Impact of Famotidine Use on Clinical Outcomes of Hospitalized Patients with COVID-19 in Taiwan: A Retrospective Study
et al., International Journal of Gerontology, doi:10.6890/IJGE.202307_17(3).0008, Jul 2023
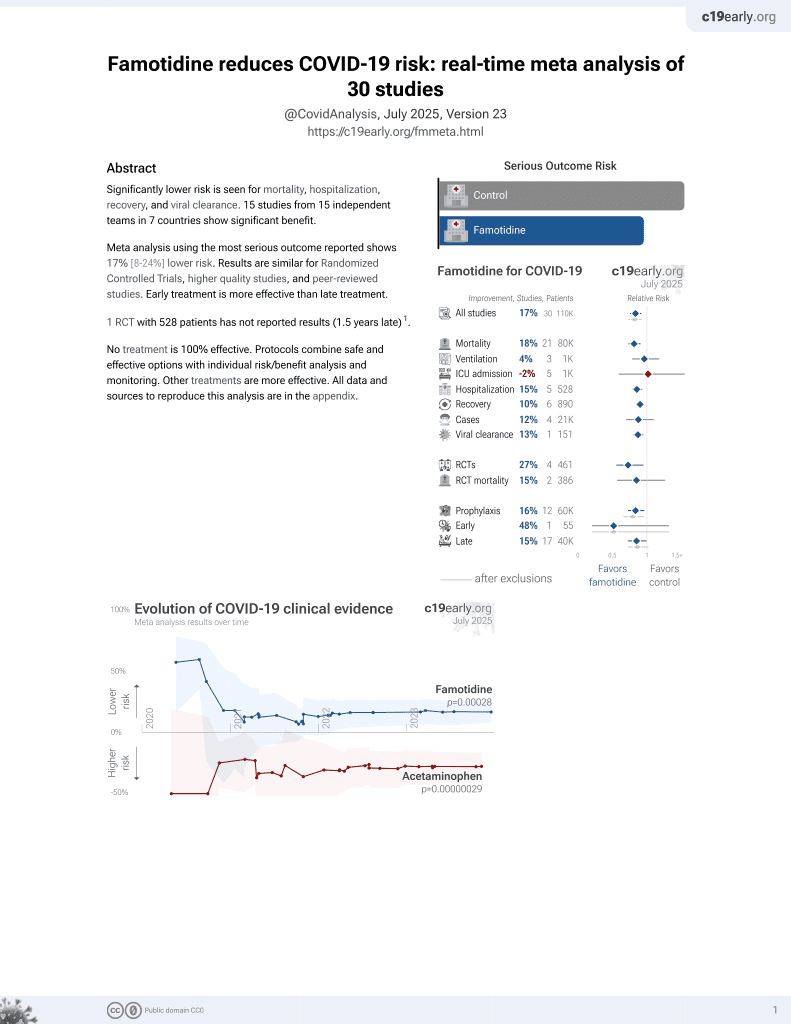
Famotidine for COVID-19
29th treatment shown to reduce risk in
October 2021, now with p = 0.00028 from 30 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 171 hospitalized patients in Taiwan, showing no signficant differences with famotidine, but a trend towards lower ICU admission. However, authors present only unadjusted results with groups that are not very comparable for ICU/mortality outcomes (e.g., 24% vs. 10% had ordinal score ≥5 at baseline), without mentioning the differences (they note only "confounding due of unobserved factors").
This study is excluded in meta-analysis:
significant unadjusted confounding factors.
Lin et al., 1 Jul 2023, retrospective, Taiwan, peer-reviewed, 4 authors, study period 1 May, 2021 - 31 August, 2021.
Impact of Famotidine Use on Clinical Outcomes of Hospitalized Patients with COVID-19 in Taiwan: A Retrospective Study
doi:10.6890/IJGE.202307_17(3).0008
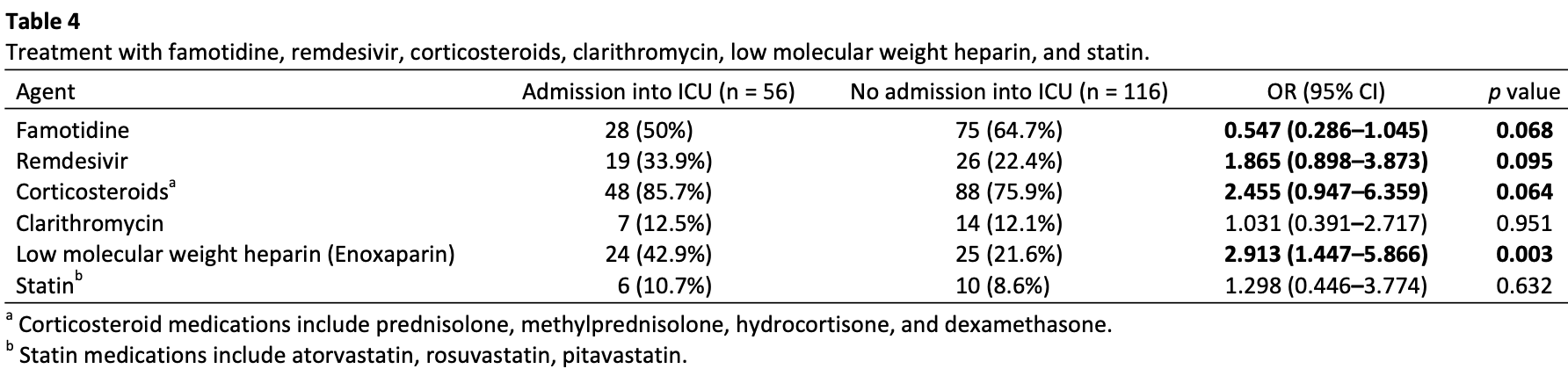
The aim of this study was to investigate the association between famotidine treatment and severity, as well as mortality, for patients with COVID-19. In addition, to investigate whether this association was changed in cases of concomitant treatment with corticosteroids, remdesivir, clarithromycin, low molecular weight heparin, or statin. Material and methods: This is a retrospective cohort study conducted by analyzing electronic medical records of 171 hospitalized patients into the Infectious Disease Ward of a 2068-bed tertiary care medical center, with laboratory-confirmed COVID-19 between May 01, 2021 and August 31, 2021. Patients were classified as receiving famotidine if they were treated with oral drug, at any dose, within ± 7 days of COVID-19 screening and/or hospital admission. Famotidine use was extracted directly from the electronic medical record. Results: Current study failed to identify famotidine as a protective factor associated with a significant reduction in the risk of in-hospital mortality (odds ratio 1.573, 95% confidence interval (CI) 0.464-5.325, p = 0.467) or a significant reduction in the risk of ICU admission (odds ratio 0.547, 95% confidence interval (CI) 0.286-1.045, p = 0.068). However, non-significant trend towards a lower rate of ICU admission in association with famotidine prescription was observed.
Conclusions: The results of this study reflect the real-world use of famotidine does not reduce the risk of in-hospital-mortality or ICU admission of hospitalized COVID-19 patients.
References
Anand, Ziebuhr, Wadhwani, Mesters, Hilgenfeld, Coronavirus main proteinase (3CLpro) structure: basis for design of anti-SARS drugs, Science, doi:10.1126/science.1085658
Birch, Molinar-Inglis, Trejo, Subcellular hot spots of GPCR signaling promote vascular inflammation, Curr Opin Endocr Metab Res, doi:10.1016/j.coemr.2020.07.011
Bourinbaiar, Fruhstorfer, The effect of histamine type 2 receptor antagonists on human immunodeficiency virus (HIV) replication: identification of a new class of antiviral agents, Life Sci, doi:10.1016/s0024-3205(96)00553-x
Cheung, Hung, Leung, Association between famotidine use and COVID-19 severity in Hong Kong: A territory-wide study, Gastroenterology, doi:10.1053/j.gastro.2020.05.098
Chiu, Shen, Lo, Effect of famotidine on hospitalized patients with COVID-19: A systematic review and meta-analysis, PLoS One, doi:10.1371/journal.pone.0259514
Freedberg, Conigliaro, Wang, Famotidine use is associated with improved clinical outcomes in hospitalized COVID-19 patients: A propensity score matched retrospective cohort study, Gastroenterology, doi:10.1053/j.gastro.2020.05.053
Harapan, Itoh, Yufika, Coronavirus disease 2019 (COVID-19): A literature review, J Infect Public Health, doi:10.1016/j.jiph.2020.03.019
Ii, Iii, Cannon, Dual-histamine receptor blockade with cetirizine -famotidine reduces pulmonary symptoms in COVID-19 patients, Pulm Pharmacol Ther, doi:10.1016/j.pupt.2020.101942
Kritas, Ronconi, Caraffa, Gallenga, Ross et al., Mast cells contribute to coronavirus-induced inflammation: new anti-inflammatory strategy, J Biol Regul Homeost Agents, doi:10.23812/20-Editorial-Kritas
Krystel-Whittemore, Dileepan, Wood, Mast cell: A multi-functional master cell, Front Immunol, doi:10.3389/fimmu.2015.00620
Kuno, So, Takahashi, Egorova, The association between famotidine and in-hospital mortality of patients with COVID-19, J Med Virol, doi:10.1002/jmv.27375
Lai, Shih, Ko, Tang, Hsueh, Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2020.105924
Li, Dong, Lei, No evidence indicates famotidine reduces the risk of serious disease in COVID-19 patients after propensity score matching: Meta-analysis and systematic reviews, Dig Dis Sci, doi:10.1007/s10620-021-07214-9
Malone, Tisdall, Smith, COVID-19: Famotidine, histamine, mast cells, and mechanisms, Front Pharmacol, doi:10.3389/fphar.2021.633680
Mather, Seip, Mckay, Impact of famotidine use on clinical outcomes of hospitalized patients with COVID-19, Am J Gastroenterol, doi:10.14309/ajg.0000000000000832
Shoaibi, Fortin, Weinstein, Berlin, Ryan, Comparative effectiveness of famotidine in hospitalized COVID-19 patients, Am J Gastroenterol, doi:10.14309/ajg.0000000000001153
Sun, Chen, Hu, Does famotidine reduce the risk of progression to severe disease, death, and intubation for COVID-19 patients? A systemic review and meta-analysis, Dig Dis Sci, doi:10.1007/s10620-021-06872-z
Wiersinga, Rhodes, Cheng, Peacock, Prescott, Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): A review, JAMA, doi:10.1001/jama.2020.12839
Wu, Liu, Yang, Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods, Acta Pharm Sin B, doi:10.1016/j.apsb.2020.02.008
DOI record:
{
"DOI": "10.6890/IJGE.202307_17(3).0008",
"ISSN": "1873-9598",
"URL": "",
"abstract": "Objectives: The aim of this study was to investigate the association between famotidine treatment and severity, as well as mortality, for patients with COVID-19. In addition, to investigate whether this association was changed in cases of concomitant treatment with corticosteroids, remdesivir, clarithromycin, low molecular weight heparin, or statin. Material and methods: This is a retrospective cohort study conducted by analyzing electronic medical records of 171 hospitalized patients into the Infectious Disease Ward of a 2068-bed tertiary care medical center, with laboratory-confirmed COVID-19 between May 01, 2021 and August 31, 2021. Patients were classified as receiving famotidine if they were treated with oral drug, at any dose, within ± 7 days of COVID-19 screening and/or hospital admission. Famotidine use was extracted directly from the electronic medical record. Results: Current study failed to identify famotidine as a protective factor associated with a significant reduction in the risk of in-hospital mortality (odds ratio 1.573, 95% confidence interval (CI) 0.464-5.325, p = 0.467) or a significant reduction in the risk of ICU admission (odds ratio 0.547, 95% confidence interval (CI) 0.286-1.045, p = 0.068). However, non-significant trend towards a lower rate of ICU admission in association with famotidine prescription was observed. Conclusions: The results of this study reflect the real-world use of famotidine does not reduce the risk of in-hospital-mortality or ICU admission of hospitalized COVID-19 patients.",
"author": [
{
"literal": "Hsiang-Ling Lin"
},
{
"literal": "Winter Yu-Ning Lee"
},
{
"literal": "Fang-Ju Sun"
},
{
"literal": "Ming-Wei Cheng"
}
],
"container-title": "International Journal of Gerontology",
"issue": "3",
"issued": {
"date-parts": [
[
"2023",
"7",
"1"
]
]
},
"language": "en",
"page-first": "183",
"title": "Impact of Famotidine Use on Clinical Outcomes of Hospitalized Patients with COVID-19 in Taiwan: A Retrospective Study",
"type": "article-journal",
"volume": "17"
}