Effects of Metformin on COVID-19 Patients with Type 2 Diabetes: A Retrospective Study
et al., Diabetes, Metabolic Syndrome and Obesity, doi:10.2147/DMSO.S417925, Aug 2023
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 571 type 2 diabetes patients with COVID-19 in China, showing lower combined mortality/mechanical ventilation with metformin.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
|
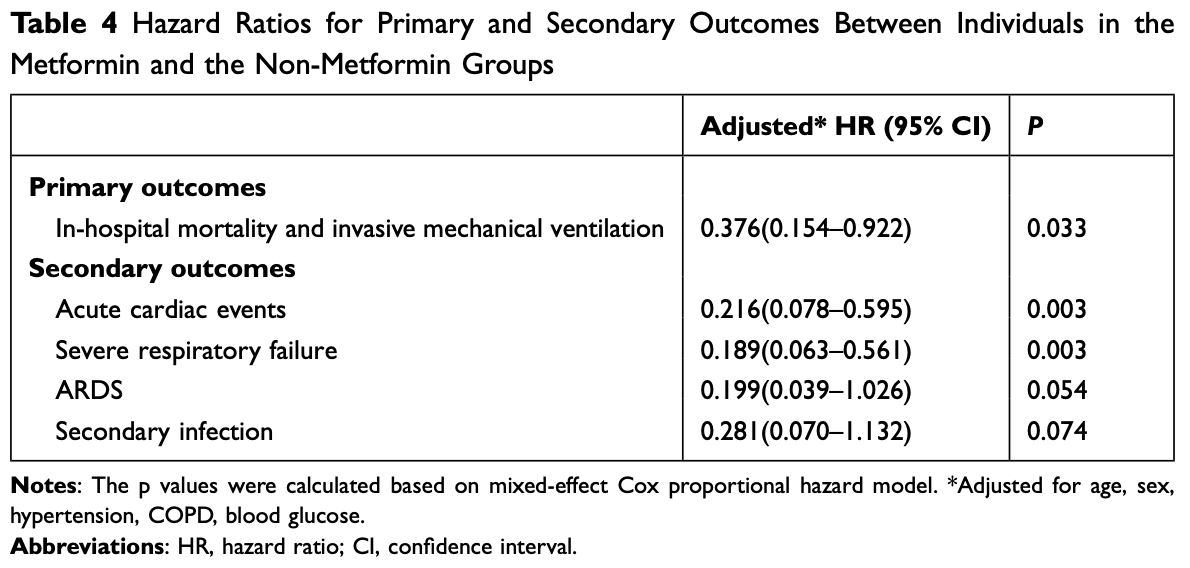
risk of death/intubation, 62.4% lower, HR 0.38, p = 0.03, treatment 241, control 330, adjusted per study, multivariable, Cox proportional hazards.
|
|
risk of progression, 81.1% lower, HR 0.19, p = 0.003, treatment 241, control 330, adjusted per study, severe respiratory failure, multivariable, Cox proportional hazards.
|
|
risk of progression, 80.1% lower, HR 0.20, p = 0.05, treatment 241, control 330, adjusted per study, ARDS, multivariable, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Guo et al., 24 Aug 2023, retrospective, China, peer-reviewed, median age 65.0, 8 authors, study period 4 February, 2020 - 11 April, 2020.
Contact: mdjingangzheng@yeah.net.
Effects of Metformin on COVID-19 Patients with Type 2 Diabetes: A Retrospective Study
Diabetes, Metabolic Syndrome and Obesity, doi:10.2147/dmso.s417925
The pandemic of coronavirus disease 2019 (COVID-19) has highlighted the intricate relationship between underlying conditions and death. We designed this study to determine whether metformin therapy for type 2 diabetes mellitus (T2D) is associated with low in-hospital mortality in patients hospitalized for COVID-19. Materials and Methods: This was a retrospective study including patients with COVID-19 and T2D in Wuhan, from February 4th to April 11th, 2020. Patients were divided into two groups according to metformin exposure. The hazard ratio (HR) of COVID-19-related mortality and invasive mechanical ventilation was estimated using Cox regression. Results: There were 571 T2D patients among the 4330 confirmed COVID-19 patients. Of those patients, 241 received metformin therapy. The in-hospital mortality and invasive mechanical ventilation of metformin group was lower than non-metformin group. In the multivariate model, metformin use was linked to a decreased in-hospital mortality and invasive mechanical ventilation when compared with that of the control group (HR: 0.376 [95% CI 0.154-0.922]; P = 0.033).
Conclusion: Our study indicated that metformin therapy was associated with decreased death risk in COVID-19 patients with T2D.
Abbreviations T2D, type 2 diabetes mellitus; COVID-19, coronavirus disease 2019; HR, hazard ratio; SARA-COV-2, severe acute respiratory syndrome coronavirus 2; ACE2, angiotensin-converting enzyme 2; AMPK, 5'-AMP-activated protein kinase; DPP4, dipeptidyl peptidase-4; CK-MB, creatine kinase-myocardial band; ALT, alanine aminotransferase; LDH, lactic https://doi.org/10.2147/DMSO.S417925
DovePress Diabetes, Metabolic Syndrome and Obesity 2023:16
Disclosure The authors declare that they have no known competing commercial or financial relationships that could have appeared to influence the work reported in this paper.
References
Apicella, Campopiano, Mantuano, COVID-19 in people with diabetes: understanding the reasons for worse outcomes, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30238-2
Bornstein, Rubino, Khunti, Practical recommendations for the management of diabetes in patients with COVID-19, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30152-2
Bramante, Huling, Tignanelli, Randomized trial of metformin, ivermectin, and fluvoxamine for Covid-19, N Engl J Med, doi:10.1056/NEJMoa2201662
Bramante, The COVID-OUT study: a randomized, double-blind, placebo-controlled trial of metformin for the treatment of COVID-19 sequelae
Buse, Wexler, Tsapas, 2019 update to: management of hyperglycaemia in type 2 diabetes, doi:10.1007/s00125-019-05039-w
Cariou, Hadjadj, Wargny, Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Ceriello, Hyperglycemia and the worse prognosis of COVID-19. Why a fast blood glucose control should be mandatory, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108186
Cheng, Liu, Li, Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and Pre-existing type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.08.013
Crouse, Grimes, Li, Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes, Front Endocrinol, doi:10.3389/fendo.2020.600439
Hashemi, Pezeshki, Repurposing metformin for covid-19 complications in patients with type 2 diabetes and insulin resistance, Immunopharmacol Immunotoxicol, doi:10.1080/08923973.2021.1925294
Iacobellis, Penaherrera, Bermudez, Admission hyperglycemia and radiological findings of SARS-CoV2 in patients with and without diabetes, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108185
Nguyen, Ho, Nguyen, Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: a meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155196
Remuzzi, Remuzzi, COVID-19 and Italy: what next?, Lancet, doi:10.1016/S0140-6736(20)30627-9
Richardson, Hirsch, Narasimhan, Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area, JAMA, doi:10.1001/jama.2020.6775
Roca-Ho, Riera, Palau, Characterization of ACE and ACE2 expression within different organs of the NOD mouse, Int J Mol Sci, doi:10.3390/ijms18030563
Sancho-López, Caballero-Bermejo, Ruiz-Antorán, Efficacy and safety of sarilumab in patients with COVID19 pneumonia: a randomized, phase III clinical trial (SARTRE study), Infect Dis Ther
Sharma, Ray, Sadasivam, Metformin in COVID-19: a possible role beyond diabetes, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108183
Singh, Khunti, Assessment of risk, severity, mortality, glycemic control and antidiabetic agents in patients with diabetes and COVID-19: a narrative review, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108266
Targher, Mantovani, Wang, Patients with diabetes are at higher risk for severe illness from COVID-19, Diabetes Metab, doi:10.1016/j.diabet.2020.05.001
Ursini, Ciaffi, Landini, COVID-19 and diabetes: is metformin a friend or foe?, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108167
Wang, Cooper, Gokhale, Association of metformin with susceptibility to COVID-19 in people with type 2 diabetes, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab067
Yu, Li, Sun, Insulin treatment is associated with increased mortality in patients with COVID-19 and type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.11.014
Zhang, Dong, Martin, AMP-activated protein kinase phosphorylation of angiotensin-converting enzyme 2 in endothelium mitigates pulmonary hypertension, Am J Respir Crit Care Med, doi:10.1164/rccm.201712-2570OC
Zhang, Qin, Cheng, In-hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19, Cell Metab, doi:10.1016/j.cmet.2020.06.015
Zhu, She, Cheng, Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.04.021
DOI record:
{
"DOI": "10.2147/dmso.s417925",
"ISSN": [
"1178-7007"
],
"URL": "http://dx.doi.org/10.2147/DMSO.S417925",
"author": [
{
"affiliation": [],
"family": "Guo",
"given": "Ziyu",
"sequence": "first"
},
{
"affiliation": [],
"family": "Gao",
"given": "Yanxiang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xie",
"given": "Enmin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ye",
"given": "Zixiang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Yike",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhao",
"given": "Xuecheng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shen",
"given": "Nan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zheng",
"given": "Jingang",
"sequence": "additional"
}
],
"container-title": "Diabetes, Metabolic Syndrome and Obesity",
"container-title-short": "DMSO",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
8,
24
]
],
"date-time": "2023-08-24T02:00:12Z",
"timestamp": 1692842412000
},
"deposited": {
"date-parts": [
[
2023,
8,
24
]
],
"date-time": "2023-08-24T02:00:17Z",
"timestamp": 1692842417000
},
"indexed": {
"date-parts": [
[
2023,
8,
24
]
],
"date-time": "2023-08-24T04:24:26Z",
"timestamp": 1692851066943
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
8
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/3.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
8,
1
]
],
"date-time": "2023-08-01T00:00:00Z",
"timestamp": 1690848000000
}
}
],
"link": [
{
"URL": "https://www.dovepress.com/getfile.php?fileID=92248",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.dovepress.com/getfile.php?fileID=92248",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "2573-2582",
"prefix": "10.2147",
"published": {
"date-parts": [
[
2023,
8
]
]
},
"published-online": {
"date-parts": [
[
2023,
8
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.1016/S2213-8587(20)30238-2",
"author": "Apicella",
"doi-asserted-by": "publisher",
"first-page": "782",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "ref1",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.6775",
"author": "Richardson",
"doi-asserted-by": "publisher",
"first-page": "2052",
"journal-title": "JAMA",
"key": "ref2",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.04.021",
"author": "Zhu",
"doi-asserted-by": "publisher",
"first-page": "1068",
"journal-title": "Cell Metab",
"key": "ref3",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2020.05.001",
"author": "Targher",
"doi-asserted-by": "publisher",
"first-page": "335",
"journal-title": "Diabetes Metab",
"key": "ref4",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108266",
"author": "Singh",
"doi-asserted-by": "publisher",
"first-page": "108266",
"journal-title": "Diabetes Res Clin Pract",
"key": "ref5",
"volume": "165",
"year": "2020"
},
{
"DOI": "10.1007/s00125-019-05039-w",
"author": "Buse",
"doi-asserted-by": "publisher",
"first-page": "221",
"journal-title": "Diabetologia",
"key": "ref6",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.08.013",
"author": "Cheng",
"doi-asserted-by": "publisher",
"first-page": "537",
"journal-title": "Cell Metab",
"key": "ref7",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1080/08923973.2021.1925294",
"author": "Hashemi",
"doi-asserted-by": "publisher",
"first-page": "265",
"journal-title": "Immunopharmacol Immunotoxicol",
"key": "ref8",
"volume": "43",
"year": "2021"
},
{
"DOI": "10.1016/j.diabres.2020.108183",
"author": "Sharma",
"doi-asserted-by": "publisher",
"first-page": "108183",
"journal-title": "Diabetes Res Clin Pract",
"key": "ref9",
"volume": "164",
"year": "2020"
},
{
"DOI": "10.1164/rccm.201712-2570OC",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "509",
"journal-title": "Am J Respir Crit Care Med",
"key": "ref10",
"volume": "198",
"year": "2018"
},
{
"key": "ref11",
"unstructured": "Bramante C. The COVID-OUT study: a randomized, double-blind, placebo-controlled trial of metformin for the treatment of COVID-19 sequelae. medRxiv; 2021."
},
{
"DOI": "10.1016/j.cmet.2020.11.014",
"author": "Yu",
"doi-asserted-by": "publisher",
"first-page": "65",
"journal-title": "Cell Metab",
"key": "ref12",
"volume": "33",
"year": "2021"
},
{
"author": "Sancho-López",
"first-page": "1",
"journal-title": "Infect Dis Ther",
"key": "ref13",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.1016/j.cmet.2020.06.015",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "176",
"journal-title": "Cell Metab",
"key": "ref14",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30627-9",
"author": "Remuzzi",
"doi-asserted-by": "publisher",
"first-page": "1225",
"journal-title": "Lancet",
"key": "ref15",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108185",
"author": "Iacobellis",
"doi-asserted-by": "publisher",
"first-page": "108185",
"journal-title": "Diabetes Res Clin Pract",
"key": "ref16",
"volume": "164",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30152-2",
"author": "Bornstein",
"doi-asserted-by": "publisher",
"first-page": "546",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "ref17",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1007/s00125-020-05180-x",
"author": "Cariou",
"doi-asserted-by": "publisher",
"first-page": "1500",
"journal-title": "Diabetologia",
"key": "ref18",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.3389/fendo.2020.600439",
"author": "Crouse",
"doi-asserted-by": "publisher",
"first-page": "600439",
"journal-title": "Front Endocrinol",
"key": "ref19",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.metabol.2022.155196",
"author": "Nguyen",
"doi-asserted-by": "publisher",
"first-page": "155196",
"journal-title": "Metabolism",
"key": "ref20",
"volume": "131",
"year": "2022"
},
{
"DOI": "10.1210/clinem/dgab067",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "1255",
"journal-title": "J Clin Endocrinol Metab",
"key": "ref21",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2201662",
"author": "Bramante",
"doi-asserted-by": "publisher",
"first-page": "599",
"journal-title": "N Engl J Med",
"key": "ref22",
"volume": "387",
"year": "2022"
},
{
"DOI": "10.1016/j.diabres.2020.108186",
"author": "Ceriello",
"doi-asserted-by": "publisher",
"first-page": "108186",
"journal-title": "Diabetes Res Clin Pract",
"key": "ref23",
"volume": "163",
"year": "2020"
},
{
"DOI": "10.3390/ijms18030563",
"author": "Roca-Ho",
"doi-asserted-by": "publisher",
"first-page": "563",
"journal-title": "Int J Mol Sci",
"key": "ref24",
"volume": "18",
"year": "2017"
},
{
"DOI": "10.1016/j.diabres.2020.108167",
"author": "Ursini",
"doi-asserted-by": "publisher",
"first-page": "108167",
"journal-title": "Diabetes Res Clin Pract",
"key": "ref25",
"volume": "164",
"year": "2020"
}
],
"reference-count": 25,
"references-count": 25,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.dovepress.com/effects-of-metformin-on-covid-19-patients-with-type-2-diabetes-a-retro-peer-reviewed-fulltext-article-DMSO"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology",
"Internal Medicine"
],
"subtitle": [],
"title": "Effects of Metformin on COVID-19 Patients with Type 2 Diabetes: A Retrospective Study",
"type": "journal-article",
"volume": "Volume 16"
}
