COVID-19 illness in relation to sleep and burnout
et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000228, Mar 2021
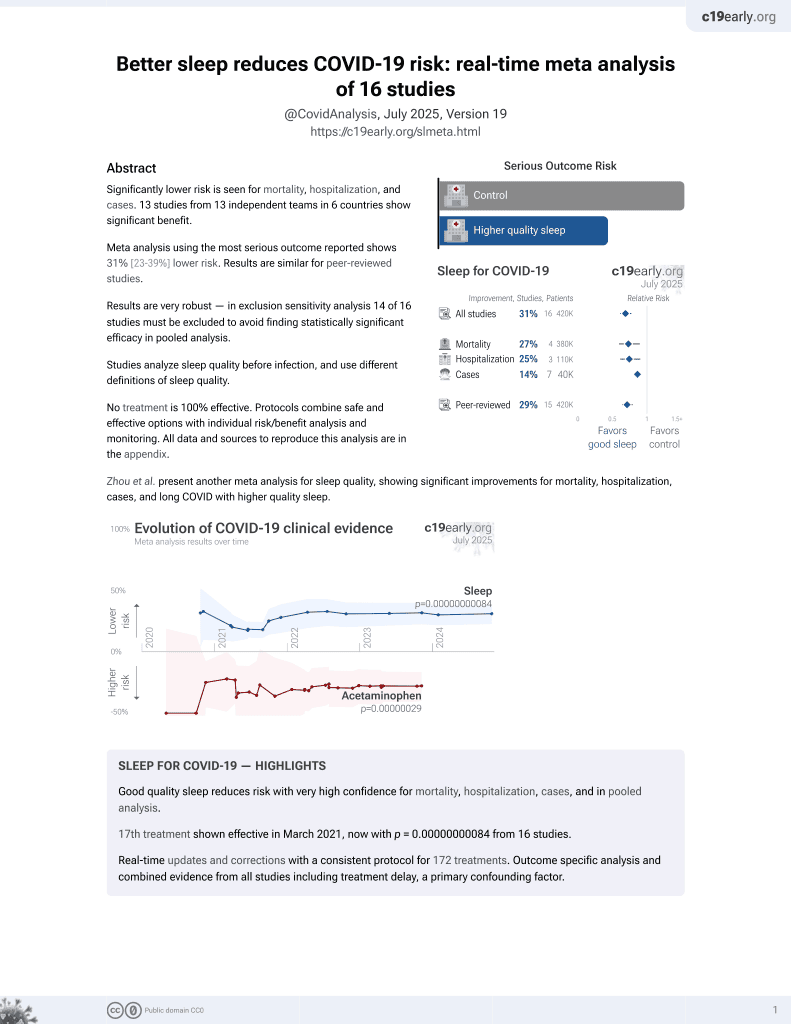
Sleep for COVID-19
18th treatment shown to reduce risk in
March 2021, now with p = 0.00000000084 from 16 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 2,884 high-risk healthcare workers in France, Germany, Italy, Spain, UK, and the USA, showing shorter sleep duration associated with increased risk of COVID-19 cases and severity.
|
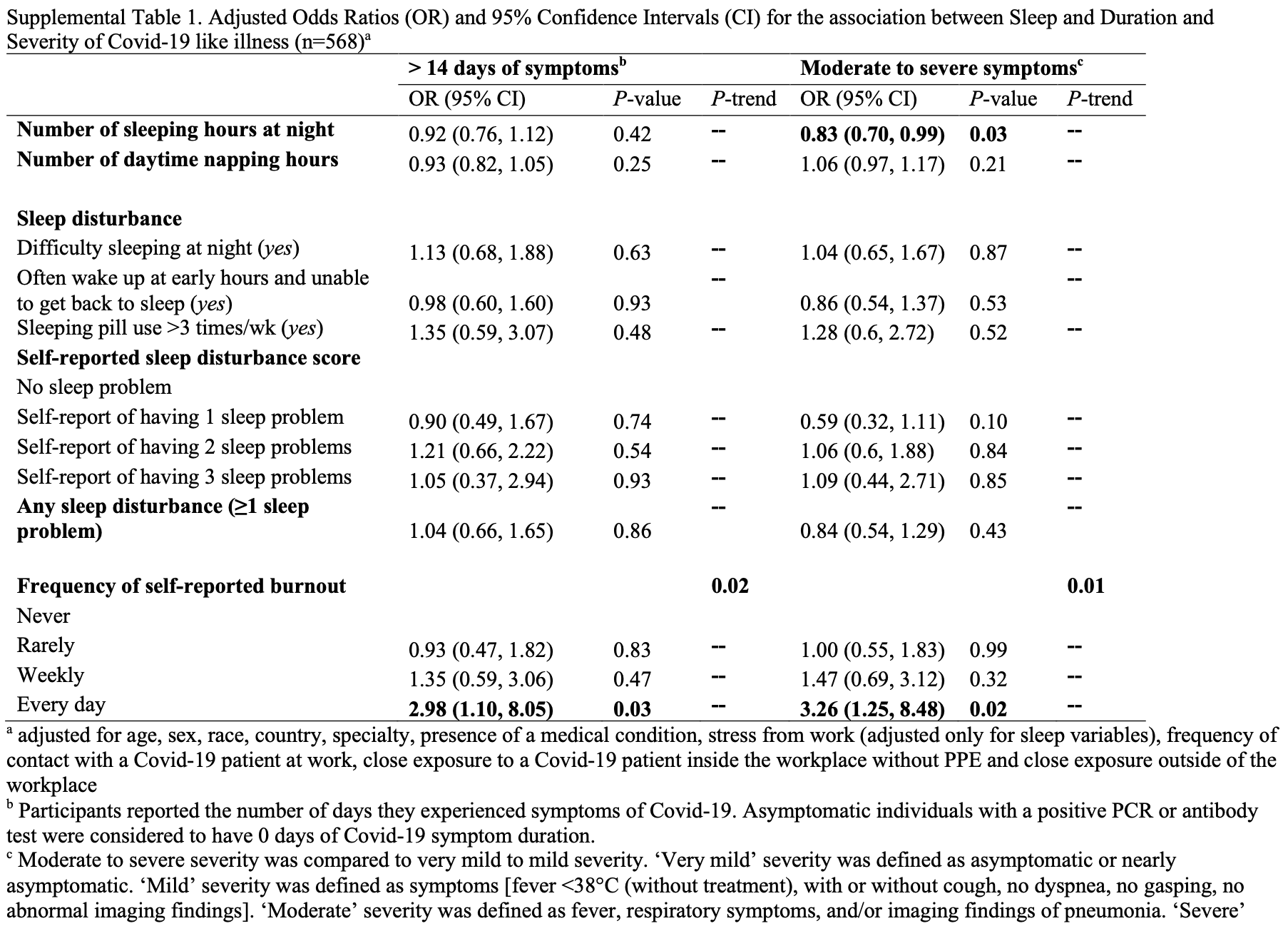
risk of moderate/severe case, 17.0% lower, OR 0.83, p = 0.03, per extra hour of sleep, RR approximated with OR.
|
|
risk of case, 11.0% lower, OR 0.89, p = 0.003, per extra hour of sleep, model 3, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Kim et al., 22 Mar 2021, retrospective, multiple countries, peer-reviewed, survey, mean age 48.0, 8 authors, study period 17 July, 2020 - 25 September, 2020.
Contact: smb88@caa.columbia.edu.
COVID-19 illness in relation to sleep and burnout
BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000228
Background Sleep habits and burnout have been shown to be associated with increase in infectious diseases, but it is unknown if these factors are associated with risk of COVID-19. We assessed whether sleep and self-reported burnout may be risk factors for COVID-19 among high-risk healthcare workers (HCWs). Methods From 17 July to 25 September 2020, a webbased survey was administered to HCWs in six countries (France, Germany, Italy, Spain, UK, USA) with a high frequency of workplace exposure. Participants provided information on demographics, sleep (number of sleep hours at night, daytime napping hours, sleep problems), burnout from work and COVID-19 exposures. We used multivariable linear and logistic regression models to evaluate the associations between sleep, burnout and COVID-19. Results Among 2884 exposed HCWs, there were 568 COVID-19 cases and 2316 controls. After adjusting for confounders, 1-hour longer sleep duration at night was associated with 12% lower odds of COVID-19 (p=0.003). Daytime napping hours was associated with 6% higher odds, but the association varied by countries, with a nonsignificant inverse association in Spain. Compared with having no sleep problems, having three sleep problems was associated with 88% greater odds of COVID-19. Reporting burnout 'every day' was associated with greater odds of COVID-19 (OR: 2.60, 95% CI 1.57 to 4.31, p trend across categories=0.001), longer duration (OR: 2.98, 95% CI 1.10 to 8.05, p trend=0.02) and severity (OR: 3.26, 95% CI 1.25 to 8.48, p trend=0.02) compared with reporting no burnout. These associations remained significant after adjusting for frequency of COVID-19 exposures. Conclusions In six countries, longer sleep duration was associated with lower odds of COVID-19, but the association with daytime nap may not be consistent across countries. Greater sleep problems and high level of burnout were robustly associated with greater odds of COVID-19. Sleep and burnout may be risk factors for COVID-19 in high-risk HCWs.
Competing interests None declared. Patient consent for publication Not required.
Ethics approval The Western IRB at Stamford Hospital reviewed the study protocol and determined the study to be exempt. Provenance and peer review Not commissioned; externally peer reviewed. Data availability statement Data are not publicly available. Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise. To explore this further, they drew on the responses to an online survey for healthcare workers repeatedly exposed to patients with COVID-19 infection, such as those working in emergency or intensive care, and so at heightened risk of becoming infected themselves. The survey ran from 17 July to 25 September 2020, and was open to healthcare workers in France, Germany, Italy, Spain, the UK, and the USA. Respondents provided personal details on..
References
Ahola, Väänänen, Koskinen, Burnout as a predictor of allcause mortality among industrial employees: a 10-year prospective register-linkage study, J Psychosom Res, doi:10.1016/j.jpsychores.2010.01.002
Campos, Siles, Siesta and the risk of coronary heart disease: results from a population-based, case-control study in Costa Rica, Int J Epidemiol, doi:10.1093/ije/29.3.429
Cohen, Doyle, Alper, Sleep habits and susceptibility to the common cold, Arch Intern Med, doi:10.1001/archinternmed.2008.505
Dupont, Power calculations for matched case-control studies, Biometrics, doi:10.2307/2531743
Dyrbye, West, Satele, among U.S. medical students, residents, and early career physicians relative to the general U.S. population, Acad Med, doi:10.1097/ACM.0000000000000134
Honkonen, Ahola, Pertovaara, The association between burnout and physical illness in the general population--results from the Finnish Health 2000 Study, J Psychosom Res, doi:10.1016/j.jpsychores.2005.10.002
Huang, Niu, Zhao, Reduced sleep in the week prior to diagnosis of COVID-19 is associated with the severity of COVID-19, Nat Sci Sleep, doi:10.2147/NSS.S263488
Ingelsson, Lind, Arnlöv, Sleep disturbances independently predict heart failure in overweight middle-aged men, Eur J Heart Fail, doi:10.1016/j.ejheart.2006.05.012
Kim, Hegde, Lafiura, Access to personal protective equipment in exposed healthcare workers and COVID-19 illness, severity, symptoms and duration: a population-based case-control study in six countries, BMJ Glob Health, doi:10.1136/bmjgh-2020-004611
Lh, Graham, Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study, Lancet Public Health, doi:10.1016/S2468-2667(20)30164-X
Melamed, Shirom, Toker, Burnout and risk of type 2 diabetes: a prospective study of apparently healthy employed persons, Psychosom Med, doi:10.1097/01.psy.0000242860.24009.f0
Mohren, Swaen, Kant, Common infections and the role of burnout in a Dutch working population, J Psychosom Res, doi:10.1016/S0022-3999(02)00517-2
Patel, Malhotra, Gao, A prospective study of sleep duration and pneumonia risk in women, Sleep, doi:10.5665/sleep.1594
Prather, Janicki-Deverts, Hall, Behaviorally assessed sleep and susceptibility to the common cold, Sleep, doi:10.5665/sleep.4968
Prather, Leung, Association of insufficient sleep with respiratory infection among adults in the United States, JAMA Intern Med, doi:10.1001/jamainternmed.2016.0787
Sasangohar, Jones, Masud, Provider burnout and fatigue during the COVID-19 pandemic: lessons learned from a highvolume intensive care unit, Anesth Analg, doi:10.1213/ANE.0000000000004866
Shah, Wood, Gribben, Risk of hospital admission with coronavirus disease 2019 in healthcare workers and their households: nationwide linkage cohort study, BMJ, doi:10.1136/bmj.m3582
Toppinen-Tanner, Ojajärvi, Väänänen, Burnout as a predictor of medically certified sick-leave absences and their diagnosed causes, Behav Med, doi:10.3200/BMED.31.1.18-32
Van Egmond, Moulin, Schiöth, Meal timing and subjective sleep disturbances in older men, Exp Gerontol, doi:10.1016/j.exger.2020.111089
West, Dyrbye, Sloan, Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals, J Gen Intern Med, doi:10.1007/s11606-009-1129-z
Worldometer, Coronavirus graphs: worldwide cases and deaths
DOI record:
{
"DOI": "10.1136/bmjnph-2021-000228",
"ISSN": [
"2516-5542"
],
"URL": "http://dx.doi.org/10.1136/bmjnph-2021-000228",
"abstract": "<jats:sec><jats:title>Background</jats:title><jats:p>Sleep habits and burnout have been shown to be associated with increase in infectious diseases, but it is unknown if these factors are associated with risk of COVID-19. We assessed whether sleep and self-reported burnout may be risk factors for COVID-19 among high-risk healthcare workers (HCWs).</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>From 17 July to 25 September 2020, a web-based survey was administered to HCWs in six countries (France, Germany, Italy, Spain, UK, USA) with a high frequency of workplace exposure. Participants provided information on demographics, sleep (number of sleep hours at night, daytime napping hours, sleep problems), burnout from work and COVID-19 exposures. We used multivariable linear and logistic regression models to evaluate the associations between sleep, burnout and COVID-19.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Among 2884 exposed HCWs, there were 568 COVID-19 cases and 2316 controls. After adjusting for confounders, 1-hour longer sleep duration at night was associated with 12% lower odds of COVID-19 (p=0.003). Daytime napping hours was associated with 6% higher odds, but the association varied by countries, with a non-significant inverse association in Spain. Compared with having no sleep problems, having three sleep problems was associated with 88% greater odds of COVID-19. Reporting burnout ‘every day’ was associated with greater odds of COVID-19 (OR: 2.60, 95% CI 1.57 to 4.31, p trend across categories=0.001), longer duration (OR: 2.98, 95% CI 1.10 to 8.05, p trend=0.02) and severity (OR: 3.26, 95% CI 1.25 to 8.48, p trend=0.02) compared with reporting no burnout. These associations remained significant after adjusting for frequency of COVID-19 exposures.</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>In six countries, longer sleep duration was associated with lower odds of COVID-19, but the association with daytime nap may not be consistent across countries. Greater sleep problems and high level of burnout were robustly associated with greater odds of COVID-19. Sleep and burnout may be risk factors for COVID-19 in high-risk HCWs.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjnph-2021-000228"
],
"author": [
{
"affiliation": [],
"family": "Kim",
"given": "Hyunju",
"sequence": "first"
},
{
"affiliation": [],
"family": "Hegde",
"given": "Sheila",
"sequence": "additional"
},
{
"affiliation": [],
"family": "LaFiura",
"given": "Christine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Raghavan",
"given": "Madhunika",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Luong",
"given": "Eric",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cheng",
"given": "Susan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rebholz",
"given": "Casey M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Seidelmann",
"given": "Sara B",
"sequence": "additional"
}
],
"container-title": "BMJ Nutrition, Prevention & Health",
"container-title-short": "BMJNPH",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
3,
22
]
],
"date-time": "2021-03-22T22:50:12Z",
"timestamp": 1616453412000
},
"deposited": {
"date-parts": [
[
2021,
7,
27
]
],
"date-time": "2021-07-27T21:07:52Z",
"timestamp": 1627420072000
},
"funder": [
{
"DOI": "10.13039/100000062",
"award": [
"K01 DK107782"
],
"doi-asserted-by": "publisher",
"name": "National Institute of Diabetes and Digestive and Kidney Diseases"
},
{
"DOI": "10.13039/100000002",
"award": [
"U54CA260591"
],
"doi-asserted-by": "publisher",
"name": "National Institutes of Health"
},
{
"DOI": "10.13039/100000050",
"award": [
"R21 HL143089",
"R56 HL153178"
],
"doi-asserted-by": "publisher",
"name": "National Heart, Lung, and Blood Institute"
}
],
"indexed": {
"date-parts": [
[
2022,
4,
19
]
],
"date-time": "2022-04-19T23:28:09Z",
"timestamp": 1650410889719
},
"is-referenced-by-count": 15,
"issue": "1",
"issued": {
"date-parts": [
[
2021,
3,
22
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2021,
6,
30
]
]
},
"published-print": {
"date-parts": [
[
2021,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
3,
22
]
],
"date-time": "2021-03-22T00:00:00Z",
"timestamp": 1616371200000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjnph-2021-000228",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "132-139",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
3,
22
]
]
},
"published-online": {
"date-parts": [
[
2021,
3,
22
]
]
},
"published-print": {
"date-parts": [
[
2021,
6
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1016/S2468-2667(20)30164-X",
"article-title": "Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study",
"author": "Nguyen",
"doi-asserted-by": "crossref",
"first-page": "e475",
"journal-title": "Lancet Public Health",
"key": "2021072714060116000_4.1.132.1",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m3582",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.2"
},
{
"DOI": "10.5665/sleep.4968",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.3"
},
{
"DOI": "10.1016/S0022-3999(02)00517-2",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.4"
},
{
"DOI": "10.2147/NSS.S263488",
"article-title": "Reduced sleep in the week prior to diagnosis of COVID-19 is associated with the severity of COVID-19",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "999",
"journal-title": "Nat Sci Sleep",
"key": "2021072714060116000_4.1.132.5",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.2307/2531743",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.6"
},
{
"DOI": "10.1136/bmjgh-2020-004611",
"article-title": "Access to personal protective equipment in exposed healthcare workers and COVID-19 illness, severity, symptoms and duration: a population-based case-control study in six countries",
"author": "Kim",
"doi-asserted-by": "crossref",
"journal-title": "BMJ Glob Health",
"key": "2021072714060116000_4.1.132.7",
"volume": "6",
"year": "2021"
},
{
"key": "2021072714060116000_4.1.132.8",
"unstructured": "Worldometer . Coronavirus graphs: worldwide cases and deaths. Available: https://www.worldometers.info/coronavirus/worldwide-graphs/ [Accessed 21 Jan 2021]."
},
{
"DOI": "10.1016/j.ejheart.2006.05.012",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.9"
},
{
"DOI": "10.1016/j.exger.2020.111089",
"article-title": "Meal timing and subjective sleep disturbances in older men",
"author": "van Egmond",
"doi-asserted-by": "crossref",
"journal-title": "Exp Gerontol",
"key": "2021072714060116000_4.1.132.10",
"volume": "141",
"year": "2020"
},
{
"DOI": "10.1007/s11606-009-1129-z",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.11"
},
{
"DOI": "10.1097/ACM.0000000000000134",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.12"
},
{
"key": "2021072714060116000_4.1.132.13",
"unstructured": "American Sleep Association . COVID-19 and sleep, 2020. Available: https://www.sleepassociation.org/about-sleep/covid-19-and-sleep/ [Accessed 27 Nov 2020]."
},
{
"key": "2021072714060116000_4.1.132.14",
"unstructured": "Centers for Disease Control and Prevention . Obesity, Race/Ethnicity, and COVID-19, 2020. Available: http://www.cdc.gov/obesity/data/obesity-and-covid-19.html [Accessed 27 Nov 2020]."
},
{
"DOI": "10.1001/archinternmed.2008.505",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.15"
},
{
"DOI": "10.5665/sleep.1594",
"article-title": "A prospective study of sleep duration and pneumonia risk in women",
"author": "Patel",
"doi-asserted-by": "crossref",
"first-page": "97",
"journal-title": "Sleep",
"key": "2021072714060116000_4.1.132.16",
"volume": "35",
"year": "2012"
},
{
"DOI": "10.1001/jamainternmed.2016.0787",
"article-title": "Association of insufficient sleep with respiratory infection among adults in the United States",
"author": "Prather",
"doi-asserted-by": "crossref",
"first-page": "850",
"journal-title": "JAMA Intern Med",
"key": "2021072714060116000_4.1.132.17",
"volume": "176",
"year": "2016"
},
{
"DOI": "10.1097/01.psy.0000242860.24009.f0",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.18"
},
{
"DOI": "10.1016/j.jpsychores.2005.10.002",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.19"
},
{
"DOI": "10.1016/j.jpsychores.2010.01.002",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.20"
},
{
"DOI": "10.3200/BMED.31.1.18-32",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.21"
},
{
"DOI": "10.1213/ANE.0000000000004866",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.22"
},
{
"DOI": "10.1093/ije/29.3.429",
"doi-asserted-by": "publisher",
"key": "2021072714060116000_4.1.132.23"
}
],
"reference-count": 23,
"references-count": 23,
"relation": {},
"resource": {
"primary": {
"URL": "https://nutrition.bmj.com/lookup/doi/10.1136/bmjnph-2021-000228"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Nutrition and Dietetics",
"Medicine (miscellaneous)",
"Health (social science)"
],
"subtitle": [],
"title": "COVID-19 illness in relation to sleep and burnout",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "4"
}