Do selected lifestyle parameters affect the severity and symptoms of COVID-19 among elderly patients? The retrospective evaluation of individuals from the STOP-COVID registry of the PoLoCOV study
et al., Journal of Infection and Public Health, doi:10.1016/j.jiph.2022.12.008, NCT05018052, Dec 2022
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
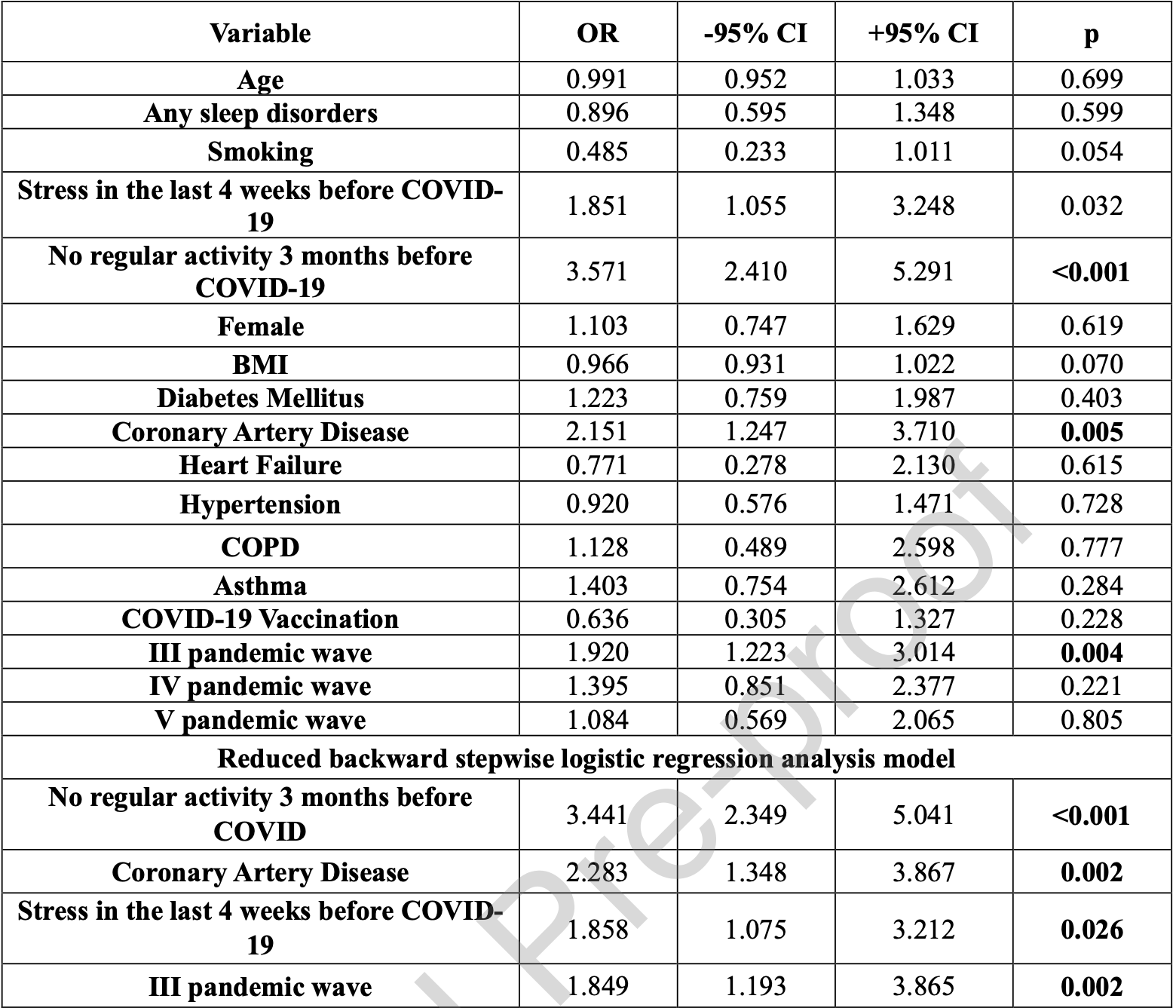
Retrospective 568 convalescent COVID-19 patients in Poland, showing lower risk of severe cases with regular physical activity in the 3 months before COVID-19.
|
risk of severe case, 70.9% lower, OR 0.29, p = 0.001, high activity levels 181, low activity levels 387, inverted to make OR<1 favor high activity levels, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Kapusta et al., 12 Dec 2022, retrospective, Poland, peer-reviewed, survey, mean age 70.4, 7 authors, study period 1 March, 2020 - 30 August, 2020, trial NCT05018052 (history).
Contact: joanna.kapusta@umed.lodz.pl, michalchudzik@wp.pl.
Do selected lifestyle parameters affect the severity and symptoms of COVID-19 among elderly patients? The retrospective evaluation of individuals from the STOP-COVID registry of the PoLoCOV study
Journal of Infection and Public Health, doi:10.1016/j.jiph.2022.12.008
This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author contributions: JKinterpretation of obtained results, preparation of the text of the study, review and editing. MCdevelopment of assumptions and research methods, collecting source materials and carrying out research, preparation of the text of the study; ŻKKpreparation of the text of the study, data collection, review and editing; DKpreparation of the text of the study, data collection, review and editing; MBustatistical analysis of research results, interpretation of the obtained results; PJinterpretation of obtained results, review and editing; MBastatistical analysis of research results, interpretation of the obtained results, preparation of the text of the study, review and editing.
Competing interests: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Data and materials availability: The data underlying this article cannot be shared publicly, to protect the privacy of individuals that participated in the study.
Conflicts of Interest: The authors declare no conflict of interest.
References
Abdelbasset, Stay Home: Role of Physical Exercise Training in Elderly Individuals' Ability to Face the COVID-19 Infection, J Immunol Res, doi:10.1155/2020/8375096
Abdulhasan, Ruden, Rappolee, Dutta, Gurdziel et al., Stress Decreases Host Viral Resistance and Increases Covid Susceptibility in Embryonic Stem Cells, Stem Cell Rev Rep, doi:10.1007/s12015-021-10188-w
Akinci, Basar, Relationship between sleep quality and the psychological status of patients hospitalised with COVID-19, Sleep Med, doi:10.1016/j.sleep.2021.01.034
Ayling, Jia, Coupland, Chalder, Massey et al., Psychological Predictors of Self-reported COVID-19 Outcomes: Results From a Prospective Cohort Study, Ann Behav Med, doi:10.1093/abm/kaab106
Baum, Poukka, Leino, Kilpi, Nohynek et al., High vaccine effectiveness against severe Covid-19 in the elderly in Finland before and after the emergence of Omicron, doi:10.1101/2022.03.11.22272140
Bentlage, Ammar, How, Ahmed, Trabelsi et al., Practical Recommendations for Maintaining Active Lifestyle during the COVID-19 Pandemic: A Systematic Literature Review, Int J Environ Res Public Health, doi:10.3390/ijerph17176265
Betancourt-Peña, Rodríguez-Castro, Avila-Valencia, Benavides, Clinical Condition and Symptoms of Patients with Copd with Sars-Cov-2 Infection, Chest, doi:10.1016/j.chest.2021.07.1626
Bhat, Chokroverty, Sleep disorders and COVID-19, Sleep Med, doi:10.1016/j.sleep.2021.07.021
Bielik, Grendar, Kolisek, A Possible Preventive Role of Physically Active Lifestyle during the SARS-CoV-2 Pandemic; Might Regular Cold-Water Swimming and Exercise Reduce the Symptom Severity of COVID-19?, Int J Environ Res Public Health, doi:10.3390/ijerph18137158
Cenko, Badimon, Bugiardini, Claeys, Luca et al., Cardiovascular disease and COVID-19: a consensus paper from the ESC Working Group on Coronary Pathophysiology & Microcirculation, ESC Working Group on Thrombosis and the Association for Acute CardioVascular Care (ACVC), in collaboration with the European Heart Rhythm Association (EHRA), Cardiovasc Res, doi:10.1093/cvr/cvab298.JournalPre-proof
Chastin, Abaraogu, Bourgois, Dall, Darnborough et al., Effects of Regular Physical Activity on the Immune System, Vaccination and Risk of Community-Acquired Infectious Disease in the General Population: Systematic Review and Meta-Analysis, Sports Med, doi:10.1007/s40279-021-01466-1
Chudzik, Babicki, Kapusta, Kolat, Kaluzinska et al., Do the Successive Waves of SARS-CoV-2, Vaccination Status and Place of Infection Influence the Clinical Picture and COVID-19 Severity among Patients with Persistent Clinical Symptoms? The Retrospective Study of Patients from the STOP-COVID Registry of the PoLoCOV-Study, J Pers Med, doi:10.3390/jpm12050706
Ciaula, Krawczyk, Filipiak, Geier, Bonfrate et al., Noncommunicable diseases, climate change and iniquities: What COVID-19 has taught us about syndemic, Eur J Clin Invest, doi:10.1111/eci.13682
Clerkin, Fried, Raikhelkar, Sayer, Griffin et al., COVID-19 and Cardiovascular Disease, Circulation, doi:10.1161/CIRCULATIONAHA.120.046941
Cortes-Borra, Aranda-Abreu, Amantadine in the prevention of clinical symptoms caused by SARS-CoV-2, Pharmacol Rep, doi:10.1007/s43440-021-00231-5
Dadras, Seyedalinaghi, Karimi, Shamsabadi, Qaderi et al., COVID-19 mortality and its predictors in the elderly: A systematic review, Health Sci Rep, doi:10.1002/hsr2.657
De Frel, Atsma, Pijl, Seidell, Leenen et al., The Impact of Obesity and Lifestyle on the Immune System and Susceptibility to Infections Such as COVID-19, Front Nutr, doi:10.3389/fnut.2020.597600
Doerre, Doblhammer, The influence of gender on COVID-19 infections and mortality in Germany: Insights from age-and gender-specific modeling of contact rates, infections, and deaths in the early phase of the pandemic, PLoS One, doi:10.1371/journal.pone.0268119
Driggin, Madhavan, Bikdeli, Chuich, Laracy et al., Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic, J Am Coll Cardiol, doi:10.1016/j.jacc.2020.03.031
Farshbafnadi, Zonouzi, Sabahi, Dolatshahi, Aarabi, Aging & COVID-19 susceptibility, disease severity, and clinical outcomes: The role of entangled risk factors, Exp Gerontol, doi:10.1016/j.exger.2021.111507
Fernandez-De-Las-Penas, Pellicer-Valero, Navarro-Pardo, Gomez-Mayordomo, Cuadrado, Female Sex Is a Risk Factor Associated with Long-Term Post-COVID Related-Symptoms but Not with COVID-19 Symptoms: The LONG-COVID-EXP-CM Multicenter Study, J Clin Med, doi:10.3390/jcm11020413
Filgueira, Castoldi, Santos, De Amorim, De Sousa Fernandes et al., The Relevance of a Physical Active Lifestyle and Physical Fitness on Immune Defense: Mitigating Disease Burden, With Focus on COVID-19 Consequences, Front Immunol, doi:10.3389/fimmu.2021.587146
Gerayeli, Milne, Cheung, Li, Yang et al., COPD and the risk of poor outcomes in COVID-19: A systematic review and meta-analysis, EClinicalMedicine, doi:10.1016/j.eclinm.2021.100789
Gibson, Qin, Puah, COVID-19 acute respiratory distress syndrome (ARDS): clinical features and differences from typical pre-COVID-19 ARDS, Med J Aust, doi:10.5694/mja2.50674
Grolli, Mingoti, Bertollo, Luzardo, Quevedo et al., Impact of COVID-19 in the Mental Health in Elderly: Psychological and Biological Updates, Mol Neurobiol, doi:10.1007/s12035-020-02249-x
Gujski, Mularczyk-Tomczewska, Raciborski, Samel-Kowalik, Samolinski et al., Screening for SARS-CoV-2 Infection in Students at the Medical University of Warsaw, Poland Between November 15 and, Med Sci Monit, doi:10.12659/MSM.936962
Hadjistavropoulos, Asmundson, COVID stress in older adults: Considerations during the Omicron wave and beyond, J Anxiety Disord, doi:10.1016/j.janxdis.2022.102535
Hamer, Kivimaki, Gale, Batty, Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK, Brain Behav Immun, doi:10.1016/j.bbi.2020.05.059
He, Cheng, Feng, Wan, Chen et al., Clinical Symptom Differences Between Mild and Severe COVID-19 Patients in China: A Meta-Analysis, Front Public Health, doi:10.3389/fpubh.2020.561264
Higham, Mathioudakis, Vestbo, Singh, COVID-19 and COPD: a narrative review of the basic science and clinical outcomes, Eur Respir Rev, doi:10.1183/16000617.0199-2020
Holly, Biernacka, Maskell, Perks, Obesity, Diabetes and COVID-19: An Infectious Disease Spreading From the East Collides With the Consequences of an Unhealthy J o u r n a l P r e -p r o o f Western Lifestyle, Front Endocrinol, doi:10.3389/fendo.2020.582870
Holshue, Debolt, Lindquist, Lofy, Wiesman et al., First Case of 2019 Novel Coronavirus in the United States, N Engl J Med, doi:10.1056/NEJMoa2001191.JournalPre-proof
Ibarra-Coronado, Martinez, Velazquez-Moctezuma, Garcia, Mendez-Diaz et al., The Bidirectional Relationship between Sleep and Immunity against Infections, J Immunol Res, doi:10.1155/2015/678164
J O U R N A L P R E, -p r o o f
Jacobs, Paleoudis, Bari, Nyirenda, Friedman et al., Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection, PLoS One, doi:10.1371/journal.pone.0243882
Jassat, Karim, Mudara, Welch, Ozougwu et al., Clinical severity of COVID-19 in patients admitted to hospital during the omicron wave in South Africa: a retrospective observational study, Lancet Glob Health, doi:10.1016/S2214-109X(22)00114-0
Jimeno-Almazan, Pallares, Buendia-Romero, Martinez-Cava, Franco-Lopez et al., Post-COVID-19 Syndrome and the Potential Benefits of Exercise, Int J Environ Res Public Health, doi:10.3390/ijerph18105329
Jin, Bai, He, Wu, Liu et al., Gender Differences in Patients With COVID-19: Focus on Severity and Mortality, Front Public Health, doi:10.3389/fpubh.2020.00152
Karadavut, Altintop, Long-term cardiovascular adverse events in very elderly COVID-19 patients, Arch Gerontol Geriatr, doi:10.1016/j.archger.2022.104628
Kim, Hegde, Lafiura, Raghavan, Luong et al., COVID-19 illness in relation to sleep and burnout, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2021-000228
Klein, Flanagan, Sex differences in immune responses, Nat Rev Immunol, doi:10.1038/nri.2016.90
Lane, Hunter, Lee, Hyman, Bross et al., Clinical characteristics and symptom duration among outpatients with COVID-19, Am J Infect Control, doi:10.1016/j.ajic.2021.10.039
Langhammer, Bergland, Rydwik, The Importance of Physical Activity Exercise among Older People, Biomed Res Int, doi:10.1155/2018/7856823
Lee, Park, Jeong, Ahn, Choi et al., Immunophenotyping of COVID-19 and influenza highlights the role of type I interferons in development of severe COVID-19, Sci Immunol, doi:10.1126/sciimmunol.abd1554
Leung, Yang, Tam, Shaipanich, Hackett et al., ACE-2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19, Eur Respir J
Li, Guan, Su, Liu, Chen et al., Impact of cardiovascular disease and cardiac injury on in-hospital mortality in patients with COVID-19: a systematic review and meta-analysis, Heart, doi:10.1136/heartjnl-2020-317062
Li, Li, Qing, Hu, COVID-19 and the Change in Lifestyle: Bodyweight, Time Allocation, and Food Choices, Int J Environ Res Public Health, doi:10.3390/ijerph181910552
Lippi, Henry, Chronic obstructive pulmonary disease is associated with severe coronavirus disease 2019 (COVID-19), Respir Med, doi:10.1016/j.rmed.2020.105941
Liu, Wang, Sun, Teng, Li et al., Thrombosis and Coagulopathy in COVID-19: Current Understanding and Implications for Antithrombotic Treatment in Patients Treated With Percutaneous Coronary Intervention, Front Cardiovasc Med, doi:10.3389/fcvm.2020.599334
Madjid, Safavi-Naeini, Solomon, Vardeny, Potential Effects of Coronaviruses on the Cardiovascular System: A Review, JAMA Cardiol, doi:10.1001/jamacardio.2020.1286
Mallia, Message, Gielen, Contoli, Gray et al., Experimental rhinovirus infection as a human model of chronic obstructive pulmonary disease exacerbation, Am J Respir Crit Care Med, doi:10.1164/rccm.201006-0833OC
Matsunaga, Hayakawa, Asai, Tsuzuki, Terada et al., Clinical characteristics of the first three waves of hospitalised patients with COVID-19 in Japan prior to the widespread use of vaccination: a nationwide observational study, Lancet Reg Health West Pac, doi:10.1016/j.lanwpc.2022.100421
Milne, Yang, Timens, Bosse, Sin, SARS-CoV-2 receptor ACE2 gene expression and RAAS inhibitors, Lancet Respir Med, doi:10.1016/S2213-2600(20)30224-1
Napoli, Tritto, Benincasa, Mansueto, Cardiovascular involvement during COVID-19 and clinical implications in elderly patients. A review, Ann Med Surg (Lond), doi:10.1016/j.amsu.2020.07.054
Pataka, Kotoulas, Sakka, Katsaounou, Pappa, Sleep Dysfunction in COVID-19 Patients: Prevalence, Risk Factors, Mechanisms, and Management, J Pers Med, doi:10.3390/jpm11111203
Pela, Goldoni, Solinas, Cavalli, Tagliaferri et al., Sex-Related Differences in Long-COVID-19 Syndrome, J Womens Health (Larchmt), doi:10.1089/jwh.2021.0411
Petrilli, Jones, Yang, Rajagopalan, Donnell et al., Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study, BMJ, doi:10.1136/bmj.m1966
Popp, Stegemann, Metzendorf, Gould, Kranke et al., Ivermectin for preventing and treating COVID-19, Cochrane Database Syst Rev, doi:10.1002/14651858.CD015017.pub2
Popp, Stegemann, Riemer, Metzendorf, Romero et al., Antibiotics for the treatment of COVID-19, Cochrane Database Syst Rev, doi:10.1002/14651858.CD015025
Radhakrishnan, Govindaraj, Sasidharan, Ravindra, Yadav et al., People with dyssomnia showed increased vulnerability to CoVID-19 pandemic: a questionnaire-based study exploring the patterns and predictors of sleep quality using the latent class analysis technique in Indian population, Sleep Med, doi:10.1016/j.sleep.2020.12.041
Ronchini, Gandini, Pasqualato, Mazzarella, Facciotti et al., Lower probability and shorter duration of infections after COVID-19 vaccine correlate with anti-SARS-CoV-2 circulating IgGs, PLoS One, doi:10.1371/journal.pone.0263014
Roschel, Artioli, Gualano, Risk of Increased Physical Inactivity During COVID-19 Outbreak in Older People: A Call for Actions, J Am Geriatr Soc, doi:10.1111/jgs.16550
Sallis, Young, Tartof, Sallis, Sall et al., Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients, Br J Sports Med, doi:10.1136/bjsports-2021-104080
Scartoni, Sant'ana, Lo, Murillo-Rodriguez, Yamamoto et al., Physical Exercise and Immune System in the Elderly: Implications and Importance in COVID-19 Pandemic Period, Front Psychol, doi:10.3389/fpsyg.2020.593903
Schetelig, Baldauf, Wendler, Heidenreich, Real et al., Risk Factors for a Severe Course of COVID-19 in Persons Aged 18 to 61, Dtsch Arztebl Int, doi:10.3238/arztebl.m2021.0200
Schou, Joca, Wegener, Richter, Psychiatric and neuropsychiatric sequelae of COVID-19 -A systematic review, Brain Behav Immun, doi:10.1016/j.bbi.2021.07.018
Sharma, Volgman, Michos, Sex Differences in Mortality From COVID-19 Pandemic: Are Men Vulnerable and Women Protected?, JACC Case Rep, doi:10.1016/j.jaccas.2020.04.027
Simonnet, Chetboun, Poissy, Raverdy, Noulette et al., High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2)
Singh, Kishore, Singh, Pathak, Ranjan, Higher BCG-induced trained immunity prevalence predicts protection from COVID-19: Implications for ongoing BCG trials, Clin Transl Discov, doi:10.1002/ctd2.60
Sjoberg, Triolo, Saadeh, Dekhtyar, Calderon-Larranaga et al., Factors associated with physical activity reduction in Swedish older adults during the first COVID-19 outbreak: a longitudinal population-based study, Eur Rev Aging Phys Act, doi:10.1186/s11556-022-00287-z
Stewart, Newson, Briggs, Grammatopoulos, Young et al., Long COVID risk -a signal to address sex hormones and women's health, Lancet Reg Health Eur, doi:10.1016/j.lanepe.2021.100242
Sylvester, Rusu, Chan, Bellows, 'keefe et al., Sex differences in sequelae from COVID-19 infection and in long COVID syndrome: a review, Curr Med Res Opin, doi:10.1080/03007995.2022
Tenforde, Kim, Lindsell, Rose, Shapiro et al., Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network -United States, March, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6930e1
Thompson, Burgess, Naleway, Tyner, Yoon et al., Prevention and Attenuation of Covid-19 with the BNT162b2 and mRNA-1273 Vaccines, N Engl J Med, doi:10.1056/NEJMoa2107058
Ugarte, Achilleos, Quattrocchi, Gabel, Kolokotroni et al., Premature mortality attributable to COVID-19: potential years of life lost in 17 countries around the world, January, BMC Public Health, doi:10.1186/s12889-021-12377-1
Vegivinti, Evanson, Lyons, Akosman, Barrett et al., Efficacy of antiviral therapies for COVID-19: a systematic review of randomized controlled trials, BMC Infect Dis, doi:10.1186/s12879-
Vf, Madjid, Musher, Role of acute infection in triggering acute coronary syndromes, Lancet Infect Dis, doi:10.1016/S1473-3099
Visseren, Mach, Smulders, Carballo, Koskinas et al., ESC Guidelines on cardiovascular disease prevention in clinical practice, Eur Heart J, doi:10.1093/eurheartj/ehab484
Wang, Hu, Hu, Zhu, Liu et al., Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China, JAMA, doi:10.1001/jama.2020.1585
Wolff, Nee, Hickey, Marschollek, Risk factors for Covid-19 severity and fatality: a structured literature review, Infection, doi:10.1007/s15010-020-01509-1
Worldometer, Worldometer's COVID-19 Data
Yang, An Acute Respiratory Infection Runs Into the Most Common Noncommunicable Epidemic-COVID-19 and Cardiovascular Diseases, JAMA Cardiol, doi:10.1001/jamacardio.2020.0934
Yuan, Huang, Chen, Chen, Zhang et al., Does pre-existent physical inactivity have a role in the severity of COVID-19?, Ther Adv Respir Dis, doi:10.1177/17534666211025221
Zaki, Alashwal, Association of hypertension, diabetes, stroke, cancer, kidney disease, and high-cholesterol with COVID-19 disease severity and fatality: A systematic review, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.07.005
Zeng, Huang, Pan, How to balance acute myocardial infarction and COVID-19: the protocols from Sichuan Provincial People's Hospital, Intensive Care Med, doi:10.1007/s00134-020-05993-9
Zhang, Cui, Shen, Zhang, Liu et al., Association of diabetes mellitus with disease severity and prognosis in COVID-19: A retrospective cohort study, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108227
Zhang, Dong, Cao, Yuan, Yang et al., Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China, Allergy, doi:10.1111/all.14238
Zhang, Xu, Xie, Zhang, Huang et al., Poor-sleep is associated with slow recovery from lymphopenia and an increased need for ICU care in hospitalized patients with COVID-19: A retrospective cohort study, Brain Behav Immun, doi:10.1016/j.bbi.2020.05.075
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736
Ziegler, Allon, Nyquist, Mbano, Miao et al., SARS-CoV-2 Receptor ACE2 Is an Interferon-Stimulated Gene in Human Airway Epithelial Cells and Is Detected in Specific Cell Subsets across Tissues, Cell, doi:10.1016/j.cell.2020.04.035
DOI record:
{
"DOI": "10.1016/j.jiph.2022.12.008",
"ISSN": [
"1876-0341"
],
"URL": "http://dx.doi.org/10.1016/j.jiph.2022.12.008",
"alternative-id": [
"S1876034122003495"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Do selected lifestyle parameters affect the severity and symptoms of COVID-19 among elderly patients? The retrospective evaluation of individuals from the STOP-COVID registry of the PoLoCOV study"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Journal of Infection and Public Health"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.jiph.2022.12.008"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2022 Published by Elsevier Ltd on behalf of King Saud Bin Abdulaziz University for Health Sciences."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-5082-3641",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kapusta",
"given": "Joanna",
"sequence": "first"
},
{
"affiliation": [],
"family": "Chudzik",
"given": "Michał",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kałuzińska-Kołat",
"given": "Żaneta",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kołat",
"given": "Damian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Burzyńska",
"given": "Monika",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6223-8821",
"affiliation": [],
"authenticated-orcid": false,
"family": "Jankowski",
"given": "Piotr",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7719-6959",
"affiliation": [],
"authenticated-orcid": false,
"family": "Babicki",
"given": "Mateusz",
"sequence": "additional"
}
],
"container-title": "Journal of Infection and Public Health",
"container-title-short": "Journal of Infection and Public Health",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2022,
12,
12
]
],
"date-time": "2022-12-12T16:32:19Z",
"timestamp": 1670862739000
},
"deposited": {
"date-parts": [
[
2022,
12,
12
]
],
"date-time": "2022-12-12T16:33:18Z",
"timestamp": 1670862798000
},
"indexed": {
"date-parts": [
[
2022,
12,
12
]
],
"date-time": "2022-12-12T17:11:49Z",
"timestamp": 1670865109829
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
12
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
12,
1
]
],
"date-time": "2022-12-01T00:00:00Z",
"timestamp": 1669852800000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 8,
"start": {
"date-parts": [
[
2022,
12,
9
]
],
"date-time": "2022-12-09T00:00:00Z",
"timestamp": 1670544000000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S1876034122003495?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S1876034122003495?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
12
]
]
},
"published-print": {
"date-parts": [
[
2022,
12
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1056/NEJMoa2001191",
"article-title": "First Case of 2019 Novel Coronavirus in the United States",
"author": "Holshue",
"doi-asserted-by": "crossref",
"first-page": "929",
"issue": "10",
"journal-title": "N Engl J Med",
"key": "10.1016/j.jiph.2022.12.008_bib1",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.5694/mja2.50674",
"article-title": "COVID-19 acute respiratory distress syndrome (ARDS): clinical features and differences from typical pre-COVID-19 ARDS",
"author": "Gibson",
"doi-asserted-by": "crossref",
"first-page": "54",
"issue": "2",
"journal-title": "Med J Aust",
"key": "10.1016/j.jiph.2022.12.008_bib2",
"volume": "213",
"year": "2020"
},
{
"key": "10.1016/j.jiph.2022.12.008_bib3",
"unstructured": "World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19, https://www.who.int/emergencies/diseases/novel-coronavi-rus-2019/events-as-theyhappen; 2020 [accessed 18 February 2022]."
},
{
"key": "10.1016/j.jiph.2022.12.008_bib4",
"unstructured": "Our World in Data. Daily new confirmed COVID-19 deaths per million people, https://ourworldindata.org/explorers/coronavirus-data-explorer; 2020 [accessed 20 February 2022]."
},
{
"DOI": "10.3390/ijerph17176265",
"article-title": "Practical Recommendations for Maintaining Active Lifestyle during the COVID-19 Pandemic: A Systematic Literature Review",
"author": "Bentlage",
"doi-asserted-by": "crossref",
"issue": "17",
"journal-title": "Int J Environ Res Public Health",
"key": "10.1016/j.jiph.2022.12.008_bib5",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1111/jgs.16550",
"article-title": "Risk of Increased Physical Inactivity During COVID-19 Outbreak in Older People: A Call for Actions",
"author": "Roschel",
"doi-asserted-by": "crossref",
"first-page": "1126",
"issue": "6",
"journal-title": "J Am Geriatr Soc",
"key": "10.1016/j.jiph.2022.12.008_bib6",
"volume": "68",
"year": "2020"
},
{
"article-title": "Risk Factors for a Severe Course of COVID-19 in Persons Aged 18 to 61",
"author": "Schetelig",
"first-page": "288",
"issue": "16",
"journal-title": "Dtsch Arztebl Int",
"key": "10.1016/j.jiph.2022.12.008_bib7",
"volume": "118",
"year": "2021"
},
{
"DOI": "10.1007/s15010-020-01509-1",
"article-title": "Risk factors for Covid-19 severity and fatality: a structured literature review",
"author": "Wolff",
"doi-asserted-by": "crossref",
"first-page": "15",
"issue": "1",
"journal-title": "Infection",
"key": "10.1016/j.jiph.2022.12.008_bib8",
"volume": "49",
"year": "2021"
},
{
"DOI": "10.3389/fpubh.2020.00152",
"article-title": "Gender Differences in Patients With COVID-19: Focus on Severity and Mortality",
"author": "Jin",
"doi-asserted-by": "crossref",
"first-page": "152",
"journal-title": "Front Public Health",
"key": "10.1016/j.jiph.2022.12.008_bib9",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1966",
"article-title": "Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study",
"author": "Petrilli",
"doi-asserted-by": "crossref",
"first-page": "m1966",
"journal-title": "BMJ",
"key": "10.1016/j.jiph.2022.12.008_bib10",
"volume": "369",
"year": "2020"
},
{
"author": "Simonnet",
"first-page": "1195",
"key": "10.1016/j.jiph.2022.12.008_bib11",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.1585",
"article-title": "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1061",
"issue": "11",
"journal-title": "JAMA",
"key": "10.1016/j.jiph.2022.12.008_bib12",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1111/all.14238",
"article-title": "Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "1730",
"issue": "7",
"journal-title": "China. Allergy",
"key": "10.1016/j.jiph.2022.12.008_bib13",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108227",
"article-title": "Association of diabetes mellitus with disease severity and prognosis in COVID-19: A retrospective cohort study",
"author": "Zhang",
"doi-asserted-by": "crossref",
"journal-title": "Diabetes Res Clin Pract",
"key": "10.1016/j.jiph.2022.12.008_bib14",
"volume": "165",
"year": "2020"
},
{
"DOI": "10.3390/jpm12050706",
"author": "Chudzik",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "J Pers Med",
"key": "10.1016/j.jiph.2022.12.008_bib15",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.3389/fendo.2020.582870",
"article-title": "Obesity, Diabetes and COVID-19: An Infectious Disease Spreading From the East Collides With the Consequences of an Unhealthy Western Lifestyle",
"author": "Holly",
"doi-asserted-by": "crossref",
"journal-title": "Front Endocrinol (Lausanne)",
"key": "10.1016/j.jiph.2022.12.008_bib16",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1007/s12015-021-10188-w",
"article-title": "Stress Decreases Host Viral Resistance and Increases Covid Susceptibility in Embryonic Stem Cells",
"author": "Abdulhasan",
"doi-asserted-by": "crossref",
"first-page": "2164",
"issue": "6",
"journal-title": "Stem Cell Rev Rep",
"key": "10.1016/j.jiph.2022.12.008_bib17",
"volume": "17",
"year": "2021"
},
{
"DOI": "10.1016/j.sleep.2020.12.041",
"article-title": "People with dyssomnia showed increased vulnerability to CoVID-19 pandemic: a questionnaire-based study exploring the patterns and predictors of sleep quality using the latent class analysis technique in Indian population",
"author": "Radhakrishnan",
"doi-asserted-by": "crossref",
"first-page": "29",
"journal-title": "Sleep Med",
"key": "10.1016/j.jiph.2022.12.008_bib18",
"volume": "79",
"year": "2021"
},
{
"DOI": "10.3389/fpsyg.2020.593903",
"article-title": "Physical Exercise and Immune System in the Elderly: Implications and Importance in COVID-19 Pandemic Period",
"author": "Scartoni",
"doi-asserted-by": "crossref",
"journal-title": "Front Psychol",
"key": "10.1016/j.jiph.2022.12.008_bib19",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1007/s40279-021-01466-1",
"article-title": "Effects of Regular Physical Activity on the Immune System, Vaccination and Risk of Community-Acquired Infectious Disease in the General Population: Systematic Review and Meta-Analysis",
"author": "Chastin",
"doi-asserted-by": "crossref",
"first-page": "1673",
"issue": "8",
"journal-title": "Sports Med",
"key": "10.1016/j.jiph.2022.12.008_bib20",
"volume": "51",
"year": "2021"
},
{
"DOI": "10.3390/ijerph18105329",
"article-title": "Post-COVID-19 Syndrome and the Potential Benefits of Exercise",
"author": "Jimeno-Almazan",
"doi-asserted-by": "crossref",
"issue": "10",
"journal-title": "Int J Environ Res Public Health",
"key": "10.1016/j.jiph.2022.12.008_bib21",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.3389/fnut.2020.597600",
"article-title": "The Impact of Obesity and Lifestyle on the Immune System and Susceptibility to Infections Such as COVID-19",
"author": "de Frel",
"doi-asserted-by": "crossref",
"journal-title": "Front Nutr",
"key": "10.1016/j.jiph.2022.12.008_bib22",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1002/ctd2.60",
"article-title": "Higher BCG-induced trained immunity prevalence predicts protection from COVID-19: Implications for ongoing BCG trials",
"author": "Singh",
"doi-asserted-by": "crossref",
"issue": "2",
"journal-title": "Clin Transl Discov",
"key": "10.1016/j.jiph.2022.12.008_bib23",
"volume": "2",
"year": "2022"
},
{
"DOI": "10.12659/MSM.936962",
"article-title": "Screening for SARS-CoV-2 Infection in Students at the Medical University of Warsaw, Poland Between November 15 and December 10, 2021 Using a Single Lateral Flow Test, the Panbio COVID-19 Ag Rapid Test",
"author": "Gujski",
"doi-asserted-by": "crossref",
"journal-title": "Med Sci Monit",
"key": "10.1016/j.jiph.2022.12.008_bib24",
"volume": "28",
"year": "2022"
},
{
"key": "10.1016/j.jiph.2022.12.008_bib25",
"unstructured": "Worldometer. Worldometer's COVID-19 Data, https://www.worldometers.info/coronavirus/country/poland; 2020 [accessed 27 September 2022]."
},
{
"DOI": "10.1093/eurheartj/ehab484",
"article-title": "ESC Guidelines on cardiovascular disease prevention in clinical practice",
"author": "Visseren",
"doi-asserted-by": "crossref",
"first-page": "3227",
"issue": "42",
"journal-title": "Eur Heart J",
"key": "10.1016/j.jiph.2022.12.008_bib26",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.3390/ijerph181910552",
"article-title": "COVID-19 and the Change in Lifestyle: Bodyweight, Time Allocation, and Food Choices",
"author": "Li",
"doi-asserted-by": "crossref",
"issue": "19",
"journal-title": "Int J Environ Res Public Health",
"key": "10.1016/j.jiph.2022.12.008_bib27",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1111/eci.13682",
"article-title": "Noncommunicable diseases, climate change and iniquities: What COVID-19 has taught us about syndemic",
"author": "Di Ciaula",
"doi-asserted-by": "crossref",
"issue": "12",
"journal-title": "Eur J Clin Invest",
"key": "10.1016/j.jiph.2022.12.008_bib28",
"volume": "51",
"year": "2021"
},
{
"DOI": "10.1155/2018/7856823",
"article-title": "The Importance of Physical Activity Exercise among Older People",
"author": "Langhammer",
"doi-asserted-by": "crossref",
"journal-title": "Biomed Res Int",
"key": "10.1016/j.jiph.2022.12.008_bib29",
"volume": "2018",
"year": "2018"
},
{
"DOI": "10.1186/s12889-021-12377-1",
"article-title": "Premature mortality attributable to COVID-19: potential years of life lost in 17 countries around the world, January-August 2020",
"author": "Ugarte",
"doi-asserted-by": "crossref",
"first-page": "54",
"issue": "1",
"journal-title": "BMC Public Health",
"key": "10.1016/j.jiph.2022.12.008_bib30",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1155/2020/8375096",
"article-title": "Stay Home: Role of Physical Exercise Training in Elderly Individuals' Ability to Face the COVID-19 Infection",
"author": "Abdelbasset",
"doi-asserted-by": "crossref",
"journal-title": "J Immunol Res",
"key": "10.1016/j.jiph.2022.12.008_bib31",
"volume": "2020",
"year": "2020"
},
{
"DOI": "10.1177/17534666211025221",
"article-title": "Does pre-existent physical inactivity have a role in the severity of COVID-19",
"author": "Yuan",
"doi-asserted-by": "crossref",
"journal-title": "Ther Adv Respir Dis",
"key": "10.1016/j.jiph.2022.12.008_bib32",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.3390/ijerph18137158",
"article-title": "A Possible Preventive Role of Physically Active Lifestyle during the SARS-CoV-2 Pandemic; Might Regular Cold-Water Swimming and Exercise Reduce the Symptom Severity of COVID-19?",
"author": "Bielik",
"doi-asserted-by": "crossref",
"issue": "13",
"journal-title": "Int J Environ Res Public Health",
"key": "10.1016/j.jiph.2022.12.008_bib33",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1016/j.bbi.2020.05.059",
"article-title": "Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK",
"author": "Hamer",
"doi-asserted-by": "crossref",
"first-page": "184",
"journal-title": "Brain Behav Immun",
"key": "10.1016/j.jiph.2022.12.008_bib34",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2021.587146",
"article-title": "The Relevance of a Physical Active Lifestyle and Physical Fitness on Immune Defense: Mitigating Disease Burden, With Focus on COVID-19 Consequences",
"author": "Filgueira",
"doi-asserted-by": "crossref",
"journal-title": "Front Immunol",
"key": "10.1016/j.jiph.2022.12.008_bib35",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2021-104080",
"article-title": "Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients",
"author": "Sallis",
"doi-asserted-by": "crossref",
"first-page": "1099",
"issue": "19",
"journal-title": "Br J Sports Med",
"key": "10.1016/j.jiph.2022.12.008_bib36",
"volume": "55",
"year": "2021"
},
{
"DOI": "10.1016/j.exger.2021.111507",
"article-title": "Aging & COVID-19 susceptibility, disease severity, and clinical outcomes: The role of entangled risk factors",
"author": "Farshbafnadi",
"doi-asserted-by": "crossref",
"journal-title": "Exp Gerontol",
"key": "10.1016/j.jiph.2022.12.008_bib37",
"volume": "154",
"year": "2021"
},
{
"DOI": "10.1016/j.bbi.2021.07.018",
"article-title": "Psychiatric and neuropsychiatric sequelae of COVID-19 - A systematic review",
"author": "Schou",
"doi-asserted-by": "crossref",
"first-page": "328",
"journal-title": "Brain Behav Immun",
"key": "10.1016/j.jiph.2022.12.008_bib38",
"volume": "97",
"year": "2021"
},
{
"DOI": "10.1093/abm/kaab106",
"article-title": "Psychological Predictors of Self-reported COVID-19 Outcomes: Results From a Prospective Cohort Study",
"author": "Ayling",
"doi-asserted-by": "crossref",
"first-page": "484",
"issue": "5",
"journal-title": "Ann Behav Med",
"key": "10.1016/j.jiph.2022.12.008_bib39",
"volume": "56",
"year": "2022"
},
{
"DOI": "10.1186/s11556-022-00287-z",
"article-title": "Factors associated with physical activity reduction in Swedish older adults during the first COVID-19 outbreak: a longitudinal population-based study",
"author": "Sjoberg",
"doi-asserted-by": "crossref",
"first-page": "9",
"issue": "1",
"journal-title": "Eur Rev Aging Phys Act",
"key": "10.1016/j.jiph.2022.12.008_bib40",
"volume": "19",
"year": "2022"
},
{
"DOI": "10.1016/j.janxdis.2022.102535",
"article-title": "COVID stress in older adults: Considerations during the Omicron wave and beyond",
"author": "Hadjistavropoulos",
"doi-asserted-by": "crossref",
"journal-title": "J Anxiety Disord",
"key": "10.1016/j.jiph.2022.12.008_bib41",
"volume": "86",
"year": "2022"
},
{
"DOI": "10.1007/s12035-020-02249-x",
"article-title": "Impact of COVID-19 in the Mental Health in Elderly: Psychological and Biological Updates",
"author": "Grolli",
"doi-asserted-by": "crossref",
"first-page": "1905",
"issue": "5",
"journal-title": "Mol Neurobiol",
"key": "10.1016/j.jiph.2022.12.008_bib42",
"volume": "58",
"year": "2021"
},
{
"DOI": "10.1093/cvr/cvab298",
"author": "Cenko",
"doi-asserted-by": "crossref",
"first-page": "2705",
"issue": "14",
"journal-title": "Cardiovasc Res",
"key": "10.1016/j.jiph.2022.12.008_bib43",
"volume": "117",
"year": "2021"
},
{
"DOI": "10.1001/jamacardio.2020.1286",
"article-title": "Potential Effects of Coronaviruses on the Cardiovascular System: A Review",
"author": "Madjid",
"doi-asserted-by": "crossref",
"first-page": "831",
"issue": "7",
"journal-title": "JAMA Cardiol",
"key": "10.1016/j.jiph.2022.12.008_bib44",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.046941",
"article-title": "COVID-19 and Cardiovascular Disease",
"author": "Clerkin",
"doi-asserted-by": "crossref",
"first-page": "1648",
"issue": "20",
"journal-title": "Circulation",
"key": "10.1016/j.jiph.2022.12.008_bib45",
"volume": "141",
"year": "2020"
},
{
"DOI": "10.46234/ccdcw2020.032",
"doi-asserted-by": "crossref",
"key": "10.1016/j.jiph.2022.12.008_bib46",
"unstructured": "The Novel Coronavirus Pneumonia Emergency Response Epidemiology T. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) - China, 2020. China CDC Wkly. 2020;2(8):113-22."
},
{
"DOI": "10.1136/heartjnl-2020-317062",
"article-title": "Impact of cardiovascular disease and cardiac injury on in-hospital mortality in patients with COVID-19: a systematic review and meta-analysis",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "1142",
"issue": "15",
"journal-title": "Heart",
"key": "10.1016/j.jiph.2022.12.008_bib47",
"volume": "106",
"year": "2020"
},
{
"DOI": "10.1001/jamacardio.2020.0934",
"article-title": "An Acute Respiratory Infection Runs Into the Most Common Noncommunicable Epidemic-COVID-19 and Cardiovascular Diseases",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "743",
"issue": "7",
"journal-title": "JAMA Cardiol",
"key": "10.1016/j.jiph.2022.12.008_bib48",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.04.035",
"article-title": "SARS-CoV-2 Receptor ACE2 Is an Interferon-Stimulated Gene in Human Airway Epithelial Cells and Is Detected in Specific Cell Subsets across Tissues",
"author": "Ziegler",
"doi-asserted-by": "crossref",
"first-page": "1016",
"issue": "5",
"journal-title": "Cell",
"key": "10.1016/j.jiph.2022.12.008_bib49",
"volume": "181",
"year": "2020"
},
{
"article-title": "Thrombosis and Coagulopathy in COVID-19: Current Understanding and Implications for Antithrombotic Treatment in Patients Treated With Percutaneous Coronary Intervention",
"author": "Liu",
"journal-title": "Front Cardiovasc Med",
"key": "10.1016/j.jiph.2022.12.008_bib50",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2020.03.031",
"article-title": "Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic",
"author": "Driggin",
"doi-asserted-by": "crossref",
"first-page": "2352",
"issue": "18",
"journal-title": "J Am Coll Cardiol",
"key": "10.1016/j.jiph.2022.12.008_bib51",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1016/S1473-3099(09)70331-7",
"article-title": "Role of acute infection in triggering acute coronary syndromes",
"author": "Corrales-Medina",
"doi-asserted-by": "crossref",
"first-page": "83",
"issue": "2",
"journal-title": "Lancet Infect Dis",
"key": "10.1016/j.jiph.2022.12.008_bib52",
"volume": "10",
"year": "2010"
},
{
"DOI": "10.1007/s00134-020-05993-9",
"article-title": "How to balance acute myocardial infarction and COVID-19: the protocols from Sichuan Provincial People's Hospital",
"author": "Zeng",
"doi-asserted-by": "crossref",
"first-page": "1111",
"issue": "6",
"journal-title": "Intensive Care Med",
"key": "10.1016/j.jiph.2022.12.008_bib53",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "1054",
"issue": "10229",
"journal-title": "Lancet.",
"key": "10.1016/j.jiph.2022.12.008_bib54",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.archger.2022.104628",
"article-title": "Long-term cardiovascular adverse events in very elderly COVID-19 patients",
"author": "Karadavut",
"doi-asserted-by": "crossref",
"journal-title": "Arch Gerontol Geriatr",
"key": "10.1016/j.jiph.2022.12.008_bib55",
"volume": "100",
"year": "2022"
},
{
"DOI": "10.1016/j.amsu.2020.07.054",
"article-title": "Cardiovascular involvement during COVID-19 and clinical implications in elderly patients. A review",
"author": "Napoli",
"doi-asserted-by": "crossref",
"first-page": "236",
"journal-title": "Ann Med Surg (Lond)",
"key": "10.1016/j.jiph.2022.12.008_bib56",
"volume": "57",
"year": "2020"
},
{
"DOI": "10.1016/j.eclinm.2021.100789",
"article-title": "COPD and the risk of poor outcomes in COVID-19: A systematic review and meta-analysis",
"author": "Gerayeli",
"doi-asserted-by": "crossref",
"journal-title": "EClinicalMedicine",
"key": "10.1016/j.jiph.2022.12.008_bib57",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.1183/16000617.0199-2020",
"article-title": "COVID-19 and COPD: a narrative review of the basic science and clinical outcomes",
"author": "Higham",
"doi-asserted-by": "crossref",
"issue": "158",
"journal-title": "Eur Respir Rev",
"key": "10.1016/j.jiph.2022.12.008_bib58",
"volume": "29",
"year": "2020"
},
{
"DOI": "10.1016/j.rmed.2020.105941",
"article-title": "Chronic obstructive pulmonary disease is associated with severe coronavirus disease 2019 (COVID-19)",
"author": "Lippi",
"doi-asserted-by": "crossref",
"journal-title": "Respir Med",
"key": "10.1016/j.jiph.2022.12.008_bib59",
"volume": "167",
"year": "2020"
},
{
"DOI": "10.1183/13993003.00688-2020",
"article-title": "ACE-2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19",
"author": "Leung",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "Eur Respir J",
"key": "10.1016/j.jiph.2022.12.008_bib60",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30224-1",
"article-title": "SARS-CoV-2 receptor ACE2 gene expression and RAAS inhibitors",
"author": "Milne",
"doi-asserted-by": "crossref",
"first-page": "e50",
"issue": "6",
"journal-title": "Lancet Respir Med",
"key": "10.1016/j.jiph.2022.12.008_bib61",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1164/rccm.201006-0833OC",
"article-title": "Experimental rhinovirus infection as a human model of chronic obstructive pulmonary disease exacerbation",
"author": "Mallia",
"doi-asserted-by": "crossref",
"first-page": "734",
"issue": "6",
"journal-title": "Am J Respir Crit Care Med",
"key": "10.1016/j.jiph.2022.12.008_bib62",
"volume": "183",
"year": "2011"
},
{
"DOI": "10.1126/sciimmunol.abd1554",
"article-title": "Immunophenotyping of COVID-19 and influenza highlights the role of type I interferons in development of severe COVID-19",
"author": "Lee",
"doi-asserted-by": "crossref",
"issue": "49",
"journal-title": "Sci Immunol",
"key": "10.1016/j.jiph.2022.12.008_bib63",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.07.005",
"article-title": "Association of hypertension, diabetes, stroke, cancer, kidney disease, and high-cholesterol with COVID-19 disease severity and fatality: A systematic review",
"author": "Zaki",
"doi-asserted-by": "crossref",
"first-page": "1133",
"issue": "5",
"journal-title": "Diabetes Metab Syndr",
"key": "10.1016/j.jiph.2022.12.008_bib64",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.chest.2021.07.1626",
"article-title": "Clinical Condition and Symptoms of Patients with Copd with Sars-Cov-2 Infection",
"author": "Betancourt-PeñA",
"doi-asserted-by": "crossref",
"issue": "4",
"journal-title": "Chest",
"key": "10.1016/j.jiph.2022.12.008_bib65",
"volume": "160",
"year": "2021"
},
{
"DOI": "10.1136/bmjnph-2021-000228",
"article-title": "COVID-19 illness in relation to sleep and burnout",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "132",
"issue": "1",
"journal-title": "BMJ Nutr Prev Health",
"key": "10.1016/j.jiph.2022.12.008_bib66",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1016/j.sleep.2021.01.034",
"article-title": "Relationship between sleep quality and the psychological status of patients hospitalised with COVID-19",
"author": "Akinci",
"doi-asserted-by": "crossref",
"first-page": "167",
"journal-title": "Sleep Med",
"key": "10.1016/j.jiph.2022.12.008_bib67",
"volume": "80",
"year": "2021"
},
{
"DOI": "10.3390/jpm11111203",
"article-title": "Sleep Dysfunction in COVID-19 Patients: Prevalence, Risk Factors, Mechanisms, and Management",
"author": "Pataka",
"doi-asserted-by": "crossref",
"issue": "11",
"journal-title": "J Pers Med",
"key": "10.1016/j.jiph.2022.12.008_bib68",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.sleep.2021.07.021",
"article-title": "Sleep disorders and COVID-19",
"author": "Bhat",
"doi-asserted-by": "crossref",
"first-page": "253",
"journal-title": "Sleep Med",
"key": "10.1016/j.jiph.2022.12.008_bib69",
"volume": "91",
"year": "2022"
},
{
"DOI": "10.1016/j.bbi.2020.05.075",
"article-title": "Poor-sleep is associated with slow recovery from lymphopenia and an increased need for ICU care in hospitalized patients with COVID-19: A retrospective cohort study",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "50",
"journal-title": "Brain Behav Immun",
"key": "10.1016/j.jiph.2022.12.008_bib70",
"volume": "88",
"year": "2020"
},
{
"DOI": "10.1155/2015/678164",
"article-title": "The Bidirectional Relationship between Sleep and Immunity against Infections",
"author": "Ibarra-Coronado",
"doi-asserted-by": "crossref",
"journal-title": "J Immunol Res",
"key": "10.1016/j.jiph.2022.12.008_bib71",
"volume": "2015",
"year": "2015"
},
{
"DOI": "10.1089/jwh.2021.0411",
"article-title": "Sex-Related Differences in Long-COVID-19 Syndrome",
"author": "Pela",
"doi-asserted-by": "crossref",
"first-page": "620",
"issue": "5",
"journal-title": "J Womens Health (Larchmt)",
"key": "10.1016/j.jiph.2022.12.008_bib72",
"volume": "31",
"year": "2022"
},
{
"DOI": "10.3390/jcm11020413",
"article-title": "Female Sex Is a Risk Factor Associated with Long-Term Post-COVID Related-Symptoms but Not with COVID-19 Symptoms: The LONG-COVID-EXP-CM Multicenter Study",
"author": "Fernandez-de-Las-Penas",
"doi-asserted-by": "crossref",
"issue": "2",
"journal-title": "J Clin Med",
"key": "10.1016/j.jiph.2022.12.008_bib73",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1080/03007995.2022.2081454",
"article-title": "Sex differences in sequelae from COVID-19 infection and in long COVID syndrome: a review",
"author": "Sylvester",
"doi-asserted-by": "crossref",
"first-page": "1391",
"issue": "8",
"journal-title": "Curr Med Res Opin",
"key": "10.1016/j.jiph.2022.12.008_bib74",
"volume": "38",
"year": "2022"
},
{
"DOI": "10.1038/nri.2016.90",
"article-title": "Sex differences in immune responses",
"author": "Klein",
"doi-asserted-by": "crossref",
"first-page": "626",
"issue": "10",
"journal-title": "Nat Rev Immunol",
"key": "10.1016/j.jiph.2022.12.008_bib75",
"volume": "16",
"year": "2016"
},
{
"DOI": "10.1016/j.jaccas.2020.04.027",
"article-title": "Sex Differences in Mortality From COVID-19 Pandemic: Are Men Vulnerable and Women Protected?",
"author": "Sharma",
"doi-asserted-by": "crossref",
"first-page": "1407",
"issue": "9",
"journal-title": "JACC Case Rep",
"key": "10.1016/j.jiph.2022.12.008_bib76",
"volume": "2",
"year": "2020"
},
{
"article-title": "Long COVID risk - a signal to address sex hormones and women's health",
"author": "Stewart",
"journal-title": "Lancet Reg Health Eur",
"key": "10.1016/j.jiph.2022.12.008_bib77",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0243882",
"article-title": "Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection",
"author": "Jacobs",
"doi-asserted-by": "crossref",
"issue": "12",
"journal-title": "PLoS One",
"key": "10.1016/j.jiph.2022.12.008_bib78",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0268119",
"article-title": "The influence of gender on COVID-19 infections and mortality in Germany: Insights from age- and gender-specific modeling of contact rates, infections, and deaths in the early phase of the pandemic",
"author": "Doerre",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "PLoS One",
"key": "10.1016/j.jiph.2022.12.008_bib79",
"volume": "17",
"year": "2022"
},
{
"article-title": "Clinical Symptom Differences Between Mild and Severe COVID-19 Patients in China: A Meta-Analysis",
"author": "He",
"journal-title": "Front Public Health",
"key": "10.1016/j.jiph.2022.12.008_bib80",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm6930e1",
"article-title": "Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network - United States, March-June 2020",
"author": "Tenforde",
"doi-asserted-by": "crossref",
"first-page": "993",
"issue": "30",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "10.1016/j.jiph.2022.12.008_bib81",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/j.ajic.2021.10.039",
"article-title": "Clinical characteristics and symptom duration among outpatients with COVID-19",
"author": "Lane",
"doi-asserted-by": "crossref",
"first-page": "383",
"issue": "4",
"journal-title": "Am J Infect Control",
"key": "10.1016/j.jiph.2022.12.008_bib82",
"volume": "50",
"year": "2022"
},
{
"DOI": "10.1002/hsr2.657",
"article-title": "COVID-19 mortality and its predictors in the elderly: A systematic review",
"author": "Dadras",
"doi-asserted-by": "crossref",
"issue": "3",
"journal-title": "Health Sci Rep",
"key": "10.1016/j.jiph.2022.12.008_bib83",
"volume": "5",
"year": "2022"
},
{
"DOI": "10.1016/S2214-109X(22)00114-0",
"article-title": "Clinical severity of COVIbD-19 in patients admitted to hospital during the omicron wave in South Africa: a retrospective observational study",
"author": "Jassat",
"doi-asserted-by": "crossref",
"first-page": "e961",
"issue": "7",
"journal-title": "Lancet Glob Health",
"key": "10.1016/j.jiph.2022.12.008_bib84",
"volume": "10",
"year": "2022"
},
{
"article-title": "Clinical characteristics of the first three waves of hospitalised patients with COVID-19 in Japan prior to the widespread use of vaccination: a nationwide observational study",
"author": "Matsunaga",
"journal-title": "Lancet Reg Health West Pac",
"key": "10.1016/j.jiph.2022.12.008_bib85",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2107058",
"article-title": "Prevention and Attenuation of Covid-19 with the BNT162b2 and mRNA-1273 Vaccines",
"author": "Thompson",
"doi-asserted-by": "crossref",
"first-page": "320",
"issue": "4",
"journal-title": "N Engl J Med",
"key": "10.1016/j.jiph.2022.12.008_bib86",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0263014",
"article-title": "Lower probability and shorter duration of infections after COVID-19 vaccine correlate with anti-SARS-CoV-2 circulating IgGs",
"author": "Ronchini",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "PLoS One",
"key": "10.1016/j.jiph.2022.12.008_bib87",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.21203/rs.3.rs-1489822/v1",
"doi-asserted-by": "crossref",
"key": "10.1016/j.jiph.2022.12.008_bib88",
"unstructured": "Baum U., Poukka E., Leino T., Kilpi T., Nohynek H., Palmu A.A. High vaccine effectiveness against severe Covid-19 in the elderly in Finland before and after the emergence of Omicron (preprint). 2022. https://doi.org/10.1101/2022.03.11.22272140."
},
{
"article-title": "Antibiotics for the treatment of COVID-19",
"author": "Popp",
"journal-title": "Cochrane Database Syst Rev",
"key": "10.1016/j.jiph.2022.12.008_bib89",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1186/s12879-022-07068-0",
"article-title": "Efficacy of antiviral therapies for COVID-19: a systematic review of randomized controlled trials",
"author": "Vegivinti",
"doi-asserted-by": "crossref",
"first-page": "107",
"issue": "1",
"journal-title": "BMC Infect Dis",
"key": "10.1016/j.jiph.2022.12.008_bib90",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1007/s43440-021-00231-5",
"article-title": "Amantadine in the prevention of clinical symptoms caused by SARS-CoV-2",
"author": "Cortes-Borra",
"doi-asserted-by": "crossref",
"first-page": "962",
"issue": "3",
"journal-title": "Pharmacol Rep",
"key": "10.1016/j.jiph.2022.12.008_bib91",
"volume": "73",
"year": "2021"
},
{
"article-title": "Ivermectin for preventing and treating COVID-19",
"author": "Popp",
"journal-title": "Cochrane Database Syst Rev",
"key": "10.1016/j.jiph.2022.12.008_bib92",
"volume": "7",
"year": "2021"
}
],
"reference-count": 92,
"references-count": 92,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S1876034122003495"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Public Health, Environmental and Occupational Health",
"General Medicine"
],
"subtitle": [],
"title": "Do selected lifestyle parameters affect the severity and symptoms of COVID-19 among elderly patients? The retrospective evaluation of individuals from the STOP-COVID registry of the PoLoCOV study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy"
}
