).",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1101/2020.12.07.20245431",
"author": "AM Sholukh",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv.",
"key": "9785_CR50",
"unstructured": "Sholukh, A. M. et al. Evaluation of SARS-CoV-2 neutralization assays for antibody monitoring in natural infection and vaccine trials. Preprint. medRxiv. https://doi.org/10.1101/2020.12.07.20245431 (2020).",
"year": "2020"
},
{
"DOI": "10.1038/s41467-020-19943-y",
"author": "K Li",
"doi-asserted-by": "publisher",
"first-page": "6044",
"issue": "1",
"journal-title": "Nat. Commun.",
"key": "9785_CR51",
"unstructured": "Li, K. et al. Dynamic changes in anti-SARS-CoV-2 antibodies during SARS-CoV-2 infection and recovery from COVID-19. Nat. Commun. 11(1), 6044. https://doi.org/10.1038/s41467-020-19943-y (2020).",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/S1473-3099(20)30196-1",
"author": "KK To",
"doi-asserted-by": "publisher",
"first-page": "565",
"issue": "5",
"journal-title": "Lancet Infect. Dis.",
"key": "9785_CR52",
"unstructured": "To, K. K. et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: An observational cohort study. Lancet Infect. Dis. 20(5), 565–574. https://doi.org/10.1016/S1473-3099(20)30196-1 (2020).",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1126/scitranslmed.abf8654",
"author": "W Hoepel",
"doi-asserted-by": "publisher",
"first-page": "eabf8654",
"issue": "596",
"journal-title": "Sci. Transl. Med.",
"key": "9785_CR53",
"unstructured": "Hoepel, W. et al. High titers and low fucosylation of early human anti-SARS-CoV-2 IgG promote inflammation by alveolar macrophages. Sci. Transl. Med. 13(596), eabf8654. https://doi.org/10.1126/scitranslmed.abf8654 (2021).",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1038/s41392-021-00525-3",
"author": "L Gao",
"doi-asserted-by": "publisher",
"first-page": "113",
"issue": "1",
"journal-title": "Signal Transduct. Target Ther.",
"key": "9785_CR54",
"unstructured": "Gao, L. et al. The dichotomous and incomplete adaptive immunity in COVID-19 patients with different disease severity. Signal Transduct. Target Ther. 6(1), 113. https://doi.org/10.1038/s41392-021-00525-3 (2021).",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1002/onco.13828",
"author": "M Esperança-Martins",
"doi-asserted-by": "publisher",
"first-page": "e1619",
"issue": "9",
"journal-title": "Oncologist.",
"key": "9785_CR55",
"unstructured": "Esperança-Martins, M. et al. Humoral immune response of SARS-CoV-2-infected patients with cancer: Influencing factors and mechanisms. Oncologist. 26(9), e1619–e1632. https://doi.org/10.1002/onco.13828 (2021).",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1371/journal.pntd.0010102",
"author": "A Akter",
"doi-asserted-by": "publisher",
"issue": "1",
"journal-title": "PLoS Negl. Trop. Dis.",
"key": "9785_CR56",
"unstructured": "Akter, A. et al. Disease characteristics and serological responses in patients with differing severity of COVID-19 infection: A longitudinal cohort study in Dhaka, Bangladesh. PLoS Negl. Trop. Dis. 16(1), e0010102. https://doi.org/10.1371/journal.pntd.0010102 (2022).",
"volume": "16",
"year": "2022"
},
{
"DOI": "10.3390/v14010080",
"author": "X Li",
"doi-asserted-by": "publisher",
"first-page": "80",
"issue": "1",
"journal-title": "Viruses",
"key": "9785_CR57",
"unstructured": "Li, X. et al. Patient and clinical factors at admission affect the levels of neutralizing antibodies six months after recovering from COVID-19. Viruses 14(1), 80. https://doi.org/10.3390/v14010080 (2022).",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1128/mSphere.00362-20",
"author": "Y Wu",
"doi-asserted-by": "publisher",
"first-page": "e00362",
"issue": "4",
"journal-title": "mSphere.",
"key": "9785_CR58",
"unstructured": "Wu, Y. et al. Clinical characteristics and immune injury mechanisms in 71 patients with COVID-19. mSphere. 5(4), e00362-e420. https://doi.org/10.1128/mSphere.00362-20 (2020).",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1002/jcla.23483",
"author": "G Zhao",
"doi-asserted-by": "publisher",
"issue": "10",
"journal-title": "J. Clin. Lab. Anal.",
"key": "9785_CR59",
"unstructured": "Zhao, G. et al. A comparative study of the laboratory features of COVID-19 and other viral pneumonias in the recovery stage. J. Clin. Lab. Anal. 34(10), e23483. https://doi.org/10.1002/jcla.23483 (2020).",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.23736/S0031-0808.21.04277-4",
"author": "A Barassi",
"doi-asserted-by": "publisher",
"journal-title": "Panminerva Med.",
"key": "9785_CR60",
"unstructured": "Barassi, A. et al. Vitamin D in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) patients with non-invasive ventilation support. Panminerva Med. https://doi.org/10.23736/S0031-0808.21.04277-4 (2021).",
"year": "2021"
},
{
"DOI": "10.1002/eji.202048970",
"author": "P Figueiredo-Campos",
"doi-asserted-by": "publisher",
"first-page": "2025",
"issue": "12",
"journal-title": "Eur. J. Immunol.",
"key": "9785_CR61",
"unstructured": "Figueiredo-Campos, P. et al. Seroprevalence of anti-SARS-CoV-2 antibodies in COVID-19 patients and healthy volunteers up to 6 months post disease onset. Eur. J. Immunol. 50(12), 2025–2040. https://doi.org/10.1002/eji.202048970 (2020).",
"volume": "50",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0241104",
"author": "E Marklund",
"doi-asserted-by": "publisher",
"issue": "10",
"journal-title": "PLoS ONE",
"key": "9785_CR62",
"unstructured": "Marklund, E. et al. Serum-IgG responses to SARS-CoV-2 after mild and severe COVID-19 infection and analysis of IgG non-responders. PLoS ONE 15(10), e0241104. https://doi.org/10.1371/journal.pone.0241104 (2020).",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1007/s11427-020-1805-0",
"author": "H Ma",
"doi-asserted-by": "publisher",
"first-page": "482",
"issue": "3",
"journal-title": "Sci. China Life Sci.",
"key": "9785_CR63",
"unstructured": "Ma, H. et al. Decline of SARS-CoV-2-specific IgG, IgM and IgA in convalescent COVID-19 patients within 100 days after hospital discharge. Sci. China Life Sci. 64(3), 482–485. https://doi.org/10.1007/s11427-020-1805-0 (2021).",
"volume": "64",
"year": "2021"
}
],
"reference-count": 63,
"references-count": 63,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41598-022-09785-7"
}
},
"score": 1,
"short-container-title": [
"Sci Rep"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": [
"Relationship of anti-SARS-CoV-2 IgG antibodies with Vitamin D and inflammatory markers in COVID-19 patients"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "12"
}
