Inadequate Physical Activity Is Associated with Worse Physical Function in a Sample of COVID-19 Survivors with Post-Acute Symptoms
et al., Journal of Clinical Medicine, doi:10.3390/jcm12072517, Mar 2023
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 1,846 post-acute COVID-19 patients in Italy, showing inadequate physical activity after recovering from COVID-19 associated with lower physical function.
Galluzzo et al., 27 Mar 2023, Italy, peer-reviewed, 12 authors, study period 21 April, 2020 - 31 December, 2021.
Contact: v91galluzzo@gmail.com (corresponding author).
Inadequate Physical Activity Is Associated with Worse Physical Function in a Sample of COVID-19 Survivors with Post-Acute Symptoms
Journal of Clinical Medicine, doi:10.3390/jcm12072517
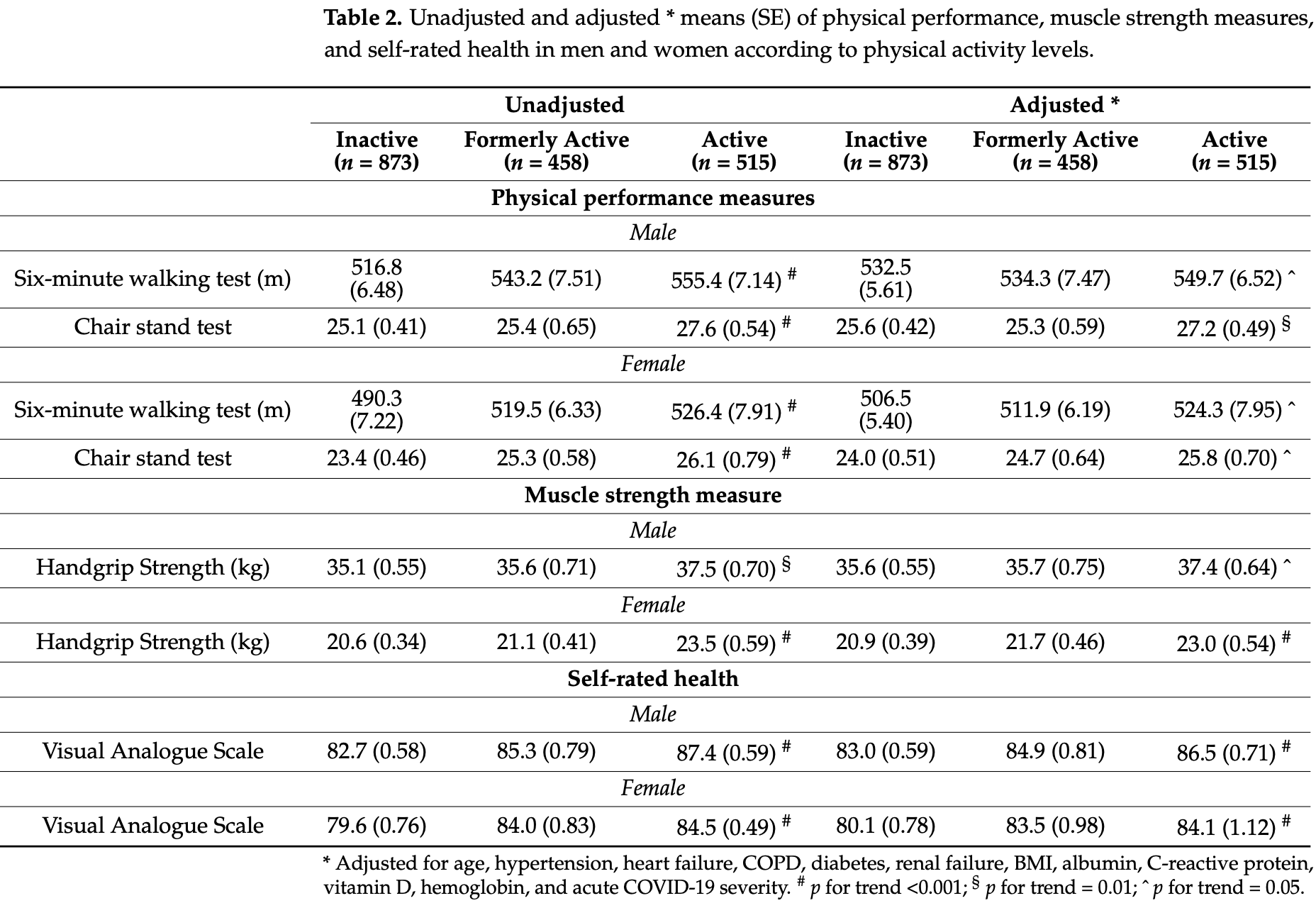
Background-Patients affected by Long COVID often report shorter times spent doing physical activity (PA) after COVID-19. The aim of the present study was to evaluate potential associations between PA levels and parameters of physical function in a cohort of COVID-19 survivors with postacute symptoms, with a particular focus on individuals aged 65 and older. Materials and methods-PA levels before and after COVID-19 were assessed in a sample of patients that had recovered from COVID-19 and were admitted to a post-acute outpatient service at the Fondazione Policlinico Universitario Agostino Gemelli IRCCS (Rome, Italy). Participation in PA was operationalized as the engagement in leisure-time PA for at least 150 min per week in the last 3 months. Self-rated health and measures of physical performance and muscle strength were assessed. Results-Mean age of 1846 participants was 55.2 ± 14.4 years and 47% were women. Before COVID-19, inactivity was detected in 47% of the whole study population; only 28% maintained pre-COVID-19 PA engagement. Inactivity was more frequent in women. The stopping of physical activity was associated with increased BMI and CRP levels, lower vitamin D levels and a higher prevalence of post-COVID-19 fatigue, dyspnea, arthralgia, and myalgia. Active participants had higher handgrip strength and performed better on both the six-minute walking test (6MWT) and at the one-minute sit-to-stand test (1MSTST). In particular, at the 6MWT, participants 65 and older that were still active after COVID-19 walked 32 m more than sedentary peers. Moreover, the distance covered was 28 m more than those who were active only before COVID-19 (p = 0.05). Formerly active subjects performed similarly at the 6MWT to inactive participants. PA was associated with better self-rated health. Conclusions-Our findings reveal that inactivity is frequent in the post-acute COVID-19 phase. Stopping physical activity after COVID-19 results in measures of performance that are comparable to those who were never active. Relevant differences in the distance covered at the 6MWT were found between older active subjects and their sedentary peers.
Funding: The study was unconditionally supported by Fondazione Angelini, Fondazione Memmo, Danone, Nutricia.
Institutional Review Board Statement: The study was approved by the Ethics Committee of the Università Cattolica del Sacro Cuore (Rome, Italy) (IRB number: 32/20). Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: None of the participants in the
References
Aghagoli, Gallo Marin, Katchur, Chaves-Sell, Asaad et al., Neurological Involvement in COVID-19 and Potential Mechanisms: A Review, Neurocrit. Care, doi:10.1007/s12028-020-01049-4
Ahmed, Patel, Greenwood, Halpin, Lewthwaite et al., Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis, J. Rehabil. Med
Alkodaymi, Omrani, Fawzy, Shaar, Almamlouk et al., Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: A systematic review and meta-analysis, Clin. Microbiol. Infect, doi:10.1016/j.cmi.2022.01.014
Amin, COVID-19 and the liver: Overview, Eur. J. Gastroenterol. Hepatol, doi:10.1097/MEG.0000000000001808
Asadi-Pooya, Akbari, Emami, Lotfi, Rostamihosseinkhani et al., Risk Factors Associated with Long COVID Syndrome: A Retrospective Study, Iran. J. Med. Sci
Awick, Ehlers, Aguiñaga, Daugherty, Kramer et al., Effects of a randomized exercise trial on physical activity, psychological distress and quality of life in older adults, Gen. Hosp. Psychiatry, doi:10.1016/j.genhosppsych.2017.06.005
Bayer, Hoegberget-Kalisz, Jensen, Olesen, Svensson et al., Role of tissue perfusion, muscle strength recovery, and pain in rehabilitation after acute muscle strain injury: A randomized controlled trial comparing early and delayed rehabilitation, Scand. J. Med. Sci. Sport
Bhutani, Vandellen, Cooper, Longitudinal Weight Gain and Related Risk Behaviors during the COVID-19 Pandemic in Adults in the US, Nutrients, doi:10.3390/nu13020671
Bislev, Langagergaard Rødbro, Rolighed, Sikjaer, Rejnmark, Effects of Vitamin D3 Supplementation on Muscle Strength, Mass, and Physical Performance in Women with Vitamin D Insufficiency: A Randomized Placebo-Controlled Trial, Calcif. Tissue Int, doi:10.1007/s00223-018-0443-z
Bohannon, Crouch, Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: A systematic review, J. Eval. Clin. Pract, doi:10.1111/jep.12629
Briand, Behal, Chenivesse, Wémeau-Stervinou, Wallaert, The 1-minute sit-to-stand test to detect exercise-induced oxygen desaturation in patients with interstitial lung disease, Ther. Adv. Respir. Dis, doi:10.1177/1753466618793028
Carfì, Bernabei, Landi, Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19, JAMA, doi:10.1001/jama.2020.12603
Chastin, Abaraogu, Bourgois, Dall, Darnborough et al., Effects of Regular Physical Activity on the Immune System, Vaccination and Risk of Community-Acquired Infectious Disease in the General Population: Systematic Review and Meta-Analysis, Sport. Med, doi:10.1007/s40279-021-01466-1
De Boer, Van Lanschot, Stalmeier, Van Sandick, Hulscher et al., Is a single-item visual analogue scale as valid, reliable and responsive as multi-item scales in measuring quality of life?, Qual. Life Res, doi:10.1023/B:QURE.0000018499.64574.1f
Delbressine, Machado, Goërtz, Van Herck, Meys et al., The Impact of Post-COVID-19 Syndrome on Self-Reported Physical Activity, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph18116017
Ekelund, Tarp, Steene-Johannessen, Hansen, Jefferis et al., Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonised meta-analysis, BMJ, doi:10.1136/bmj.l4570
Falck, Davis, Best, Crockett, Liu-Ambrose, Impact of exercise training on physical and cognitive function among older adults: A systematic review and meta-analysis, Neurobiol. Aging, doi:10.1016/j.neurobiolaging.2019.03.007
Fernández-De-Las-Peñas, Notarte, Peligro, Velasco, Ocampo et al., Long-COVID Symptoms in Individuals Infected with Different SARS-CoV-2 Variants of Concern: A Systematic Review of the Literature, Viruses, doi:10.3390/v14122629
Galluzzo, Ciciarello, Tosato, Zazzara, Pais et al., Association between vitamin D status and physical performance in COVID-19 survivors: Results from the Gemelli against COVID-19 post-acute care project, Mech. Ageing Dev, doi:10.1016/j.mad.2022.111684
Galluzzo, Zazzara, Ciciarello, Savera, Pais et al., Fatigue in Covid-19 survivors: The potential impact of a nutritional supplement on muscle strength and function, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2022.08.029
Gemelli, Against COVID-19 Post-Acute Care Study Group. Post-COVID-19 global health strategies: The need for an interdisciplinary approach, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01616-x
Gleeson, Bishop, Stensel, Lindley, Mastana et al., The anti-inflammatory effects of exercise: Mechanisms and implications for the prevention and treatment of disease, Nat. Rev. Immunol, doi:10.1038/nri3041
Groessl, Kaplan, Rejeski, Katula, Glynn et al., Physical Activity and Performance Impact Long-term Quality of Life in Older Adults at Risk for Major Mobility Disability, Am. J. Prev. Med, doi:10.1016/j.amepre.2018.09.006
Guyatt, Sullivan, Thompson, Fallen, Pugsley et al., The 6-minute walk: A new measure of exercise capacity in patients with chronic heart failure, Can. Med. Assoc. J
Hansen, Ambroziak, Thornton, Mundt, Kahn et al., Vitamin D Status and Physical Activity during Wintertime in Forensic Inpatients-A Randomized Clinical Trial, Nutrients
Jonsson, Hurtig-Wennlöf, Ahlsson, Vidlund, Cao et al., In-hospital physiotherapy improves physical activity level after lung cancer surgery: A randomized controlled trial, Physiotherapy, doi:10.1016/j.physio.2018.11.001
Landi, Calvani, Martone, Salini, Zazzara et al., Normative values of muscle strength across ages in a "real world" population: Results from the longevity check-up 7+ project, J. Cachexia Sarcopenia Muscle, doi:10.1002/jcsm.12610
Landi, Martone, Ciciarello, Galluzzo, Savera et al., On behalf of Gemelli Against COVID-19 Post-Acute Care Team. Effects of a New Multicomponent Nutritional Supplement on Muscle Mass and Physical Performance in Adult and Old Patients Recovered from COVID-19: A Pilot Observational Case-Control Study, Nutrients, doi:10.3390/nu14112316
Lee, Lee, Moon, Jin, Yang et al., Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: A nationwide cohort study, Br. J. Sport. Med, doi:10.1136/bjsports-2021-104203
Lee, Shiroma, Lobelo, Puska, Blair et al., Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy, Lancet, doi:10.1016/S0140-6736(12)61031-9
Levis, Gómez-Marín, Vitamin D and Physical Function in Sedentary Older Men, J. Am. Geriatr. Soc
Lombardo, Foppiani, Peretti, Mangiavini, Battezzati et al., Long-Term Coronavirus Disease 2019 Complications in Inpatients and Outpatients: A One-Year Follow-up Cohort Study, Open Forum Infect. Dis, doi:10.1093/ofid/ofab384
Martone, Tosato, Ciciarello, Galluzzo, Zazzara et al., Sarcopenia as potential biological substrate of long COVID-19 syndrome: Prevalence, clinical features, and risk factors, J. Cachexia Sarcopenia Muscle, doi:10.1002/jcsm.12931
Mascherini, Catelan, Pellegrini-Giampietro, Petri, Scaletti et al., Changes in physical activity levels, eating habits and psychological well-being during the Italian COVID-19 pandemic lockdown: Impact of socio-demographic factors on the Florentine academic population, PLoS ONE, doi:10.1371/journal.pone.0252395
Mcnarry, Berg, Shelley, Hudson, Saynor et al., Inspiratory muscle training enhances recovery post-COVID-19: A randomised controlled trial, Eur. Respir. J, doi:10.1183/13993003.03101-2021
Mohamed, Alawna, The effect of aerobic exercise on immune biomarkers and symptoms severity and progression in patients with COVID-19: A randomized control trial, J. Bodyw. Mov. Ther, doi:10.1016/j.jbmt.2021.07.012
Nieman, Henson, Austin, Sha, Upper respiratory tract infection is reduced in physically fit and active adults, Br. J. Sport. Med, doi:10.1136/bjsm.2010.077875
Notarte, De Oliveira, Peligro, Velasco, Macaranas et al., Sex and Previous Comorbidities as Risk Factors Not Associated with SARS-CoV-2 Infection for Long COVID-19: A Systematic Review and Meta-Analysis, J. Clin. Med, doi:10.3390/jcm11247314
Paneroni, Simonelli, Saleri, Bertacchini, Venturelli et al., Muscle Strength and Physical Performance in Patients Without Previous Disabilities Recovering From COVID-19 Pneumonia, Am. J. Phys. Med. Rehabil, doi:10.1097/PHM.0000000000001641
Polly, Tan, The role of vitamin D in skeletal and cardiac muscle function, Front. Physiol, doi:10.3389/fphys.2014.00145
Prete, Luzzetti, Augustin, Porciello, Montagnese et al., Changes in Lifestyle and Dietary Habits during COVID-19 Lockdown in Italy: Results of an Online Survey, Nutrients, doi:10.3390/nu13061923
Pérez-Gisbert, Torres-Sánchez, Ortiz-Rubio, Calvache-Mateo, López-López et al., Effects of the COVID-19 Pandemic on Physical Activity in Chronic Diseases: A Systematic Review and Meta-Analysis, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph182312278
Sallis, Young, Tartof, Sallis, Sall et al., Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients, Br. J. Sport. Med, doi:10.1136/bjsports-2021-104080
Samefors, Tengblad, Östgren, Sunlight Exposure and Vitamin D Levels in Older People-An Intervention Study in Swedish Nursing Homes, J. Nutr. Health Aging, doi:10.1007/s12603-020-1435-z
Sandler, Wyller, Moss-Morris, Buchwald, Crawley et al., Long COVID and Post-infective Fatigue Syndrome: A Review, Open Forum Infect. Dis, doi:10.1093/ofid/ofab440
Sardeli, Tomeleri, Cyrino, Fernhall, Cavaglieri et al., Effect of resistance training on inflammatory markers of older adults: A meta-analysis, Exp. Gerontol, doi:10.1016/j.exger.2018.07.021
Schipper, Prakken, Kalkhoven, Boes, Adipose tissue-resident immune cells: Key players in immunometabolism, Trends Endocrinol. Metab, doi:10.1016/j.tem.2012.05.011
Simpson, Kunz, Agha, Graff, Exercise and the Regulation of Immune Functions, Prog. Mol. Biol. Transl. Sci
Stengel, Malek, Zipfel, Goepel, Long Haulers-What Is the Evidence for Post-COVID Fatigue? Front, Psychiatry, doi:10.3389/fpsyt.2021.677934
Stockwell, Trott, Tully, Shin, Barnett et al., Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review, BMJ Open Sport Exerc. Med, doi:10.1136/bmjsem-2020-000960
Tajbakhsh, Gheibi Hayat, Taghizadeh, Akbari, Inabadi et al., COVID-19 and cardiac injury: Clinical manifestations, biomarkers, mechanisms, diagnosis, treatment, and follow up, Expert Rev. Anti. Infect. Ther, doi:10.1080/14787210.2020.1822737
Tir, Labor, Plavec, The effects of physical activity on chronic subclinical systemic inflammation, Arch. Ind. Hyg. Toxicol, doi:10.1515/aiht-2017-68-2965
Tosato, Calvani, Picca, Ciciarello, Galluzzo et al., Effects of l-Arginine Plus Vitamin C Supplementation on Physical Performance, Endothelial Function, and Persistent Fatigue in Adults with Long COVID: A Single-Blind Randomized Controlled Trial, Nutrients, doi:10.3390/nu14234984
Tosato, Ciciarello, Zazzara, Janiri, Pais et al., Lifestyle Changes and Psychological Well-Being in Older Adults During COVID-19 Pandemic, Clin. Geriatr. Med, doi:10.1016/j.cger.2022.05.002
Townsend, Dyer, Mccluskey, O'brien, Dowds et al., Investigating the Relationship between Vitamin D and Persistent Symptoms Following SARS-CoV-2 Infection, Nutrients, doi:10.3390/nu13072430
Wahid, Manek, Nichols, Kelly, Foster et al., Quantifying the Association Between Physical Activity and Cardiovascular Disease and Diabetes: A Systematic Review and Meta-Analysis, J. Am. Heart Assoc, doi:10.1161/JAHA.115.002495
Wang, Kream, Stefano, Long-Term Respiratory and Neurological Sequelae of COVID-19, Med. Sci. Monit, doi:10.12659/MSM.928996
Wang, Liu, Li, Xiao, Exercise Regulates the Immune System, Adv. Exp. Med. Biol
Wong, Lai, Ou, Ho, Chan et al., Is exercise protective against influenza-associated mortality?, PLoS ONE, doi:10.1371/journal.pone.0002108
Wright, Astill, Sivan, The Relationship between Physical Activity and Long COVID: A Cross-Sectional Study, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19095093
Zaccagni, Toselli, Barbieri, Physical Activity during COVID-19 Lockdown in Italy: A Systematic Review, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph18126416
Zanini, Aiello, Cherubino, Zampogna, Chetta et al., The one repetition maximum test and the sit-to-stand test in the assessment of a specific pulmonary rehabilitation program on peripheral muscle strength in COPD patients, Int. J. Chronic Obstr. Pulm. Dis, doi:10.2147/COPD.S91176
DOI record:
{
"DOI": "10.3390/jcm12072517",
"ISSN": [
"2077-0383"
],
"URL": "http://dx.doi.org/10.3390/jcm12072517",
"abstract": "<jats:p>Background—Patients affected by Long COVID often report shorter times spent doing physical activity (PA) after COVID-19. The aim of the present study was to evaluate potential associations between PA levels and parameters of physical function in a cohort of COVID-19 survivors with post-acute symptoms, with a particular focus on individuals aged 65 and older. Materials and methods—PA levels before and after COVID-19 were assessed in a sample of patients that had recovered from COVID-19 and were admitted to a post-acute outpatient service at the Fondazione Policlinico Universitario Agostino Gemelli IRCCS (Rome, Italy). Participation in PA was operationalized as the engagement in leisure-time PA for at least 150 min per week in the last 3 months. Self-rated health and measures of physical performance and muscle strength were assessed. Results—Mean age of 1846 participants was 55.2 ± 14.4 years and 47% were women. Before COVID-19, inactivity was detected in 47% of the whole study population; only 28% maintained pre-COVID-19 PA engagement. Inactivity was more frequent in women. The stopping of physical activity was associated with increased BMI and CRP levels, lower vitamin D levels and a higher prevalence of post-COVID-19 fatigue, dyspnea, arthralgia, and myalgia. Active participants had higher handgrip strength and performed better on both the six-minute walking test (6MWT) and at the one-minute sit-to-stand test (1MSTST). In particular, at the 6MWT, participants 65 and older that were still active after COVID-19 walked 32 m more than sedentary peers. Moreover, the distance covered was 28 m more than those who were active only before COVID-19 (p = 0.05). Formerly active subjects performed similarly at the 6MWT to inactive participants. PA was associated with better self-rated health. Conclusions—Our findings reveal that inactivity is frequent in the post-acute COVID-19 phase. Stopping physical activity after COVID-19 results in measures of performance that are comparable to those who were never active. Relevant differences in the distance covered at the 6MWT were found between older active subjects and their sedentary peers.</jats:p>",
"alternative-id": [
"jcm12072517"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-4620-5979",
"affiliation": [
{
"name": "Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, 00168 Rome, Italy"
}
],
"authenticated-orcid": false,
"family": "Galluzzo",
"given": "Vincenzo",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, 00168 Rome, Italy"
}
],
"family": "Zazzara",
"given": "Maria Beatrice",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, 00168 Rome, Italy"
}
],
"family": "Ciciarello",
"given": "Francesca",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5750-9746",
"affiliation": [
{
"name": "Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, 00168 Rome, Italy"
}
],
"authenticated-orcid": false,
"family": "Tosato",
"given": "Matteo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, 00168 Rome, Italy"
}
],
"family": "Martone",
"given": "Anna Maria",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, 00168 Rome, Italy"
}
],
"family": "Pais",
"given": "Cristina",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, 00168 Rome, Italy"
}
],
"family": "Savera",
"given": "Giulia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5472-2365",
"affiliation": [
{
"name": "Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, 00168 Rome, Italy"
}
],
"authenticated-orcid": false,
"family": "Calvani",
"given": "Riccardo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7032-3487",
"affiliation": [
{
"name": "Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, 00168 Rome, Italy"
}
],
"authenticated-orcid": false,
"family": "Picca",
"given": "Anna",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9567-6983",
"affiliation": [
{
"name": "Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, 00168 Rome, Italy"
},
{
"name": "Department of Geriatrics and Orthopedics, Università Cattolica del Sacro Cuore, 00168 Rome, Italy"
}
],
"authenticated-orcid": false,
"family": "Marzetti",
"given": "Emanuele",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS, 00168 Rome, Italy"
},
{
"name": "Department of Geriatrics and Orthopedics, Università Cattolica del Sacro Cuore, 00168 Rome, Italy"
}
],
"family": "Landi",
"given": "Francesco",
"sequence": "additional"
},
{
"affiliation": [],
"name": "on behalf of Gemelli Against COVID-19 Post-Acute Care Team",
"sequence": "additional"
}
],
"container-title": "Journal of Clinical Medicine",
"container-title-short": "JCM",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
3,
27
]
],
"date-time": "2023-03-27T09:34:30Z",
"timestamp": 1679909670000
},
"deposited": {
"date-parts": [
[
2023,
3,
27
]
],
"date-time": "2023-03-27T10:31:53Z",
"timestamp": 1679913113000
},
"funder": [
{
"name": "Fondazione Angelini, Fondazione Memmo, Danone, Nutricia"
}
],
"indexed": {
"date-parts": [
[
2023,
3,
28
]
],
"date-time": "2023-03-28T04:41:14Z",
"timestamp": 1679978474414
},
"is-referenced-by-count": 0,
"issue": "7",
"issued": {
"date-parts": [
[
2023,
3,
27
]
]
},
"journal-issue": {
"issue": "7",
"published-online": {
"date-parts": [
[
2023,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
3,
27
]
],
"date-time": "2023-03-27T00:00:00Z",
"timestamp": 1679875200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2077-0383/12/7/2517/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "2517",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
3,
27
]
]
},
"published-online": {
"date-parts": [
[
2023,
3,
27
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/S0140-6736(12)61031-9",
"article-title": "Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "219",
"journal-title": "Lancet",
"key": "ref_1",
"volume": "380",
"year": "2012"
},
{
"DOI": "10.1161/JAHA.115.002495",
"article-title": "Quantifying the Association Between Physical Activity and Cardiovascular Disease and Diabetes: A Systematic Review and Meta-Analysis",
"author": "Wahid",
"doi-asserted-by": "crossref",
"first-page": "e002495",
"journal-title": "J. Am. Heart Assoc.",
"key": "ref_2",
"volume": "5",
"year": "2016"
},
{
"key": "ref_3",
"unstructured": "National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP) (2020). Physical Activity Prevents Chronic Disease."
},
{
"DOI": "10.1136/bmj.l4570",
"article-title": "Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: Systematic review and harmonised meta-analysis",
"author": "Ekelund",
"doi-asserted-by": "crossref",
"first-page": "l4570",
"journal-title": "BMJ",
"key": "ref_4",
"volume": "366",
"year": "2019"
},
{
"DOI": "10.1111/sms.13269",
"article-title": "Role of tissue perfusion, muscle strength recovery, and pain in rehabilitation after acute muscle strain injury: A randomized controlled trial comparing early and delayed rehabilitation",
"author": "Bayer",
"doi-asserted-by": "crossref",
"first-page": "2579",
"journal-title": "Scand. J. Med. Sci. Sport.",
"key": "ref_5",
"volume": "28",
"year": "2018"
},
{
"DOI": "10.1016/j.physio.2018.11.001",
"article-title": "In-hospital physiotherapy improves physical activity level after lung cancer surgery: A randomized controlled trial",
"author": "Jonsson",
"doi-asserted-by": "crossref",
"first-page": "434",
"journal-title": "Physiotherapy",
"key": "ref_6",
"volume": "105",
"year": "2019"
},
{
"DOI": "10.1183/13993003.03101-2021",
"article-title": "Inspiratory muscle training enhances recovery post-COVID-19: A randomised controlled trial",
"author": "McNarry",
"doi-asserted-by": "crossref",
"first-page": "2103101",
"journal-title": "Eur. Respir. J.",
"key": "ref_7",
"volume": "60",
"year": "2022"
},
{
"DOI": "10.1007/978-981-15-1792-1_27",
"article-title": "Exercise Regulates the Immune System",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "395",
"journal-title": "Adv. Exp. Med. Biol.",
"key": "ref_8",
"volume": "1228",
"year": "2020"
},
{
"DOI": "10.1007/s40279-021-01466-1",
"article-title": "Effects of Regular Physical Activity on the Immune System, Vaccination and Risk of Community-Acquired Infectious Disease in the General Population: Systematic Review and Meta-Analysis",
"author": "Chastin",
"doi-asserted-by": "crossref",
"first-page": "1673",
"journal-title": "Sport. Med.",
"key": "ref_9",
"volume": "51",
"year": "2021"
},
{
"DOI": "10.1136/bjsm.2010.077875",
"article-title": "Upper respiratory tract infection is reduced in physically fit and active adults",
"author": "Nieman",
"doi-asserted-by": "crossref",
"first-page": "987",
"journal-title": "Br. J. Sport. Med.",
"key": "ref_10",
"volume": "45",
"year": "2011"
},
{
"DOI": "10.1371/journal.pone.0002108",
"doi-asserted-by": "crossref",
"key": "ref_11",
"unstructured": "Wong, C.-M., Lai, H.-K., Ou, C.-Q., Ho, S.-Y., Chan, K.-P., Thach, T.-Q., Yang, L., Chau, Y.-K., Lam, T.-H., and Hedley, A.J. (2008). Is exercise protective against influenza-associated mortality?. PLoS ONE, 3."
},
{
"DOI": "10.1136/bmjsem-2020-000960",
"article-title": "Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review",
"author": "Stockwell",
"doi-asserted-by": "crossref",
"first-page": "e000960",
"journal-title": "BMJ Open Sport Exerc. Med.",
"key": "ref_12",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.3390/ijerph182312278",
"doi-asserted-by": "crossref",
"key": "ref_13",
"unstructured": "Pérez-Gisbert, L., Torres-Sánchez, I., Ortiz-Rubio, A., Calvache-Mateo, A., López-López, L., Cabrera-Martos, I., and Valenza, M.C. (2021). Effects of the COVID-19 Pandemic on Physical Activity in Chronic Diseases: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health, 18."
},
{
"DOI": "10.3390/ijerph18126416",
"doi-asserted-by": "crossref",
"key": "ref_14",
"unstructured": "Zaccagni, L., Toselli, S., and Barbieri, D. (2021). Physical Activity during COVID-19 Lockdown in Italy: A Systematic Review. Int. J. Environ. Res. Public Health, 18."
},
{
"DOI": "10.1371/journal.pone.0252395",
"doi-asserted-by": "crossref",
"key": "ref_15",
"unstructured": "Mascherini, G., Catelan, D., Pellegrini-Giampietro, D.E., Petri, C., Scaletti, C., and Gulisano, M. (2021). Changes in physical activity levels, eating habits and psychological well-being during the Italian COVID-19 pandemic lockdown: Impact of socio-demographic factors on the Florentine academic population. PLoS ONE, 16."
},
{
"DOI": "10.1136/bjsports-2021-104080",
"article-title": "Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients",
"author": "Sallis",
"doi-asserted-by": "crossref",
"first-page": "1099",
"journal-title": "Br. J. Sport. Med.",
"key": "ref_16",
"volume": "55",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2021-104203",
"article-title": "Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: A nationwide cohort study",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "901",
"journal-title": "Br. J. Sport. Med.",
"key": "ref_17",
"volume": "56",
"year": "2022"
},
{
"DOI": "10.1016/j.jbmt.2021.07.012",
"article-title": "The effect of aerobic exercise on immune biomarkers and symptoms severity and progression in patients with COVID-19: A randomized control trial",
"author": "Mohamed",
"doi-asserted-by": "crossref",
"first-page": "425",
"journal-title": "J. Bodyw. Mov. Ther.",
"key": "ref_18",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.12603",
"article-title": "Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19",
"author": "Bernabei",
"doi-asserted-by": "crossref",
"first-page": "603",
"journal-title": "JAMA",
"key": "ref_19",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.3390/ijerph18116017",
"doi-asserted-by": "crossref",
"key": "ref_20",
"unstructured": "Delbressine, J., Machado, F., Goërtz, Y., Van Herck, M., Meys, R., Houben-Wilke, S., Burtin, C., Franssen, F., Spies, Y., and Vijlbrief, H. (2021). The Impact of Post-COVID-19 Syndrome on Self-Reported Physical Activity. Int. J. Environ. Res. Public Health, 18."
},
{
"article-title": "Risk Factors Associated with Long COVID Syndrome: A Retrospective Study",
"author": "Akbari",
"first-page": "428",
"journal-title": "Iran. J. Med. Sci.",
"key": "ref_21",
"volume": "46",
"year": "2021"
},
{
"article-title": "Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis",
"author": "Ahmed",
"first-page": "jrm00063",
"journal-title": "J. Rehabil. Med.",
"key": "ref_22",
"volume": "52",
"year": "2020"
},
{
"key": "ref_23",
"unstructured": "Gemelli Against COVID-19 Post-Acute Care Study Group (2020). Post-COVID-19 global health strategies: The need for an interdisciplinary approach. Aging Clin. Exp. Res., 32, 1613–1620."
},
{
"key": "ref_24",
"unstructured": "World Health Organization (2020, June 17). Criteria for Releasing COVID-19 Patients from Isolation, Available online: https://www.who.int/news-room/commentaries/detail/criteria-for-releasing-covid-19-patients-from-isolation."
},
{
"DOI": "10.1080/14787210.2020.1822737",
"article-title": "COVID-19 and cardiac injury: Clinical manifestations, biomarkers, mechanisms, diagnosis, treatment, and follow up",
"author": "Tajbakhsh",
"doi-asserted-by": "crossref",
"first-page": "345",
"journal-title": "Expert Rev. Anti. Infect. Ther.",
"key": "ref_25",
"volume": "19",
"year": "2021"
},
{
"article-title": "Long-Term Respiratory and Neurological Sequelae of COVID-19",
"author": "Wang",
"first-page": "e928996-1",
"journal-title": "Med. Sci. Monit.",
"key": "ref_26",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1007/s12028-020-01049-4",
"article-title": "Neurological Involvement in COVID-19 and Potential Mechanisms: A Review",
"author": "Aghagoli",
"doi-asserted-by": "crossref",
"first-page": "1062",
"journal-title": "Neurocrit. Care",
"key": "ref_27",
"volume": "34",
"year": "2021"
},
{
"DOI": "10.1097/MEG.0000000000001808",
"article-title": "COVID-19 and the liver: Overview",
"author": "Amin",
"doi-asserted-by": "crossref",
"first-page": "309",
"journal-title": "Eur. J. Gastroenterol. Hepatol.",
"key": "ref_28",
"volume": "33",
"year": "2020"
},
{
"DOI": "10.1016/j.mad.2022.111684",
"article-title": "Association between vitamin D status and physical performance in COVID-19 survivors: Results from the Gemelli against COVID-19 post-acute care project",
"author": "Galluzzo",
"doi-asserted-by": "crossref",
"first-page": "111684",
"journal-title": "Mech. Ageing Dev.",
"key": "ref_29",
"volume": "205",
"year": "2022"
},
{
"key": "ref_30",
"unstructured": "U.S. Department of Health and Human Services (2018). Physical Activity Guidelines for Americans."
},
{
"DOI": "10.1002/jcsm.12610",
"article-title": "Normative values of muscle strength across ages in a “real world” population: Results from the longevity check-up 7+ project",
"author": "Landi",
"doi-asserted-by": "crossref",
"first-page": "1562",
"journal-title": "J. Cachexia Sarcopenia Muscle",
"key": "ref_31",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1177/1753466618793028",
"article-title": "The 1-minute sit-to-stand test to detect exercise-induced oxygen desaturation in patients with interstitial lung disease",
"author": "Briand",
"doi-asserted-by": "crossref",
"first-page": "1753466618793028",
"journal-title": "Ther. Adv. Respir. Dis.",
"key": "ref_32",
"volume": "12",
"year": "2018"
},
{
"DOI": "10.2147/COPD.S91176",
"article-title": "The one repetition maximum test and the sit-to-stand test in the assessment of a specific pulmonary rehabilitation program on peripheral muscle strength in COPD patients",
"author": "Zanini",
"doi-asserted-by": "crossref",
"first-page": "2423",
"journal-title": "Int. J. Chronic Obstr. Pulm. Dis.",
"key": "ref_33",
"volume": "10",
"year": "2015"
},
{
"article-title": "The 6-minute walk: A new measure of exercise capacity in patients with chronic heart failure",
"author": "Guyatt",
"first-page": "919",
"journal-title": "Can. Med. Assoc. J.",
"key": "ref_34",
"volume": "132",
"year": "1985"
},
{
"DOI": "10.1023/B:QURE.0000018499.64574.1f",
"article-title": "Is a single-item visual analogue scale as valid, reliable and responsive as multi-item scales in measuring quality of life?",
"author": "Stalmeier",
"doi-asserted-by": "crossref",
"first-page": "311",
"journal-title": "Qual. Life Res.",
"key": "ref_35",
"volume": "13",
"year": "2004"
},
{
"DOI": "10.3390/nu13061923",
"doi-asserted-by": "crossref",
"key": "ref_36",
"unstructured": "Prete, M., Luzzetti, A., Augustin, L.S.A., Porciello, G., Montagnese, C., Calabrese, I., Ballarin, G., Coluccia, S., Patel, L., and Vitale, S. (2021). Changes in Lifestyle and Dietary Habits during COVID-19 Lockdown in Italy: Results of an Online Survey. Nutrients, 13."
},
{
"DOI": "10.3390/jcm11247314",
"doi-asserted-by": "crossref",
"key": "ref_37",
"unstructured": "Notarte, K.I., de Oliveira, M.H.S., Peligro, P.J., Velasco, J.V., Macaranas, I., Ver, A.T., Pangilinan, F.C., Pastrana, A., Goldrich, N., and Kavteladze, D. (2022). Age, Sex and Previous Comorbidities as Risk Factors Not Associated with SARS-CoV-2 Infection for Long COVID-19: A Systematic Review and Meta-Analysis. J. Clin. Med., 11."
},
{
"DOI": "10.1016/j.cmi.2022.01.014",
"article-title": "Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: A systematic review and meta-analysis",
"author": "Alkodaymi",
"doi-asserted-by": "crossref",
"first-page": "657",
"journal-title": "Clin. Microbiol. Infect.",
"key": "ref_38",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1093/ofid/ofab440",
"article-title": "Long COVID and Post-infective Fatigue Syndrome: A Review",
"author": "Sandler",
"doi-asserted-by": "crossref",
"first-page": "ofab440",
"journal-title": "Open Forum Infect. Dis.",
"key": "ref_39",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.3389/fpsyt.2021.677934",
"article-title": "Long Haulers—What Is the Evidence for Post-COVID Fatigue?",
"author": "Stengel",
"doi-asserted-by": "crossref",
"first-page": "677934",
"journal-title": "Front. Psychiatry",
"key": "ref_40",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.3390/nu14234984",
"doi-asserted-by": "crossref",
"key": "ref_41",
"unstructured": "Tosato, M., Calvani, R., Picca, A., Ciciarello, F., Galluzzo, V., Coelho-Júnior, H.J., Di Giorgio, A., Di Mario, C., Gervasoni, J., and Gremese, E. (2022). Effects of l-Arginine Plus Vitamin C Supplementation on Physical Performance, Endothelial Function, and Persistent Fatigue in Adults with Long COVID: A Single-Blind Randomized Controlled Trial. Nutrients, 14."
},
{
"DOI": "10.1016/j.clnesp.2022.08.029",
"article-title": "Fatigue in Covid-19 survivors: The potential impact of a nutritional supplement on muscle strength and function",
"author": "Galluzzo",
"doi-asserted-by": "crossref",
"first-page": "215",
"journal-title": "Clin. Nutr. ESPEN",
"key": "ref_42",
"volume": "51",
"year": "2022"
},
{
"DOI": "10.3390/nu14112316",
"doi-asserted-by": "crossref",
"key": "ref_43",
"unstructured": "Landi, F., Martone, A.M., Ciciarello, F., Galluzzo, V., Savera, G., Calvani, R., Picca, A., Marzetti, E., Tosato, M., and On behalf of Gemelli Against COVID-19 Post-Acute Care Team (2022). Effects of a New Multicomponent Nutritional Supplement on Muscle Mass and Physical Performance in Adult and Old Patients Recovered from COVID-19: A Pilot Observational Case–Control Study. Nutrients, 14."
},
{
"DOI": "10.3390/ijerph19095093",
"doi-asserted-by": "crossref",
"key": "ref_44",
"unstructured": "Wright, J., Astill, S.L., and Sivan, M. (2022). The Relationship between Physical Activity and Long COVID: A Cross-Sectional Study. Int. J. Environ. Res. Public Health, 19."
},
{
"DOI": "10.1093/ofid/ofab384",
"article-title": "Long-Term Coronavirus Disease 2019 Complications in Inpatients and Outpatients: A One-Year Follow-up Cohort Study",
"author": "Lombardo",
"doi-asserted-by": "crossref",
"first-page": "ofab384",
"journal-title": "Open Forum Infect. Dis.",
"key": "ref_45",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.3390/nu13020671",
"doi-asserted-by": "crossref",
"key": "ref_46",
"unstructured": "Bhutani, S., vanDellen, M.R., and Cooper, J.A. (2021). Longitudinal Weight Gain and Related Risk Behaviors during the COVID-19 Pandemic in Adults in the US. Nutrients, 13."
},
{
"DOI": "10.1016/j.exger.2018.07.021",
"article-title": "Effect of resistance training on inflammatory markers of older adults: A meta-analysis",
"author": "Sardeli",
"doi-asserted-by": "crossref",
"first-page": "188",
"journal-title": "Exp. Gerontol.",
"key": "ref_47",
"volume": "111",
"year": "2018"
},
{
"article-title": "The effects of physical activity on chronic subclinical systemic inflammation",
"author": "Tir",
"first-page": "276",
"journal-title": "Arch. Ind. Hyg. Toxicol.",
"key": "ref_48",
"volume": "68",
"year": "2017"
},
{
"DOI": "10.1038/nri3041",
"article-title": "The anti-inflammatory effects of exercise: Mechanisms and implications for the prevention and treatment of disease",
"author": "Gleeson",
"doi-asserted-by": "crossref",
"first-page": "607",
"journal-title": "Nat. Rev. Immunol.",
"key": "ref_49",
"volume": "11",
"year": "2011"
},
{
"DOI": "10.1016/bs.pmbts.2015.08.001",
"article-title": "Exercise and the Regulation of Immune Functions",
"author": "Simpson",
"doi-asserted-by": "crossref",
"first-page": "355",
"journal-title": "Prog. Mol. Biol. Transl. Sci.",
"key": "ref_50",
"volume": "135",
"year": "2015"
},
{
"DOI": "10.1016/j.tem.2012.05.011",
"article-title": "Adipose tissue-resident immune cells: Key players in immunometabolism",
"author": "Schipper",
"doi-asserted-by": "crossref",
"first-page": "407",
"journal-title": "Trends Endocrinol. Metab.",
"key": "ref_51",
"volume": "23",
"year": "2012"
},
{
"DOI": "10.3390/nu13103510",
"doi-asserted-by": "crossref",
"key": "ref_52",
"unstructured": "Hansen, A.L., Ambroziak, G., Thornton, D.M., Mundt, J.C., Kahn, R.E., Dahl, L., Waage, L., Kattenbraker, D., and Grung, B. (2021). Vitamin D Status and Physical Activity during Wintertime in Forensic Inpatients-A Randomized Clinical Trial. Nutrients, 13."
},
{
"DOI": "10.1111/jgs.14510",
"article-title": "Vitamin D and Physical Function in Sedentary Older Men",
"author": "Levis",
"doi-asserted-by": "crossref",
"first-page": "323",
"journal-title": "J. Am. Geriatr. Soc.",
"key": "ref_53",
"volume": "65",
"year": "2017"
},
{
"DOI": "10.1007/s00223-018-0443-z",
"article-title": "Effects of Vitamin D3 Supplementation on Muscle Strength, Mass, and Physical Performance in Women with Vitamin D Insufficiency: A Randomized Placebo-Controlled Trial",
"author": "Bislev",
"doi-asserted-by": "crossref",
"first-page": "483",
"journal-title": "Calcif. Tissue Int.",
"key": "ref_54",
"volume": "103",
"year": "2018"
},
{
"DOI": "10.3389/fphys.2014.00145",
"article-title": "The role of vitamin D in skeletal and cardiac muscle function",
"author": "Polly",
"doi-asserted-by": "crossref",
"first-page": "145",
"journal-title": "Front. Physiol.",
"key": "ref_55",
"volume": "5",
"year": "2014"
},
{
"DOI": "10.1007/s12603-020-1435-z",
"article-title": "Sunlight Exposure and Vitamin D Levels in Older People—An Intervention Study in Swedish Nursing Homes",
"author": "Samefors",
"doi-asserted-by": "crossref",
"first-page": "1047",
"journal-title": "J. Nutr. Health Aging",
"key": "ref_56",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.3390/nu13072430",
"doi-asserted-by": "crossref",
"key": "ref_57",
"unstructured": "Townsend, L., Dyer, A.H., McCluskey, P., O’Brien, K., Dowds, J., Laird, E., Bannan, C., Bourke, N.M., Cheallaigh, C.N., and Byrne, D.G. (2021). Investigating the Relationship between Vitamin D and Persistent Symptoms Following SARS-CoV-2 Infection. Nutrients, 13."
},
{
"DOI": "10.1111/jep.12629",
"article-title": "Crouch R. Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: A systematic review",
"author": "Bohannon",
"doi-asserted-by": "crossref",
"first-page": "377",
"journal-title": "J. Eval. Clin. Pract.",
"key": "ref_58",
"volume": "23",
"year": "2017"
},
{
"DOI": "10.1016/j.neurobiolaging.2019.03.007",
"article-title": "Impact of exercise training on physical and cognitive function among older adults: A systematic review and meta-analysis",
"author": "Falck",
"doi-asserted-by": "crossref",
"first-page": "119",
"journal-title": "Neurobiol. Aging",
"key": "ref_59",
"volume": "79",
"year": "2019"
},
{
"DOI": "10.1097/PHM.0000000000001641",
"article-title": "Muscle Strength and Physical Performance in Patients Without Previous Disabilities Recovering From COVID-19 Pneumonia",
"author": "Paneroni",
"doi-asserted-by": "crossref",
"first-page": "105",
"journal-title": "Am. J. Phys. Med. Rehabil.",
"key": "ref_60",
"volume": "100",
"year": "2021"
},
{
"DOI": "10.1002/jcsm.12931",
"article-title": "Sarcopenia as potential biological substrate of long COVID-19 syndrome: Prevalence, clinical features, and risk factors",
"author": "Martone",
"doi-asserted-by": "crossref",
"first-page": "1974",
"journal-title": "J. Cachexia Sarcopenia Muscle",
"key": "ref_61",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.genhosppsych.2017.06.005",
"article-title": "Effects of a randomized exercise trial on physical activity, psychological distress and quality of life in older adults",
"author": "Awick",
"doi-asserted-by": "crossref",
"first-page": "44",
"journal-title": "Gen. Hosp. Psychiatry",
"key": "ref_62",
"volume": "49",
"year": "2017"
},
{
"DOI": "10.1016/j.amepre.2018.09.006",
"article-title": "Physical Activity and Performance Impact Long-term Quality of Life in Older Adults at Risk for Major Mobility Disability",
"author": "Groessl",
"doi-asserted-by": "crossref",
"first-page": "141",
"journal-title": "Am. J. Prev. Med.",
"key": "ref_63",
"volume": "56",
"year": "2019"
},
{
"DOI": "10.1016/j.cger.2022.05.002",
"article-title": "Lifestyle Changes and Psychological Well-Being in Older Adults During COVID-19 Pandemic",
"author": "Tosato",
"doi-asserted-by": "crossref",
"first-page": "449",
"journal-title": "Clin. Geriatr. Med.",
"key": "ref_64",
"volume": "38",
"year": "2022"
},
{
"DOI": "10.3390/v14122629",
"doi-asserted-by": "crossref",
"key": "ref_65",
"unstructured": "Fernández-de-Las-Peñas, C., Notarte, K.I., Peligro, P.J., Velasco, J.V., Ocampo, M.J., Henry, B.M., Arendt-Nielsen, L., Torres-Macho, J., and Plaza-Manzano, G. (2022). Long-COVID Symptoms in Individuals Infected with Different SARS-CoV-2 Variants of Concern: A Systematic Review of the Literature. Viruses, 14."
}
],
"reference-count": 65,
"references-count": 65,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2077-0383/12/7/2517"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Inadequate Physical Activity Is Associated with Worse Physical Function in a Sample of COVID-19 Survivors with Post-Acute Symptoms",
"type": "journal-article",
"volume": "12"
}
