The role of serum vitamin D concentrations in predicting COVID-19 course and outcome
et al., Acta Facultatis Medicae Naissensis, doi:10.5937/afmnai41-42961, Jun 2024
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of 329 hospitalized COVID-19 patients in Serbia showing vitamin D deficiency associated with significantly higher mortality.
This is the 200th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
|
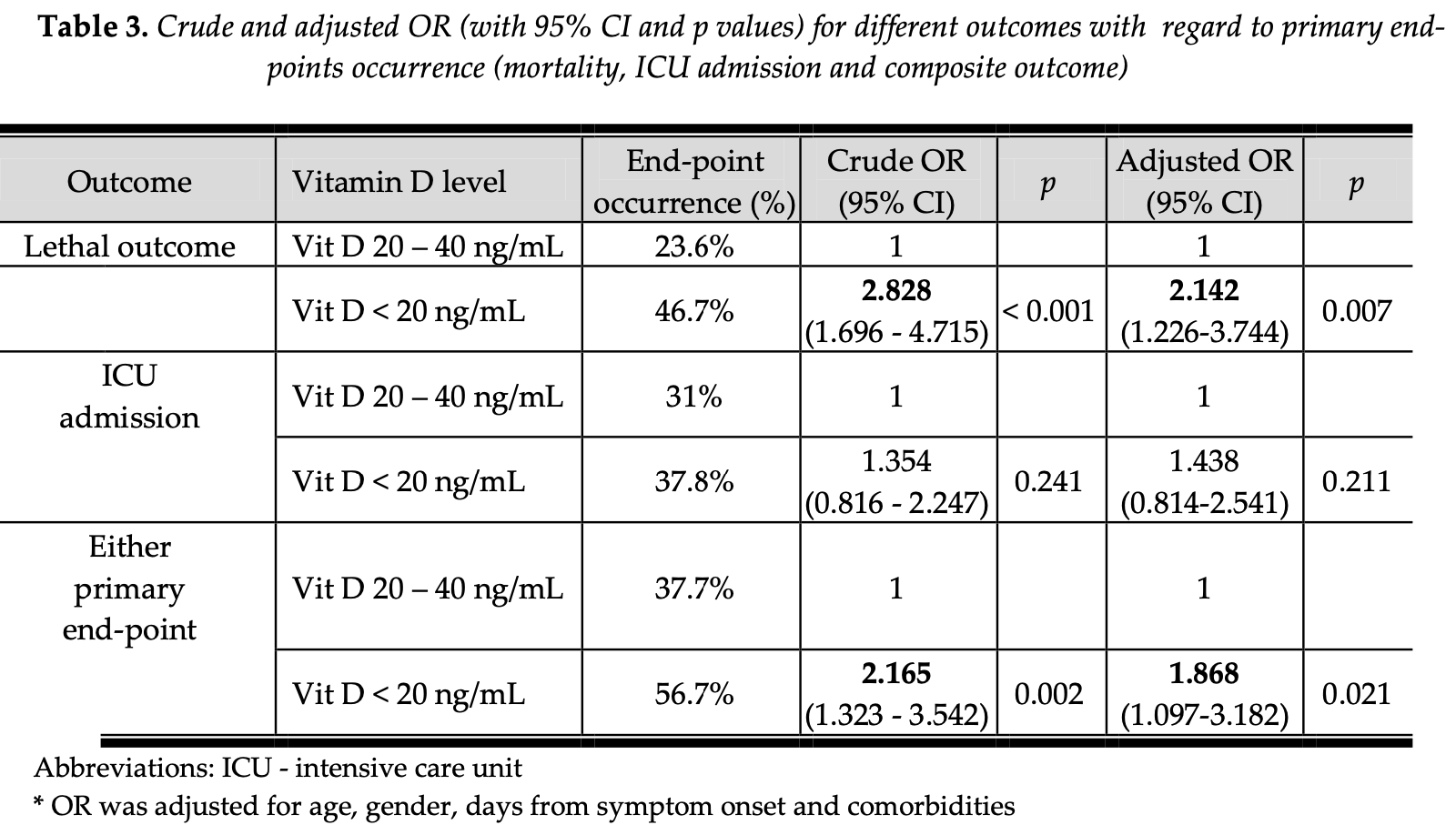
risk of death, 53.3% lower, OR 0.47, p = 0.007, cutoff 20ng/mL, adjusted per study, inverted to make OR<1 favor high D levels (≥20ng/mL), multivariable, RR approximated with OR.
|
|
risk of ICU admission, 30.5% lower, OR 0.70, p = 0.21, cutoff 20ng/mL, adjusted per study, inverted to make OR<1 favor high D levels (≥20ng/mL), multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Božić et al., 20 Jun 2024, prospective, Serbia, peer-reviewed, median age 69.0, 4 authors, study period October 2021 - December 2021.
Contact: djordje.stevanovic.kg@gmail.com.
The Role of Serum Vitamin D Concentrations in Predicting COVID-19 Course and Outcome
Introduction/Aim. The coronavirus disease 2019 (COVID-19) pandemic had significant acute and longterm impact on people's health. As the available literature sources have shown that the premorbid conditions affect the course of COVID-19, we aimed to investigate the role of admission vitamin D concentration to predict the outcome of hospitalized COVID-19 patients. Methods. An observational, prospective cohort study was conducted on 329 COVID-19 patients hospitalized at the University Clinical Centre Kragujevac, between October and December 2021. Within 24 hours of admission, vitamin D level was measured from the peripheral venous blood. Medical history data and socio-demographic characteristics were obtained anamnestically and using Health Information System (COMTRADE, Serbia). Lethal outcome and intensive care unit (ICU) admission were considered primary end-points. Results. The prevalence of hypovitaminosis D on admission in our cohort was 27.7%. Both non-survivors and patients requiring ICU admission more frequently had hypovitaminosis D compared to survivors (42,9% versus 21,0%; p < 0,001) and patients on a standard level of care (31,5% verus 25,3%; p = 0,029). Our research showed that vitamin D concentration < 20 ng/mL was an independent predictor of mortality (aOR 2.142 [95% CI 1.226 -3.744]). However, hypovitaminosis D upon hospital admission did not show a significant impact on ICU admission. Conclusion. Low vitamin D concentration on admission could be a significant predictor of outcome in hospitalized COVID-19 patients.
References
Bilezikian, Bikle, Hewison, MECHANISMS IN ENDOCRINOLOGY: Vitamin D and COVID-19, Eur J Endocrinol, doi:10.1530/EJE-20-0665
Borsche, Glauner, Mendel, COVID-19 Mortality Risk Correlates Inversely with Vitamin D3 Status, and a Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 ng/mL 25(OH)D3: Results of a Systematic Review and Meta-Analysis, Nutrients, doi:10.3390/nu13103596
Charoenngam, Holick, Immunologic Effects of Vitamin D on Human Health and Disease, Nutrients, doi:10.3390/nu12072097
Chen, Mei, Xie, Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: a meta-analysis and GRADE assessment of cohort studies and RCTs, Nutr J, doi:10.1186/s12937-021-00744-y
Chiodini, Gatti, Soranna, Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes, Front Public Health, doi:10.3389/fpubh.2021.736665
Djaharuddin, Munawwarah, Nurulita, Comorbidities and mortality in COVID-19 patients, Gac Sanit, doi:10.1016/j.gaceta.2021.10.085
Gallo Marin, Aghagoli, Lavine, Predictors of COVID-19 severity: A literature review, Rev Med Virol, doi:10.1002/rmv.2146
Kaya, Pamukçu, Yakar, The role of vitamin D deficiency on COVID-19: a systematic review and meta-analysis of observational studies, Epidemiol Health, doi:10.4178/epih.e2021074
Mercola, Grant, Wagner, Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity, Nutrients, doi:10.3390/nu12113361
Name, Souza, Vasconcelos, Zinc, Vitamin D and Vitamin C: Perspectives for COVID-19 With a Focus on Physical Tissue Barrier Integrity, Front Nutr, doi:10.3389/fnut.2020.606398
Petrelli, Luciani, Perego, Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2021.105883
Shi, Liu, Zhang, Severe Type of COVID-19: Pathogenesis, Warning Indicators and Treatment, Chin J Integr Med, doi:10.1007/s11655-021-3313-x
Teshome, Adane, Girma, Mekonnen, The Impact of Vitamin D Level on COVID-19 Infection: Systematic Review and Meta-Analysis, Front Public Health, doi:10.3389/fpubh.2021.624559
Zappulo, Cappuccilli, Cingolani, Vitamin D and the Kidney: Two Players, One Console, Int J Mol Sci, doi:10.3390/ijms23169135
DOI record:
{
"DOI": "10.5937/afmnai41-42961",
"ISSN": [
"0351-6083",
"2217-2521"
],
"URL": "http://dx.doi.org/10.5937/afmnai41-42961",
"abstract": "<jats:p>Introduction/Aim. The coronavirus disease 2019 (COVID-19) pandemic had significant acute and long-term impact on people's health. As the available literature sources have shown that the premorbid conditions affect the course of COVID-19, we aimed to investigate the role of admission vitamin D concentration to predict the outcome of hospitalized COVID-19 patients. Methods. An observational, prospective cohort study was conducted on 329 COVID-19 patients hospitalized at the University Clinical Centre Kragujevac, between October and December 2021. Within 24 hours of admission, vitamin D level was measured from the peripheral venous blood. Medical history data and socio-demographic characteristics were obtained anamnestically and using Health Information System (COMTRADE, Serbia). Lethal outcome and intensive care unit (ICU) admission were considered primary end-points. Results. The prevalence of hypovitaminosis D on admission in our cohort was 27.7%. Both non-survivors and patients requiring ICU admission more frequently had hypovitaminosis D compared to survivors (42,9% versus 21,0%; p < 0,001) and patients on a standard level of care (31,5% verus 25,3%; p = 0,029). Our research showed that vitamin D concentration < 20 ng/mL was an independent predictor of mortality (aOR 2.142 [95% CI 1.226 - 3.744]). However, hypovitaminosis D upon hospital admission did not show a significant impact on ICU admission. Conclusion. Low vitamin D concentration on admission could be a significant predictor of outcome in hospitalized COVID-19 patients.</jats:p>",
"author": [
{
"affiliation": [
{
"id": [
{
"asserted-by": "publisher",
"id": "https://ror.org/054nax084",
"id-type": "ROR"
}
]
}
],
"family": "Božić",
"given": "Dunja",
"sequence": "first"
},
{
"affiliation": [
{
"id": [
{
"asserted-by": "publisher",
"id": "https://ror.org/054nax084",
"id-type": "ROR"
}
]
}
],
"family": "Stevanović",
"given": "Đorđe",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1770-3733",
"affiliation": [
{
"id": [
{
"asserted-by": "publisher",
"id": "https://ror.org/054nax084",
"id-type": "ROR"
}
]
}
],
"authenticated-orcid": false,
"family": "Poskurica",
"given": "Mina",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7646-5144",
"affiliation": [
{
"id": [
{
"asserted-by": "publisher",
"id": "https://ror.org/054nax084",
"id-type": "ROR"
}
]
}
],
"authenticated-orcid": false,
"family": "Petrović",
"given": "Marina",
"sequence": "additional"
}
],
"container-title": "Acta Facultatis Medicae Naissensis",
"container-title-short": "Acta fac medic Naissensis",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
7,
9
]
],
"date-time": "2024-07-09T15:15:31Z",
"timestamp": 1720538131000
},
"deposited": {
"date-parts": [
[
2024,
7,
9
]
],
"date-time": "2024-07-09T15:16:13Z",
"timestamp": 1720538173000
},
"indexed": {
"date-parts": [
[
2024,
7,
10
]
],
"date-time": "2024-07-10T00:02:40Z",
"timestamp": 1720569760288
},
"is-referenced-by-count": 0,
"issue": "2",
"issued": {
"date-parts": [
[
2024
]
]
},
"journal-issue": {
"issue": "2",
"published-print": {
"date-parts": [
[
2024
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/BY-NC-ND/4.0",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
1,
1
]
],
"date-time": "2024-01-01T00:00:00Z",
"timestamp": 1704067200000
}
}
],
"link": [
{
"URL": "https://scindeks-clanci.ceon.rs/data/pdf/0351-6083/2024/0351-60832402244B.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "3964",
"original-title": [
"Uloga serumske koncentracije vitamina D u predikciji toka i ishoda COVID-19 infekcije"
],
"page": "244-251",
"prefix": "10.5937",
"published": {
"date-parts": [
[
2024
]
]
},
"published-print": {
"date-parts": [
[
2024
]
]
},
"publisher": "Centre for Evaluation in Education and Science (CEON/CEES)",
"reference": [
{
"DOI": "10.1007/s11655-021-3313-x",
"doi-asserted-by": "crossref",
"key": "ref1",
"unstructured": "Shi K, Liu Y, Zhang Q, et al. Severe Type of COVID-19: Pathogenesis, Warning Indicators and Treatment. Chin J Integr Med. 2022;28(1):3-11. https://doi.org/10.1007/s11655-021-3313-x;"
},
{
"DOI": "10.3389/fpubh.2021.736665",
"doi-asserted-by": "crossref",
"key": "ref2",
"unstructured": "Chiodini I, Gatti D, Soranna D, et al. Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes. Front Public Health. 2021;9:736665. https://doi.org/10.3389/fpubh.2021.736665;"
},
{
"key": "ref3",
"unstructured": "World Health Organisation. COVID-19 Clinical Management: Living Guidance. 2021. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1 (accessed on 25 January 2023) https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2;"
},
{
"DOI": "10.1530/EJE-20-0665",
"doi-asserted-by": "crossref",
"key": "ref4",
"unstructured": "Bilezikian JP, Bikle D, Hewison M, et al. MECHANISMS IN ENDOCRINOLOGY: Vitamin D and COVID-19. Eur J Endocrinol. 2020;183(5):R133-R147. https://doi.org/10.1530/EJE-20-0665;"
},
{
"DOI": "10.3390/nu12113361",
"doi-asserted-by": "crossref",
"key": "ref5",
"unstructured": "Mercola J, Grant WB, Wagner CL. Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity. Nutrients. 2020;12(11):3361. https://doi.org/10.3390/nu12113361;"
},
{
"DOI": "10.3390/nu12072097",
"doi-asserted-by": "crossref",
"key": "ref6",
"unstructured": "Charoenngam N, Holick MF. Immunologic Effects of Vitamin D on Human Health and Disease. Nutrients. 2020 Jul 15;12(7):2097. https://doi.org/10.3390/nu12072097;"
},
{
"DOI": "10.1002/rmv.2146",
"doi-asserted-by": "crossref",
"key": "ref7",
"unstructured": "Gallo Marin B, Aghagoli G, Lavine K, et al. Predictors of COVID-19 severity: A literature review. Rev Med Virol. 2021;31(1):1-10. https://doi.org/10.1002/rmv.2146;"
},
{
"DOI": "10.1016/j.gaceta.2021.10.085",
"doi-asserted-by": "crossref",
"key": "ref8",
"unstructured": "Djaharuddin I, Munawwarah S, Nurulita A, et al. Comorbidities and mortality in COVID-19 patients. Gac Sanit. 2021;35 Suppl 2:S530-S532. https://doi.org/10.1016/j.gaceta.2021.10.085;"
},
{
"DOI": "10.3389/fnut.2020.606398",
"doi-asserted-by": "crossref",
"key": "ref9",
"unstructured": "Name JJ, Souza ACR, Vasconcelos AR, et al. Zinc, Vitamin D and Vitamin C: Perspectives for COVID-19 With a Focus on Physical Tissue Barrier Integrity. Front Nutr. 2020;7:606398. https://doi.org/10.3389/fnut.2020.606398;"
},
{
"DOI": "10.4178/epih.e2021074",
"doi-asserted-by": "crossref",
"key": "ref10",
"unstructured": "Kaya MO, Pamukçu E, Yakar B. The role of vitamin D deficiency on COVID-19: a systematic review and meta-analysis of observational studies. Epidemiol Health. 2021;43:e2021074. https://doi.org/10.4178/epih.e2021074;"
},
{
"DOI": "10.3389/fpubh.2021.624559",
"doi-asserted-by": "crossref",
"key": "ref11",
"unstructured": "Teshome A, Adane A, Girma B, Mekonnen ZA. The Impact of Vitamin D Level on COVID-19 Infection: Systematic Review and Meta-Analysis. Front Public Health. 2021;9:624559. https://doi.org/10.3389/fpubh.2021.624559;"
},
{
"DOI": "10.1186/s12937-021-00744-y",
"doi-asserted-by": "crossref",
"key": "ref12",
"unstructured": "Chen J, Mei K, Xie L, et al. Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: a meta-analysis and GRADE assessment of cohort studies and RCTs. Nutr J. 2021;20(1):89. https://doi.org/10.1186/s12937-021-00744-y;"
},
{
"DOI": "10.3390/nu13103596",
"doi-asserted-by": "crossref",
"key": "ref13",
"unstructured": "Borsche L, Glauner B, von Mendel J. COVID-19 Mortality Risk Correlates Inversely with Vitamin D3 Status, and a Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 ng/mL 25(OH)D3: Results of a Systematic Review and Meta-Analysis. Nutrients. 2021;13(10):3596. https://doi.org/10.3390/nu13103596;"
},
{
"DOI": "10.3390/ijms23169135",
"doi-asserted-by": "crossref",
"key": "ref14",
"unstructured": "Zappulo F, Cappuccilli M, Cingolani A, et al. Vitamin D and the Kidney: Two Players, One Console. Int J Mol Sci. 2022;23(16):9135. https://doi.org/10.3390/ijms23169135;"
},
{
"DOI": "10.1016/j.jsbmb.2021.105883",
"doi-asserted-by": "crossref",
"key": "ref15",
"unstructured": "Petrelli F, Luciani A, Perego G, et al. Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies. J Steroid Biochem Mol Biol. 2021;211:105883. https://doi.org/10.1016/j.jsbmb.2021.105883;"
}
],
"reference-count": 15,
"references-count": 15,
"relation": {},
"resource": {
"primary": {
"URL": "https://scindeks.ceon.rs/Article.aspx?artid=0351-60832402244B"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "The role of serum vitamin D concentrations in predicting COVID-19 course and outcome",
"type": "journal-article",
"volume": "41"
}
