Association between Vitamin D Status and Secondary Infections in Patients with Severe COVID-19 Admitted in the Intensive Care Unit of a Tertiary-Level Hospital in Turkey
et al., Diagnostics, doi:10.3390/diagnostics13010059, Dec 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
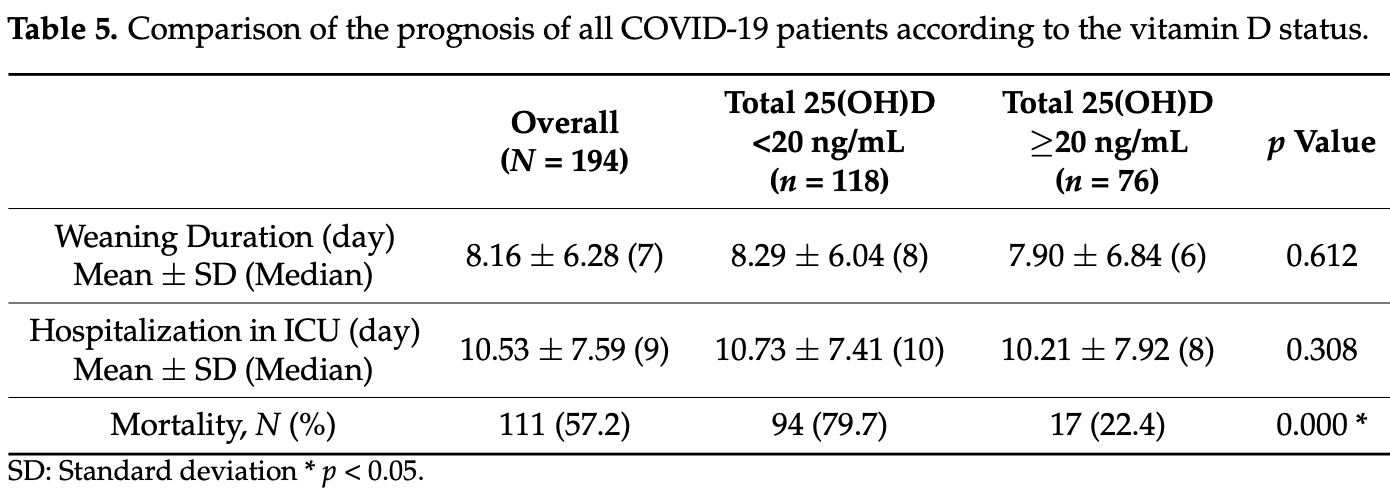
Retrospective 194 ICU patients and 30 non-COVID-19 patients in Turkey, showing significantly lower vitamin D levels in COVID-19 patients. There was significantly higher COVID-19 mortality with vitamin D deficiency, and significantly higher risk of secondary hospital infections.
Severe COVID-19 patients with vitamin D deficiency may have increased risks due to secondary infections.
This is the 154th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted differences between groups.
|
risk of death, 71.9% lower, RR 0.28, p < 0.001, high D levels (≥20ng/mL) 17 of 76 (22.4%), low D levels (<20ng/mL) 94 of 118 (79.7%), NNT 1.7.
|
|
secondary infection, 23.3% lower, RR 0.77, p = 0.03, high D levels (≥20ng/mL) 40 of 76 (52.6%), low D levels (<20ng/mL) 81 of 118 (68.6%), NNT 6.2, growth in culture.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Batur et al., 26 Dec 2022, retrospective, Turkey, peer-reviewed, 2 authors, study period March 2020 - June 2021.
Contact: lbatur@biruni.edu.tr (corresponding author).
Association between Vitamin D Status and Secondary Infections in Patients with Severe COVID-19 Admitted in the Intensive Care Unit of a Tertiary-Level Hospital in Turkey
Diagnostics, doi:10.3390/diagnostics13010059
There are several studies showing that the vitamin D status can determine risk of COVID-19 infections, severity and mortality from coronavirus disease 2019 . However, the association between vitamin D (25(OH)D) and secondary infections in the prognosis of COVID-19 patients has not been reported yet. The aim was to investigate whether the vitamin D status affects the rates of secondary infections in patients with severe COVID-19 hospitalized in the intensive care unit (ICU) of a tertiary-level hospital in Turkey. The data of 194 patients with diagnosis of severe COVID-19 who were admitted to the ICU from March 2020 to June 2021 and older than 18 years were evaluated in this retrospective study. The patients were divided into two groups according to total serum 25(OH)D level as normal group (≥20 ng/mL) and low group (<20 ng/mL). The 25(OH)D level was low in 118 (60.8%) and normal in 76 (39.2%) patients. The mean age of the low group was significantly higher than that of the normal group (67.02 ± 14.47 vs. 61.70 ± 14.38; p = 0.013). The systolic and diastolic blood pressure as well as the Glasgow coma scale score of the low group were significantly lower than that of the normal group (p = 0.004, 0.002 and 0.001, respectively). The intubation rate and APACHE (Acute Physiology and Chronic Health Evaluation) score of the low group was significantly higher than that of the normal group (p = 0.001). The platelets number and blood pH decreased, and the neutrophil/lymphocyte ratio, procalcitonin, lactate, urea, creatinine and lactate dehydrogenase concentrations increased significantly in the low group (p < 0.05). The mortality rate was 79.7% in the low group and 22.4% in the normal group (p < 0.001). Microbiological growth was observed in 68.6% of the normal group and 52.6% of the normal group (p = 0.025). The number of cultures with resistant bacteria was significantly higher in the low group (25.9%) than that in the normal group (17.5%) (p = 0.035). The severe COVID-19 patients hospitalized with vitamin D deficiency may have increased risks of poor prognosis and mortality due to secondary infections in the ICU.
Author Contributions: L.K.B. designed the study and S.K. collected the patient data. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest: The authors declare no conflict of interest.
References
Agrawal, Yin, Vitamin D and inflammatory diseases, J. Inflamm. Res, doi:10.2147/JIR.S63898
Ali, Role of vitamin D in preventing of COVID-19 infection, progression and severity, J. Infect. Public Health, doi:10.1016/j.jiph.2020.06.021
Alipio, Vitamin D supplementation could possibly improve clinical outcomes of patients infected with coronavirus-2019 (COVID, SSRN Electron. J, doi:10.2139/ssrn.3571484
Batur, Özaydın, Maviş, Gürsu, Harbige et al., Vitamin-D Binding Protein Gene Polymorphisms and Serum 25-Hydroxyvitamin-D in a Turkish Population, Metabolites, doi:10.3390/metabo11100696
Bavishi, Maddox, Messerli, Coronavirus Disease 2019 (COVID-19) Infection and Renin Angiotensin System Blockers, JAMA Cardiol, doi:10.1001/jamacardio.2020.1282
Cannell, Vieth, Umhau, Holick, Grant et al., Epidemic influenza and vitamin D, Epidemiol. Infect, doi:10.1017/S0950268806007175
Caricchio, Gallucci, Dass, Zhang, Gallucci et al., Preliminary predictive criteria for COVID-19 cytokine storm, Ann. Rheum. Dis, doi:10.1136/annrheumdis-2020-218323
Carlberg, Vitamin D Signaling in the Context of Innate Immunity: Focus on Human Monocytes, Front. Immunol, doi:10.3389/fimmu.2019.02211
Dimitrov, White, Species-specific regulation of innate immunity by vitamin D signaling, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2015.09.016
Faul, Kerley, Love, O'neill, Cody et al., Vitamin D deficiency and ARDS after SARS-CoV-2 infection, Ir. Med. J
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Hanna, Ferrey, Rhee, Sam, Pearce et al., Building a hemodiafiltration system from readily available components for continuous renal replacement therapy under disasters and pandemics: Preparing for an acute kidney injury surge during COVID-19, Curr. Opin. Nephrol. Hypertens, doi:10.1097/MNH.0000000000000658
Jin, Cai, Cheng, Cheng, Deng et al., A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version), Mil. Med. Res, doi:10.1186/s40779-020-0233-6
Kara, Ekiz, Ricci, Kara, Chang et al., Scientific Strabismus' or two related pandemics: Coronavirus disease and vitamin D deficiency, Br. J. Nutr, doi:10.1017/S0007114520001749
Klapholz, Pentakota, Zertuche, Mckenna, Roque et al., Matched Cohort Study of Convalescent COVID-19 Plasma Treatment in severely or life threateningly ill COVID-19 patients, Open Forum. Infect. Dis, doi:10.1093/ofid/ofab001
Lin, Mulick, Mathur, Smeeth, Warren-Gash et al., The association between vitamin D status and COVID-19 in England: A cohort study using UK Biobank, PLoS ONE, doi:10.1371/journal.pone.0269064
Liu, Sun, Wang, Zhang, Zhao et al., Low vitamin D status is associated with coronavirus disease 2019 outcomes: A systematic review and meta-analysis, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.12.077
Maha, Talal, Can Vitamin D Deficiency Increase the Susceptibility to COVID-19?, Front. Physiol, doi:10.3389/fphys.2021.630956
Mahdavi, A brief review of interplay between vitamin D and angiotensin-converting enzyme 2: Implications for a potential treatment for COVID-19, Rev. Med. Virol, doi:10.1002/rmv.2119
Marazuela, Giustina, Puig-Domingo, Endocrine and metabolic aspects of the COVID-19 pandemic, Rev. Endocr. Metab. Disord, doi:10.1007/s11154-020-09569-2
Martineau, Jolliffe, Demaret, Vitamin D and Tuberculosis, Vitam. D
Masmouei, Harorani, Bazrafshan, Karimi, COVID-19: Hyperinflammatory Syndrome and Hemoadsorption with CytoSorb, Blood Purif, doi:10.1159/000512199
Mercola, Grant, Wagner, Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity, Nutrients, doi:10.3390/nu12113361
Naja, Hamadeh, Nutrition amid the COVID-19 pandemic: A multi-level framework for action, Eur. J. Clin. Nutr, doi:10.1038/s41430-020-0634-3
Panfili, Roversi, D'argenio, Rossi, Cappa et al., Possible role of vitamin D in COVID-19 infection in pediatric population, J. Endocrinol. Investig, doi:10.1007/s40618-020-01327-0
Pereira, Dantas Damascena, Galvão Azevedo, De Almeida Oliveira, Da Mota Santana, Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis, Crit. Rev. Food Sci. Nutr, doi:10.1080/10408398.2020.1841090
Quesada-Gomez, Castillo, Bouillon, Vitamin d receptor stimulation to reduce acute respiratory distress syndrome (ards) in patients with Coronavirus SARS-CoV-2 infections: Revised ms sbmb 2020_166, J. Steroid Biochem. Mol. Biol, doi:10.1016/j.jsbmb.2020.105719
Simonovich, Pratx, Scibona, Beruto, Vallone et al., A Randomized Trial of Convalescent Plasma in COVID-19 Severe Pneumonia, N. Engl. J. Med, doi:10.1056/NEJMoa2031304
Speeckaert, Delanghe, Association between low vitamin D and COVID-19: Don't forget the vitamin D binding protein, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01607-y
Sullivan, Gebo, Shoham, Bloch, Lau et al., Early Outpatient Treatment for COVID-19 with Convalescent Plasma, N. Engl. J. Med, doi:10.1056/NEJMoa2119657
Szeto, Zucker, Lasota, Rubin, Walker et al., Vitamin D Status and COVID-19 Clinical Outcomes in Hospitalized Patients, Endocr. Res, doi:10.1080/07435800.2020.1867162
Tay, Poh, Rénia, Macary, Ng, The trinity of COVID-19: Immunity, inflammation and intervention, Nat. Rev. Immunol, doi:10.1038/s41577-020-0311-8
Wang, Joshi, Leopold, Jackson, Christensen et al., Association of vitamin D deficiency with COVID-19 infection severity: Systematic review and meta-analysis, Clin. Endocrinol, doi:10.1111/cen.14540
Wittebole, Montiel, Mesland, Is there a role for immune-enhancing therapies for acutely ill patients with coronavirus disease 2019?, Curr. Opin. Crit. Care, doi:10.1097/MCC.0000000000000862
Xu, Yang, Chen, Luo, Zhang et al., Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system, Mol. Med. Rep, doi:10.3892/mmr.2017.7546
Yisak, Ewunetei, Kefale, Mamuye, Teshome et al., Effects of Vitamin D on COVID-19 Infection and Prognosis: A Systematic Review, Risk Manag. Healthc. Policy, doi:10.2147/RMHP.S291584
DOI record:
{
"DOI": "10.3390/diagnostics13010059",
"ISSN": [
"2075-4418"
],
"URL": "http://dx.doi.org/10.3390/diagnostics13010059",
"abstract": "<jats:p>There are several studies showing that the vitamin D status can determine risk of COVID-19 infections, severity and mortality from coronavirus disease 2019 (COVID-19). However, the association between vitamin D (25(OH)D) and secondary infections in the prognosis of COVID-19 patients has not been reported yet. The aim was to investigate whether the vitamin D status affects the rates of secondary infections in patients with severe COVID-19 hospitalized in the intensive care unit (ICU) of a tertiary-level hospital in Turkey. The data of 194 patients with diagnosis of severe COVID-19 who were admitted to the ICU from March 2020 to June 2021 and older than 18 years were evaluated in this retrospective study. The patients were divided into two groups according to total serum 25(OH)D level as normal group (≥20 ng/mL) and low group (<20 ng/mL). The 25(OH)D level was low in 118 (60.8%) and normal in 76 (39.2%) patients. The mean age of the low group was significantly higher than that of the normal group (67.02 ± 14.47 vs. 61.70 ± 14.38; p = 0.013). The systolic and diastolic blood pressure as well as the Glasgow coma scale score of the low group were significantly lower than that of the normal group (p = 0.004, 0.002 and 0.001, respectively). The intubation rate and APACHE (Acute Physiology and Chronic Health Evaluation) score of the low group was significantly higher than that of the normal group (p = 0.001). The platelets number and blood pH decreased, and the neutrophil/lymphocyte ratio, procalcitonin, lactate, urea, creatinine and lactate dehydrogenase concentrations increased significantly in the low group (p < 0.05). The mortality rate was 79.7% in the low group and 22.4% in the normal group (p < 0.001). Microbiological growth was observed in 68.6% of the normal group and 52.6% of the normal group (p = 0.025). The number of cultures with resistant bacteria was significantly higher in the low group (25.9%) than that in the normal group (17.5%) (p = 0.035). The severe COVID-19 patients hospitalized with vitamin D deficiency may have increased risks of poor prognosis and mortality due to secondary infections in the ICU.</jats:p>",
"alternative-id": [
"diagnostics13010059"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-4803-9137",
"affiliation": [],
"authenticated-orcid": false,
"family": "Batur",
"given": "Lutfiye Karcioglu",
"sequence": "first"
},
{
"affiliation": [],
"family": "Koç",
"given": "Suna",
"sequence": "additional"
}
],
"container-title": "Diagnostics",
"container-title-short": "Diagnostics",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
12,
27
]
],
"date-time": "2022-12-27T12:02:12Z",
"timestamp": 1672142532000
},
"deposited": {
"date-parts": [
[
2022,
12,
27
]
],
"date-time": "2022-12-27T12:54:52Z",
"timestamp": 1672145692000
},
"indexed": {
"date-parts": [
[
2022,
12,
28
]
],
"date-time": "2022-12-28T05:36:29Z",
"timestamp": 1672205789893
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2022,
12,
26
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2023,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
12,
26
]
],
"date-time": "2022-12-26T00:00:00Z",
"timestamp": 1672012800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2075-4418/13/1/59/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "59",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
12,
26
]
]
},
"published-online": {
"date-parts": [
[
2022,
12,
26
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/j.jiph.2020.06.021",
"article-title": "Role of vitamin D in preventing of COVID-19 infection, progression and severity",
"author": "Ali",
"doi-asserted-by": "crossref",
"first-page": "1373",
"journal-title": "J. Infect. Public Health",
"key": "ref_1",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1080/10408398.2020.1841090",
"article-title": "Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis",
"author": "Pereira",
"doi-asserted-by": "crossref",
"first-page": "1308",
"journal-title": "Crit. Rev. Food Sci. Nutr.",
"key": "ref_2",
"volume": "62",
"year": "2022"
},
{
"DOI": "10.2147/RMHP.S291584",
"article-title": "Effects of Vitamin D on COVID-19 Infection and Prognosis: A Systematic Review",
"author": "Yisak",
"doi-asserted-by": "crossref",
"first-page": "31",
"journal-title": "Risk Manag. Healthc. Policy",
"key": "ref_3",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1007/s40520-020-01607-y",
"article-title": "Association between low vitamin D and COVID-19: Don’t forget the vitamin D binding protein",
"author": "Speeckaert",
"doi-asserted-by": "crossref",
"first-page": "1207",
"journal-title": "Aging Clin. Exp. Res.",
"key": "ref_4",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1111/cen.14540",
"article-title": "Association of vitamin D deficiency with COVID-19 infection severity: Systematic review and meta-analysis",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "281",
"journal-title": "Clin. Endocrinol.",
"key": "ref_5",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.3389/fphys.2021.630956",
"article-title": "Can Vitamin D Deficiency Increase the Susceptibility to COVID-19?",
"author": "Maha",
"doi-asserted-by": "crossref",
"first-page": "630956",
"journal-title": "Front. Physiol.",
"key": "ref_6",
"volume": "12",
"year": "2021"
},
{
"article-title": "Vitamin D deficiency and ARDS after SARS-CoV-2 infection",
"author": "Faul",
"first-page": "84",
"journal-title": "Ir. Med. J.",
"key": "ref_7",
"volume": "113",
"year": "2020"
},
{
"DOI": "10.20944/preprints202003.0235.v2",
"doi-asserted-by": "crossref",
"key": "ref_8",
"unstructured": "Grant, W.B., Lahore, H., McDonnell, S.L., Baggerly, C.A., French, C.B., Aliano, J.L., and Bhattoa, H.P. (2020). Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients, 12."
},
{
"article-title": "A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version)",
"author": "Jin",
"first-page": "4",
"journal-title": "Mil. Med. Res.",
"key": "ref_9",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1007/s11154-020-09569-2",
"article-title": "Endocrine and metabolic aspects of the COVID-19 pandemic",
"author": "Marazuela",
"doi-asserted-by": "crossref",
"first-page": "495",
"journal-title": "Rev. Endocr. Metab. Disord.",
"key": "ref_10",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1038/s41430-020-0634-3",
"article-title": "Nutrition amid the COVID-19 pandemic: A multi-level framework for action",
"author": "Naja",
"doi-asserted-by": "crossref",
"first-page": "1117",
"journal-title": "Eur. J. Clin. Nutr.",
"key": "ref_11",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.2139/ssrn.3571484",
"doi-asserted-by": "crossref",
"key": "ref_12",
"unstructured": "Alipio, M. (2020). Vitamin D supplementation could possibly improve clinical outcomes of patients infected with coronavirus-2019 (COVID-2019). SSRN Electron. J."
},
{
"DOI": "10.1080/07435800.2020.1867162",
"article-title": "Vitamin D Status and COVID-19 Clinical Outcomes in Hospitalized Patients",
"author": "Szeto",
"doi-asserted-by": "crossref",
"first-page": "66",
"journal-title": "Endocr. Res.",
"key": "ref_13",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0269064",
"doi-asserted-by": "crossref",
"key": "ref_14",
"unstructured": "Lin, L.-Y., Mulick, A., Mathur, R., Smeeth, L., Warren-Gash, C., and Langan, S.M. (2022). The association between vitamin D status and COVID-19 in England: A cohort study using UK Biobank. PLoS ONE, 17."
},
{
"key": "ref_15",
"unstructured": "COVID-19 Treatment Guidelines Panel (2022, July 29). Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health, Available online: https://www.covid19treatmentguidelines.nih.gov/."
},
{
"DOI": "10.3390/metabo11100696",
"doi-asserted-by": "crossref",
"key": "ref_16",
"unstructured": "Batur, L.K., Özaydın, A., Maviş, M.E., Gürsu, G.G., Harbige, L., and Hekim, N. (2021). Vitamin-D Binding Protein Gene Polymorphisms and Serum 25-Hydroxyvitamin-D in a Turkish Population. Metabolites, 11."
},
{
"DOI": "10.1016/j.ijid.2020.12.077",
"article-title": "Low vitamin D status is associated with coronavirus disease 2019 outcomes: A systematic review and meta-analysis",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "58",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_17",
"volume": "104",
"year": "2021"
},
{
"DOI": "10.3390/nu12113361",
"doi-asserted-by": "crossref",
"key": "ref_18",
"unstructured": "Mercola, J., Grant, W.B., and Wagner, C.L. (2020). Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity. Nutrients, 12."
},
{
"DOI": "10.3389/fimmu.2019.02211",
"article-title": "Vitamin D Signaling in the Context of Innate Immunity: Focus on Human Monocytes",
"author": "Carlberg",
"doi-asserted-by": "crossref",
"first-page": "2211",
"journal-title": "Front. Immunol.",
"key": "ref_19",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.2147/JIR.S63898",
"article-title": "Vitamin D and inflammatory diseases",
"author": "Agrawal",
"doi-asserted-by": "crossref",
"first-page": "69",
"journal-title": "J. Inflamm. Res.",
"key": "ref_20",
"volume": "7",
"year": "2014"
},
{
"DOI": "10.1007/s40618-020-01327-0",
"article-title": "Possible role of vitamin D in COVID-19 infection in pediatric population",
"author": "Panfili",
"doi-asserted-by": "crossref",
"first-page": "27",
"journal-title": "J. Endocrinol. Investig.",
"key": "ref_21",
"volume": "44",
"year": "2020"
},
{
"DOI": "10.1016/j.jsbmb.2015.09.016",
"article-title": "Species-specific regulation of innate immunity by vitamin D signaling",
"author": "Dimitrov",
"doi-asserted-by": "crossref",
"first-page": "246",
"journal-title": "J. Steroid Biochem. Mol. Biol.",
"key": "ref_22",
"volume": "164",
"year": "2016"
},
{
"DOI": "10.1016/B978-0-12-809963-6.00103-6",
"article-title": "Vitamin D and Tuberculosis",
"author": "Martineau",
"doi-asserted-by": "crossref",
"first-page": "915",
"journal-title": "Vitam. D",
"key": "ref_23",
"volume": "2",
"year": "2018"
},
{
"DOI": "10.1017/S0950268806007175",
"article-title": "Epidemic influenza and vitamin D",
"author": "Cannell",
"doi-asserted-by": "crossref",
"first-page": "1129",
"journal-title": "Epidemiol. Infect.",
"key": "ref_24",
"volume": "134",
"year": "2006"
},
{
"DOI": "10.1017/S0007114520001749",
"article-title": "‘Scientific Strabismus’ or two related pandemics: Coronavirus disease and vitamin D deficiency",
"author": "Kara",
"doi-asserted-by": "crossref",
"first-page": "736",
"journal-title": "Br. J. Nutr.",
"key": "ref_25",
"volume": "124",
"year": "2020"
},
{
"DOI": "10.1001/jamacardio.2020.1282",
"article-title": "Coronavirus Disease 2019 (COVID-19) Infection and Renin Angiotensin System Blockers",
"author": "Bavishi",
"doi-asserted-by": "crossref",
"first-page": "745",
"journal-title": "JAMA Cardiol.",
"key": "ref_26",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.3892/mmr.2017.7546",
"article-title": "Vitamin D alleviates lipopolysaccharide-induced acute lung injury via regulation of the renin-angiotensin system",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "7432",
"journal-title": "Mol. Med. Rep.",
"key": "ref_27",
"volume": "16",
"year": "2017"
},
{
"article-title": "A brief review of interplay between vitamin D and angiotensin-converting enzyme 2: Implications for a potential treatment for COVID-19",
"author": "Mahdavi",
"first-page": "e2119",
"journal-title": "Rev. Med. Virol.",
"key": "ref_28",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1136/annrheumdis-2020-218323",
"article-title": "Preliminary predictive criteria for COVID-19 cytokine storm",
"author": "Caricchio",
"doi-asserted-by": "crossref",
"first-page": "88",
"journal-title": "Ann. Rheum. Dis.",
"key": "ref_29",
"volume": "80",
"year": "2021"
},
{
"DOI": "10.1038/s41577-020-0311-8",
"article-title": "The trinity of COVID-19: Immunity, inflammation and intervention",
"author": "Tay",
"doi-asserted-by": "crossref",
"first-page": "363",
"journal-title": "Nat. Rev. Immunol.",
"key": "ref_30",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1016/j.jsbmb.2020.105719",
"article-title": "Vitamin d receptor stimulation to reduce acute respiratory distress syndrome (ards) in patients with Coronavirus SARS-CoV-2 infections: Revised ms sbmb 2020_166",
"author": "Castillo",
"doi-asserted-by": "crossref",
"first-page": "105719",
"journal-title": "J. Steroid Biochem. Mol. Biol.",
"key": "ref_31",
"volume": "202",
"year": "2020"
},
{
"DOI": "10.1097/MCC.0000000000000862",
"article-title": "Is there a role for immune-enhancing therapies for acutely ill patients with coronavirus disease 2019?",
"author": "Wittebole",
"doi-asserted-by": "crossref",
"first-page": "480",
"journal-title": "Curr. Opin. Crit. Care",
"key": "ref_32",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1093/ofid/ofab001",
"article-title": "Matched Cohort Study of Convalescent COVID-19 Plasma Treatment in severely or life threateningly ill COVID-19 patients",
"author": "Klapholz",
"doi-asserted-by": "crossref",
"first-page": "ofab001",
"journal-title": "Open Forum. Infect. Dis.",
"key": "ref_33",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2031304",
"article-title": "A Randomized Trial of Convalescent Plasma in COVID-19 Severe Pneumonia",
"author": "Simonovich",
"doi-asserted-by": "crossref",
"first-page": "619",
"journal-title": "N. Engl. J. Med.",
"key": "ref_34",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1101/2021.03.09.21252736",
"doi-asserted-by": "crossref",
"key": "ref_35",
"unstructured": "RECOVERY Collaborative Group (2021). Convalescent plasma in patients admitted to hospital with COVID-19 (RECOVERY): A randomised controlled, open-label, platform trial. Lancet, 397, 2049–2059."
},
{
"DOI": "10.1056/NEJMoa2119657",
"article-title": "Early Outpatient Treatment for COVID-19 with Convalescent Plasma",
"author": "Sullivan",
"doi-asserted-by": "crossref",
"first-page": "1700",
"journal-title": "N. Engl. J. Med.",
"key": "ref_36",
"volume": "386",
"year": "2022"
},
{
"DOI": "10.1097/MNH.0000000000000658",
"article-title": "Building a hemodiafiltration system from readily available components for continuous renal replacement therapy under disasters and pandemics: Preparing for an acute kidney injury surge during COVID-19",
"author": "Hanna",
"doi-asserted-by": "crossref",
"first-page": "93",
"journal-title": "Curr. Opin. Nephrol. Hypertens.",
"key": "ref_37",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1159/000512199",
"article-title": "COVID-19: Hyperinflammatory Syndrome and Hemoadsorption with CytoSorb",
"author": "Masmouei",
"doi-asserted-by": "crossref",
"first-page": "976",
"journal-title": "Blood Purif.",
"key": "ref_38",
"volume": "50",
"year": "2021"
}
],
"reference-count": 38,
"references-count": 38,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2075-4418/13/1/59"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Clinical Biochemistry"
],
"subtitle": [],
"title": "Association between Vitamin D Status and Secondary Infections in Patients with Severe COVID-19 Admitted in the Intensive Care Unit of a Tertiary-Level Hospital in Turkey",
"type": "journal-article",
"volume": "13"
}
