Clinical progression and outcomes of patients hospitalized with COVID-19 in humanitarian settings: A prospective cohort study in South Sudan and Eastern Democratic Republic of the Congo
et al., PLOS Global Public Health, doi:10.1371/journal.pgph.0000924, NCT04568499, Oct 2022
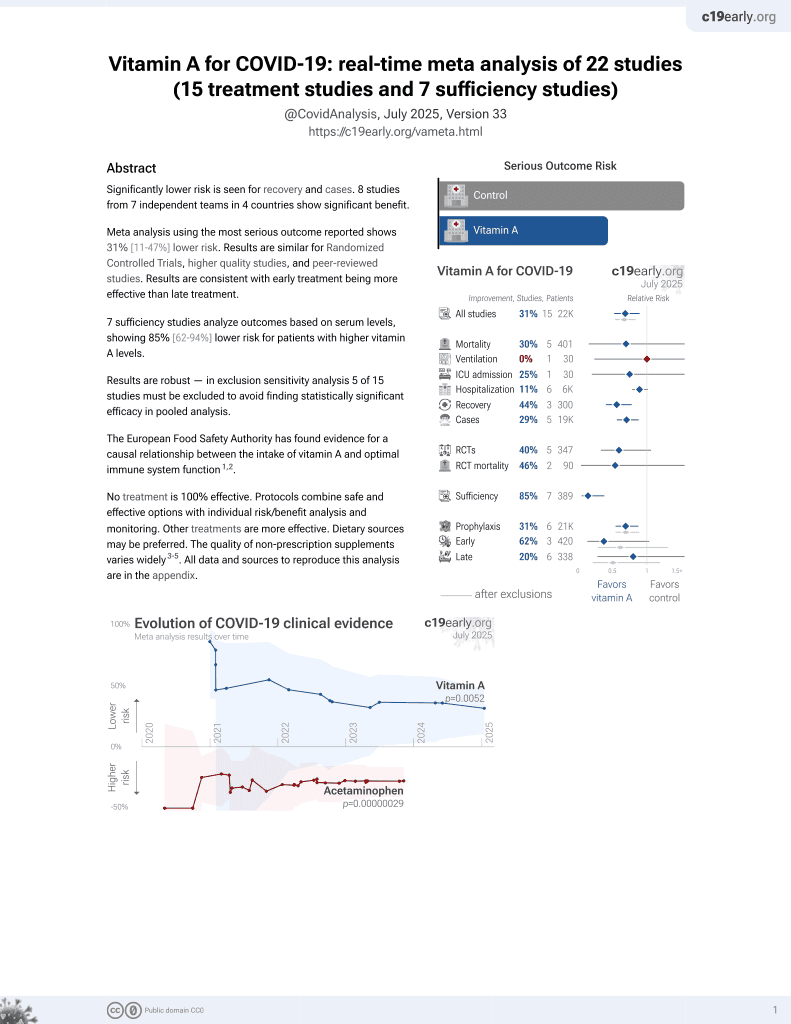
Vitamin A for COVID-19
49th treatment shown to reduce risk in
May 2023, now with p = 0.004 from 14 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Prospective study of 144 hospitalized COVID-19 patients in the DRC and South Sudan, showing no significant difference with vitamin A treatment in unadjusted results with only 8 patients receiving vitamin A.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
|
risk of death, 26.1% lower, RR 0.74, p = 1.00, treatment 1 of 8 (12.5%), control 23 of 136 (16.9%), NNT 23, unadjusted.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Doocy et al., 19 Oct 2022, prospective, multiple countries, peer-reviewed, 6 authors, study period December 2020 - June 2021, average treatment delay 7.8 days, trial NCT04568499 (history).
Contact: doocy1@jhu.edu.
Clinical progression and outcomes of patients hospitalized with COVID-19 in humanitarian settings: A prospective cohort study in South Sudan and Eastern Democratic Republic of the Congo
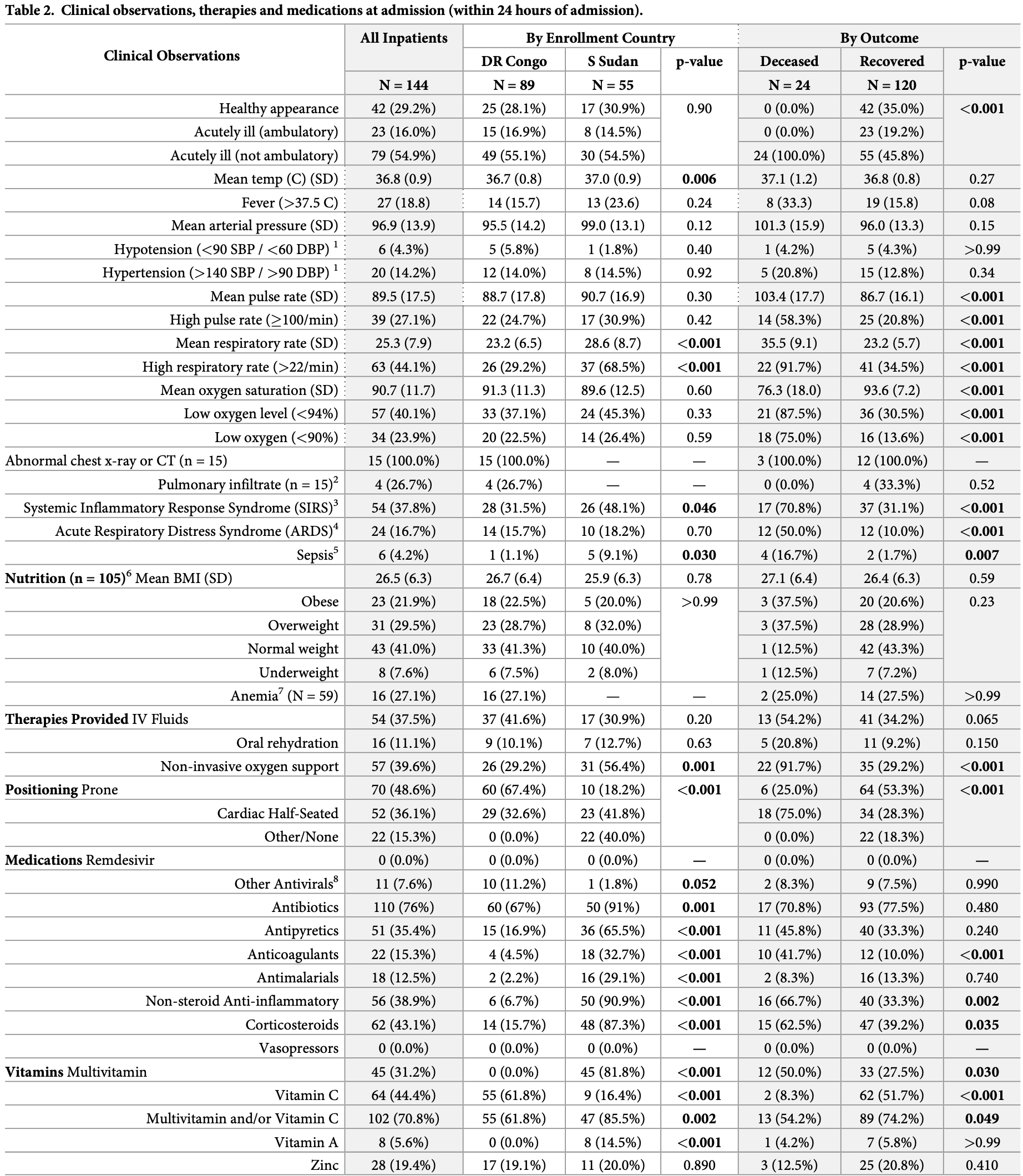
PLOS Global Public Health, doi:10.1371/journal.pgph.0000924
Little information is available on COVID-19 in Africa and virtually none is from humanitarian and more resource-constrained settings. This study characterizes hospitalized patients in the African humanitarian contexts of Juba, South Sudan and North and South Kivu in Eastern Democratic Republic of the Congo. This observational cohort was conducted between December 2020 and June 2021. Patients presenting for care at five facilities or referred from home-based care by mobile medical teams were eligible for enrollment and followed until death or recovery. Disease progression was characterized for hospitalized patients using survival analysis and mixed effects regression model to estimate survival odds for patient characteristics and treatments received. 144 COVID-19 cases enrolled as hospitalized patients were followed to recovery/death. The observed mortality proportion among hospitalized patients was 16.7% (CI: 11.2-23.3%); mortality was three times higher in South Sudan, where patients presented later after symptom onset and in worse conditions. Age and diabetes history were the only patient characteristics associated with decreased survival; clinical status indicators associated with decreased survival included fever, low oxygen level, elevated respiratory and pulse rates. The only therapy associated with survival was non-invasive oxygen; invasive oxygen therapies and other specialized treatments were rarely received. Improving availability of oxygen monitoring and proven COVID-19 therapies in humanitarian and resource-poor settings is critical for health equity. Customizing training to reflect availability of specific medications, therapies and operational constraints is particularly important given the range of challenges faced by providers in these settings.
Supporting information
S1
References
Achan, Serwanga, Wanzira, Kyagulanyi, Nuwa et al., a prospective cohort study
Bahl, Van Baalen, Ortiz, Chen, Todd et al., Early predictors of in-hospital mortality in patients with COVID-19 in a large American cohort, Intern Emerg Med, doi:10.1007/s11739-020-02509-7
Berendes, Lako, Whitson, Gould, Valadez, Assessing the quality of care in a new nation: South Sudan's first national health facility assessment, Trop Med Intl Health, doi:10.1111/tmi.12363
Chanda, Minchella, Kampamba, Itoh, Hines et al., COVID-19 Severity and COVID-19-Associated Deaths Among Hospitalized Patients with HIV Infection-Zambia, March-December 2020, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm7022a2
Dessie, Zewotir, Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients, BMC Infect Dis, doi:10.1186/s12879-021-06536-3
Dong, Li, Ding, Liu, Tang et al., HIV infection and risk of COVID-19 mortality: A metaanalysis, Medicine, doi:10.1097/MD.0000000000026573
Hariyanto, Kurniawan, Anemia is associated with severe coronavirus disease 2019 (COVID-19) infection, Transfus Apher Sci, doi:10.1016/j.transci.2020.102926
Hiscock, Kumar, Simmons, Systematic review and meta-analysis of method comparison studies of Masimo pulse co-oximeters (Radical-7 or Pronto-7) and HemoCue(R) absorption spectrometers (B-Hemoglobin or 201+) with laboratory haemoglobin estimation, Anaesth Intensive Care, doi:10.1177/0310057X1504300310
Kakodkar, Kaka, Baig, A Comprehensive Literature Review on the Clinical Presentation, and Management of the Pandemic Coronavirus Disease 2019 (COVID-19), Cureus, doi:10.7759/cureus.7560
Katchunga, Murhula, Akilimali, Zaluka, Karhikalembu et al., Seroprevalence of anti-SARS-CoV-2 antibodies among travelers and workers screened at the Saint Luc clinic in Bukavu, eastern Democratic Republic of the Congo, from May to August 2020, Pan African Medical Journal, doi:10.11604/pamj.2021.38.93.26663
Leidman, Doocy, Heymsfield, Sebushishe, Ngole et al., Risk Factors for Hospitalization and Death from COVID-19 in South Sudan and Eastern Democratic Republic of the Congo
Macedo, Gonc ¸alves, Febra, COVID-19 fatality rates in hospitalized patients: systematic review and meta-analysis, Ann Epidemiol, doi:10.1016/j.annepidem.2021.02.012
Majer, Udoh, Baleke, Ahmed, Kumar et al., Eastern Democratic Republic of the Congo
Makulo, Mandina, Mbala, Wumba, Akilmali et al., SARS-CoV2 infection in symptomatic patients: interest of serological tests and predictors of mortality: experience of DR Congo, BMC Infect Dis, doi:10.1186/s12879-021-07003-9
Milani, Macchi, Guz-Mark, Vitamin C in the Treatment of COVID-19, Nutrients, doi:10.3390/nu13041172
Nandy, Salunke, Pathak, Pandey, Doctor et al., Coronavirus disease (COVID-19): A systematic review and meta-analysis to evaluate the impact of various comorbidities on serious events, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.06.064
Nlandu, Mafuta, Sakaji, Brecknell, Engole et al., Predictors of mortality in COVID-19 patients at Kinshasa Medical Center and a survival analysis: a retrospective cohort study, BMC Infect Dis, doi:10.1186/s12879-021-06984-x
Rawat, Roy, Maitra, Gulati, Khanna et al., Vitamin C and COVID-19 treatment: A systematic review and meta-analysis of randomized controlled trials, Diabetes & Metabolic Syndrome, doi:10.1016/j.dsx.2021.102324
Richardson, Hirsch, Narasimhan, Crawford, Mcginn et al., Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area, JAMA, doi:10.1001/jama.2020.6775
Schuetz, Gregoriano, Keller, Supplementation of the population during the COVID-19 pandemic with vitamins and micronutrients-how much evidence is needed?, Swiss Med Wkly, doi:10.4414/smw.2021.20522
Valle, Kim-Schulze, Huang, Beckman, Nirenburg et al., An inflammatory cytokine signature predicts COVID-19 severity and survival, Nature Medicine, doi:10.1038/s41591-020-1051-9
Whitehead, Mei, Mapango, Jefferds, Methods and analyzers for hemoglobin measurement in clinical laboratories and field settings, Annals of the New York Academy of Sciences
Wiens, Mawien, Rumunu, Slater, Jones et al., Seroprevalence of Severe Acute Respiratory Syndrome Coronavirus 2 IgG in Juba, South Sudan, 2020 1, Emerg Infect Dis, doi:10.3201/eid2706.210568
Zhang, Rao, Li, Yuan, Liu et al., Pilot trial of high-dose vitamin C in critically ill COVID-19 patients, Ann Intensive Care, doi:10.1186/s13613-020-00792-3
DOI record:
{
"DOI": "10.1371/journal.pgph.0000924",
"ISSN": [
"2767-3375"
],
"URL": "http://dx.doi.org/10.1371/journal.pgph.0000924",
"abstract": "<jats:p>Little information is available on COVID-19 in Africa and virtually none is from humanitarian and more resource-constrained settings. This study characterizes hospitalized patients in the African humanitarian contexts of Juba, South Sudan and North and South Kivu in Eastern Democratic Republic of the Congo. This observational cohort was conducted between December 2020 and June 2021. Patients presenting for care at five facilities or referred from home-based care by mobile medical teams were eligible for enrollment and followed until death or recovery. Disease progression was characterized for hospitalized patients using survival analysis and mixed effects regression model to estimate survival odds for patient characteristics and treatments received. 144 COVID-19 cases enrolled as hospitalized patients were followed to recovery/death. The observed mortality proportion among hospitalized patients was 16.7% (CI: 11.2–23.3%); mortality was three times higher in South Sudan, where patients presented later after symptom onset and in worse conditions. Age and diabetes history were the only patient characteristics associated with decreased survival; clinical status indicators associated with decreased survival included fever, low oxygen level, elevated respiratory and pulse rates. The only therapy associated with survival was non-invasive oxygen; invasive oxygen therapies and other specialized treatments were rarely received. Improving availability of oxygen monitoring and proven COVID-19 therapies in humanitarian and resource-poor settings is critical for health equity. Customizing training to reflect availability of specific medications, therapies and operational constraints is particularly important given the range of challenges faced by providers in these settings.</jats:p>",
"author": [
{
"ORCID": "http://orcid.org/0000-0003-2363-7998",
"affiliation": [],
"authenticated-orcid": true,
"family": "Doocy",
"given": "Shannon",
"sequence": "first"
},
{
"affiliation": [],
"family": "Bollemeijer",
"given": "Iris",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4191-5931",
"affiliation": [],
"authenticated-orcid": true,
"family": "Leidman",
"given": "Eva",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3010-9790",
"affiliation": [],
"authenticated-orcid": true,
"family": "Sebushishe",
"given": "Abdou",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8911-0684",
"affiliation": [],
"authenticated-orcid": true,
"family": "Mbong",
"given": "Eta Ngole",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6859-1973",
"affiliation": [],
"authenticated-orcid": true,
"family": "Page",
"given": "Kathleen",
"sequence": "additional"
}
],
"container-title": "PLOS Global Public Health",
"container-title-short": "PLOS Glob Public Health",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosglobalpublichealth.org"
]
},
"created": {
"date-parts": [
[
2022,
10,
19
]
],
"date-time": "2022-10-19T17:26:37Z",
"timestamp": 1666200397000
},
"deposited": {
"date-parts": [
[
2022,
10,
19
]
],
"date-time": "2022-10-19T17:27:22Z",
"timestamp": 1666200442000
},
"editor": [
{
"affiliation": [],
"family": "Ratnayake",
"given": "Ruwan",
"sequence": "first"
}
],
"funder": [
{
"DOI": "10.13039/100000200",
"award": [
"72OFDA20GR0221"
],
"doi-asserted-by": "publisher",
"name": "United States Agency for International Development"
}
],
"indexed": {
"date-parts": [
[
2022,
10,
20
]
],
"date-time": "2022-10-20T05:13:48Z",
"timestamp": 1666242828326
},
"is-referenced-by-count": 0,
"issue": "10",
"issued": {
"date-parts": [
[
2022,
10,
19
]
]
},
"journal-issue": {
"issue": "10",
"published-online": {
"date-parts": [
[
2022,
10,
19
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/publicdomain/zero/1.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
10,
19
]
],
"date-time": "2022-10-19T00:00:00Z",
"timestamp": 1666137600000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pgph.0000924",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0000924",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2022,
10,
19
]
]
},
"published-online": {
"date-parts": [
[
2022,
10,
19
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"author": "World Health Organization",
"first-page": "2021",
"journal-title": "COVID-19 Dashboard. URL",
"key": "pgph.0000924.ref001",
"volume": "21"
},
{
"key": "pgph.0000924.ref002",
"unstructured": "World Health Organization (WHO). The Global Health Observatory Data Repository. Population Estimates by WHO Region. URL: https://apps.who.int/gho/data/view.main.POP2020. Accessed Aug 21, 2021."
},
{
"article-title": "Seroprevalence of anti-SARS-CoV-2 antibodies among travelers and workers screened at the Saint Luc clinic in Bukavu, eastern Democratic Republic of the Congo, from May to August 2020",
"author": "PB Katchunga",
"first-page": "93",
"journal-title": "Pan African Medical Journal",
"key": "pgph.0000924.ref003",
"volume": "38",
"year": "2021"
},
{
"DOI": "10.3201/eid2706.210568",
"article-title": "Seroprevalence of Severe Acute Respiratory Syndrome Coronavirus 2 IgG in Juba, South Sudan, 20201",
"author": "KE Wiens",
"doi-asserted-by": "crossref",
"first-page": "1598",
"issue": "6",
"journal-title": "Emerg Infect Dis",
"key": "pgph.0000924.ref004",
"volume": "27",
"year": "2021"
},
{
"key": "pgph.0000924.ref005",
"unstructured": "The World Bank. Open Data on physicians and hospital beds by country. Available at https://data.worldbank.org/indicator/SH.MED.PHYS.ZS and https://data.worldbank.org/indicator/ SH.MED.BEDS.ZS. Accessed Aug 22, 2021."
},
{
"key": "pgph.0000924.ref006",
"unstructured": "World Health Organization (WHO) Global Health Work force Alliance. South Sudan Country Profile. URL: https://www.who.int/workforcealliance/countries/ssd/en/. Accessed Aug 22, 2021."
},
{
"DOI": "10.1111/tmi.12363",
"article-title": "Assessing the quality of care in a new nation: South Sudan’s first national health facility assessment",
"author": "S Berendes",
"doi-asserted-by": "crossref",
"issue": "10",
"journal-title": "Trop Med Intl Health",
"key": "pgph.0000924.ref007",
"volume": "19",
"year": "2014"
},
{
"DOI": "10.1016/S0140-6736(21)00441-4",
"article-title": "Patient care and clinical outcomes for patients with COVID-19 infection admitted to African high-care or intensive care units (ACCCOS): a multicentre, prospective, observational cohort study",
"author": "The African COVID-19 Critical Care Outcomes Study (ACCOS) Investigators",
"doi-asserted-by": "crossref",
"first-page": "1885",
"journal-title": "Lancet",
"key": "pgph.0000924.ref008",
"volume": "397",
"year": "2021"
},
{
"article-title": "Risk Factors for Hospitalization and Death from COVID-19 in South Sudan and Eastern Democratic Republic of the Congo.",
"author": "E Leidman",
"journal-title": "Manuscript under review.",
"key": "pgph.0000924.ref009"
},
{
"article-title": "Methods and analyzers for hemoglobin measurement in clinical laboratories and field settings",
"author": "RD Whitehead",
"journal-title": "Annals of the New York Academy of Sciences",
"key": "pgph.0000924.ref010",
"year": "2019"
},
{
"DOI": "10.1177/0310057X1504300310",
"article-title": "Systematic review and meta-analysis of method comparison studies of Masimo pulse co-oximeters (Radical-7 or Pronto-7) and HemoCue(R) absorption spectrometers (B-Hemoglobin or 201+) with laboratory haemoglobin estimation.",
"author": "R Hiscock",
"doi-asserted-by": "crossref",
"first-page": "341",
"issue": "3",
"journal-title": "Anaesth Intensive Care.",
"key": "pgph.0000924.ref011",
"volume": "43",
"year": "2015"
},
{
"key": "pgph.0000924.ref012",
"unstructured": "World Health Organization (WHO). Growth reference data for children 5–19 years. URL: https://www.who.int/toolkits/growth-reference-data-for-5to19-years/indicators/bmi-for-age."
},
{
"key": "pgph.0000924.ref013",
"unstructured": "World Health Organization (WHO). The Global Health Observatory Data Repository. Body Mass Index (BMI). URL: https://apps.who.int/gho/data/node.main.BMIANTHROPOMETRY?lang=en. Accessed July 14, 2021."
},
{
"key": "pgph.0000924.ref014",
"unstructured": "World Health Organization (WHO). Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. WHO/NMH/NHD/MNM/11.1. 2011. Available at URL: https://www.who.int/vmnis/indicators/haemoglobin.pdf."
},
{
"article-title": "Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients.",
"author": "ZG Dessie",
"first-page": "855",
"issue": "1",
"journal-title": "Published 2021 Aug 21",
"key": "pgph.0000924.ref015",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1016/j.annepidem.2021.02.012",
"article-title": "COVID-19 fatality rates in hospitalized patients: systematic review and meta-analysis.",
"author": "A Macedo",
"doi-asserted-by": "crossref",
"first-page": "14",
"journal-title": "Ann Epidemiol",
"key": "pgph.0000924.ref016",
"volume": "57",
"year": "2021"
},
{
"article-title": "Operational challenges and considerations for COVID-19 research in humanitarian settings: A qualitative study of a project in South Sudan and Eastern Democratic Republic of the Congo.",
"author": "J Majer",
"journal-title": "Manuscript in press.",
"key": "pgph.0000924.ref017"
},
{
"DOI": "10.1186/s12879-021-07003-9",
"article-title": "SARS-CoV2 infection in symptomatic patients: interest of serological tests and predictors of mortality: experience of DR Congo.",
"author": "JR Makulo",
"doi-asserted-by": "crossref",
"first-page": "21",
"journal-title": "BMC Infect Dis",
"key": "pgph.0000924.ref018",
"volume": "22",
"year": "2022"
},
{
"DOI": "10.1186/s12879-021-06984-x",
"article-title": "Predictors of mortality in COVID-19 patients at Kinshasa Medical Center and a survival analysis: a retrospective cohort study.",
"author": "Y Nlandu",
"doi-asserted-by": "crossref",
"first-page": "1272",
"journal-title": "BMC Infect Dis",
"key": "pgph.0000924.ref019",
"volume": "21",
"year": "2021"
},
{
"key": "pgph.0000924.ref020",
"unstructured": "Centers for Disease Control and Prevention. People with certain medical conditions. Updated March 29, 2021. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed April 8, 2021."
},
{
"DOI": "10.1016/j.dsx.2020.06.064",
"article-title": "Coronavirus disease (COVID-19): A systematic review and meta-analysis to evaluate the impact of various comorbidities on serious events.",
"author": "K Nandy",
"doi-asserted-by": "crossref",
"first-page": "1017",
"issue": "5",
"journal-title": "Diabetes Metab Syndr 2020",
"key": "pgph.0000924.ref021",
"volume": "14"
},
{
"DOI": "10.1097/MD.0000000000026573",
"article-title": "HIV infection and risk of COVID-19 mortality: A meta-analysis.",
"author": "Y Dong",
"doi-asserted-by": "crossref",
"first-page": "e26573",
"issue": "26",
"journal-title": "Medicine",
"key": "pgph.0000924.ref022",
"volume": "100",
"year": "2021"
},
{
"DOI": "10.15585/mmwr.mm7022a2",
"article-title": "COVID-19 Severity and COVID-19–Associated Deaths Among Hospitalized Patients with HIV Infection---Zambia, March–December 2020.",
"author": "D Chanda",
"doi-asserted-by": "crossref",
"first-page": "807",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "pgph.0000924.ref023",
"volume": "70",
"year": "2021"
},
{
"article-title": "Impact of current malaria infection and previous malaria exposure on the clinical profiles and outcome of COVID-19 in a high malaria transmission setting: a prospective cohort study",
"author": "J Achan",
"journal-title": "Lancet prepreint.",
"key": "pgph.0000924.ref024"
},
{
"DOI": "10.1016/j.transci.2020.102926",
"article-title": "Anemia is associated with severe coronavirus disease 2019 (COVID-19) infection.",
"author": "TI Hariyanto",
"doi-asserted-by": "crossref",
"first-page": "102926",
"issue": "6",
"journal-title": "Transfus Apher Sci",
"key": "pgph.0000924.ref025",
"volume": "59",
"year": "2020"
},
{
"article-title": "A Comprehensive Literature Review on the Clinical Presentation, and Management of the Pandemic Coronavirus Disease 2019 (COVID-19).",
"author": "P Kakodkar",
"first-page": "e7560",
"issue": "4",
"journal-title": "Cureus",
"key": "pgph.0000924.ref026",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.6775",
"article-title": "Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area",
"author": "S Richardson",
"doi-asserted-by": "crossref",
"first-page": "2052",
"issue": "20",
"journal-title": "JAMA",
"key": "pgph.0000924.ref027",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1007/s11739-020-02509-7",
"article-title": "Early predictors of in-hospital mortality in patients with COVID-19 in a large American cohort.",
"author": "A Bahl",
"doi-asserted-by": "crossref",
"first-page": "1485",
"issue": "8",
"journal-title": "Intern Emerg Med",
"key": "pgph.0000924.ref028",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1038/s41591-020-1051-9",
"article-title": "An inflammatory cytokine signature predicts COVID-19 severity and survival",
"author": "DM Del Valle",
"doi-asserted-by": "crossref",
"first-page": "1636",
"issue": "10",
"journal-title": "Nature Medicine",
"key": "pgph.0000924.ref029",
"volume": "26",
"year": "2020"
},
{
"article-title": "Pilot trial of high-dose vitamin C in critically ill COVID-19 patients.",
"author": "J Zhang",
"first-page": "5",
"issue": "1",
"key": "pgph.0000924.ref030",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2021.102324",
"article-title": "Vitamin C and COVID-19 treatment: A systematic review and meta-analysis of randomized controlled trials",
"author": "D Rawat",
"doi-asserted-by": "crossref",
"first-page": "102324",
"journal-title": "Diabetes & Metabolic Syndrome: Clinical Research & Reviews",
"key": "pgph.0000924.ref031",
"volume": "15",
"year": "2021"
},
{
"article-title": "Supplementation of the population during the COVID-19 pandemic with vitamins and micronutrients---how much evidence is needed?.",
"author": "P Schuetz",
"first-page": "w20522",
"journal-title": "Swiss Med Wkly",
"key": "pgph.0000924.ref032",
"volume": "151",
"year": "2021"
},
{
"DOI": "10.3390/nu13041172",
"article-title": "Vitamin C in the Treatment of COVID-19.",
"author": "GP Milani",
"doi-asserted-by": "crossref",
"first-page": "1172",
"issue": "4",
"journal-title": "Nutrients",
"key": "pgph.0000924.ref033",
"volume": "13",
"year": "2021"
}
],
"reference-count": 33,
"references-count": 33,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pgph.0000924"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"title": "Clinical progression and outcomes of patients hospitalized with COVID-19 in humanitarian settings: A prospective cohort study in South Sudan and Eastern Democratic Republic of the Congo",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pgph.corrections_policy",
"volume": "2"
}
doocy