Secondary pulmonary infection and co-infection in elderly COVID-19 patients during the pandemics in a tertiary general hospital in Beijing, China
et al., Frontiers in Microbiology, doi:10.3389/fmicb.2023.1280026, Oct 2023
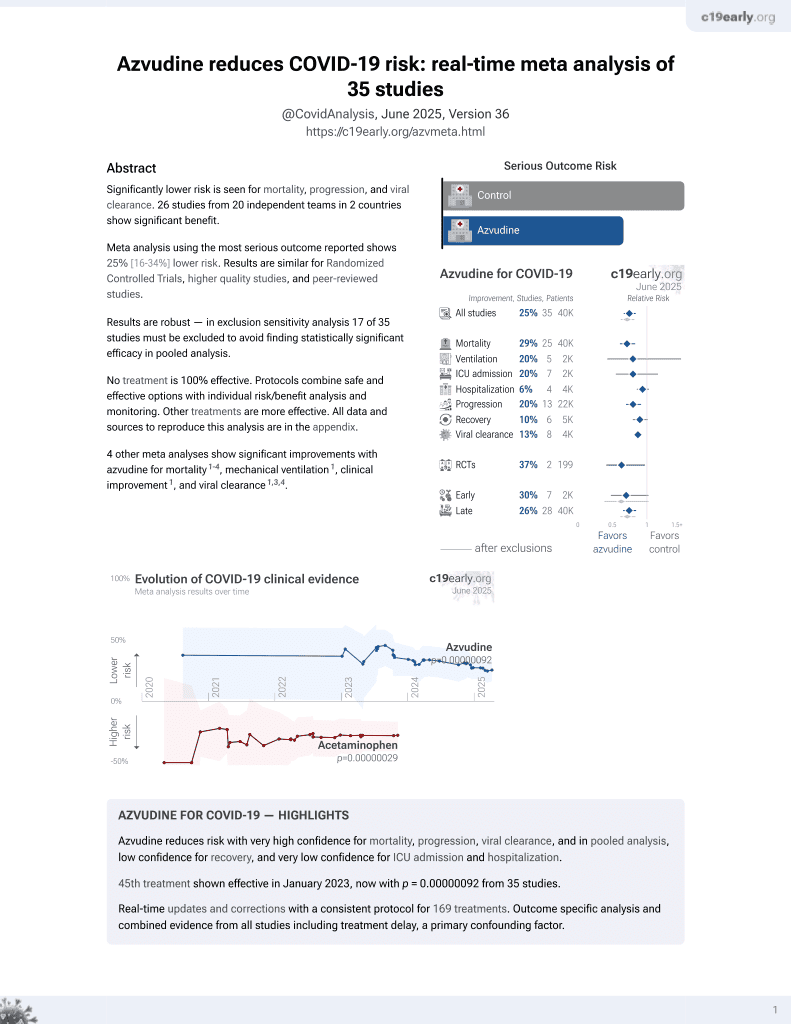
Azvudine for COVID-19
48th treatment shown to reduce risk in
January 2023, now with p = 0.000000017 from 39 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 322 hospitalized patients ≥65 in China, showing lower mortality with azvudine treatment, without statistical significance.
Although the 22% lower mortality is not statistically significant, it is consistent with the significant 30% lower mortality [20‑39%] from meta-analysis of the 28 mortality results to date.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments3.
This may explain in part the very high mortality seen in this study.
This study is excluded in the after exclusion results of meta-analysis:
substantial unadjusted confounding by indication likely; unadjusted results with no group details.
Study covers azvudine and paxlovid.
|
risk of death, 21.8% lower, RR 0.78, p = 0.15, treatment 37 of 131 (28.2%), control 69 of 191 (36.1%), NNT 13.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Xiong et al., Real-world data of Azvudine-induced hepatotoxicity among hospitalized COVID-19 patients in China: a retrospective case-control study, Frontiers in Pharmacology, doi:10.3389/fphar.2025.1558054.
Zhou et al., 12 Oct 2023, retrospective, China, peer-reviewed, median age 81.0, 6 authors, study period 1 December, 2022 - 31 January, 2023.
Contact: lxm2128@163.com, leihuang2031@bjmu.edu.cn.
Secondary pulmonary infection and co-infection in elderly COVID-19 patients during the pandemics in a tertiary general hospital in Beijing, China
Frontiers in Microbiology, doi:10.3389/fmicb.2023.1280026
Background: Most people are infected with COVID-19 during pandemics at the end of 2022. Older patients were more vulnerable. However, the incidence of secondary bacterial, fungal or viral pulmonary infection and co-infection is not well described in elderly hospitalized COVID-19 patients.
Methods: We retrospectively reviewed the medical records of all elderly (≥65 years) hospitalized patients with laboratory-confirmed COVID-19 from December 1, 2022 to January 31, 2023. Demographics, underlying diseases, treatments, and laboratory data were collected. Univariate and multivariate logistic regression models were used to explore the risk factors associated with secondary bacterial, fungal or viral pulmonary infection and co-infection. Results: A total of 322 older patients with COVID-19 were enrolled. The incidence of secondary bacterial, fungal or viral pulmonary infection and co-infection was 27.3% (88/322) and 7.5% (24/322), respectively. The overall in-hospital mortality of all patients was 32.9% (106/322), and the in-hospital mortality among patients who acquired with secondary pulmonary infection and co-infection was 57.0% (57/100). A total of 23.9% (77/322) of patients were admitted to ICU within 48 h of hospitalization. The incidence of secondary pulmonary infection and co-infection among patients admitted to the ICU was 50.6% (39/77) and 13.0% (10/77), respectively. The overall in-hospital mortality of ICU patients was 48.1% (37/77), and the in-hospital mortality of ICU patients acquired with secondary pulmonary infection and co-infection was 61.4% (27/44). A total of 83.5% (269/322) of the included patients received empirical antibiotic therapy before positive Clinical Microbiology results. Influenza A virus (the vast majority were the H3N2 subtype) was the most common community acquired pathogen for co-infection. While A. baumannii, K. pneumoniae, and P. aeruginosa were the common hospital acquired pathogens for co-infection and secondary pulmonary infection. The incidence of Carbapenem-resistant Gram-negative bacilli (CR-GNB) infections was high, and the mortality reached 76.9%. Predictors of secondary pulmonary infection and co-infection were ICU admission within 48 h of hospitalization, cerebrovascular diseases, critical COVID-19, and PCT > 0.5 ng/mL.
Ethics statement The studies involving humans were approved by the Ethics Committee of Peking University First Hospital, Beijing, China (Approval No. 2023-yan-090) . The studies were conducted in accordance with the local legislation and institutional requirements. The Ethics Committee/Institutional Review Board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because Due to the retrospective observational study and the confidentiality of patient information.
Author contributions CZ: Formal analysis, Data curation, Writing -original draft. YJ: Writing -review and editing, Data curation. LS: Data curation, Writing -review and editing. HL: Conceptualization, Writingreview and editing. XL: Conceptualization, Funding acquisition, Writing -review and editing. LH: Data curation, Funding acquisition, Writing -review and editing.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Akrami, Montazeri, Saki, Neisi, Khedri et al., Bacterial profiles and their antibiotic resistance background in superinfections caused by multidrug-resistant bacteria among COVID-19 ICU patients from southwest Iran, J. Med. Virol, doi:10.1002/jmv.28403
Campion, Scully, Antibiotic use in the intensive care unit: Optimization and de-escalation, J. Intensive Care Med, doi:10.1177/0885066618762747
Chong, Saha, Ananthakrishnan, Chopra, Stateof-the-art review of secondary pulmonary infections in patients with COVID-19 pneumonia, doi:10.1007/s15010-021-01602-z
Croxatto, Prod'hom, Greub, Applications of MALDI-TOF mass spectrometry in clinical diagnostic microbiology, FEMS Microbiol. Rev
Du, Liu, Yin, Wang, Guan et al., Hospitalization and critical care of 109 decedents with COVID-19 Pneumonia in Wuhan, China, Ann. Am. Thorac. Soc, doi:10.1513/AnnalsATS.202003-225OC
Feng, Ling, Bai, Xie, Huang et al., COVID-19 with different severities: A multicenter study of clinical features, Am. J. Respir. Crit. Care Med, doi:10.1164/rccm.202002-0445OC
Huang, Pranata, Lymphopenia in severe coronavirus disease-2019 (COVID-19): systematic review and meta-analysis, J. Intensive Care, doi:10.1186/s40560-020-00453-4
Iacovelli, Oliva, Siccardi, Tramontano, Pellegrino et al., Risk factors and effect on mortality of superinfections in a newly established COVID-19 respiratory sub-intensive care unit at University Hospital in Rome, BMC Pulm. Med, doi:10.1186/s12890-023-02315-9
Jones, Microbial etiologies of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia, Clin. Infect. Dis, doi:10.1086/653053
Langford, So, Raybardhan, Leung, Westwood et al., Bacterial co-infection and secondary infection in patients with COVID-19: A living rapid review and meta-analysis, Clin. Microbiol. Infect, doi:10.1016/j.cmi.2020.07.016
Lansbury, Lim, Baskaran, Lim, Co-infections in people with COVID-19: A systematic review and meta-analysis, J. Infect, doi:10.1016/j.jinf.2020.05.046
Li, Wang, Yang, Cai, Cao et al., Etiology and antimicrobial resistance of secondary bacterial infections in patients hospitalized with COVID-19 in Wuhan, China: A retrospective analysis, Antimicrob. Resist. Infect. Control, doi:10.1186/s13756-020-00819-1
Lin, Lu, Cao, Li, Hypothesis for potential pathogenesis of SARS-CoV-2 infection-a review of immune changes in patients with viral pneumonia, Emerg. Microbes Infect, doi:10.1080/22221751.2020.1746199
Majumder, Rahman, Cohall, Bharatha, Singh et al., Antimicrobial stewardship: Fighting antimicrobial resistance and protecting global public health, Infect. Drug Resist, doi:10.2147/idr.S290835
Malik, Patel, Mehta, Patel, Kelkar et al., Biomarkers and outcomes of COVID-19 hospitalisations: Systematic review and meta-analysis, BMJ Evid. Based Med, doi:10.1136/bmjebm-2020-111536
Moreno-García, Puerta-Alcalde, Letona, Meira, Dueñas et al., Bacterial co-infection at hospital admission in patients with COVID-19, Int. J. Infect. Dis, doi:10.1016/j.ijid.2022.03.003
Najjar-Debbiny, Gronich, Weber, Khoury, Amar et al., Effectiveness of Paxlovid in Reducing Severe Coronavirus Disease 2019 and Mortality in High-Risk Patients, Clin. Infect. Dis, doi:10.1093/cid/ciac443
Owens, Antimicrobial stewardship: Application in the intensive care unit, Infect. Dis. Clin. North Am, doi:10.1016/j.idc.2009.04.015
Pandey, May, Tan, Hughes, Jones et al., Comparative incidence of early and late bloodstream and respiratory tract co-infection in patients admitted to ICU with COVID-19 pneumonia versus Influenza A or B pneumonia versus no viral pneumonia: Wales multicentre ICU cohort study, Crit. Care, doi:10.1186/s13054-022-04026-9
Patton, Orihuela, Harrod, Bhuiyan, Dominic et al., COVID-19 bacteremic co-infection is a major risk factor for mortality, ICU admission, and mechanical ventilation, Crit. Care, doi:10.1186/s13054-023-04312-0
Poston, Patel, Davis, Management of critically ill adults with COVID-19, JAMA, doi:10.1001/jama.2020.4914
Pourajam, Kalantari, Talebzadeh, Mellali, Sami et al., Secondary bacterial infection and clinical characteristics in patients with COVID-19 admitted to two intensive care units of an academic hospital in Iran during the first wave of the pandemic, Front. Cell Infect. Microbiol, doi:10.3389/fcimb.2022.784130
Ripa, Galli, Poli, Oltolini, Spagnuolo et al., Secondary infections in patients hospitalized with COVID-19: Incidence and predictive factors, Clin. Microbiol. Infect, doi:10.1016/j.cmi.2020.10.021
Schuetz, Albrich, Mueller, Procalcitonin for diagnosis of infection and guide to antibiotic decisions: Past, present and future, BMC Med, doi:10.1186/1741-7015-9-107
Shankar-Hari, Vale, Godolphin, Fisher, Higgins et al., Association between administration of IL-6 antagonists and mortality among patients hospitalized for COVID-19: A meta-analysis, JAMA, doi:10.1001/jama.2021.11330
Shu, Fang, De Vlas, Gao, Richardus et al., Dual seasonal patterns for influenza, China, Emerg. Infect. Dis, doi:10.3201/eid1604.091578
Singer, Deutschman, Seymour, Shankar-Hari, Annane et al., The third international consensus definitions for sepsis and septic shock (Sepsis-3), JAMA, doi:10.1001/jama.2016.0287
Wang, He, Yu, Hu, Bao et al., Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up, J. Infect, doi:10.1016/j.jinf.2020.03.019
Wang, Hou, Luo, Tang, Wu et al., The laboratory tests and host immunity of COVID-19 patients with different severity of illness, JCI Insight, doi:10.1172/jci.insight.137799
Wang, Yang, Li, Wen, Zhang, Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China, Clin. Infect. Dis, doi:10.1093/cid/ciaa272
Wu, Chen, Cai, Xia, Zhou et al., Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 Pneumonia in Wuhan, China, JAMA Intern. Med, doi:10.1001/jamainternmed.2020.0994
Yang, Li, Tao, Yang, Wang et al., Infection with SARS-CoV-2 causes abnormal laboratory results of multiple organs in patients, Aging, doi:10.18632/aging.103255
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study, Lancet, doi:10.1016/s0140-6736(20)30566-3
Çölkesen, Tarakçı, Eroglu, Kacar, Özdemir Armagan et al., Carbapenem-resistant Klebsiella pneumoniae infection and its risk factors in older adult patients, Clin. Interv. Aging, doi:10.2147/cia.S406214
DOI record:
{
"DOI": "10.3389/fmicb.2023.1280026",
"ISSN": [
"1664-302X"
],
"URL": "http://dx.doi.org/10.3389/fmicb.2023.1280026",
"abstract": "<jats:sec><jats:title>Background</jats:title><jats:p>Most people are infected with COVID-19 during pandemics at the end of 2022. Older patients were more vulnerable. However, the incidence of secondary bacterial, fungal or viral pulmonary infection and co-infection is not well described in elderly hospitalized COVID-19 patients.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>We retrospectively reviewed the medical records of all elderly (≥65 years) hospitalized patients with laboratory-confirmed COVID-19 from December 1, 2022 to January 31, 2023. Demographics, underlying diseases, treatments, and laboratory data were collected. Univariate and multivariate logistic regression models were used to explore the risk factors associated with secondary bacterial, fungal or viral pulmonary infection and co-infection.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>A total of 322 older patients with COVID-19 were enrolled. The incidence of secondary bacterial, fungal or viral pulmonary infection and co-infection was 27.3% (88/322) and 7.5% (24/322), respectively. The overall in-hospital mortality of all patients was 32.9% (106/322), and the in-hospital mortality among patients who acquired with secondary pulmonary infection and co-infection was 57.0% (57/100). A total of 23.9% (77/322) of patients were admitted to ICU within 48 h of hospitalization. The incidence of secondary pulmonary infection and co-infection among patients admitted to the ICU was 50.6% (39/77) and 13.0% (10/77), respectively. The overall in-hospital mortality of ICU patients was 48.1% (37/77), and the in-hospital mortality of ICU patients acquired with secondary pulmonary infection and co-infection was 61.4% (27/44). A total of 83.5% (269/322) of the included patients received empirical antibiotic therapy before positive Clinical Microbiology results. Influenza A virus (the vast majority were the H3N2 subtype) was the most common community acquired pathogen for co-infection. While <jats:italic>A. baumannii</jats:italic>, <jats:italic>K. pneumoniae</jats:italic>, and <jats:italic>P. aeruginosa</jats:italic> were the common hospital acquired pathogens for co-infection and secondary pulmonary infection. The incidence of Carbapenem-resistant Gram-negative bacilli (CR-GNB) infections was high, and the mortality reached 76.9%. Predictors of secondary pulmonary infection and co-infection were ICU admission within 48 h of hospitalization, cerebrovascular diseases, critical COVID-19, and PCT &gt; 0.5 ng/mL.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>The prognosis for elderly hospitalized COVID-19 patients with secondary pulmonary infection or co-infection is poor. The inflammatory biomarker PCT &gt; 0.5 ng/mL played an important role in the early prediction of secondary pulmonary infection and co-infection in COVID-19 patients.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fmicb.2023.1280026"
],
"author": [
{
"affiliation": [],
"family": "Zhou",
"given": "Chaoe",
"sequence": "first"
},
{
"affiliation": [],
"family": "Jiang",
"given": "Yaping",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sun",
"given": "Liying",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Haixia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liu",
"given": "Xinmin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Huang",
"given": "Lei",
"sequence": "additional"
}
],
"container-title": "Frontiers in Microbiology",
"container-title-short": "Front. Microbiol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2023,
10,
12
]
],
"date-time": "2023-10-12T09:06:14Z",
"timestamp": 1697101574000
},
"deposited": {
"date-parts": [
[
2023,
10,
12
]
],
"date-time": "2023-10-12T09:06:16Z",
"timestamp": 1697101576000
},
"indexed": {
"date-parts": [
[
2023,
10,
13
]
],
"date-time": "2023-10-13T05:32:56Z",
"timestamp": 1697175176999
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
10,
12
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
10,
12
]
],
"date-time": "2023-10-12T00:00:00Z",
"timestamp": 1697068800000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmicb.2023.1280026/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2023,
10,
12
]
]
},
"published-online": {
"date-parts": [
[
2023,
10,
12
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1002/jmv.28403",
"article-title": "Bacterial profiles and their antibiotic resistance background in superinfections caused by multidrug-resistant bacteria among COVID-19 ICU patients from southwest Iran.",
"author": "Akrami",
"doi-asserted-by": "publisher",
"journal-title": "J. Med. Virol.",
"key": "B1",
"volume": "95",
"year": "2023"
},
{
"DOI": "10.1177/0885066618762747",
"article-title": "Antibiotic use in the intensive care unit: Optimization and de-escalation.",
"author": "Campion",
"doi-asserted-by": "publisher",
"first-page": "647",
"journal-title": "J. Intensive Care Med.",
"key": "B2",
"volume": "33",
"year": "2018"
},
{
"DOI": "10.1007/s15010-021-01602-z",
"article-title": "State-of-the-art review of secondary pulmonary infections in patients with COVID-19 pneumonia.",
"author": "Chong",
"doi-asserted-by": "publisher",
"first-page": "591",
"journal-title": "Infection",
"key": "B3",
"volume": "49",
"year": "2021"
},
{
"journal-title": "Performance standards for antimicrobial susceptibility testing.",
"key": "B4",
"year": "2021"
},
{
"DOI": "10.2147/cia.S406214",
"article-title": "Carbapenem-resistant Klebsiella pneumoniae infection and its risk factors in older adult patients.",
"author": "Çölkesen",
"doi-asserted-by": "publisher",
"first-page": "1037",
"journal-title": "Clin. Interv. Aging",
"key": "B5",
"volume": "18",
"year": "2023"
},
{
"DOI": "10.1111/j.1574-6976.2011.00298.x",
"article-title": "Applications of MALDI-TOF mass spectrometry in clinical diagnostic microbiology.",
"author": "Croxatto",
"doi-asserted-by": "publisher",
"first-page": "380",
"journal-title": "FEMS Microbiol. Rev.",
"key": "B6",
"volume": "36",
"year": "2012"
},
{
"DOI": "10.1513/AnnalsATS.202003-225OC",
"article-title": "Hospitalization and critical care of 109 decedents with COVID-19 Pneumonia in Wuhan, China.",
"author": "Du",
"doi-asserted-by": "publisher",
"first-page": "839",
"journal-title": "Ann. Am. Thorac. Soc.",
"key": "B7",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1164/rccm.202002-0445OC",
"article-title": "COVID-19 with different severities: A multicenter study of clinical features.",
"author": "Feng",
"doi-asserted-by": "publisher",
"first-page": "1380",
"journal-title": "Am. J. Respir. Crit. Care Med.",
"key": "B8",
"volume": "201",
"year": "2020"
},
{
"DOI": "10.1186/s40560-020-00453-4",
"article-title": "Lymphopenia in severe coronavirus disease-2019 (COVID-19): systematic review and meta-analysis.",
"author": "Huang",
"doi-asserted-by": "publisher",
"journal-title": "J. Intensive Care",
"key": "B9",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1186/s12890-023-02315-9",
"article-title": "Risk factors and effect on mortality of superinfections in a newly established COVID-19 respiratory sub-intensive care unit at University Hospital in Rome.",
"author": "Iacovelli",
"doi-asserted-by": "publisher",
"journal-title": "BMC Pulm. Med.",
"key": "B10",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.1086/653053",
"article-title": "Microbial etiologies of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia.",
"author": "Jones",
"doi-asserted-by": "publisher",
"first-page": "S81",
"journal-title": "Clin. Infect. Dis.",
"key": "B11",
"volume": "51",
"year": "2010"
},
{
"DOI": "10.1016/j.cmi.2020.07.016",
"article-title": "Bacterial co-infection and secondary infection in patients with COVID-19: A living rapid review and meta-analysis.",
"author": "Langford",
"doi-asserted-by": "publisher",
"first-page": "1622",
"journal-title": "Clin. Microbiol. Infect.",
"key": "B12",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.05.046",
"article-title": "Co-infections in people with COVID-19: A systematic review and meta-analysis.",
"author": "Lansbury",
"doi-asserted-by": "publisher",
"first-page": "266",
"journal-title": "J. Infect.",
"key": "B13",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1186/s13756-020-00819-1",
"article-title": "Etiology and antimicrobial resistance of secondary bacterial infections in patients hospitalized with COVID-19 in Wuhan, China: A retrospective analysis.",
"author": "Li",
"doi-asserted-by": "publisher",
"journal-title": "Antimicrob. Resist. Infect. Control",
"key": "B14",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1080/22221751.2020.1746199",
"article-title": "Hypothesis for potential pathogenesis of SARS-CoV-2 infection-a review of immune changes in patients with viral pneumonia.",
"author": "Lin",
"doi-asserted-by": "publisher",
"first-page": "727",
"journal-title": "Emerg. Microbes Infect.",
"key": "B15",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.2147/idr.S290835",
"article-title": "Antimicrobial stewardship: Fighting antimicrobial resistance and protecting global public health.",
"author": "Majumder",
"doi-asserted-by": "publisher",
"first-page": "4713",
"journal-title": "Infect. Drug Resist.",
"key": "B16",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1136/bmjebm-2020-111536",
"article-title": "Biomarkers and outcomes of COVID-19 hospitalisations: Systematic review and meta-analysis.",
"author": "Malik",
"doi-asserted-by": "publisher",
"first-page": "107",
"journal-title": "BMJ Evid. Based Med.",
"key": "B17",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2022.03.003",
"article-title": "Bacterial co-infection at hospital admission in patients with COVID-19.",
"author": "Moreno-García",
"doi-asserted-by": "publisher",
"first-page": "197",
"journal-title": "Int. J. Infect. Dis.",
"key": "B18",
"volume": "118",
"year": "2022"
},
{
"DOI": "10.1093/cid/ciac443",
"article-title": "Effectiveness of Paxlovid in Reducing Severe Coronavirus Disease 2019 and Mortality in High-Risk Patients.",
"author": "Najjar-Debbiny",
"doi-asserted-by": "publisher",
"first-page": "e342",
"journal-title": "Clin. Infect. Dis.",
"key": "B19",
"volume": "76",
"year": "2023"
},
{
"DOI": "10.1016/j.idc.2009.04.015",
"article-title": "Antimicrobial stewardship: Application in the intensive care unit.",
"author": "Owens",
"doi-asserted-by": "publisher",
"first-page": "683",
"journal-title": "Infect. Dis. Clin. North Am.",
"key": "B20",
"volume": "23",
"year": "2009"
},
{
"DOI": "10.1186/s13054-022-04026-9",
"article-title": "Comparative incidence of early and late bloodstream and respiratory tract co-infection in patients admitted to ICU with COVID-19 pneumonia versus Influenza A or B pneumonia versus no viral pneumonia: Wales multicentre ICU cohort study.",
"author": "Pandey",
"doi-asserted-by": "publisher",
"journal-title": "Crit. Care",
"key": "B21",
"volume": "26",
"year": "2022"
},
{
"DOI": "10.1186/s13054-023-04312-0",
"article-title": "COVID-19 bacteremic co-infection is a major risk factor for mortality, ICU admission, and mechanical ventilation.",
"author": "Patton",
"doi-asserted-by": "publisher",
"journal-title": "Crit. Care",
"key": "B22",
"volume": "27",
"year": "2023"
},
{
"DOI": "10.1001/jama.2020.4914",
"article-title": "Management of critically ill adults with COVID-19.",
"author": "Poston",
"doi-asserted-by": "publisher",
"first-page": "1839",
"journal-title": "JAMA",
"key": "B23",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.3389/fcimb.2022.784130",
"article-title": "Secondary bacterial infection and clinical characteristics in patients with COVID-19 admitted to two intensive care units of an academic hospital in Iran during the first wave of the pandemic.",
"author": "Pourajam",
"doi-asserted-by": "publisher",
"journal-title": "Front. Cell Infect. Microbiol.",
"key": "B24",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/j.cmi.2020.10.021",
"article-title": "Secondary infections in patients hospitalized with COVID-19: Incidence and predictive factors.",
"author": "Ripa",
"doi-asserted-by": "publisher",
"first-page": "451",
"journal-title": "Clin. Microbiol. Infect.",
"key": "B25",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1186/1741-7015-9-107",
"article-title": "Procalcitonin for diagnosis of infection and guide to antibiotic decisions: Past, present and future.",
"author": "Schuetz",
"doi-asserted-by": "publisher",
"journal-title": "BMC Med.",
"key": "B26",
"volume": "9",
"year": "2011"
},
{
"DOI": "10.1001/jama.2021.11330",
"article-title": "Association between administration of IL-6 antagonists and mortality among patients hospitalized for COVID-19: A meta-analysis.",
"author": "Shankar-Hari",
"doi-asserted-by": "publisher",
"first-page": "499",
"journal-title": "JAMA",
"key": "B27",
"volume": "326",
"year": "2021"
},
{
"DOI": "10.3201/eid1604.091578",
"article-title": "Dual seasonal patterns for influenza, China.",
"author": "Shu",
"doi-asserted-by": "publisher",
"first-page": "725",
"journal-title": "Emerg. Infect. Dis.",
"key": "B28",
"volume": "16",
"year": "2010"
},
{
"DOI": "10.1001/jama.2016.0287",
"article-title": "The third international consensus definitions for sepsis and septic shock (Sepsis-3).",
"author": "Singer",
"doi-asserted-by": "publisher",
"first-page": "801",
"journal-title": "JAMA",
"key": "B29",
"volume": "315",
"year": "2016"
},
{
"DOI": "10.1172/jci.insight.137799",
"article-title": "The laboratory tests and host immunity of COVID-19 patients with different severity of illness.",
"author": "Wang",
"doi-asserted-by": "publisher",
"journal-title": "JCI Insight",
"key": "B30",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.03.019",
"article-title": "Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up.",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "639",
"journal-title": "J. Infect.",
"key": "B31",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa272",
"article-title": "Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China.",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "769",
"journal-title": "Clin. Infect. Dis.",
"key": "B32",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"article-title": "Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 Pneumonia in Wuhan, China.",
"author": "Wu",
"doi-asserted-by": "publisher",
"first-page": "934",
"journal-title": "JAMA Intern. Med.",
"key": "B33",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.18632/aging.103255",
"article-title": "Infection with SARS-CoV-2 causes abnormal laboratory results of multiple organs in patients.",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "10059",
"journal-title": "Aging",
"key": "B34",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/s0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study.",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "1054",
"journal-title": "Lancet",
"key": "B35",
"volume": "395",
"year": "2020"
}
],
"reference-count": 35,
"references-count": 35,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fmicb.2023.1280026/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Microbiology (medical)",
"Microbiology"
],
"subtitle": [],
"title": "Secondary pulmonary infection and co-infection in elderly COVID-19 patients during the pandemics in a tertiary general hospital in Beijing, China",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "14"
}
zhou13