Long-term diet and risk of SARS -CoV-2 infection and Coronavirus Disease 2019 (COVID-19) severity
et al., The American Journal of Clinical Nutrition, doi:10.1093/ajcn/nqac219, Aug 2022
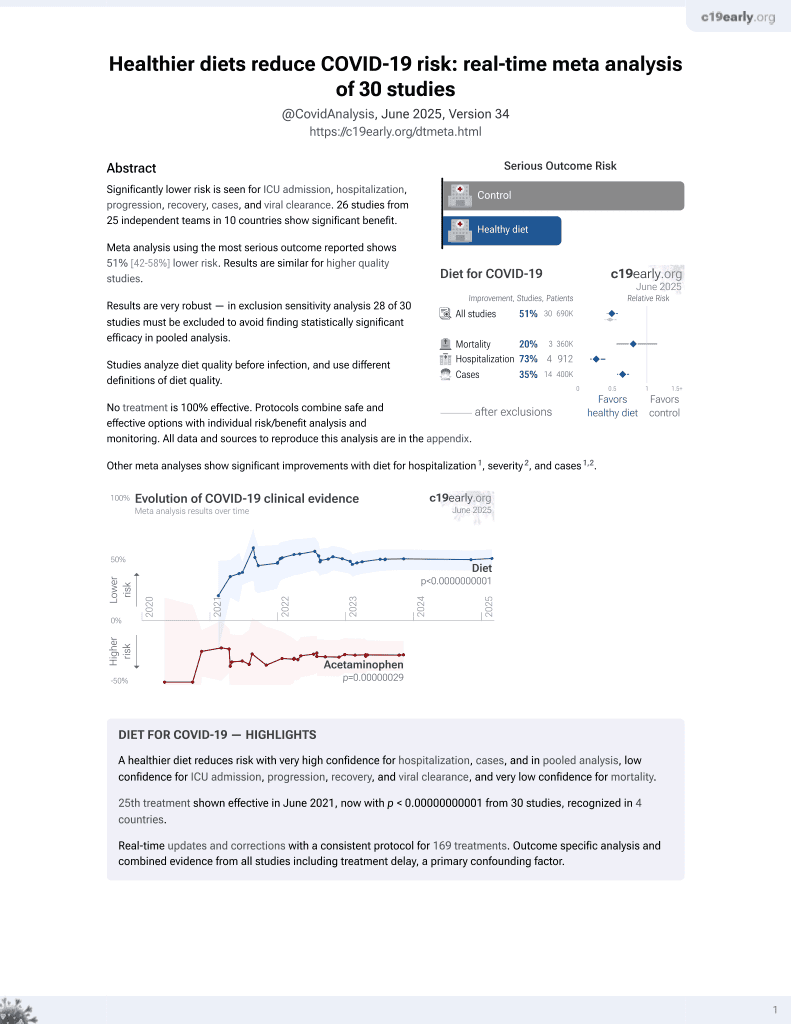
Diet for COVID-19
26th treatment shown to reduce risk in
June 2021, now with p < 0.00000000001 from 30 studies, recognized in 4 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Analysis of 42,935 participants showing lower risk of COVID-19 with healthier diets. Risk of severe cases was also lower with healthier diets, while not reaching statistical significance. Severity results are only provided with diet indices as a continuous variable.
|
risk of case, 19.0% lower, OR 0.81, p = 0.008, Q4 vs. Q1, model 3 + IPW, AHEI, RR approximated with OR.
|
|
risk of case, 21.0% lower, OR 0.79, p = 0.006, Q4 vs. Q1, model 3 + IPW, AMED, RR approximated with OR.
|
|
risk of case, 28.6% lower, OR 0.71, p < 0.001, inverted to make OR<1 favor higher quality diet, Q1 vs. Q4, model 3 + IPW, EDIH, RR approximated with OR.
|
|
risk of case, 11.5% lower, OR 0.88, p = 0.10, inverted to make OR<1 favor higher quality diet, Q1 vs. Q4, model 3 + IPW, EDIP, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Yue et al., 9 Aug 2022, retrospective, multiple countries, peer-reviewed, survey, 11 authors.
Contact: sbhupath@hsph.harvard.edu.
Long-term diet and risk of SARS -CoV-2 infection and Coronavirus Disease 2019 (COVID-19) severity
doi:10.1093/ajcn/nqac219/6659183
Background The role of diet on COVID-19 is emerging.
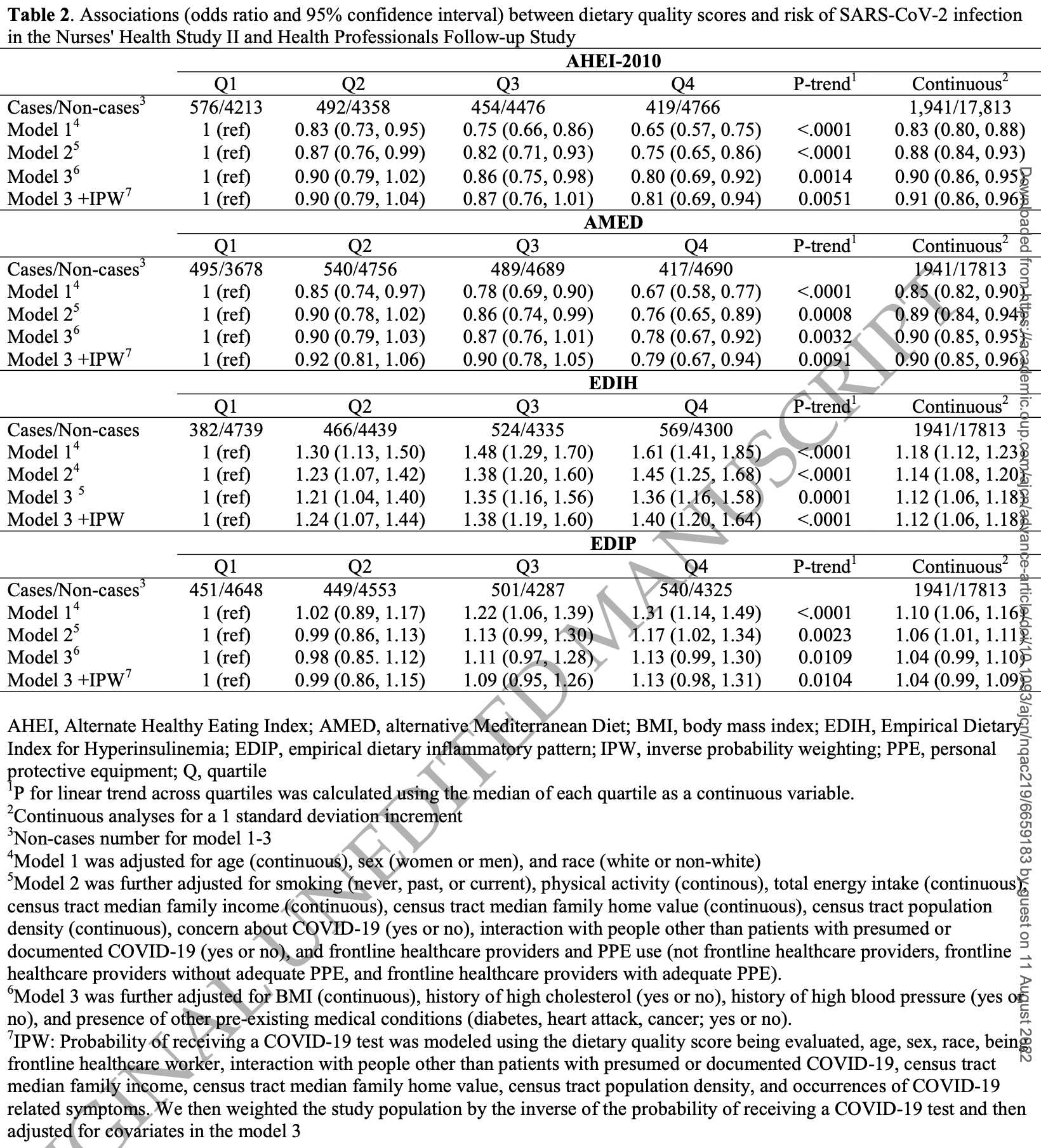
Methods We included 42,935 participants aged 55 to 99 years in two ongoing cohort studies, Nurses' Health Study II and Health Professionals Follow-up Study, who completed a series of COVID-19 surveys in 2020 and 2021. Using data from food frequency questionnaires prior to COVID-19, we assessed diet quality using the Alternative Healthy Eating Index (AHEI)-2010, the alternative Mediterranean Diet (AMED) score, an Empirical Dietary Index for Hyperinsulinemia (EDIH), and an Empirical Dietary Inflammatory Pattern (EDIP). We calculated multivariable adjusted odds ratios (ORs) and 95% confidence intervals (95% CIs) for SARS-CoV-2 infection and severity of COVID-19 after controlling for demographic, medical, and lifestyle factors.
Results Among 19,754 participants tested for SARS-CoV-2, 1,941 participants reported a positive result. Of these, 1,327 reported symptoms needing assistance and another 109 were hospitalized. Healthier diet, represented by higher AHEI-2010 and AMED scores and lower EDIH and EDIP scores, were associated with lower likelihood of SARS-CoV-2 infection (ORs Q (quartile) 4 vs. Q1 (95%CI) were 0.80 (0.69, 0.92) for AHEI-2010; 0.78 (0.67, 0.92) for AMED; 1.36 (1.16, 1.57) for EDIH; and 1.13 (0.99, 1.30) for EDIP; all p for trend ≤ 0.01). In the analysis of COVID-19 severity, participants with healthier diet had lower likelihood of severe infection and were less likely to be hospitalized due to COVID-19. However, associations were no longer significant after controlling for BMI and pre-existing medical conditions.
P for linear trend across quartiles was calculated using the median of each quartile as a continuous variable. 2 Continuous analyses for a 1 standard deviation increment 3 Non-cases number for model 1-3 4 Model 1 was adjusted for age (continuous), sex (women or men), and race (white or non-white) 5 Model 2 was further adjusted for smoking (never, past, or current), physical activity (continous), total energy intake (continuous), census tract median family income (continuous), census tract median family home value (continuous), census tract population density (continuous), concern about COVID-19 (yes or no), interaction with people other than patients with presumed or documented COVID-19 (yes or no), and frontline healthcare providers and PPE use (not frontline healthcare providers, frontline healthcare providers without adequate PPE, and frontline healthcare providers with adequate PPE). 6 Model 3 was further adjusted for BMI (continuous), history of high cholesterol (yes or no), history of high blood pressure (yes or no), and presence of other pre-existing medical conditions (diabetes, heart attack, cancer; yes or no). 7 IPW: Probability of receiving a COVID-19 test was modeled using the dietary quality score being evaluated, age, sex, race, being frontline healthcare worker, interaction with people other than patients with presumed or documented COVID-19, census tract median family income, census tract median family home value, census tract population density, and..
References
Ahei-, Alternative Healthy Eating Index
Ainsworth, Haskell, Leon, Jacobs, Montoye et al., Compendium of physical activities: classification of energy costs of human physical activities, Medicine and science in sports and exercise
Al-Shaar, Yuan, Rosner, Dean, Ivey et al., Reproducibility and Validity of a Semiquantitative Food Frequency Questionnaire in Men Assessed by Multiple Methods, Am J Epidemiol, doi:10.1093/aje/kwaa280
Angelidi, Kokkinos, Katechaki, Mantzoros, Mediterranean diet as a nutritional approach for COVID-19, Metabolism, doi:10.1016/j.metabol.2020.154407
Bao, Bertoia, Lenart, Stampfer, Willett et al., Origin, Methods, and Evolution of the Three Nurses' Health Studies, American journal of public health, doi:10.2105/ajph.2016.303338
Bao, Bertoia, Lenart, Stampfer, Willett et al., Origin, methods, and evolution of the three Nurses' Health Studies, American journal of public health
Belanger, Hill, Angelidi, Dalamaga, Sowers et al., Covid-19 and Disparities in Nutrition and Obesity, New England Journal of Medicine, doi:10.1056/NEJMp2021264.291
Calder, Nutrition, immunity and COVID-19, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000085
Catanzaro, Fagiani, Racchi, Corsini, Govoni et al., Immune response in COVID-19: addressing a pharmacological challenge by targeting pathways triggered by SARS-CoV-2, Signal transduction and targeted therapy
Chiuve, Fung, Rimm, Hu, Mccullough et al., Alternative dietary indices both strongly predict risk of chronic disease, J Nutr, doi:10.3945/jn.111.157222
Codo, Davanzo, Monteiro, De Souza, Muraro et al., Elevated Glucose Levels Favor SARS-CoV-2 Infection and Monocyte Response through a HIF-1α/Glycolysis-Dependent Axis, Cell Metab, doi:10.1016/j.cmet.2020.07.007
Ding, Rocheleau, Boiano, Kang, Becene et al., American Frontline Healthcare Personnel's Access to and Use of Personal Protective Equipment Early in the COVID-19 Pandemic, J Occup Environ Med, doi:10.1097/jom.0000000000002308
Edih, Empirical Dietary Index for Hyperinsulinemia; EDIP, Empirical Dietary Inflammatory Pattern; MET, metabolic equivalent of tasks Values are means (SD) or percentages standardized to the distribution of age, with the exception of age itself
Fung, Hu, Mccullough, Newby, Willett et al., Diet quality is associated with the risk of estrogen receptor-negative breast cancer in postmenopausal women, J Nutr, doi:10.1093/jn/136.2.466
Greene, Roberts, Frugé, Negative Association Between Mediterranean Diet Adherence and COVID-19 Cases and Related Deaths in Spain and 23 OECD Countries: An Ecological Study, Front Nutr, doi:10.3389/fnut.2021.591964
Gustine, Jones, Immunopathology of Hyperinflammation in COVID-19, Am J Pathol, doi:10.1016/j.ajpath.2020.08.009
Hosseini, Berthon, Saedisomeolia, Starkey, Collison et al., Effects of fruit and vegetable consumption on inflammatory biomarkers and immune cell populations: a systematic literature review and meta-analysis, The American Journal of Clinical Nutrition, doi:10.1093/ajcn/nqy082
Hosseini, Hashemi, Shomali, Asghari, Gharibi et al., Innate and adaptive immune responses against coronavirus, Biomedicine & Pharmacotherapy
Ji, Zhu, Zhong, Li, Pang et al., Association of elevated inflammatory markers and severe COVID-19: A meta-analysis, Medicine, doi:10.1097/md.0000000000023315
Kim, Rebholz, Hegde, Lafiura, Raghavan et al., Plant-based diets, pescatarian diets and COVID-19 severity: a population-based casecontrol study in six countries, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2021-000272
Leung, Clinical features of deaths in the novel coronavirus epidemic in China, Rev Med Virol, doi:10.1002/rmv.2103
Li, Liu, Chen, Yang, Huang et al., Effects of indoor environment and lifestyle on respiratory health of children in Chongqing, China, J Thorac Dis, doi:10.21037/jtd.2020.03.102
Lim, Bae, Kwon, Nauck, COVID-19 and diabetes mellitus: from pathophysiology to clinical management, Nature Reviews Endocrinology, doi:10.1038/s41574-020-00435-4
Liu, Zhou, Li, Garner, Watkins et al., Research and Development on Therapeutic Agents and Vaccines for COVID-19 and Related Human Coronavirus Diseases, ACS Central Science, doi:10.1021/acscentsci.0c00272
Maiorino, Bellastella, Longo, Caruso, Esposito, Mediterranean Diet and COVID-19: Hypothesizing Potential Benefits in People With Diabetes, Front Endocrinol, doi:10.3389/fendo.2020.574315
Menni, Valdes, Freidin, Sudre, Nguyen et al., Real-time tracking of self-reported symptoms to predict potential COVID-19, Nature Medicine, doi:10.1038/s41591-020-0916-2
Merino, Joshi, Nguyen, Leeming, Mazidi et al., Diet quality and risk and severity of COVID-19: a prospective cohort study, Gut, doi:10.1136/gutjnl-2021-325353
Moscatelli, Sessa, Valenzano, Polito, Monda et al., COVID-19: Role of Nutrition and Supplementation, Nutrients, doi:10.3390/nu13030976
Rimm, Giovannucci, Willett, Colditz, Ascherio et al., Prospective study of alcohol consumption and risk of coronary disease in men, The Lancet
Santos, Magro, Evangelista-Poderoso, Saad, Diabetes, obesity, and insulin resistance in COVID-19: molecular interrelationship and therapeutic implications, Diabetol Metab Syndr, doi:10.1186/s13098-021-00639-2
Schwingshackl, Hoffmann, Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension score, and health outcomes: a systematic review and meta-analysis of cohort studies, Journal of the Academy of Nutrition and Dietetics
Suardi, Cazzaniga, Graci, Dongo, Palestini, Link between Viral Infections, Immune System, Inflammation and Diet, Int J Environ Res Public Health, doi:10.3390/ijerph18052455
Tabung, Brown, Fung, Dietary patterns and colorectal cancer risk: a review of 17 years of evidence (2000-2016), Current colorectal cancer reports
Tabung, Smith-Warner, Chavarro, Wu, Fuchs et al., Development and validation of an empirical index of dietary inflammatory potential, The Journal of Nutrition, doi:10.3945/jn.115.228718
Tabung, Wang, Fung, Hu, Smith-Warner et al., Development and validation of empirical indices to assess the insulinaemic potential of diet and lifestyle, The British journal of nutrition, doi:10.1017/s0007114516003755
Tabung, Wang, Fung, Smith-Warner, Keum et al., Association of dietary insulinemic potential and colorectal cancer risk in men and women, Am J Clin Nutr, doi:10.1093/ajcn/nqy093
Tavakol, Ghannadi, Tabesh, Halabchi, Noormohammadpour et al., Relationship between physical activity, healthy lifestyle and COVID-19 disease severity; a cross-sectional study, Z Gesundh Wiss, doi:10.1007/s10389-020-01468-9
Wang, Spiegelman, Kuchiba, Lochhead, Kim et al., Statistical methods for studying disease subtype heterogeneity, Statistics in medicine
Whowgotc, Management of C-i. A minimal common outcome measure set for COVID-19 clinical research, Lancet Infect Dis, doi:10.1016/S1473-3099(20)30483-7
Wolf, Hunter, Colditz, Manson, Stampfer et al., Reproducibility and validity of a self-administered physical activity questionnaire, Int J Epidemiol
Wolff, Nee, Hickey, Marschollek, Risk factors for Covid-19 severity and fatality: a structured literature review, Infection, doi:10.1007/s15010-020-01509-1
Wu, Wu, Liu, Yang, The SARS-CoV-2 outbreak: What we know, Int J Infect Dis, doi:10.1016/j.ijid.2020.03.004
Yuan, Spiegelman, Rimm, Rosner, Stampfer et al., Validity of a dietary questionnaire assessed by comparison with multiple weighed dietary records or 24-hour recalls, American journal of epidemiology
Yue, Petimar, Willett, Smith-Warner, Yuan et al., Dietary flavonoids and flavonoid-rich foods: validity and reproducibility of FFQ-derived intake estimates, Public Health Nutrition
Yue, Yuan, Wang, Wang, Song et al., Reproducibility and validity of diet quality scores derived from food frequency questionnaires, Am J Clin Nutr, doi:10.1093/ajcn/nqab368
Zabetakis, Lordan, Norton, Tsoupras, COVID-19: The Inflammation Link and the Role of Nutrition in Potential Mitigation, Nutrients, doi:10.3390/nu12051466
DOI record:
{
"DOI": "10.1093/ajcn/nqac219",
"ISSN": [
"0002-9165",
"1938-3207"
],
"URL": "http://dx.doi.org/10.1093/ajcn/nqac219",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>The role of diet on COVID-19 is emerging.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>We included 42,935 participants aged 55 to 99 years in two ongoing cohort studies, Nurses’ Health Study II and Health Professionals Follow-up Study, who completed a series of COVID-19 surveys in 2020 and 2021. Using data from food frequency questionnaires prior to COVID-19, we assessed diet quality using the Alternative Healthy Eating Index (AHEI)-2010, the alternative Mediterranean Diet (AMED) score, an Empirical Dietary Index for Hyperinsulinemia (EDIH), and an Empirical Dietary Inflammatory Pattern (EDIP). We calculated multivariable adjusted odds ratios (ORs) and 95% confidence intervals (95% CIs) for SARS-CoV-2 infection and severity of COVID-19 after controlling for demographic, medical, and lifestyle factors.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Among 19,754 participants tested for SARS-CoV-2, 1,941 participants reported a positive result. Of these, 1,327 reported symptoms needing assistance and another 109 were hospitalized. Healthier diet, represented by higher AHEI-2010 and AMED scores and lower EDIH and EDIP scores, were associated with lower likelihood of SARS-CoV-2 infection (ORs Q (quartile) 4 vs. Q1 (95%CI) were 0.80 (0.69, 0.92) for AHEI-2010; 0.78 (0.67, 0.92) for AMED; 1.36 (1.16, 1.57) for EDIH; and 1.13 (0.99, 1.30) for EDIP; all p for trend ≤ 0.01). In the analysis of COVID-19 severity, participants with healthier diet had lower likelihood of severe infection and were less likely to be hospitalized due to COVID-19. However, associations were no longer significant after controlling for BMI and pre-existing medical conditions.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusion</jats:title>\n <jats:p>Diet may be an important modifiable risk factor for SARS-CoV-2 infection, as well as for severity of COVID-19. This association is partially mediated by BMI and pre-existing medical conditions.</jats:p>\n </jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-6018-2980",
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health , Boston, MA , USA"
}
],
"authenticated-orcid": false,
"family": "Yue",
"given": "Yiyang",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Clinical and Translational Epidemiology Unit, Massachusetts General Hospital and Harvard Medical School , Boston, MA"
},
{
"name": "Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School , Boston, MA"
}
],
"family": "Ma",
"given": "Wenjie",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Center for Communicable Disease Dynamics, Department of Epidemiology, Harvard T.H. Chan School of Public Health , Boston, MA , USA"
}
],
"family": "Accorsi",
"given": "Emma K",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health , Boston, MA , USA"
}
],
"family": "Ding",
"given": "Ming",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health , Boston, MA , USA"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health , Boston, MA"
},
{
"name": "Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School , Boston, MA"
}
],
"family": "Hu",
"given": "Frank",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health , Boston, MA , USA"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health , Boston, MA"
},
{
"name": "Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School , Boston, MA"
}
],
"family": "Willett",
"given": "Walter C",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3662-5964",
"affiliation": [
{
"name": "Clinical and Translational Epidemiology Unit, Massachusetts General Hospital and Harvard Medical School , Boston, MA"
},
{
"name": "Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School , Boston, MA"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health , Boston, MA"
},
{
"name": "Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School , Boston, MA"
}
],
"authenticated-orcid": false,
"family": "Chan",
"given": "Andrew T",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8480-1563",
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health , Boston, MA , USA"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health , Boston, MA"
},
{
"name": "Division of Women's Health, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School , Boston, MA"
}
],
"authenticated-orcid": false,
"family": "Sun",
"given": "Qi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health , Boston, MA"
},
{
"name": "Division of Women's Health, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School , Boston, MA"
}
],
"family": "Edwards",
"given": "Janet Rich",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health , Boston, MA , USA"
},
{
"name": "Department of Epidemiology, Harvard T.H. Chan School of Public Health , Boston, MA"
}
],
"family": "Smith-Warner",
"given": "Stephanie A",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Nutrition, Harvard T.H. Chan School of Public Health , Boston, MA , USA"
},
{
"name": "Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School , Boston, MA"
}
],
"family": "Bhupathiraju",
"given": "Shilpa N",
"sequence": "additional"
}
],
"container-title": "The American Journal of Clinical Nutrition",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
8,
10
]
],
"date-time": "2022-08-10T03:08:48Z",
"timestamp": 1660100928000
},
"deposited": {
"date-parts": [
[
2022,
8,
10
]
],
"date-time": "2022-08-10T03:08:49Z",
"timestamp": 1660100929000
},
"indexed": {
"date-parts": [
[
2022,
8,
10
]
],
"date-time": "2022-08-10T03:42:04Z",
"timestamp": 1660102924057
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
8,
9
]
]
},
"language": "en",
"license": [
{
"URL": "https://academic.oup.com/journals/pages/open_access/funder_policies/chorus/standard_publication_model",
"content-version": "am",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
9
]
],
"date-time": "2022-08-09T00:00:00Z",
"timestamp": 1660003200000
}
}
],
"link": [
{
"URL": "https://academic.oup.com/ajcn/advance-article-pdf/doi/10.1093/ajcn/nqac219/45298001/nqac219.pdf",
"content-type": "application/pdf",
"content-version": "am",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/ajcn/advance-article-pdf/doi/10.1093/ajcn/nqac219/45298001/nqac219.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "286",
"original-title": [],
"prefix": "10.1093",
"published": {
"date-parts": [
[
2022,
8,
9
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
9
]
]
},
"publisher": "Oxford University Press (OUP)",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://academic.oup.com/ajcn/advance-article/doi/10.1093/ajcn/nqac219/6659183"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Nutrition and Dietetics",
"Medicine (miscellaneous)"
],
"subtitle": [],
"title": "Long-term diet and risk of SARS -CoV-2 infection and Coronavirus Disease 2019 (COVID-19) severity",
"type": "journal-article"
}