Fitness, strength and severity of COVID-19: a prospective register study of 1 559 187 Swedish conscripts
et al., BMJ Open, doi:10.1136/bmjopen-2021-051316, Jul 2021
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
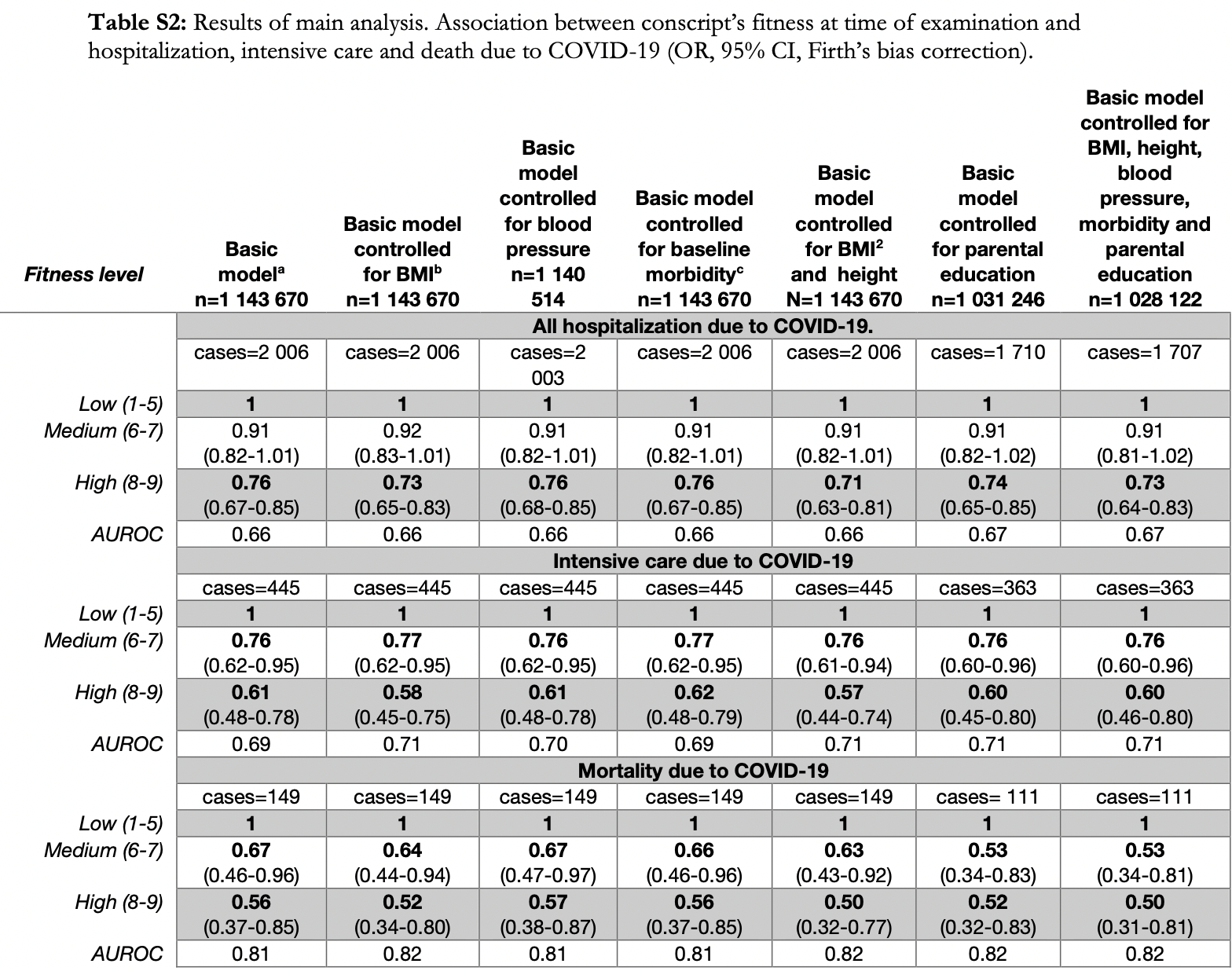
Prospective study of 1,559,187 men in Sweden with cardiorespiratory fitness levels measured on military conscription, showing high cardiorespiratory fitness associated with lower risk of COVID-19 hospitalization, ICU admission, and death.
|
risk of death, 50.0% lower, OR 0.50, p = 0.005, high vs. low fitness, model 7, RR approximated with OR.
|
|
risk of ICU admission, 40.0% lower, OR 0.60, p < 0.001, high vs. low fitness, model 7, RR approximated with OR.
|
|
risk of hospitalization, 27.0% lower, OR 0.73, p < 0.001, high vs. low fitness, model 7, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
af Geijerstam et al., 5 Jul 2021, prospective, Sweden, peer-reviewed, 9 authors, study period March 2020 - September 2020.
Contact: eijerstam@gu.se.
Fitness, strength and severity of COVID-19: a prospective register study of 1 559 187 Swedish conscripts
BMJ Open, doi:10.1136/bmjopen-2021-051316
Objective To investigate the possible connection between cardiorespiratory fitness (CRF) and muscle strength in early adulthood and severity of COVID-19 later in life. Design Prospective registry-based cohort study. Participants 1 559 187 Swedish men, undergoing military conscription between 1968 and 2005 at a mean age of 18.3 (SD 0.73) years. Main outcome measures Hospitalisation, intensive care or death due to COVID-19 from March to September 2020, in relation to CRF and muscle strength. Results High CRF in late adolescence and early adulthood had a protective association with severe COVID-19 later in life with OR (95% CI) 0.76 (0.67 to 0.85) for hospitalisation (n=2 006), 0.61 (0.48 to 0.78) for intensive care (n=445) and 0.56 (0.37 to 0.85) for mortality (n=149), compared with the lowest category of CRF. The association remains unchanged when controlled for body mass index (BMI), blood pressure, chronic diseases and parental education level at baseline, and incident cardiovascular disease before 2020. Moreover, lower muscle strength in late adolescence showed a linear association with a higher risk of all three outcomes when controlled for BMI and height. Conclusions Physical fitness at a young age is associated with severity of COVID-19 many years later. This underscores the necessity to increase the general physical fitness of the population to offer protection against future viral pandemics.
Regionhälsan, Region Västra Götaland, Göteborg, Sweden Twitter Agnes af Geijerstam @agnesafg Contributors LL and MÅ initiated the project. AaG and KM performed all statistical analyses. AaG had main responsibility for writing the article. MB, JR, JN, MA and AR all made substantial contributions to the interpretation of the analyses, the structure and content of the manuscript and have read and approved of the final draft. All authors have agreed to be accountable for all aspects of the work.
Competing interests None declared. Patient consent for publication Not required.
Ethics approval The Ethics Committee of the University of Gothenburg and Confidentiality Clearance at Statistics Sweden approved the study (EPN Reference numbers EPN 462-14 and 567-15; T174-15, T653-17, T196-17, T 2020-01325, T 2020-02420). The requirement for informed consent was waived by the Ethics Committee of the University of Gothenburg for secondary analysis of existing data. Provenance and peer review Not commissioned; externally peer reviewed. Data availability statement Data may be obtained from a third party and are not publicly available. The data used in this study is available on request from the Swedish National Board of Health and Welfare, the Swedish intensive care registry and Statistics Sweden. Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or..
References
Aberg, Pedersen, Torén, Cardiovascular fitness is associated with cognition in young adulthood, Proc Natl Acad Sci U S A, doi:10.1073/pnas.0905307106
Berg, Rosengren, Aires, Trends in overweight and obesity from 1985 to 2002 in Göteborg, West Sweden, Int J Obes, doi:10.1038/sj.ijo.0802964
Blom, Lönn, Ekblom, Lifestyle habits and mental health in light of the two COVID-19 pandemic waves in Sweden, 2020, Int J Environ Res Public Health, doi:10.3390/ijerph18063313
Braekkan, Borch, Mathiesen, Body height and risk of venous thromboembolism: the Tromsø study, Am J Epidemiol, doi:10.1093/aje/kwq066
Burtscher, Millet, Burtscher, Low cardiorespiratory and mitochondrial fitness as risk factors in viral infections: implications for COVID-19
Cheval, Sieber, Maltagliati, Muscle strength is associated with COVID-19 hospitalization in adults 50 years of age and older, MedRxiv
Cheval, Sivaramakrishnan, Maltagliati, Relationships between changes in self-reported physical activity, sedentary behaviour and health during the coronavirus (COVID-19) pandemic in France and Switzerland, J Sports Sci, doi:10.1080/02640414.2020.1841396
Clark, Jit, Gash, Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study, Lancet Glob Health, doi:10.1016/S2214-109X(20)30264-3
Cole, Lobstein, Extended International (IOTF) body mass index cut-offs for thinness, overweight and obesity, Pediatr Obes, doi:10.1111/j.2047-6310.2012.00064.x
Crump, Sundquist, Winkleby, Interactive effects of obesity and physical fitness on risk of ischemic heart disease, Int J Obes, doi:10.1038/ijo.2016.209
Crump, Sundquist, Winkleby, Interactive effects of physical fitness and body mass index on the risk of hypertension, JAMA Intern Med, doi:10.1001/jamainternmed.2015.7444
Crump, Sundquist, Winkleby, Physical fitness among Swedish military conscripts and long-term risk for type 2 diabetes mellitus: a cohort study, Ann Intern Med, doi:10.7326/M15-2002
Ekblom-Bak, Ekblom, Söderling, Sex-and age-specific associations between cardiorespiratory fitness, CVD morbidity and all-cause mortality in 266.109 adults, Prev Med, doi:10.1016/j.ypmed.2019.105799
Flanagan, Beyl, Fearnbach, The impact of COVID-19 Stay-At-Home orders on health behaviors in adults, Obesity, doi:10.1002/oby.23066
Gao, Piernas, Astbury,
Gleeson, Bishop, Stensel, The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease, Nat Rev Immunol, doi:10.1038/nri3041
Hamer, Gale, Kivimäki, Overweight, obesity, and risk of hospitalization for COVID-19: a community-based cohort study of adults in the United Kingdom, Proc Natl Acad Sci U S A, doi:10.1073/pnas.2011086117
In, Brawner, Ehrman, Bole, Inverse relationship of maximal exercise capacity to hospitalization secondary to coronavirus disease 2019, Mayo Clin Proc, doi:10.1016/j.mayocp.2020.10.003
King, Zeng, Logistic regression in rare events data, Polit. anal, doi:10.1093/oxfordjournals.pan.a004868
Li, Hertzmark, Louie, The SAS lgtphcurv9 macro
Lindgren, Börjesson, Örjan, Physical activity pattern, cardiorespiratory fitness, and socioeconomic status in the SCAPIS pilot trial -A cross-sectional study, Prev Med Rep, doi:10.1016/j.pmedr.2016.04.010
Lindgren, Åberg, Schaufelberger, Cardiorespiratory fitness and muscle strength in late adolescence and long-term risk of early heart failure in Swedish men, Eur J Prev Cardiol, doi:10.1177/2047487317689974
Lissner, Mehlig, Rosengren, A growing social divide in body mass index, strength, and fitness of Swedish male conscripts, J Adolesc Health, doi:10.1016/j.jadohealth.2019.02.016
Ludvigsson, Andersson, Ekbom, External review and validation of the Swedish national inpatient register, BMC Public Health, doi:10.1186/1471-2458-11-450
Nordesjö, Schéle, Validity of an ergometer cycle test and measures of isometric muscle strength when prediction some aspects of military performance, Swed J Def Med
O'driscoll, Dos Santos, Wang, Age-Specific mortality and immunity patterns of SARS-CoV-2, Nature, doi:10.1038/s41586-020-2918-0
Peckham, De Gruijter, Raine, Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission, Nat Commun, doi:10.1038/s41467-020-19741-6
Prince, Adamo, Hamel, A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review, Int J Behav Nutr Phys Act, doi:10.1186/1479-5868-5-56
Ross, Blair, Arena, American heart association physical activity Committee of the Council on lifestyle and cardiometabolic health; Council on clinical cardiology; Council on epidemiology and prevention; Council on cardiovascular and stroke nursing; Council on functional genomics and translational biology; stroke Council. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American heart association, Circulation
Salgado-Aranda, Pérez-Castellano, Núñez-Gil, Influence of baseline physical activity as a modifying factor on COVID-19 mortality: a single-center, retrospective study, Infect Dis Ther, doi:10.1007/s40121-021-00418-6
Sallis, Young, Tartof, Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients, Br J Sports Med, doi:10.1136/bjsports-2021-104080
Valeri, Vanderweele, Mediation analysis allowing for exposuremediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros, Psychol Methods, doi:10.1037/a0031034
Williams, Mancia, Spiering, ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of cardiology (ESC) and the European Society of hypertension (ESH), Eur Heart J
Yates, Razieh, Zaccardi, Obesity, walking PACE and risk of severe COVID-19 and mortality: analysis of UK Biobank, Int J Obes, doi:10.1038/s41366-021-00771-z
Zbinden-Foncea, Francaux, Deldicque, Does high cardiorespiratory fitness confer some protection against proinflammatory responses after infection by SARS-CoV-2?, Obesity, doi:10.1002/oby.22849
Åberg, Kuhn, Nyberg, Influence of cardiovascular fitness and muscle strength in early adulthood on long-term risk of stroke in Swedish men, Stroke, doi:10.1161/STROKEAHA.115.009008
DOI record:
{
"DOI": "10.1136/bmjopen-2021-051316",
"ISSN": [
"2044-6055",
"2044-6055"
],
"URL": "http://dx.doi.org/10.1136/bmjopen-2021-051316",
"abstract": "<jats:sec><jats:title>Objective</jats:title><jats:p>To investigate the possible connection between cardiorespiratory fitness (CRF) and muscle strength in early adulthood and severity of COVID-19 later in life.</jats:p></jats:sec><jats:sec><jats:title>Design</jats:title><jats:p>Prospective registry-based cohort study.</jats:p></jats:sec><jats:sec><jats:title>Participants</jats:title><jats:p>1 559 187 Swedish men, undergoing military conscription between 1968 and 2005 at a mean age of 18.3 (SD 0.73) years.</jats:p></jats:sec><jats:sec><jats:title>Main outcome measures</jats:title><jats:p>Hospitalisation, intensive care or death due to COVID-19 from March to September 2020, in relation to CRF and muscle strength.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>High CRF in late adolescence and early adulthood had a protective association with severe COVID-19 later in life with OR (95% CI) 0.76 (0.67 to 0.85) for hospitalisation (n=2 006), 0.61 (0.48 to 0.78) for intensive care (n=445) and 0.56 (0.37 to 0.85) for mortality (n=149), compared with the lowest category of CRF. The association remains unchanged when controlled for body mass index (BMI), blood pressure, chronic diseases and parental education level at baseline, and incident cardiovascular disease before 2020. Moreover, lower muscle strength in late adolescence showed a linear association with a higher risk of all three outcomes when controlled for BMI and height.</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>Physical fitness at a young age is associated with severity of COVID-19 many years later. This underscores the necessity to increase the general physical fitness of the population to offer protection against future viral pandemics.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjopen-2021-051316"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-0897-6548",
"affiliation": [],
"authenticated-orcid": false,
"family": "af Geijerstam",
"given": "Agnes",
"sequence": "first"
},
{
"affiliation": [],
"family": "Mehlig",
"given": "Kirsten",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Börjesson",
"given": "Mats",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Robertson",
"given": "Josefina",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4336-3886",
"affiliation": [],
"authenticated-orcid": false,
"family": "Nyberg",
"given": "Jenny",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Adiels",
"given": "Martin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rosengren",
"given": "Annika",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Åberg",
"given": "Maria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lissner",
"given": "Lauren",
"sequence": "additional"
}
],
"container-title": "BMJ Open",
"container-title-short": "BMJ Open",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
7,
5
]
],
"date-time": "2021-07-05T16:02:39Z",
"timestamp": 1625500959000
},
"deposited": {
"date-parts": [
[
2021,
7,
5
]
],
"date-time": "2021-07-05T16:03:01Z",
"timestamp": 1625500981000
},
"funder": [
{
"DOI": "10.13039/501100004359",
"award": [
"02508",
"VRREG 2019-00193",
"VRREG 2020-05792"
],
"doi-asserted-by": "crossref",
"name": "Swedish Research Council"
},
{
"award": [
"FORMAS-2012-00038"
],
"name": "EpiLife-Teens Research Program"
},
{
"award": [
"ALFGBG-720201"
],
"name": "Swedish ALF-agreement"
}
],
"indexed": {
"date-parts": [
[
2022,
5,
24
]
],
"date-time": "2022-05-24T04:24:52Z",
"timestamp": 1653366292583
},
"is-referenced-by-count": 11,
"issue": "7",
"issued": {
"date-parts": [
[
2021,
7
]
]
},
"journal-issue": {
"issue": "7",
"published-online": {
"date-parts": [
[
2021,
7,
5
]
]
},
"published-print": {
"date-parts": [
[
2021,
7
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 4,
"start": {
"date-parts": [
[
2021,
7,
5
]
],
"date-time": "2021-07-05T00:00:00Z",
"timestamp": 1625443200000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjopen-2021-051316",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e051316",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
7
]
]
},
"published-online": {
"date-parts": [
[
2021,
7,
5
]
]
},
"published-print": {
"date-parts": [
[
2021,
7
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1016/S2214-109X(20)30264-3",
"article-title": "Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study",
"author": "Clark",
"doi-asserted-by": "crossref",
"first-page": "e1003",
"journal-title": "Lancet Glob Health",
"key": "2021070509002767000_11.7.e051316.1",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1073/pnas.2011086117",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.2"
},
{
"DOI": "10.1038/s41586-020-2918-0",
"article-title": "Age-Specific mortality and immunity patterns of SARS-CoV-2",
"author": "O'Driscoll",
"doi-asserted-by": "crossref",
"first-page": "140",
"journal-title": "Nature",
"key": "2021070509002767000_11.7.e051316.3",
"volume": "590",
"year": "2021"
},
{
"DOI": "10.1161/CIR.0000000000000461",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.4"
},
{
"DOI": "10.1002/oby.22849",
"article-title": "Does high cardiorespiratory fitness confer some protection against proinflammatory responses after infection by SARS-CoV-2?",
"author": "Zbinden-Foncea",
"doi-asserted-by": "crossref",
"first-page": "1378",
"journal-title": "Obesity",
"key": "2021070509002767000_11.7.e051316.5",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1038/s41366-021-00771-z",
"article-title": "Obesity, walking PACE and risk of severe COVID-19 and mortality: analysis of UK Biobank",
"author": "Yates",
"doi-asserted-by": "crossref",
"first-page": "1155",
"journal-title": "Int J Obes",
"key": "2021070509002767000_11.7.e051316.6",
"volume": "45",
"year": "2021"
},
{
"DOI": "10.1136/bjsports-2021-104080",
"article-title": "Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients",
"author": "Sallis",
"doi-asserted-by": "crossref",
"journal-title": "Br J Sports Med",
"key": "2021070509002767000_11.7.e051316.7",
"year": "2021"
},
{
"DOI": "10.1007/s40121-021-00418-6",
"article-title": "Influence of baseline physical activity as a modifying factor on COVID-19 mortality: a single-center, retrospective study",
"author": "Salgado-Aranda",
"doi-asserted-by": "crossref",
"first-page": "801",
"journal-title": "Infect Dis Ther",
"key": "2021070509002767000_11.7.e051316.8",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1016/j.mayocp.2020.10.003",
"article-title": "Inverse relationship of maximal exercise capacity to hospitalization secondary to coronavirus disease 2019",
"author": "Brawner",
"doi-asserted-by": "crossref",
"first-page": "32",
"journal-title": "Mayo Clin Proc",
"key": "2021070509002767000_11.7.e051316.9",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1101/2021.02.02.21250909",
"doi-asserted-by": "crossref",
"key": "2021070509002767000_11.7.e051316.10",
"unstructured": "Cheval B , Sieber S , Maltagliati S . Muscle strength is associated with COVID-19 hospitalization in adults 50 years of age and older. MedRxiv 2021."
},
{
"DOI": "10.1073/pnas.0905307106",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.11"
},
{
"DOI": "10.1016/S2213-8587(21)00089-9",
"doi-asserted-by": "crossref",
"key": "2021070509002767000_11.7.e051316.12",
"unstructured": "Gao M , Piernas C , Astbury NM . Associations between body-mass index and COVID-19 severity in 6· 9 million people in England: a prospective, community-based, cohort study. Lancet Diabetes Endocrinol 2021."
},
{
"DOI": "10.1186/1479-5868-5-56",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.13"
},
{
"DOI": "10.1038/sj.ijo.0802964",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.14"
},
{
"DOI": "10.1161/STROKEAHA.115.009008",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.15"
},
{
"article-title": "Validity of an ergometer cycle test and measures of isometric muscle strength when prediction some aspects of military performance",
"author": "Nordesjö",
"first-page": "11",
"journal-title": "Swed J Def Med",
"key": "2021070509002767000_11.7.e051316.16",
"volume": "10",
"year": "1974"
},
{
"DOI": "10.1016/j.jadohealth.2019.02.016",
"article-title": "A growing social divide in body mass index, strength, and fitness of Swedish male conscripts",
"author": "Lissner",
"doi-asserted-by": "crossref",
"first-page": "232",
"journal-title": "J Adolesc Health",
"key": "2021070509002767000_11.7.e051316.17",
"volume": "65",
"year": "2019"
},
{
"key": "2021070509002767000_11.7.e051316.18",
"unstructured": "World Health Organization . The Asia-Pacific perspective: redefining obesity and its treatment 2000."
},
{
"DOI": "10.1111/j.2047-6310.2012.00064.x",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.19"
},
{
"DOI": "10.1093/eurheartj/ehy339",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.20"
},
{
"DOI": "10.1186/1471-2458-11-1",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.21"
},
{
"DOI": "10.1093/oxfordjournals.pan.a004868",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.22"
},
{
"key": "2021070509002767000_11.7.e051316.23",
"unstructured": "Li R , Hertzmark E , Louie M . The SAS lgtphcurv9 macro. Boston Channing Lab 2011."
},
{
"DOI": "10.1037/a0031034",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.24"
},
{
"DOI": "10.1177/2047487317689974",
"article-title": "Cardiorespiratory fitness and muscle strength in late adolescence and long-term risk of early heart failure in Swedish men",
"author": "Lindgren",
"doi-asserted-by": "crossref",
"first-page": "876",
"journal-title": "Eur J Prev Cardiol",
"key": "2021070509002767000_11.7.e051316.25",
"volume": "24",
"year": "2017"
},
{
"DOI": "10.1038/ijo.2016.209",
"article-title": "Interactive effects of obesity and physical fitness on risk of ischemic heart disease",
"author": "Crump",
"doi-asserted-by": "crossref",
"first-page": "255",
"journal-title": "Int J Obes",
"key": "2021070509002767000_11.7.e051316.26",
"volume": "41",
"year": "2017"
},
{
"DOI": "10.1001/jamainternmed.2015.7444",
"article-title": "Interactive effects of physical fitness and body mass index on the risk of hypertension",
"author": "Crump",
"doi-asserted-by": "crossref",
"first-page": "210",
"journal-title": "JAMA Intern Med",
"key": "2021070509002767000_11.7.e051316.27",
"volume": "176",
"year": "2016"
},
{
"DOI": "10.7326/M15-2002",
"article-title": "Physical fitness among Swedish military conscripts and long-term risk for type 2 diabetes mellitus: a cohort study",
"author": "Crump",
"doi-asserted-by": "crossref",
"first-page": "577",
"journal-title": "Ann Intern Med",
"key": "2021070509002767000_11.7.e051316.28",
"volume": "164",
"year": "2016"
},
{
"DOI": "10.1038/nri3041",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.29"
},
{
"DOI": "10.1016/j.ypmed.2019.105799",
"article-title": "Sex- and age-specific associations between cardiorespiratory fitness, CVD morbidity and all-cause mortality in 266.109 adults",
"author": "Ekblom-Bak",
"doi-asserted-by": "crossref",
"journal-title": "Prev Med",
"key": "2021070509002767000_11.7.e051316.30",
"volume": "127",
"year": "2019"
},
{
"DOI": "10.1136/bjsports-2020-103572",
"doi-asserted-by": "crossref",
"key": "2021070509002767000_11.7.e051316.31",
"unstructured": "Burtscher J , Millet GP , Burtscher M . Low cardiorespiratory and mitochondrial fitness as risk factors in viral infections: implications for COVID-19 2020."
},
{
"DOI": "10.1016/j.pmedr.2016.04.010",
"article-title": "Physical activity pattern, cardiorespiratory fitness, and socioeconomic status in the SCAPIS pilot trial - A cross-sectional study",
"author": "Lindgren",
"doi-asserted-by": "crossref",
"first-page": "44",
"journal-title": "Prev Med Rep",
"key": "2021070509002767000_11.7.e051316.32",
"volume": "4",
"year": "2016"
},
{
"DOI": "10.1093/aje/kwq066",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.33"
},
{
"DOI": "10.3390/ijerph18063313",
"article-title": "Lifestyle habits and mental health in light of the two COVID-19 pandemic waves in Sweden, 2020",
"author": "Blom",
"doi-asserted-by": "crossref",
"journal-title": "Int J Environ Res Public Health",
"key": "2021070509002767000_11.7.e051316.34",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1080/02640414.2020.1841396",
"article-title": "Relationships between changes in self-reported physical activity, sedentary behaviour and health during the coronavirus (COVID-19) pandemic in France and Switzerland",
"author": "Cheval",
"doi-asserted-by": "crossref",
"first-page": "699",
"journal-title": "J Sports Sci",
"key": "2021070509002767000_11.7.e051316.35",
"volume": "39",
"year": "2021"
},
{
"DOI": "10.1002/oby.23066",
"article-title": "The impact of COVID-19 Stay-At-Home orders on health behaviors in adults",
"author": "Flanagan",
"doi-asserted-by": "crossref",
"first-page": "438",
"journal-title": "Obesity",
"key": "2021070509002767000_11.7.e051316.36",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1038/s41467-019-13889-6",
"doi-asserted-by": "publisher",
"key": "2021070509002767000_11.7.e051316.37"
}
],
"reference-count": 37,
"references-count": 37,
"relation": {},
"resource": {
"primary": {
"URL": "https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2021-051316"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Fitness, strength and severity of COVID-19: a prospective register study of 1 559 187 Swedish conscripts",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "11"
}
