The effect of aerobic exercise on immune biomarkers and symptoms severity and progression in patients with COVID-19: A randomized control trial
et al., Journal of Bodywork and Movement Therapies, doi:10.1016/j.jbmt.2021.07.012, Oct 2020
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Small RCT with 30 mild/moderate COVID-19 patients, 15 performing 2 weeks of moderate-intensity aerobic exercise, showing decreased severity (WURSS) and improved immune markers with exercise.
Mohamed et al., 31 Oct 2020, Turkey, peer-reviewed, 2 authors, study period April 2020 - June 2020.
The effect of aerobic exercise on immune biomarkers and symptoms severity and progression in patients with COVID-19: A randomized control trial
Journal of Bodywork and Movement Therapies, doi:10.1016/j.jbmt.2021.07.012
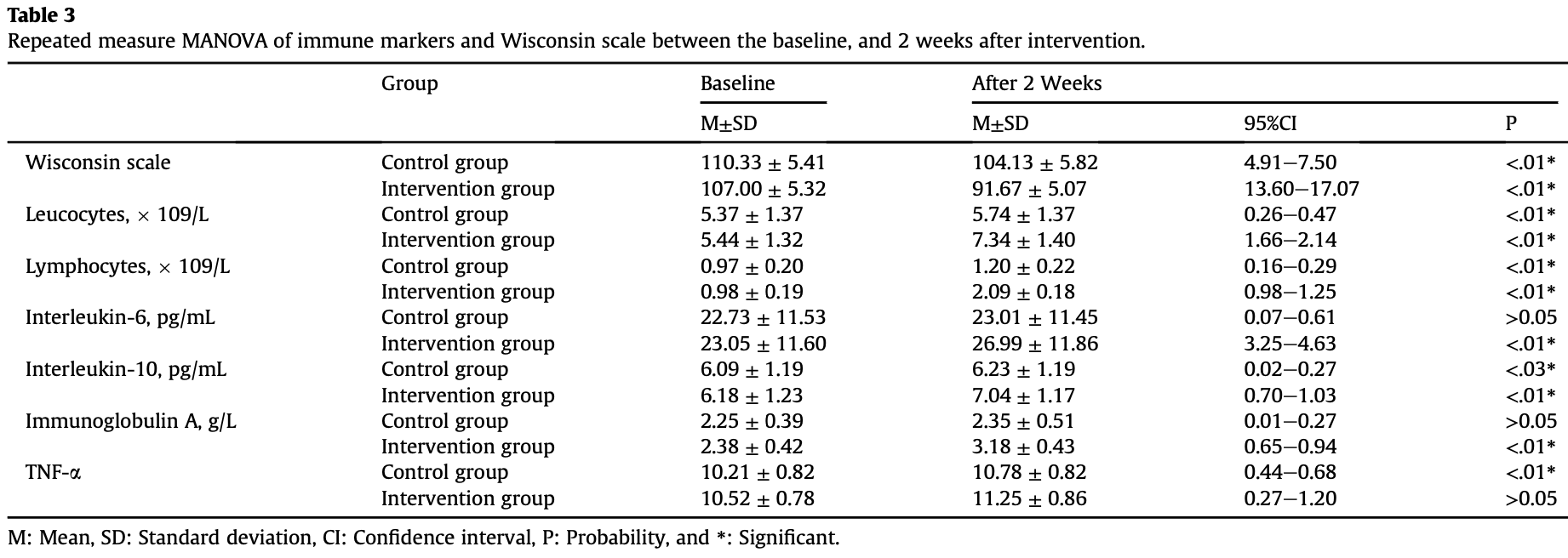
Background: The World Health Organization in March 2020 has announced that COVID-19 is a world pandemic because the number of infected cases increases rapidly. however, there are several available vaccines, their protection is limited to a certain period. Thus, the role of modalities that improve immune functions should be performed to counter COVID-19 viral load and decrease mortality rates. Objective: To investigate the effect of aerobic exercise on immune biomarkers, disease severity, and progression in patients with COVID-19. Design: A randomized controlled study. Participants: Thirty patients with COVID-19 participated in this study. Participants' age ranged from 24 to 45 years old. Participants had a mild or moderate COVID-19. Participants were assigned randomly into two groups, exercise and control groups. There were two main dependent variables including blood immune markers and severity of respiratory symptoms. Interventions: All participants performed 2 weeks of moderate-intensity aerobic exercise for 40 min/ session, 3 sessions/week. The measurements were performed at baseline, and after 2-weeks. Results: At baseline measurements, there were non-significant differences between both groups in the Wisconsin scale total score, Leucocytes, Lymphocytes, Interleukin-6, Interleukin-10, Immunoglobulin-A, and TNF-a (P > .05). After the intervention, the Wisconsin scale (patient-oriented illness-specific qualityof-life) total score significantly decreased in the intervention group (P < .05); while, Leucocytes, Lymphocytes, and Immunoglobulin-A significantly increased in the intervention group (P < .05).
Conclusion: The current study indicated that 2 weeks of moderate-intensity aerobic exercise decreased the severity and progression of COVID-19 associated disorders and quality of life. Also, a 2-weeks of aerobic exercise positively affected immune function by increasing the amounts of Leucocytes, Lymphocytes, Immunoglobulin A.
Declaration of competing interest The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
Affronti, Mansueto, Soresi, Abbene, Affronti et al., Low-grade fever: how to distinguish organic from non-organic forms, Int. J. Clin. Pract, doi:10.1111/j.1742-1241.2009.02256.x
Al-Tawfiq, Viral loads of SARS-CoV, MERS-CoV and SARS-CoV-2 in respiratory specimens: what have we learned?, Travel Med. Infect. Dis, doi:10.1016/j.tmaid.2020.101629
Alawna, Amro, Mohamed, Aerobic exercises recommendations and specifications for patients with COVID-19: a systematic review, Eur. Rev. Med. Pharmacol. Sci, doi:10.26355/eurrev_202012_24211
Albouaini, Egred, Alahmar, Wright, Cardiopulmonary exercise testing and its application, Postgrad. Med, doi:10.1136/hrt.2007.121558
Amro, Mohamed, Alawna, Effects of increasing aerobic capacity on improving psychological problems seen in patients with COVID-19: a review, Eur. Rev. Med. Pharmacol. Sci, doi:10.26355/eurrev_202103_25443
Arslan, Ipekci, Kebapcilar, Dogan Dede, Kurban et al., Effect of aerobic exercise training on MDA and TNF-a levels in patients with type 2 diabetes mellitus, Int. Sch. Res. Notices, doi:10.1155/2014/820387
Balducci, Zanuso, Nicolucci, Fernando, Cavallo et al., Anti-inflammatory effect of exercise training in subjects with type 2 diabetes and the metabolic syndrome is dependent on exercise modalities and independent of weight loss, Nutr. Metabol. Cardiovasc. Dis, doi:10.1016/j.numecd.2009.04.015
Barrett, Hayney, Muller, Rakel, Brown et al., Meditation or exercise for preventing acute respiratory infection (MEPARI-2): a randomized controlled trial, PLoS One, doi:10.1371/journal.pone.0197778
Broman-Fulks, Storey, Evaluation of a brief aerobic exercise intervention for high anxiety sensitivity, Hist. Philos. Logic, doi:10.1080/10615800701762675
Cascella, Rajnik, Cuomo, Dulebohn, Di Napoli, Features, evaluation and treatment coronavirus (COVID-19
Chan, Liu, Liang, Deng, Wu et al., Special issueetherapeutic benefits of physical activity for mood: a systematic review on the effects of exercise intensity, duration, and modality, J. Psychol, doi:10.1080/00223980.2018.1470487
Chao, R€ Otzschke, Tan, The role of IgA in COVID-19, Brain, Behav. Immun, doi:10.1016/j.bbi.2020.05.057
Chubak, Mctiernan, Sorensen, Wener, Yasui et al., Moderateintensity exercise reduces the incidence of colds among postmenopausal women, Am. J. Med, doi:10.1016/j.amjmed.2006.06.033
Crabbe, Smith, Dishman, Emotional & electroencephalographic responses during affective picture viewing after exercise, Physiol. Behav, doi:10.1016/j.physbeh.2006.10.001
Crawford, Drake, Carper, Deblauw, Heinrich, Validity, reliability, and application of the session-RPE method for quantifying training loads during high intensity functional training, Sports, doi:10.3390/sports6030084
Cunningham-Rundles, Lung disease, antibodies and other unresolved issues in immune globulin therapy for antibody deficiency, Clin. Exp. Immunol, doi:10.1111/j.1365-2249.2009.03952.x
De La Fuente, Martín, Ortega, Effect of physical exercise on the phagocytic function of peritoneal macrophages from Swiss mice, Comp. Immunol. Microbiol. Infect. Dis, doi:10.1016/0147-9571(93)90058-D
De Souza, Matos, Santos, Medeiros, Marinho et al., Effects of high-intensity interval and moderate-intensity continuous exercise on inflammatory, leptin, IgA, and lipid peroxidation responses in obese males, Front. Physiol, doi:10.3389/fphys.2018.00567
Di Gennaro, Pizzol, Marotta, Antunes, Racalbuto et al., Coronavirus diseases (COVID-19) current status and future perspectives: a narrative review, Int. J. Environ.Res. Public Health, doi:10.3390/ijerph17082690
Diao, Wang, Tan, Chen, Liu et al., Reduction and functional exhaustion of T cells in patients with coronavirus disease, Front. Immunol, doi:10.3389/fimmu.2020.00827
Dixit, Can moderate intensity aerobic exercise be an effective and valuable therapy in preventing and controlling the pandemic of COVID-19?, Med. Hypotheses, doi:10.1016/j.mehy.2020.109854
Fani, Teimoori, Ghafari, Comparison of the COVID-2019 (SARS-CoV-2) pathogenesis with SARS-CoV and MERS-CoV infections, Future Virol, doi:10.2217/fvl-2020-0050
Farhangimaleki, Zehsaz, Tiidus, The effect of tapering period on plasma pro-inflammatory cytokine levels and performance in elite male cyclists, J. Sports Sci. Med
Faul, Erdfelder, Lang, Buchner, G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences, Behav. Res. Methods, doi:10.3758/BF03193146
Gonzalo-Calvo, Montero, García-Gonz Alez, Tyshkovska, Gonz Alez-Medina et al., Circulating inflammatory miRNA signature in response to different doses of aerobic exercise, J. Appl. Physiol, doi:10.1152/japplphysiol.00077.2015
Gonçalves, Dantas, Santos, Dantas, Da Silva et al., Effect of acute and chronic aerobic exercise on immunological markers: a systematic review, Front. Physiol, doi:10.3389/fphys.2019.01602
Guan, Ni, Hu, Liang, Ou et al., Clinical characteristics of coronavirus disease 2019 in China, New Engl. J. Med, doi:10.1056/NEJMoa2002032
Hines, Schott, Bayly, Leroux, Exercise and immunity: a review with emphasis on the horse, J. Vet. Intern. Med, doi:10.1111/j.1939-1676.1996.tb02063.x
Hogan, Mata, Carstensen, Exercise holds immediate benefits for affect and cognition in younger and older adults, doi:10.1037/a0032634
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Kadam, Bhalerao, Sample size calculation, Int. J. Ayurveda Res, doi:10.4103/0974-7788.59946
Kadoglou, Iliadis, Angelopoulou, Perrea, Ampatzidis et al., The anti-inflammatory effects of exercise training in patients with type 2 diabetes mellitus, Eur. J. Prevent. Cardiol, doi:10.1097/HJR.0b013e3282efaf50
Li, Cheng, Alterations of immunoendocrine responses during the recovery period after acute prolonged cycling, Eur. J. Appl. Physiol, doi:10.1007/s00421-007-0529-1
Lippi, Banfi, Montagnana, Salvagno, Schena et al., Mean platelet volume (MPV) predicts middle distance running performance, Int. J. Lit. Humanit, doi:10.1371/journal.pone.0112892
Lira, Santos, Caldeira, Inoue, Panissa et al., Short-term high-and moderate-intensity training modifies inflammatory and metabolic factors in response to acute exercise, Front. Physiol, doi:10.3389/fphys.2017.00856
Lu, Stratton, Tang, Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle, J. Med. Virol, doi:10.1002/jmv.25678
Marklund, Mattsson, Wåhlin-Larsson, Ponsot, Lindval et al., Extensive inflammatory cell infiltration in human skeletal muscle in response to an ultraendurance exercise bout in experienced athletes, J. Appl. Physiol, doi:10.1152/japplphysiol.01538.2011
Marshall, The adverse effects of psychological stress on immunoregulatory balance: applications to human inflammatory diseases, Immunol. Allergy Clin, doi:10.1016/j.iac.2010.09.013
Martins, Cunha, Neves, Martins, Teixeira-Veríssimo et al., Effects of aerobic conditioning on salivary IgA and plasma IgA, IgG and IgM in older men and women, Int. J. Sports Med, doi:10.1055/s-0029-1237389
Matthews, Ockene, Freedson, Rosal, Merriam et al., Moderate to vigorous physical activity and risk of upper-respiratory tract infection, Med. Sci. Sports Exerc, doi:10.1097/00005768-200208000-00003
Mohamed, Alawna, Al-Turjman, Nassif, Physical therapy recommendations for patients with COVID-19, doi:10.1201/9781003098881-9
Mohamed, Alawna, Enhancing oxygenation of patients with coronavirus disease 2019: effects on immunity and other health-related conditions, World J. Clin. Cases, doi:10.12998/wjcc.v9.i19.4939
Mohamed, Alawna, Important role of relaxation techniques on immune functions, glycemic control, and stress in diabetic patients with COVID-19: a review, Curr. Diabetes Rev, doi:10.2174/1573399816999201012200109
Mohamed, Alawna, Role of increasing the aerobic capacity on improving the function of immune and respiratory systems in patients with coronavirus (COVID-19): a review, Diabetes Metab. Syndrome: Clin. Res. Rev, doi:10.1016/j.dsx.2020.04.038
Mohamed, Taha, Comparison between the effects of aerobic and resistive training on immunoglobulins in obese women, Bull. Facul. Phys. Ther, doi:10.4103/1110-6611.188023
Moldoveanu, Shephard, Shek, The cytokine response to physical activity and training, Sports Med, doi:10.2165/00007256-200131020-00004
Murphy, Davis, Brown, Carmichael, Van Rooijen et al., Role of lung macrophages on susceptibility to respiratory infection following short-term moderate exercise training, Am. J. Physiol. Regul. Integr. Comp. Physiol, doi:10.1152/ajpregu.00274.2004
Nabkasorn, Miyai, Sootmongkol, Junprasert, Yamamoto et al., Effects of physical exercise on depression, neuroendocrine stress hormones and physiological fitness in adolescent females with depressive symptoms, Eur. J. Publ. Health, doi:10.1093/eurpub/cki159
Natale, Brenner, Moldoveanu, Vasiliou, Shek et al., Effects of three different types of exercise on blood leukocyte count during and following exercise, Sao Paulo Med. J, doi:10.1590/s1516-31802003000100003
Nieman, Nehlsen-Cannarella, Markoff, Balk-Lamberton, Yang et al., The effects of moderate exercise training on natural killer cells and acute upper respiratory tract infections, Int. J. Sports Med, doi:10.1055/s-2007-1024839
Nieman, Nehlsen-Cannarella, The immune response to exercise, Semin. Hematol, doi:10.1016/b978-0-12-396454-0.00009-6
Okita, Nishijima, Murakami, Nagai, Morita et al., Can exercise training with weight loss lower serum C-reactive protein levels?, Arterioscler. Thromb. Vasc. Biol, doi:10.1161/01.ATV.0000140199.14930.32
Pedersen, Hoffman-Goetz, Exercise and the immune system: regulation, integration, and adaptation, Physiol. Rev, doi:10.1152/physrev.2000.80.3.1055
Pedersen, Influence of physical activity on the cellular immune system: mechanisms of action, Int. J. Sports Med, doi:10.1055/s-2007-1024746
Reed, Buck, The effect of regular aerobic exercise on positive-activated affect: a meta-analysis, Psychol. Sport Exerc, doi:10.1016/j.psychsport.2009.05.009
Reid, Drummond, Mackinnon, The effect of moderate aerobic exercise and relaxation on secretory immunoglobulin A, Int. J. Sports Med, doi:10.1055/s-2001-11347
Reis Gonçalves, Reis Gonçalves, De Almeida, Dos Santos Lopes, Dos Santos Durão et al., Protective effects of aerobic exercise on acute lung injury induced by LPS in mice, Crit. Care, doi:10.1186/cc11807
Rochon, Gondan, Kieser, To test or not to test: preliminary assessment of normality when comparing two independent samples, BMC Med. Res. Methodol, doi:10.1186/1471-2288-12-81
Rodríguez, Tj€ Arnlund, Ivanji, Singh, García et al., Role of IgA in the defense against respiratory infections: IgA deficient mice exhibited increased susceptibility to intranasal infection with Mycobacterium bovis BCG, Vaccine, doi:10.1016/j.vaccine.2004.11.032
Shimizu, Suzuki, Imai, Aizawa, Nanba et al., Monocyte and T-CELL responses to exercise training in elderly subjects, J. Strength Condit Res, doi:10.1519/JSC.0b013e3181fc5e67
Steensberg, Toft, Schjerling, Halkjaer-Kristensen, Pedersen, Plasma interleukin-6 during strenuous exercise: role of epinephrine, Am. J. Physiol. Cell Physiol, doi:10.1152/ajpcell.2001.281.3.c1001
Sugiura, Sugiura, Nishida, Inaba, Mirbod et al., Effects of different durations of exercise on macrophage functions in mice, J. Appl. Physiol, doi:10.1152/jappl.2001.90.3.789
Taylor, Murphy, Altered central integration of dual somatosensory input after cervical spine manipulation, J. Manipulative Physiol. Therapeut, doi:10.1093/occmed/kqx063
Toledo, Magalhaes, Hizume, Vieira, Biselli et al., Aerobic exercise attenuates pulmonary injury induced by exposure to cigarette smoke, Eur. Respir. J, doi:10.1183/09031936.00003411
Tvede, Kappel, Klarhund, Duhn, Halkjaer-Kristensen et al., Evidence that the effect of bicycle exercise on blood mononuclear cell proliferative responses and subsets is mediated by epinephrine, Int. J. Sports Med, doi:10.1055/s-2007-1021028
Viana, Kosmadakis, Watson, Bevington, Feehally et al., Evidence for anti-inflammatory effects of exercise in CKD, J. Am. Soc. Nephrol, doi:10.1681/ASN.2013070702
Who Director, s opening remarks at the media briefing on COVID-19 -11
Who, Considerations for Quarantine of Individuals in the Context of Containment for Coronavirus Disease
Who, Rational Use of Personal Protective Equipment for Coronavirus Disease
Williams, Hormonal contraception and the development of autoimmunity: a review of the literature, Linacre Q, doi:10.1080/00243639.2017.1360065
Wu, Morahan, Macrophages and other nonspecific defenses: role in modulating resistance against herpes simplex virus, Curr. Top. Microbiol. Immunol, doi:10.1007/978-3-642-77247-4_6
Xu, Fan, Wang, Zou, Yu et al., Suppressed T cell-mediated immunity in patients with COVID-19: a clinical retrospective study in Wuhan, China, J. Infect, doi:10.2139/ssrn.3558005
Yuki, Fujiogi, Koutsogiannaki, COVID-19 pathophysiology: a review, Clin. Immunol
Zheng, Qiu, Xia, Lin, Ye et al., Effect of aerobic exercise on inflammatory markers in healthy middle-aged and older adults: a systematic review and meta-analysis of randomized controlled trials, Front. Aging Neurosci, doi:10.3389/fnagi.2019.00098
Zhuang, Hu, Qiao, Lan, Lai et al., Lowgrade fever during COVID-19 convalescence: a report of 3 cases, World J. Clin. Cases, doi:10.12998/wjcc.v8.i12.2655
DOI record:
{
"DOI": "10.1016/j.jbmt.2021.07.012",
"ISSN": [
"1360-8592"
],
"URL": "http://dx.doi.org/10.1016/j.jbmt.2021.07.012",
"alternative-id": [
"S1360859221001674"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "The effect of aerobic exercise on immune biomarkers and symptoms severity and progression in patients with COVID-19: A randomized control trial"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Journal of Bodywork and Movement Therapies"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.jbmt.2021.07.012"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 Elsevier Ltd. All rights reserved."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5092-3549",
"affiliation": [],
"authenticated-orcid": false,
"family": "Mohamed",
"given": "Ayman A.",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-4936-373X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Alawna",
"given": "Motaz",
"sequence": "additional"
}
],
"container-title": [
"Journal of Bodywork and Movement Therapies"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.jp",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.fr",
"clinicalkey.com.au",
"bodyworkmovementtherapies.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
8,
5
]
],
"date-time": "2021-08-05T10:48:05Z",
"timestamp": 1628160485000
},
"deposited": {
"date-parts": [
[
2021,
11,
11
]
],
"date-time": "2021-11-11T07:31:17Z",
"timestamp": 1636615877000
},
"indexed": {
"date-parts": [
[
2022,
4,
20
]
],
"date-time": "2022-04-20T17:05:33Z",
"timestamp": 1650474333910
},
"is-referenced-by-count": 2,
"issn-type": [
{
"type": "print",
"value": "1360-8592"
}
],
"issued": {
"date-parts": [
[
2021,
10
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
10,
1
]
],
"date-time": "2021-10-01T00:00:00Z",
"timestamp": 1633046400000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S1360859221001674?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S1360859221001674?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "425-432",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
10
]
]
},
"published-print": {
"date-parts": [
[
2021,
10
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1111/j.1742-1241.2009.02256.x",
"article-title": "Low-grade fever: how to distinguish organic from non-organic forms",
"author": "Affronti",
"doi-asserted-by": "crossref",
"first-page": "316",
"issue": "3",
"journal-title": "Int. J. Clin. Pract.",
"key": "10.1016/j.jbmt.2021.07.012_bib1",
"volume": "64",
"year": "2010"
},
{
"DOI": "10.1016/j.tmaid.2020.101629",
"article-title": "Viral loads of SARS-CoV, MERS-CoV and SARS-CoV-2 in respiratory specimens: what have we learned?",
"author": "Al-Tawfiq",
"doi-asserted-by": "crossref",
"first-page": "101629",
"journal-title": "Travel Med. Infect. Dis.",
"key": "10.1016/j.jbmt.2021.07.012_bib2",
"volume": "34",
"year": "2020"
},
{
"article-title": "Aerobic exercises recommendations and specifications for patients with COVID-19: a systematic review",
"author": "Alawna",
"first-page": "13049",
"issue": "24",
"journal-title": "Eur. Rev. Med. Pharmacol. Sci.",
"key": "10.1016/j.jbmt.2021.07.012_bib3",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1136/hrt.2007.121558",
"article-title": "Cardiopulmonary exercise testing and its application",
"author": "Albouaini",
"doi-asserted-by": "crossref",
"first-page": "675",
"issue": "985",
"journal-title": "Postgrad. Med.",
"key": "10.1016/j.jbmt.2021.07.012_bib4",
"volume": "83",
"year": "2007"
},
{
"article-title": "Effects of increasing aerobic capacity on improving psychological problems seen in patients with COVID-19: a review",
"author": "Amro",
"first-page": "2808",
"issue": "6",
"journal-title": "Eur. Rev. Med. Pharmacol. Sci.",
"key": "10.1016/j.jbmt.2021.07.012_bib5",
"volume": "25",
"year": "2021"
},
{
"article-title": "Effect of aerobic exercise training on MDA and TNF- α levels in patients with type 2 diabetes mellitus",
"author": "Arslan",
"first-page": "1",
"journal-title": "Int. Sch. Res. Notices",
"key": "10.1016/j.jbmt.2021.07.012_bib6",
"year": "2014"
},
{
"DOI": "10.1016/j.numecd.2009.04.015",
"article-title": "Anti-inflammatory effect of exercise training in subjects with type 2 diabetes and the metabolic syndrome is dependent on exercise modalities and independent of weight loss",
"author": "Balducci",
"doi-asserted-by": "crossref",
"first-page": "608",
"issue": "8",
"journal-title": "Nutr. Metabol. Cardiovasc. Dis.",
"key": "10.1016/j.jbmt.2021.07.012_bib7",
"volume": "20",
"year": "2010"
},
{
"DOI": "10.1371/journal.pone.0197778",
"article-title": "Meditation or exercise for preventing acute respiratory infection (MEPARI-2): a randomized controlled trial",
"author": "Barrett",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "PLoS One",
"key": "10.1016/j.jbmt.2021.07.012_bib8",
"volume": "13",
"year": "2018"
},
{
"article-title": "Evaluation of a brief aerobic exercise intervention for high anxiety sensitivity",
"author": "Broman-Fulks",
"first-page": "117",
"issue": "2",
"journal-title": "Hist. Philos. Logic",
"key": "10.1016/j.jbmt.2021.07.012_bib9",
"volume": "21",
"year": "2008"
},
{
"article-title": "Features, evaluation and treatment coronavirus (COVID-19)",
"author": "Cascella",
"key": "10.1016/j.jbmt.2021.07.012_bib10",
"series-title": "StatPearls",
"year": "2020"
},
{
"DOI": "10.1080/00223980.2018.1470487",
"article-title": "Special issue–therapeutic benefits of physical activity for mood: a systematic review on the effects of exercise intensity, duration, and modality",
"author": "Chan",
"doi-asserted-by": "crossref",
"first-page": "102",
"issue": "1",
"journal-title": "J. Psychol.",
"key": "10.1016/j.jbmt.2021.07.012_bib11",
"volume": "153",
"year": "2019"
},
{
"DOI": "10.1016/j.bbi.2020.05.057",
"article-title": "The role of IgA in COVID-19",
"author": "Chao",
"doi-asserted-by": "crossref",
"first-page": "182",
"journal-title": "Brain, Behav. Immun.",
"key": "10.1016/j.jbmt.2021.07.012_bib12",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.1016/j.amjmed.2006.06.033",
"article-title": "Moderate-intensity exercise reduces the incidence of colds among postmenopausal women",
"author": "Chubak",
"doi-asserted-by": "crossref",
"issue": "11",
"journal-title": "Am. J. Med.",
"key": "10.1016/j.jbmt.2021.07.012_bib13",
"volume": "119",
"year": "2006"
},
{
"key": "10.1016/j.jbmt.2021.07.012_bib14",
"unstructured": "COVID-19 Tedavi. (n.d.). Retrieved July 11, 2020, from https://covid19bilgi.saglik.gov.tr/tr/tedavi."
},
{
"DOI": "10.1016/j.physbeh.2006.10.001",
"article-title": "Emotional & electroencephalographic responses during affective picture viewing after exercise ☆",
"author": "Crabbe",
"doi-asserted-by": "crossref",
"first-page": "394",
"journal-title": "Physiol. Behav.",
"key": "10.1016/j.jbmt.2021.07.012_bib15",
"volume": "90",
"year": "2007"
},
{
"DOI": "10.3390/sports6030084",
"article-title": "Validity, reliability, and application of the session-RPE method for quantifying training loads during high intensity functional training",
"author": "Crawford",
"doi-asserted-by": "crossref",
"first-page": "84",
"issue": "3",
"journal-title": "Sports",
"key": "10.1016/j.jbmt.2021.07.012_bib16",
"volume": "6",
"year": "2018"
},
{
"DOI": "10.1111/j.1365-2249.2009.03952.x",
"article-title": "Lung disease, antibodies and other unresolved issues in immune globulin therapy for antibody deficiency",
"author": "Cunningham-Rundles",
"doi-asserted-by": "crossref",
"first-page": "12",
"issue": "Suppl. 1",
"journal-title": "Clin. Exp. Immunol.",
"key": "10.1016/j.jbmt.2021.07.012_bib17",
"volume": "157",
"year": "2009"
},
{
"DOI": "10.1152/japplphysiol.00077.2015",
"article-title": "Circulating inflammatory miRNA signature in response to different doses of aerobic exercise",
"author": "De Gonzalo-Calvo",
"doi-asserted-by": "crossref",
"first-page": "124",
"issue": "2",
"journal-title": "J. Appl. Physiol.",
"key": "10.1016/j.jbmt.2021.07.012_bib18",
"volume": "119",
"year": "2015"
},
{
"DOI": "10.1016/0147-9571(93)90058-D",
"article-title": "Effect of physical exercise on the phagocytic function of peritoneal macrophages from Swiss mice",
"author": "De la Fuente",
"doi-asserted-by": "crossref",
"first-page": "29",
"issue": "1",
"journal-title": "Comp. Immunol. Microbiol. Infect. Dis.",
"key": "10.1016/j.jbmt.2021.07.012_bib19",
"volume": "16",
"year": "1993"
},
{
"article-title": "Effects of high-intensity interval and moderate-intensity continuous exercise on inflammatory, leptin, IgA, and lipid peroxidation responses in obese males",
"author": "de Souza",
"first-page": "1",
"issue": "MAY",
"journal-title": "Front. Physiol.",
"key": "10.1016/j.jbmt.2021.07.012_bib20",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.3390/ijerph17082690",
"article-title": "Coronavirus diseases (COVID-19) current status and future perspectives: a narrative review",
"author": "Di Gennaro",
"doi-asserted-by": "crossref",
"issue": "8",
"journal-title": "Int. J. Environ.Res. Public Health",
"key": "10.1016/j.jbmt.2021.07.012_bib21",
"volume": "17",
"year": "2020"
},
{
"article-title": "Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19)",
"author": "Diao",
"first-page": "1",
"issue": "May",
"journal-title": "Front. Immunol.",
"key": "10.1016/j.jbmt.2021.07.012_bib22",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.mehy.2020.109854",
"article-title": "Can moderate intensity aerobic exercise be an effective and valuable therapy in preventing and controlling the pandemic of COVID-19?",
"author": "Dixit",
"doi-asserted-by": "crossref",
"first-page": "109854",
"journal-title": "Med. Hypotheses",
"key": "10.1016/j.jbmt.2021.07.012_bib23",
"volume": "143",
"year": "2020"
},
{
"DOI": "10.2217/fvl-2020-0050",
"article-title": "Comparison of the COVID-2019 (SARS-CoV-2) pathogenesis with SARS-CoV and MERS-CoV infections",
"author": "Fani",
"doi-asserted-by": "crossref",
"journal-title": "Future Virol.",
"key": "10.1016/j.jbmt.2021.07.012_bib24",
"year": "2020"
},
{
"article-title": "The effect of tapering period on plasma pro-inflammatory cytokine levels and performance in elite male cyclists",
"author": "Farhangimaleki",
"issue": "4",
"journal-title": "J. Sports Sci. Med.",
"key": "10.1016/j.jbmt.2021.07.012_bib25",
"volume": "8",
"year": "2009"
},
{
"DOI": "10.3758/BF03193146",
"article-title": "G∗Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences",
"author": "Faul",
"doi-asserted-by": "crossref",
"first-page": "175",
"issue": "2",
"journal-title": "Behav. Res. Methods",
"key": "10.1016/j.jbmt.2021.07.012_bib26",
"volume": "39",
"year": "2007"
},
{
"article-title": "Effect of acute and chronic aerobic exercise on immunological markers: a systematic review",
"author": "Gonçalves",
"first-page": "1",
"issue": "January",
"journal-title": "Front. Physiol.",
"key": "10.1016/j.jbmt.2021.07.012_bib27",
"volume": "10",
"year": "2020"
},
{
"article-title": "Clinical characteristics of coronavirus disease 2019 in China",
"author": "Guan",
"first-page": "1",
"journal-title": "New Engl. J. Med.",
"key": "10.1016/j.jbmt.2021.07.012_bib28",
"year": "2020"
},
{
"DOI": "10.1111/j.1939-1676.1996.tb02063.x",
"article-title": "Exercise and immunity: a review with emphasis on the horse",
"author": "Hines",
"doi-asserted-by": "crossref",
"first-page": "280",
"issue": "10",
"journal-title": "J. Vet. Intern. Med.",
"key": "10.1016/j.jbmt.2021.07.012_bib29",
"volume": "10",
"year": "1996"
},
{
"author": "Hogan",
"key": "10.1016/j.jbmt.2021.07.012_bib30"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "10.1016/j.jbmt.2021.07.012_bib31",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.4103/0974-7788.59946",
"article-title": "Sample size calculation",
"author": "Kadam",
"doi-asserted-by": "crossref",
"first-page": "55",
"issue": "1",
"journal-title": "Int. J. Ayurveda Res.",
"key": "10.1016/j.jbmt.2021.07.012_bib32",
"volume": "1",
"year": "2010"
},
{
"DOI": "10.1097/HJR.0b013e3282efaf50",
"article-title": "The anti-inflammatory effects of exercise training in patients with type 2 diabetes mellitus",
"author": "Kadoglou",
"doi-asserted-by": "crossref",
"first-page": "837",
"issue": "6",
"journal-title": "Eur. J. Prevent. Cardiol.",
"key": "10.1016/j.jbmt.2021.07.012_bib33",
"volume": "14",
"year": "2007"
},
{
"DOI": "10.1007/s00421-007-0529-1",
"article-title": "Alterations of immunoendocrine responses during the recovery period after acute prolonged cycling",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "539",
"issue": "5",
"journal-title": "Eur. J. Appl. Physiol.",
"key": "10.1016/j.jbmt.2021.07.012_bib34",
"volume": "101",
"year": "2007"
},
{
"article-title": "Acute variation of leucocytes counts following a half-marathon run",
"author": "Lippi",
"first-page": "117",
"issue": "1",
"journal-title": "Int. J. Lit. Humanit.",
"key": "10.1016/j.jbmt.2021.07.012_bib35",
"volume": "32",
"year": "2010"
},
{
"DOI": "10.1371/journal.pone.0112892",
"article-title": "Mean platelet volume (MPV) predicts middle distance running performance",
"author": "Lippi",
"doi-asserted-by": "crossref",
"first-page": "8",
"issue": "11",
"journal-title": "PLoS One",
"key": "10.1016/j.jbmt.2021.07.012_bib36",
"volume": "9",
"year": "2014"
},
{
"DOI": "10.3389/fphys.2017.00856",
"article-title": "Short-term high- and moderate-intensity training modifies inflammatory and metabolic factors in response to acute exercise",
"author": "Lira",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Front. Physiol.",
"key": "10.1016/j.jbmt.2021.07.012_bib37",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.1002/jmv.25678",
"article-title": "Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle",
"author": "Lu",
"doi-asserted-by": "crossref",
"first-page": "401",
"issue": "4",
"journal-title": "J. Med. Virol.",
"key": "10.1016/j.jbmt.2021.07.012_bib38",
"volume": "92",
"year": "2020"
},
{
"article-title": "Important role of relaxation techniques on immune functions, glycemic control, and stress in diabetic patients with COVID-19: a review",
"author": "Mahmoud Mohamed",
"journal-title": "Curr. Diabetes Rev.",
"key": "10.1016/j.jbmt.2021.07.012_bib39",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1152/japplphysiol.01538.2011",
"article-title": "Extensive inflammatory cell infiltration in human skeletal muscle in response to an ultraendurance exercise bout in experienced athletes",
"author": "Marklund",
"doi-asserted-by": "crossref",
"first-page": "66",
"issue": "1",
"journal-title": "J. Appl. Physiol.",
"key": "10.1016/j.jbmt.2021.07.012_bib40",
"volume": "114",
"year": "2013"
},
{
"DOI": "10.1016/j.iac.2010.09.013",
"article-title": "The adverse effects of psychological stress on immunoregulatory balance: applications to human inflammatory diseases",
"author": "Marshall",
"doi-asserted-by": "crossref",
"first-page": "133",
"issue": "1",
"journal-title": "Immunol. Allergy Clin.",
"key": "10.1016/j.jbmt.2021.07.012_bib41",
"volume": "31",
"year": "2011"
},
{
"DOI": "10.1055/s-0029-1237389",
"article-title": "Effects of aerobic conditioning on salivary IgA and plasma IgA, IgG and IgM in older men and women",
"author": "Martins",
"doi-asserted-by": "crossref",
"first-page": "906",
"issue": "12",
"journal-title": "Int. J. Sports Med.",
"key": "10.1016/j.jbmt.2021.07.012_bib42",
"volume": "30",
"year": "2009"
},
{
"DOI": "10.1097/00005768-200208000-00003",
"article-title": "Moderate to vigorous physical activity and risk of upper-respiratory tract infection",
"author": "Matthews",
"doi-asserted-by": "crossref",
"first-page": "1242",
"issue": "8",
"journal-title": "Med. Sci. Sports Exerc.",
"key": "10.1016/j.jbmt.2021.07.012_bib43",
"volume": "34",
"year": "2002"
},
{
"article-title": "Physical therapy recommendations for patients with COVID-19",
"author": "Mohamed",
"first-page": "169",
"key": "10.1016/j.jbmt.2021.07.012_bib44",
"series-title": "AI-powered IoT for COVID-19",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.04.038",
"article-title": "Role of increasing the aerobic capacity on improving the function of immune and respiratory systems in patients with coronavirus (COVID-19): a review",
"author": "Mohamed",
"doi-asserted-by": "crossref",
"first-page": "489",
"issue": "4",
"journal-title": "Diabetes Metab. Syndrome: Clin. Res. Rev.",
"key": "10.1016/j.jbmt.2021.07.012_bib45",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.12998/wjcc.v9.i19.4939",
"article-title": "Enhancing oxygenation of patients with coronavirus disease 2019: effects on immunity and other health-related conditions",
"author": "Mohamed",
"doi-asserted-by": "crossref",
"first-page": "4939",
"issue": "19",
"journal-title": "World J. Clin. Cases",
"key": "10.1016/j.jbmt.2021.07.012_bib46",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.4103/1110-6611.188023",
"article-title": "Comparison between the effects of aerobic and resistive training on immunoglobulins in obese women",
"author": "Mohamed",
"doi-asserted-by": "crossref",
"first-page": "11",
"issue": "1",
"journal-title": "Bull. Facul. Phys. Ther.",
"key": "10.1016/j.jbmt.2021.07.012_bib47",
"volume": "21",
"year": "2016"
},
{
"DOI": "10.2165/00007256-200131020-00004",
"article-title": "The cytokine response to physical activity and training",
"author": "Moldoveanu",
"doi-asserted-by": "crossref",
"first-page": "115",
"issue": "2",
"journal-title": "Sports Med.",
"key": "10.1016/j.jbmt.2021.07.012_bib48",
"volume": "31",
"year": "2001"
},
{
"DOI": "10.1152/ajpregu.00274.2004",
"article-title": "Role of lung macrophages on susceptibility to respiratory infection following short-term moderate exercise training",
"author": "Murphy",
"doi-asserted-by": "crossref",
"first-page": "R1354",
"issue": "6",
"journal-title": "Am. J. Physiol. Regul. Integr. Comp. Physiol.",
"key": "10.1016/j.jbmt.2021.07.012_bib49",
"volume": "287",
"year": "2004"
},
{
"DOI": "10.1093/eurpub/cki159",
"article-title": "Effects of physical exercise on depression, neuroendocrine stress hormones and physiological fitness in adolescent females with depressive symptoms",
"author": "Nabkasorn",
"doi-asserted-by": "crossref",
"first-page": "179",
"issue": "2",
"journal-title": "Eur. J. Publ. Health",
"key": "10.1016/j.jbmt.2021.07.012_bib50",
"volume": "16",
"year": "2006"
},
{
"DOI": "10.1590/S1516-31802003000100003",
"article-title": "Effects of three different types of exercise on blood leukocyte count during and following exercise",
"author": "Natale",
"doi-asserted-by": "crossref",
"first-page": "9",
"issue": "1",
"journal-title": "Sao Paulo Med. J.",
"key": "10.1016/j.jbmt.2021.07.012_bib51",
"volume": "121",
"year": "2003"
},
{
"article-title": "The immune response to exercise",
"author": "Nieman",
"first-page": "166",
"issue": "2",
"journal-title": "Semin. Hematol.",
"key": "10.1016/j.jbmt.2021.07.012_bib52",
"volume": "vol. 31",
"year": "1994"
},
{
"DOI": "10.1055/s-2007-1024839",
"article-title": "The effects of moderate exercise training on natural killer cells and acute upper respiratory tract infections",
"author": "Nieman",
"doi-asserted-by": "crossref",
"first-page": "467",
"issue": "6",
"journal-title": "Int. J. Sports Med.",
"key": "10.1016/j.jbmt.2021.07.012_bib53",
"volume": "11",
"year": "1990"
},
{
"DOI": "10.1161/01.ATV.0000140199.14930.32",
"article-title": "Can exercise training with weight loss lower serum C-reactive protein levels?",
"author": "Okita",
"doi-asserted-by": "crossref",
"first-page": "1868",
"issue": "10",
"journal-title": "Arterioscler. Thromb. Vasc. Biol.",
"key": "10.1016/j.jbmt.2021.07.012_bib54",
"volume": "24",
"year": "2004"
},
{
"DOI": "10.1055/s-2007-1024746",
"article-title": "Influence of physical activity on the cellular immune system: mechanisms of action",
"author": "Pedersen",
"doi-asserted-by": "crossref",
"first-page": "S23",
"issue": "S 1",
"journal-title": "Int. J. Sports Med.",
"key": "10.1016/j.jbmt.2021.07.012_bib55",
"volume": "12",
"year": "1991"
},
{
"DOI": "10.1152/physrev.2000.80.3.1055",
"article-title": "Exercise and the immune system: regulation, integration, and adaptation",
"author": "Pedersen",
"doi-asserted-by": "crossref",
"first-page": "1055",
"issue": "3",
"journal-title": "Physiol. Rev.",
"key": "10.1016/j.jbmt.2021.07.012_bib56",
"volume": "80",
"year": "2000"
},
{
"DOI": "10.1016/j.psychsport.2009.05.009",
"article-title": "The effect of regular aerobic exercise on positive-activated affect: a meta-analysis",
"author": "Reed",
"doi-asserted-by": "crossref",
"first-page": "581",
"issue": "6",
"journal-title": "Psychol. Sport Exerc.",
"key": "10.1016/j.jbmt.2021.07.012_bib57",
"volume": "10",
"year": "2009"
},
{
"DOI": "10.1055/s-2001-11347",
"article-title": "The effect of moderate aerobic exercise and relaxation on secretory immunoglobulin A",
"author": "Reid",
"doi-asserted-by": "crossref",
"first-page": "132",
"issue": "2",
"journal-title": "Int. J. Sports Med.",
"key": "10.1016/j.jbmt.2021.07.012_bib58",
"volume": "22",
"year": "2001"
},
{
"DOI": "10.1186/cc11807",
"article-title": "Protective effects of aerobic exercise on acute lung injury induced by LPS in mice",
"author": "Reis Gonçalves",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "Crit. Care",
"key": "10.1016/j.jbmt.2021.07.012_bib59",
"volume": "16",
"year": "2012"
},
{
"DOI": "10.1186/1471-2288-12-81",
"article-title": "To test or not to test: preliminary assessment of normality when comparing two independent samples",
"author": "Rochon",
"doi-asserted-by": "crossref",
"first-page": "81",
"journal-title": "BMC Med. Res. Methodol.",
"key": "10.1016/j.jbmt.2021.07.012_bib60",
"volume": "12",
"year": "2012"
},
{
"DOI": "10.1016/j.vaccine.2004.11.032",
"article-title": "Role of IgA in the defense against respiratory infections: IgA deficient mice exhibited increased susceptibility to intranasal infection with Mycobacterium bovis BCG",
"author": "Rodríguez",
"doi-asserted-by": "crossref",
"first-page": "2565",
"issue": "20",
"journal-title": "Vaccine",
"key": "10.1016/j.jbmt.2021.07.012_bib61",
"volume": "23",
"year": "2005"
},
{
"DOI": "10.1519/JSC.0b013e3181fc5e67",
"article-title": "Monocyte and T-CELL responses to exercise training in elderly subjects",
"author": "Shimizu",
"doi-asserted-by": "crossref",
"first-page": "2565",
"issue": "9",
"journal-title": "J. Strength Condit Res.",
"key": "10.1016/j.jbmt.2021.07.012_bib62",
"volume": "25",
"year": "2011"
},
{
"DOI": "10.1152/ajpcell.2001.281.3.C1001",
"article-title": "Plasma interleukin-6 during strenuous exercise: role of epinephrine",
"author": "Steensberg",
"doi-asserted-by": "crossref",
"first-page": "1001",
"issue": "3 50–3",
"journal-title": "Am. J. Physiol. Cell Physiol.",
"key": "10.1016/j.jbmt.2021.07.012_bib63",
"volume": "281",
"year": "2001"
},
{
"DOI": "10.1152/jappl.2001.90.3.789",
"article-title": "Effects of different durations of exercise on macrophage functions in mice",
"author": "Sugiura",
"doi-asserted-by": "crossref",
"first-page": "789",
"issue": "3",
"journal-title": "J. Appl. Physiol.",
"key": "10.1016/j.jbmt.2021.07.012_bib64",
"volume": "90",
"year": "2001"
},
{
"DOI": "10.1016/j.jmpt.2010.01.005",
"article-title": "Altered central integration of dual somatosensory input after cervical spine manipulation",
"author": "Taylor",
"doi-asserted-by": "crossref",
"first-page": "178",
"issue": "3",
"journal-title": "J. Manipulative Physiol. Therapeut.",
"key": "10.1016/j.jbmt.2021.07.012_bib65",
"volume": "33",
"year": "2010"
},
{
"DOI": "10.1093/occmed/kqx063",
"doi-asserted-by": "crossref",
"key": "10.1016/j.jbmt.2021.07.012_bib66",
"unstructured": "xertion (RPE) scale. (2017). https://doi.org/10.1093/occmed/kqx063."
},
{
"key": "10.1016/j.jbmt.2021.07.012_bib67",
"unstructured": "The Wisconsin Upper Respiratory Symptom Survey (WURSS): a new research instrument for assessing the common cold - PubMed. (n.d.). Retrieved July 15, 2020, from https://pubmed.ncbi.nlm.nih.gov/11978238/."
},
{
"key": "10.1016/j.jbmt.2021.07.012_bib68",
"unstructured": "The Wisconsin Upper Respiratory Symptom Survey is responsive, reliable, and valid. (n.d.). Retrieved July 15, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7119015/."
},
{
"DOI": "10.1183/09031936.00003411",
"article-title": "Aerobic exercise attenuates pulmonary injury induced by exposure to cigarette smoke",
"author": "Toledo",
"doi-asserted-by": "crossref",
"first-page": "254",
"issue": "2",
"journal-title": "Eur. Respir. J.",
"key": "10.1016/j.jbmt.2021.07.012_bib69",
"volume": "39",
"year": "2012"
},
{
"DOI": "10.1055/s-2007-1021028",
"article-title": "Evidence that the effect of bicycle exercise on blood mononuclear cell proliferative responses and subsets is mediated by epinephrine",
"author": "Tvede",
"doi-asserted-by": "crossref",
"first-page": "100",
"issue": "2",
"journal-title": "Int. J. Sports Med.",
"key": "10.1016/j.jbmt.2021.07.012_bib70",
"volume": "15",
"year": "1994"
},
{
"DOI": "10.1681/ASN.2013070702",
"article-title": "Evidence for anti-inflammatory effects of exercise in CKD",
"author": "Viana",
"doi-asserted-by": "crossref",
"first-page": "2121",
"issue": "9",
"journal-title": "J. Am. Soc. Nephrol.",
"key": "10.1016/j.jbmt.2021.07.012_bib71",
"volume": "25",
"year": "2014"
},
{
"author": "WHO",
"key": "10.1016/j.jbmt.2021.07.012_bib72",
"series-title": "Considerations for Quarantine of Individuals in the Context of Containment for Coronavirus Disease ( COVID-19 )",
"year": "2020"
},
{
"author": "WHO",
"key": "10.1016/j.jbmt.2021.07.012_bib73",
"series-title": "Rational Use of Personal Protective Equipment for Coronavirus Disease 2019 (COVID-19) and Considerations during Severe Shortages",
"year": "2020"
},
{
"key": "10.1016/j.jbmt.2021.07.012_bib74",
"unstructured": "WHO coronavirus disease (COVID-19) Dashboard. (n.d.). Retrieved June 21, 2020, from https://covid19.who.int/."
},
{
"key": "10.1016/j.jbmt.2021.07.012_bib75",
"unstructured": "WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. (n.d.). Retrieved June 28, 2020, from https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020."
},
{
"DOI": "10.1080/00243639.2017.1360065",
"article-title": "Hormonal contraception and the development of autoimmunity: a review of the literature",
"author": "Williams",
"doi-asserted-by": "crossref",
"first-page": "275",
"issue": "3",
"journal-title": "Linacre Q.",
"key": "10.1016/j.jbmt.2021.07.012_bib76",
"volume": "84",
"year": "2017"
},
{
"key": "10.1016/j.jbmt.2021.07.012_bib77",
"unstructured": "World Health Organization. Corona- Virus Disease (COVID-19) Outbreak. [cited 15 January 2021]. Available from: https://covid19.who.int/."
},
{
"article-title": "Macrophages and other nonspecific defenses: role in modulating resistance against herpes simplex virus",
"author": "Wu",
"first-page": "89",
"journal-title": "Curr. Top. Microbiol. Immunol.",
"key": "10.1016/j.jbmt.2021.07.012_bib78",
"volume": "179",
"year": "1992"
},
{
"DOI": "10.1016/j.jinf.2020.04.012",
"article-title": "Suppressed T cell-mediated immunity in patients with COVID-19: a clinical retrospective study in Wuhan, China",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "e51",
"issue": "1",
"journal-title": "J. Infect.",
"key": "10.1016/j.jbmt.2021.07.012_bib79",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1016/j.clim.2020.108427",
"article-title": "COVID-19 pathophysiology: a review",
"author": "Yuki",
"doi-asserted-by": "crossref",
"first-page": "108427",
"journal-title": "Clin. Immunol.",
"key": "10.1016/j.jbmt.2021.07.012_bib80",
"volume": "215",
"year": "2020"
},
{
"DOI": "10.3389/fnagi.2019.00098",
"article-title": "Effect of aerobic exercise on inflammatory markers in healthy middle-aged and older adults: a systematic review and meta-analysis of randomized controlled trials",
"author": "Zheng",
"doi-asserted-by": "crossref",
"first-page": "98",
"issue": "APR",
"journal-title": "Front. Aging Neurosci.",
"key": "10.1016/j.jbmt.2021.07.012_bib81",
"volume": "11",
"year": "2019"
},
{
"DOI": "10.12998/wjcc.v8.i12.2655",
"article-title": "Low-grade fever during COVID-19 convalescence: a report of 3 cases",
"author": "Zhuang",
"doi-asserted-by": "crossref",
"first-page": "2655",
"issue": "12",
"journal-title": "World J. Clin. Cases",
"key": "10.1016/j.jbmt.2021.07.012_bib82",
"volume": "8",
"year": "2020"
}
],
"reference-count": 82,
"references-count": 82,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S1360859221001674"
}
},
"score": 1,
"short-container-title": [
"Journal of Bodywork and Movement Therapies"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Complementary and alternative medicine",
"Rehabilitation",
"Physical Therapy, Sports Therapy and Rehabilitation",
"Complementary and Manual Therapy"
],
"subtitle": [],
"title": [
"The effect of aerobic exercise on immune biomarkers and symptoms severity and progression in patients with COVID-19: A randomized control trial"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "28"
}
