The Interplay between Airway Cilia and Coronavirus Infection, Implications for Prevention and Control of Airway Viral Infections
et al., Cells, doi:10.3390/cells13161353, Aug 2024
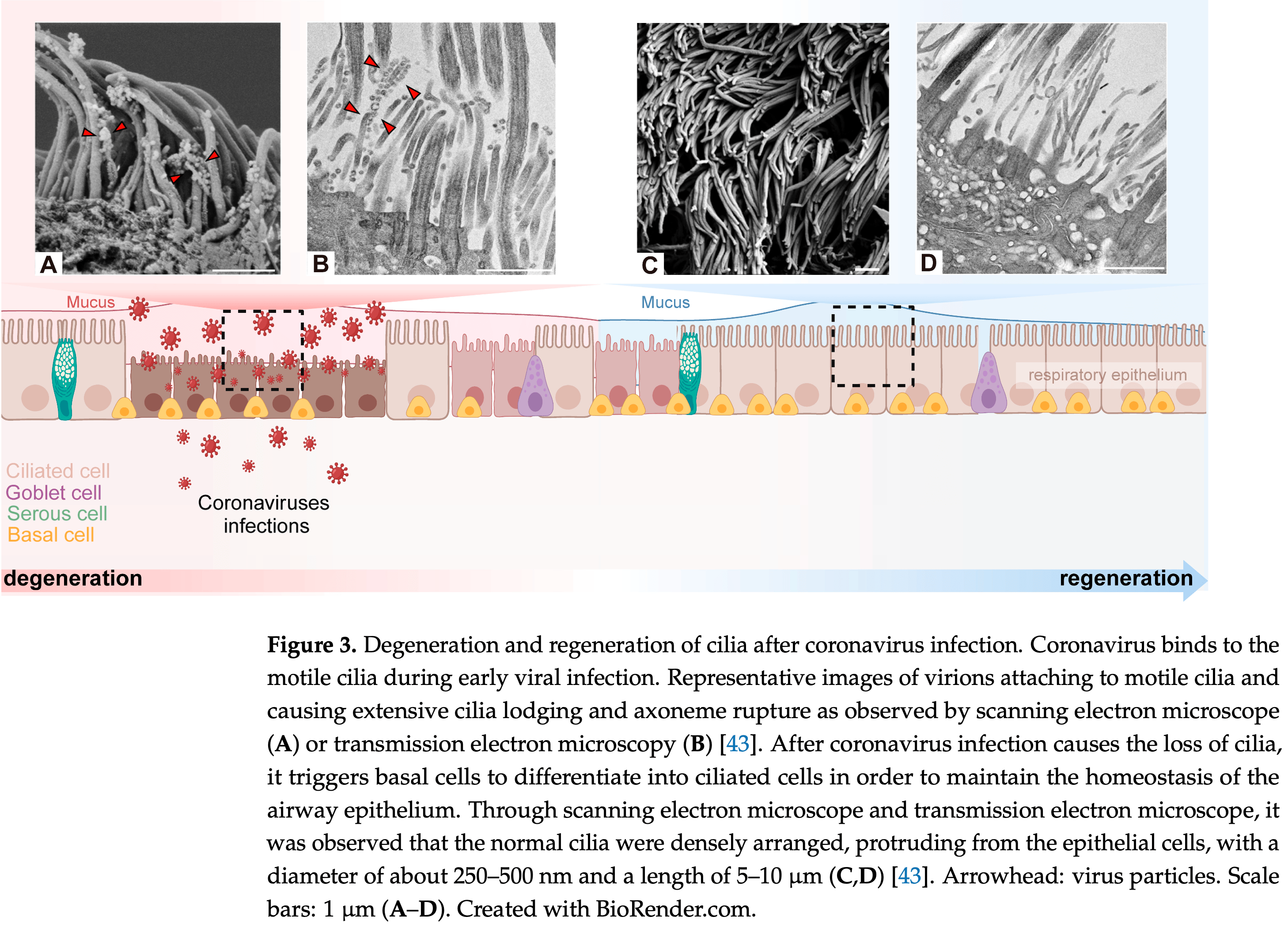
Review of the interplay between airway cilia and coronavirus infection, and the implications for prevention and treatment of respiratory viral infections. Coronaviruses target the cilia of respiratory epithelial cells, disrupting their structure and function, and impairing mucociliary clearance. This facilitates viral spread and exacerbates respiratory disease. The authors propose that protecting and restoring ciliary function may be a potential therapeutic approach for emerging coronavirus pandemics.
Dai et al., 14 Aug 2024, Democratic Republic of Congo, peer-reviewed, 3 authors.
Contact: xurd@ibtcm.ac.cn (corresponding author), daixuyao000@163.com, lin@ibtcm.ac.cn.
The Interplay between Airway Cilia and Coronavirus Infection, Implications for Prevention and Control of Airway Viral Infections
Cells, doi:10.3390/cells13161353
Coronaviruses (CoVs) are a class of respiratory viruses with the potential to cause severe respiratory diseases by infecting cells of the upper respiratory tract, bronchial epithelium, and lung. The airway cilia are distributed on the surface of respiratory epithelial cells, forming the first point of contact between the host and the inhaled coronaviruses. The function of the airway cilia is to oscillate and sense, thereby defending against and removing pathogens to maintain the cleanliness and patency of the respiratory tract. Following infection of the respiratory tract, coronaviruses exploit the cilia to invade and replicate in epithelial cells while also damaging the cilia to facilitate the spread and exacerbation of respiratory diseases. It is therefore imperative to investigate the interactions between coronaviruses and respiratory cilia, as well as to elucidate the functional mechanism of respiratory cilia following coronavirus invasion, in order to develop effective strategies for the prevention and treatment of respiratory viral infections. This review commences with an overview of the fundamental characteristics of airway cilia, and then, based on the interplay between airway cilia and coronavirus infection, we propose that ciliary protection and restoration may represent potential therapeutic approaches in emerging and re-emerging coronavirus pandemics.
Author Contributions: Conceptualization, N.L. and R.X.; methodology, N.L., R.X. and X.D.; software, X.D.; validation, N.L., R.X. and X.D.; writing-original draft preparation, X.D.; writing-review and editing, N.L. and R.X.; visualization, X.D.; supervision, N.L. and R.X.; project administration, N.L.; funding acquisition, N.L. and R.X. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest: The authors declare no conflicts of interest.
Abbreviations ACE2, angiotensin converting enzyme 2; ARDS, acute respiratory distress syndrome; ATP, Adenosine triphosphate; ATP5F1E, ATP synthase F1 subunit epsilon; ATP5MC2, ATP synthase membrane subunit C locus 2; ATP5MG, ATP synthase membrane subunit G; AHI1, Abelson helper integration site 1; ADCY3, adenylate cyclase 3; ADK, aryl diketone acid; AMT, amantadine; ALI, air-liquid interface; BPIFA1, BPI fold containing family A member 1; CoVs, coronaviruses; CECs, ciliated epithelial cells; 3CLpro, 3-chymotrypsin like protease; COVID-19, coronavirus disease 2019; CSF3, colony-stimulating factor 3; CCDC, coiled-coil domain containing; CDK1, cyclin-dependent kinase 1; CCR, C-C motif chemokine receptor; CNGA2, cyclic nucleotide gated channel subunit alpha 2; CRS, cytokine release syndrome;
References
Ahn, Kim, Hong, Choi, Yang et al., Nasal ciliated cells are primary targets for SARS-CoV-2 replication in the early stage of COVID-19, J. Clin. Investig, doi:10.1172/JCI148517
Akgoz Karaosmanoglu, Ozgen, Anatomy of the Pharynx and Cervical Esophagus, Neuroimaging Clin. N. Am, doi:10.1016/j.nic.2022.07.022
Alaofi, Exploring structural dynamics of the MERS-CoV receptor DPP4 and mutant DPP4 receptors, J. Biomol. Struct. Dyn, doi:10.1080/07391102.2020.1818626
Anderson, Daviskas, Brannan, Chan, Repurposing excipients as active inhalation agents: The mannitol story, Adv. Drug Deliv. Rev, doi:10.1016/j.addr.2018.04.003
Andrade, Fernandes, Lorenzo, Arniges, Valverde, Frontiers in Neuroscience the TRPV4 Channel in Ciliated Epithelia
Arabi, Jawdat, Hajeer, Sadat, Jose et al., Inflammatory Response and Phenotyping in Severe Acute Respiratory Infection From the Middle East Respiratory Syndrome Coronavirus and Other Etiologies, Crit. Care Med, doi:10.1097/CCM.0000000000004724
Bennett, Effect of beta-adrenergic agonists on mucociliary clearance, J. Allergy Clin. Immunol, doi:10.1067/mai.2002.129704
Bouhaddou, Memon, Meyer, White, Rezelj et al., The Global Phosphorylation Landscape of SARS-CoV-2 Infection, Cell, doi:10.1016/j.cell.2020.06.034
Brann, Tsukahara, Weinreb, Lipovsek, Van Den Berge et al., Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia, Sci. Adv, doi:10.1126/sciadv.abc5801
Breeze, Turk, Cellular structure, function and organization in the lower respiratory tract, Environ. Health Perspect, doi:10.1289/ehp.84553
Brooks, Wallingford, Multiciliated cells, Curr. Biol, doi:10.1016/j.cub.2014.08.047
Burkard, Verheije, Wicht, Van Kasteren, Van Kuppeveld et al., Coronavirus cell entry occurs through the endo-/lysosomal pathway in a proteolysis-dependent manner, PLoS Pathog, doi:10.1371/journal.ppat.1004502
Bush, Hogg, Primary ciliary dyskinesia: Recent advances in epidemiology, diagnosis, management and relationship with the expanding spectrum of ciliopathy, Expert. Rev. Respir. Med, doi:10.1586/ers.12.60
Cantuti-Castelvetri, Ojha, Pedro, Djannatian, Franz et al., Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity, Science, doi:10.1126/science.abd2985
Cao, Chen, Dong, Xie, Liu, Environmental pollutants damage airway epithelial cell cilia: Implications for the prevention of obstructive lung diseases, Thorac. Cancer, doi:10.1111/1759-7714.13323
Cao, Yang, Lee, Zhang, Sun et al., Characterization of the SARS-CoV-2 E Protein: Sequence, Structure, Viroporin, and Inhibitors, Protein Sci, doi:10.1002/pro.4075
Carfì, Bernabei, Landi, Persistent Symptoms in Patients After Acute COVID-19, JAMA, doi:10.1001/jama.2020.12603
Ceccarelli, Marino, Pulvirenti, Coco, Busà et al., Bacterial and Fungal Co-Infections and Superinfections in a Cohort of COVID-19 Patients: Real-Life Data from an Italian Third Level Hospital, Infect. Dis. Rep, doi:10.3390/idr14030041
Chacon-Heszele, Choi, Zuo, Baek, Ward et al., The exocyst and regulatory GTPases in urinary exosomes, Physiol. Rep, doi:10.14814/phy2.12116
Chatterjee, Van Putten, Strijbis, Defensive Properties of Mucin Glycoproteins during Respiratory Infections-Relevance for SARS-CoV-2, mBio, doi:10.1128/mBio.02374-20
Chen, Subbarao, The Immunobiology of SARS, Annu. Rev. Immunol, doi:10.1146/annurev.immunol.25.022106.141706
Chen, Wu, Chen, Yan, Yang et al., Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study, BMJ, doi:10.1136/bmj.m1091
Chilvers, Mckean, Rutman, Myint, Silverman et al., The effects of coronavirus on human nasal ciliated respiratory epithelium, Eur. Respir. J, doi:10.1183/09031936.01.00093001
Chinnapaiyan, Parira, Dutta, Agudelo, Morris et al., HIV Infects Bronchial Epithelium and Suppresses Components of the Mucociliary Clearance Apparatus, PLoS ONE, doi:10.1371/journal.pone.0169161
Clifton, Niemeyer, Novak, Can, Hainline et al., BPIFA1 is a secreted biomarker of differentiating human airway epithelium, Front. Cell. Infect. Microbiol, doi:10.3389/fcimb.2022.1035566
Cockx, Gouwy, Ruytinx, Lodewijckx, Van Hout et al., Monocytes from patients with Primary Ciliary Dyskinesia show enhanced inflammatory properties and produce higher levels of pro-inflammatory cytokines, Sci. Rep, doi:10.1038/s41598-017-15027-y
Davis, Marin, Yee, Nadel, Effect of terbutaline on movement of Cland Na + across the trachea of the dog in vitro, Am. Rev. Respir. Dis
Deng, Zhou, Sun, Li, Zhong et al., IFN-γ Enhances the Cough Reflex Sensitivity via Calcium Influx in Vagal Sensory Neurons, Am. J. Respir. Crit. Care Med, doi:10.1164/rccm.201709-1813OC
Devalia, Sapsford, Rusznak, Toumbis, Davies, The effects of salmeterol and salbutamol on ciliary beat frequency of cultured human bronchial epithelial cells, in vitro, Pulm. Pharmacol, doi:10.1016/0952-0600(92)90068-R
Essaidi-Laziosi, Brito, Benaoudia, Royston, Cagno et al., Propagation of respiratory viruses in human airway epithelia reveals persistent virus-specific signatures, J. Allergy Clin. Immunol, doi:10.1016/j.jaci.2017.07.018
Faure, Poissy, Goffard, Fournier, Kipnis et al., Distinct immune response in two MERS-CoV-infected patients: Can we go from bench to bedside?, PLoS ONE, doi:10.1371/journal.pone.0088716
Fehr, Perlman, Coronaviruses: An overview of their replication and pathogenesis, Methods Mol. Biol
Fink-Baldauf, Stuart, Brewington, Guo, Maeda, CRISPRi links COVID-19 GWAS loci to LZTFL1 and RAVER1, eBioMedicine, doi:10.1016/j.ebiom.2021.103806
Finlay, Brann, Abi Hachem, Jang, Oliva et al., Persistent post-COVID-19 smell loss is associated with immune cell infiltration and altered gene expression in olfactory epithelium, Sci. Transl. Med, doi:10.1126/scitranslmed.add0484
Fodoulian, Tuberosa, Rossier, Boillat, Kan et al., SARS-CoV-2 Receptors and Entry Genes Are Expressed in the Human Olfactory Neuroepithelium and Brain, iScience, doi:10.1016/j.isci.2020.101839
Francis, Chatterjee, Loges, Zentgraf, Omran et al., Initiation and maturation of cilia-generated flow in newborn and postnatal mouse airway, Am. J. Physiol. Lung Cell. Mol. Physiol, doi:10.1152/ajplung.00001.2009
Gerkin, Ohla, Veldhuizen, Joseph, Kelly et al., Recent Smell Loss Is the Best Predictor of COVID-19 among Individuals with Recent Respiratory Symptoms, Chem. Senses, doi:10.1093/chemse/bjaa081
Grant, Geoghegan, Arbyn, Mohammed, Mcguinness et al., The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): A systematic review and meta-analysis of 148 studies from 9 countries, PLoS ONE, doi:10.1371/journal.pone.0234765
Hardy, Raza, Cooper, Therapeutic glucocorticoids: Mechanisms of actions in rheumatic diseases, Nat. Rev. Rheumatol, doi:10.1038/s41584-020-0371-y
Haverkamp, Lehmbecker, Spitzbarth, Widagdo, Haagmans et al., Experimental infection of dromedaries with Middle East respiratory syndrome-Coronavirus is accompanied by massive ciliary loss and depletion of the cell surface receptor dipeptidyl peptidase 4, Sci. Rep, doi:10.1038/s41598-018-28109-2
Hay, Scheller, SNAREs and NSF in targeted membrane fusion, Curr. Opin. Cell Biol, doi:10.1016/S0955-0674(97)80026-9
He, Cai, Feng, Cai, Lin et al., Single-cell analysis reveals bronchoalveolar epithelial dysfunction in COVID-19 patients, Protein Cell, doi:10.1007/s13238-020-00752-4
Hoffmann, Kleine-Weber, Schroeder, Krüger, Herrler et al., SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Hoh, Stowe, Turk, Stearns, Transcriptional program of ciliated epithelial cells reveals new cilium and centrosome components and links to human disease, PLoS ONE, doi:10.1371/journal.pone.0052166
Horani, Ferkol, Understanding Primary Ciliary Dyskinesia and Other Ciliopathies, J. Pediatr, doi:10.1016/j.jpeds.2020.11.040
Ikegami, Ijaz, Current understandings of the relationship between extracellular vesicles and cilia, J. Biochem, doi:10.1093/jb/mvaa112
Iravani, Melville, Effects of drugs and environmental factors on ciliary movement (author's transl), Respiration, doi:10.1159/000193645
Jesenak, Durdik, Oppova, Franova, Diamant et al., Dysfunctional mucociliary clearance in asthma and airway remodeling-New insights into an old topic, Respir. Med, doi:10.1016/j.rmed.2023.107372
Jiang, Promchan, Jiang, Awasthi, Marshall et al., Depletion of BBS Protein LZTFL1 Affects Growth and Causes Retinal Degeneration in Mice, J. Genet. Genom, doi:10.1016/j.jgg.2015.11.006
Johnson, Matthay, Acute lung injury: Epidemiology, pathogenesis, and treatment, J. Aerosol Med. Pulm. Drug Deliv, doi:10.1089/jamp.2009.0775
Josset, Menachery, Gralinski, Agnihothram, Sova et al., Cell host response to infection with novel human coronavirus EMC predicts potential antivirals and important differences with SARS coronavirus, mBio, doi:10.1128/mBio.00165-13
Jácome, Campillo-Balderas, Ponce De León, Becerra, Lazcano, Sofosbuvir as a potential alternative to treat the SARS-CoV-2 epidemic, Sci. Rep, doi:10.1038/s41598-020-66440-9
Khan, Yoo, Clijsters, Backaert, Vanstapel et al., Visualizing in deceased COVID-19 patients how SARS-CoV-2 attacks the respiratory and olfactory mucosae but spares the olfactory bulb, Cell, doi:10.1016/j.cell.2021.10.027
Kikkawa, Big steps toward understanding dynein, J. Cell Biol, doi:10.1083/jcb.201304099
Klena, Pigino, Structural Biology of Cilia and Intraflagellar Transport, Annu. Rev. Cell Dev. Biol, doi:10.1146/annurev-cellbio-120219-034238
Knowles, Boucher, Mucus clearance as a primary innate defense mechanism for mammalian airways, J. Clin. Investig, doi:10.1172/JCI0215217
Knowles, Church, Waltner, Yankaskas, Gilligan et al., A pilot study of aerosolized amiloride for the treatment of lung disease in cystic fibrosis, N. Engl. J. Med, doi:10.1056/NEJM199004263221704
Kuek, Lee, First contact: The role of respiratory cilia in host-pathogen interactions in the airways, Am. J. Physiol. Lung Cell. Mol. Physiol, doi:10.1152/ajplung.00283.2020
Kuhn, Li, Choe, Farzan, Angiotensin-converting enzyme 2: A functional receptor for SARS coronavirus, Cell. Mol. Life Sci, doi:10.1007/s00018-004-4242-5
Lee, Nakayama, Wu, Goltsev, Jiang et al., ACE2 localizes to the respiratory cilia and is not increased by ACE inhibitors or ARBs, Nat. Commun, doi:10.1038/s41467-020-19145-6
Lehrich, Goshtasbi, Raad, Ganti, Papagiannopoulos et al., Aggregate Prevalence of Chemosensory and Sinonasal Dysfunction in SARS-CoV-2 and Related Coronaviruses, Otolaryngol. Head Neck Surg, doi:10.1177/0194599820929278
Leung, Yang, Tam, Shaipanich, Hackett et al., ACE-2 expression in the small airway epithelia of smokers and COPD patients: Implications for COVID-19, Eur. Respir. J, doi:10.1183/13993003.00688-2020
Li, Berardi, Li, Farzan, Dormitzer et al., Conformational states of the severe acute respiratory syndrome coronavirus spike protein ectodomain, J. Virol, doi:10.1128/JVI.02744-05
Li, Zhang, Yang, Lian, Xie et al., The MERS-CoV Receptor DPP4 as a Candidate Binding Target of the SARS-CoV-2 Spike, iScience, doi:10.1016/j.isci.2020.101160
Liang, Tian, Liu, Hui, Qiao et al., A promising antiviral candidate drug for the COVID-19 pandemic: A mini-review of remdesivir, Eur. J. Med. Chem, doi:10.1016/j.ejmech.2020.112527
Lin, Okada, Raytchev, Smith, Nicastro, Structural mechanism of the dynein power stroke, Nat. Cell Biol, doi:10.1038/ncb2939
Lindeboom, Worlock, Dratva, Yoshida, Scobie et al., Human SARS-CoV-2 challenge uncovers local and systemic response dynamics, Nature, doi:10.1038/s41586-024-07575-x
Lyu, Li, Zhou, Zhao, Formation and function of multiciliated cells, J. Cell Biol, doi:10.1083/jcb.202307150
Ma, Guo, Tang, Tseng, Wang et al., Broad ultra-potent neutralization of SARS-CoV-2 variants by monoclonal antibodies specific to the tip of RBD, Cell Discov, doi:10.1038/s41421-022-00381-7
Ma, Sun, Jiang, Zuo, Chen et al., WDPCP regulates the ciliogenesis of human sinonasal epithelial cells in chronic rhinosinusitis, Cytoskeleton, doi:10.1002/cm.21351
Machogu, Gaston, Respiratory Distress in the Newborn with Primary Ciliary Dyskinesia, Children, doi:10.3390/children8020153
Mall, Role of cilia, mucus, and airway surface liquid in mucociliary dysfunction: Lessons from mouse models, J. Aerosol Med. Pulm. Drug Deliv, doi:10.1089/jamp.2007.0659
Martinez-Garcia, Aksamit, Aliberti, Bronchiectasis as a Long-Term Consequence of SARS-COVID-19 Pneumonia: Future Studies are Needed, Arch. Bronconeumol, doi:10.1016/j.arbres.2021.04.021
Mayer-Hamblett, Ramsey, Kronmal, Advancing outcome measures for the new era of drug development in cystic fibrosis, Proc. Am. Thorac. Soc, doi:10.1513/pats.200703-040BR
Mc Fie, Koneva, Collins, Coveney, Clube et al., Ciliary proteins specify the cell inflammatory response by tuning NFκB signalling, independently of primary cilia, J. Cell Sci, doi:10.1242/jcs.239871
Menni, Valdes, Freidin, Sudre, Nguyen et al., Real-time tracking of self-reported symptoms to predict potential COVID-19, Nat. Med, doi:10.1038/s41591-020-0916-2
Molla-Herman, Ghossoub, Blisnick, Meunier, Serres et al., The ciliary pocket: An endocytic membrane domain at the base of primary and motile cilia, J. Cell Sci, doi:10.1242/jcs.059519
Moscoso, Driver, Codd, Whimster, The morphology of ciliogenesis in the developing fetal human respiratory epithelium, Pathol. Res. Pract, doi:10.1016/S0344-0338(88)80086-4
Najjar-Debbiny, Gronich, Weber, Khoury, Amar et al., Effectiveness of Paxlovid in Reducing Severe Coronavirus Disease 2019 and Mortality in High-Risk Patients, Clin. Infect. Dis, doi:10.1093/cid/ciac443
Nakayama, Lee, Jiang, Matter, Yan et al., Determinants of SARS-CoV-2 entry and replication in airway mucosal tissue and susceptibility in smokers, Cell Rep. Med, doi:10.1016/j.xcrm.2021.100421
Nicholls, Poon, Lee, Ng, Lai et al., Lung pathology of fatal severe acute respiratory syndrome, Lancet, doi:10.1016/S0140-6736(03)13413-7
Nishi, Yoshimoto, Nishi, Nishi, Nishi et al., Epipharyngeal Abrasive Therapy Down-regulates the Expression of Cav1.2: A Key Molecule in Influenza Virus Entry, Vivo, doi:10.21873/invivo.12967
Nishi, Yoshimoto, Nishi, Tsunoda, Ohno et al., Epipharyngeal Abrasive Therapy Down-regulates the Expression of SARS-CoV-2 Entry Factors ACE2 and TMPRSS2, Vivo, doi:10.21873/invivo.12712
Nunnari, Sanfilippo, Castrogiovanni, Imbesi, Li Volti et al., Network perturbation analysis in human bronchial epithelial cells following SARS-CoV2 infection, Exp. Cell Res, doi:10.1016/j.yexcr.2020.112204
Ostrowski, Blackburn, Radde, Moyer, Schlatzer et al., A proteomic analysis of human cilia: Identification of novel components, Mol. Cell. Proteom, doi:10.1074/mcp.M200037-MCP200
Ou, Liu, Lei, Li, Mi et al., Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV, Nat. Commun, doi:10.1038/s41467-020-15562-9
Pacentine, Nicolson, Subunits of the mechano-electrical transduction channel, Tmc1/2b, require Tmie to localize in zebrafish sensory hair cells, PLoS Genet, doi:10.1371/journal.pgen.1007635
Pazour, Agrin, Leszyk, Witman, Proteomic analysis of a eukaryotic cilium, J. Cell Biol, doi:10.1083/jcb.200504008
Pazour, Witman, The vertebrate primary cilium is a sensory organelle, Curr. Opin. Cell Biol, doi:10.1016/S0955-0674(02)00012-1
Pedersen, Goutaki, Harris, Dixon, Manion et al., SARS-CoV-2 infections in people with primary ciliary dyskinesia: Neither frequent, nor particularly severe, Eur. Respir. J, doi:10.1183/13993003.04548-2020
Peiris, Chu, Cheng, Chan, Hung et al., Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: A prospective study, Lancet, doi:10.1016/S0140-6736(03)13412-5
Peng, Du, Lei, Dorje, Qi et al., Structures of the SARS-CoV-2 nucleocapsid and their perspectives for drug design, Embo J, doi:10.15252/embj.2020105938
Pereira, Barbosa, Alves, Santos, Oliveira et al., Unveiling the genetic etiology of primary ciliary dyskinesia: When standard genetic approach is not enough, Adv. Med. Sci, doi:10.1016/j.advms.2019.10.003
Perez-Miller, Patek, Moutal, Duran, Cabel et al., Novel Compounds Targeting Neuropilin Receptor 1 with Potential To Interfere with SARS-CoV-2 Virus Entry, ACS Chem. Neurosci, doi:10.1021/acschemneuro.0c00619
Perico, Cortinovis, Suter, Remuzzi, Home as the new frontier for the treatment of COVID-19: The case for anti-inflammatory agents, Lancet Infect. Dis, doi:10.1016/S1473-3099(22)00433-9
Pinskey, Franks, Mcmellen, Giger, Allen, Neuropilin-1 promotes Hedgehog signaling through a novel cytoplasmic motif, J. Biol. Chem, doi:10.1074/jbc.M117.783845
Qiao, Wotring, Zheng, Zhang, Zhang et al., Proxalutamide reduces SARS-CoV-2 infection and associated inflammatory response, Proc. Natl. Acad. Sci, doi:10.1073/pnas.2221809120
Qin, Zhou, Hu, Zhang, Yang et al., Dysregulation of Immune Response in Patients with Coronavirus 2019 (COVID-19) in Wuhan, China, Clin. Infect. Dis, doi:10.1093/cid/ciaa248
Radicioni, Ceppe, Ford, Alexis, Barr et al., Airway mucin MUC5AC and MUC5B concentrations and the initiation and progression of chronic obstructive pulmonary disease: An analysis of the SPIROMICS cohort, Lancet Respir. Med, doi:10.1016/S2213-2600(21)00079-5
Raman, O'connor, Hackett, Wang, Harvey et al., Quality control in microarray assessment of gene expression in human airway epithelium, BMC Genom, doi:10.1186/1471-2164-10-493
Reis, Moreira Silva, Medeiros Silva, Thabane, Campos et al., Early Treatment with Pegylated Interferon Lambda for COVID-19, N. Engl. J. Med, doi:10.1056/NEJMoa2209760
Reiter, Leroux, Genes and molecular pathways underpinning ciliopathies, Nat. Rev. Mol. Cell Biol, doi:10.1038/nrm.2017.60
Retuerto-Guerrero, López-Medrano, De Freitas-González, Rivero-Lezcano, Nontuberculous Mycobacteria, Mucociliary Clearance, and Bronchiectasis, Microorganisms, doi:10.3390/microorganisms12040665
Reznik, Comparative anatomy, physiology, and function of the upper respiratory tract, Environ. Health Perspect
Robinot, Hubert, De Melo, Lazarini, Bruel et al., SARS-CoV-2 infection induces the dedifferentiation of multiciliated cells and impairs mucociliary clearance, Nat. Commun, doi:10.1038/s41467-021-24521-x
Saniasiaya, Islam, Abdullah, Prevalence of Olfactory Dysfunction in Coronavirus Disease 2019 (COVID-19): A Meta-analysis of 27,492 Patients, Laryngoscope, doi:10.1002/lary.29286
Satir, CILIA: Before and after, Cilia, doi:10.1186/s13630-017-0046-8
Schofield, Duff, Brennan, Airway Clearance Techniques for Primary Ciliary Dyskinesia; is the Cystic Fibrosis literature portable?, Paediatr. Respir. Rev, doi:10.1016/j.prrv.2017.03.011
Schreiner, Allnoch, Beythien, Marek, Becker et al., SARS-CoV-2 Infection Dysregulates Cilia and Basal Cell Homeostasis in the Respiratory Epithelium of Hamsters, Int. J. Mol. Sci, doi:10.3390/ijms23095124
Schwarzenbacher, Fleischer, Breer, Formation and maturation of olfactory cilia monitored by odorant receptor-specific antibodies, Histochem. Cell Biol, doi:10.1007/s00418-005-0790-5
Shah, Ben-Shahar, Moninger, Kline, Welsh, Motile cilia of human airway epithelia are chemosensory, Science, doi:10.1126/science.1173869
Shelton, Shastri, Fletez-Brant, Aslibekyan, Auton, The UGT2A1/UGT2A2 locus is associated with COVID-19related loss of smell or taste, Nat. Genet, doi:10.1038/s41588-021-00986-w
Shen, Wang, Li, Zhang, Tian et al., Structures of ACE2-SIT1 recognized by Omicron variants of SARS-CoV-2, Cell Discov, doi:10.1038/s41421-022-00488-x
Sieczkarski, Whittaker, Dissecting virus entry via endocytosis, J. Gen. Virol, doi:10.1099/0022-1317-83-7-1535
Sleigh, Blake, Liron, The propulsion of mucus by cilia, Am. Rev. Respir. Dis, doi:10.1164/ajrccm/137.3.726
Song, Hui, Hull, Birring, Mcgarvey et al., Confronting COVID-19-associated cough and the post-COVID syndrome: Role of viral neurotropism, neuroinflammation, and neuroimmune responses, Lancet Respir. Med, doi:10.1016/S2213-2600(21)00125-9
Spratt, Gallazzi, Quinn, Lorson, Sönnerborg et al., Coronavirus helicases: Attractive and unique targets of antiviral drug-development and therapeutic patents, Expert. Opin. Ther. Pat, doi:10.1080/13543776.2021.1884224
Stebbing, Sánchez Nievas, Falcone, Youhanna, Richardson et al., JAK inhibition reduces SARS-CoV-2 liver infectivity and modulates inflammatory responses to reduce morbidity and mortality, Sci. Adv, doi:10.1126/sciadv.abe4724
Sungnak, Huang, Bécavin, Berg, Queen et al., SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes, Nat. Med, doi:10.1038/s41591-020-0868-6
Taha, Hall, Shortess, Rathbone, Barham, Treatment Protocol for COVID-19 Based on T2R Phenotype, Viruses, doi:10.3390/v13030503
Tajiri, Kawachi, Yoshida, Noguchi, Terashita et al., The causes of acute cough: A tertiary-care hospital study in Japan, J. Asthma, doi:10.1080/02770903.2020.1804576
Tan, Ong, Yan, Liu, Li et al., In Vitro Model of Fully Differentiated Human Nasal Epithelial Cells Infected with Rhinovirus Reveals Epithelium-Initiated Immune Responses, J. Infect. Dis, doi:10.1093/infdis/jix640
Tay, Poh, Rénia, Macary, Ng, The trinity of COVID-19: Immunity, inflammation and intervention, Nat. Rev. Immunol, doi:10.1038/s41577-020-0311-8
Thompson, Barclay, Zambon, Pickles, Infection of human airway epithelium by human and avian strains of influenza a virus, J. Virol, doi:10.1128/JVI.00384-06
Tilley, Walters, Shaykhiev, Crystal, Cilia dysfunction in lung disease, Annu. Rev. Physiol, doi:10.1146/annurev-physiol-021014-071931
Turnbull, Shoemark, Palau, Murphy, Simbo et al., Determining the impact of the T2R38 bitter taste receptor on P. aeruginosa infection in the cystic fibrosis airway, J. Cyst. Fibros, doi:10.1016/S1569-1993(17)30457-5
Ugalde, Bretones, Rodríguez, Quesada, Llorente et al., Autophagy-linked plasma and lysosomal membrane protein PLAC8 is a key host factor for SARS-CoV-2 entry into human cells, Embo J, doi:10.15252/embj.2022110727
Verma, Zheng, Meyerholz, Perlman, SARS-CoV-2 infection of sustentacular cells disrupts olfactory signaling pathways, JCI Insight, doi:10.1172/jci.insight.160277
Viau, Bienaimé, Lukas, Todkar, Knoll et al., Cilia-localized LKB1 regulates chemokine signaling, macrophage recruitment, and tissue homeostasis in the kidney, Embo J, doi:10.15252/embj.201798615
Victores, Chen, Smith, Lane, Olfactory loss in chronic rhinosinusitis is associated with neuronal activation of c-Jun N-terminal kinase, Int. Forum Allergy Rhinol, doi:10.1002/alr.22053
Vogalis, Hegg, Lucero, Ionic conductances in sustentacular cells of the mouse olfactory epithelium, J. Physiol, doi:10.1113/jphysiol.2004.079228
Wang, Liu, Yang, Zhang, Jiao et al., SARS-CoV-2 ORF10 impairs cilia by enhancing CUL2 ZYG11B activity, J. Cell Biol, doi:10.1083/jcb.202108015
Wang, Yang, Liu, Guo, Zhang et al., SARS coronavirus entry into host cells through a novel clathrinand caveolae-independent endocytic pathway, Cell Res, doi:10.1038/cr.2008.15
Whitsett, Airway Epithelial Differentiation and Mucociliary Clearance, Ann. Am. Thorac. Soc, doi:10.1513/AnnalsATS.201802-128AW
Wiersinga, Rhodes, Cheng, Peacock, Prescott et al., Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review, JAMA, doi:10.1001/jama.2020.12839
Wu, Lidsky, Xiao, Cheng, Lee et al., SARS-CoV-2 replication in airway epithelia requires motile cilia and microvillar reprogramming, Cell, doi:10.1016/j.cell.2022.11.030
Wu, Liu, Zhao, Liu, Wang et al., Clinical Characteristics of Imported Cases of Coronavirus Disease 2019 (COVID-19) in Jiangsu Province: A Multicenter Descriptive Study, Clin. Infect. Dis, doi:10.1093/cid/ciaa199
Yang, Liu, Yan, Lu, Shan et al., SARS-CoV-2 spike protein receptor-binding domain perturbates intracellular calcium homeostasis and impairs pulmonary vascular endothelial cells, Signal Transduct. Target. Ther, doi:10.1038/s41392-023-01556-8
Yang, Shen, Targeting the Endocytic Pathway and Autophagy Process as a Novel Therapeutic Strategy in COVID-19, Int. J. Biol. Sci, doi:10.7150/ijbs.45498
Yang, Wu, Zhou, Wang, Wang, The microRNA/TET3/REST axis is required for olfactory globose basal cell proliferation and male behavior, EMBO Rep, doi:10.15252/embr.201949431
Yu, Chang, The first Chinese oral anti-COVID-19 drug Azvudine launched, Innovation, doi:10.1016/j.xinn.2022.100321
Zajkowska, Hermanowska-Szpakowicz, Pancewicz, Kondrusik, Grygorczuk, Severe acute respiratory syndrome (SARS)--new, unknown disease?, Pol. Merkur. Lek
Zazhytska, Kodra, Hoagland, Frere, Fullard et al., Non-cell-autonomous disruption of nuclear architecture as a potential cause of COVID-19-induced anosmia, Cell, doi:10.1016/j.cell.2022.01.024
Zhang, Bukreyev, Thompson, Watson, Peeples et al., Infection of ciliated cells by human parainfluenza virus type 3 in an in vitro model of human airway epithelium, J. Virol, doi:10.1128/JVI.79.2.1113-1124.2005
Zhang, Lee, Chu, Chan, Fan et al., Severe Acute Respiratory Syndrome Coronavirus 2 Infects and Damages the Mature and Immature Olfactory Sensory Neurons of Hamsters, Clin. Infect. Dis, doi:10.1093/cid/ciaa995
Zhang, Peeples, Boucher, Collins, Pickles, Respiratory syncytial virus infection of human airway epithelial cells is polarized, specific to ciliated cells, and without obvious cytopathology, J. Virol, doi:10.1128/JVI.76.11.5654-5666.2002
Zhao, Li, Zhou, Ciliary ectosomes: Critical microvesicle packets transmitted from the cell tower, Sci. Bull, doi:10.1016/j.scib.2023.09.027
Zheng, Ma, Wang, Cheng, Zhou et al., Efficacy and safety of Paxlovid for COVID-19: A meta-analysis, J. Infect, doi:10.1016/j.jinf.2022.09.027
Zhou, Yuan, Zhang, Meng, Zhang et al., DRC3 is an assembly adapter of the nexin-dynein regulatory complex functional components during spermatogenesis in humans and mice, Signal Transduct. Target. Ther, doi:10.1038/s41392-022-01293-4
Zhu, Ehre, Abdullah, Sheehan, Roy et al., Munc13-2 -/baseline secretion defect reveals source of oligomeric mucins in mouse airways, J. Physiol, doi:10.1113/jphysiol.2007.149310
Zhu, Wang, Zha, Wang, Wang et al., Transcriptomic and Lipidomic Profiles in Nasal Polyps of Glucocorticoid Responders and Non-Responders: Before and After Treatment, Front. Pharmacol, doi:10.3389/fphar.2021.814953
Zhu, Zhang, Wang, Li, Yang et al., A Novel Coronavirus from Patients with Pneumonia in China, N. Engl. J. Med, doi:10.1056/NEJMoa2001017
Zimmerman, Song, Gonzalez-Mize, Li, Yoder, Primary cilia disruption differentially affects the infiltrating and resident macrophage compartment in the liver, Am. J. Physiol. Gastrointest. Liver Physiol, doi:10.1152/ajpgi.00381.2017
Zoufaly, Poglitsch, Aberle, Hoepler, Seitz et al., Human recombinant soluble ACE2 in severe COVID-19, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30418-5
Zumla, Hui, Perlman, Middle East respiratory syndrome, Lancet, doi:10.1016/S0140-6736(15)60454-8
DOI record:
{
"DOI": "10.3390/cells13161353",
"ISSN": [
"2073-4409"
],
"URL": "http://dx.doi.org/10.3390/cells13161353",
"abstract": "<jats:p>Coronaviruses (CoVs) are a class of respiratory viruses with the potential to cause severe respiratory diseases by infecting cells of the upper respiratory tract, bronchial epithelium, and lung. The airway cilia are distributed on the surface of respiratory epithelial cells, forming the first point of contact between the host and the inhaled coronaviruses. The function of the airway cilia is to oscillate and sense, thereby defending against and removing pathogens to maintain the cleanliness and patency of the respiratory tract. Following infection of the respiratory tract, coronaviruses exploit the cilia to invade and replicate in epithelial cells while also damaging the cilia to facilitate the spread and exacerbation of respiratory diseases. It is therefore imperative to investigate the interactions between coronaviruses and respiratory cilia, as well as to elucidate the functional mechanism of respiratory cilia following coronavirus invasion, in order to develop effective strategies for the prevention and treatment of respiratory viral infections. This review commences with an overview of the fundamental characteristics of airway cilia, and then, based on the interplay between airway cilia and coronavirus infection, we propose that ciliary protection and restoration may represent potential therapeutic approaches in emerging and re-emerging coronavirus pandemics.</jats:p>",
"alternative-id": [
"cells13161353"
],
"author": [
{
"affiliation": [
{
"name": "Department of Biomedical Engineering and Technology, Institute of Basic Theory for Chinese Medicine, China Academy of Chinese Medical Sciences, Beijing 100700, China"
}
],
"family": "Dai",
"given": "Xuyao",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Biomedical Engineering and Technology, Institute of Basic Theory for Chinese Medicine, China Academy of Chinese Medical Sciences, Beijing 100700, China"
}
],
"family": "Xu",
"given": "Ruodan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Biomedical Engineering and Technology, Institute of Basic Theory for Chinese Medicine, China Academy of Chinese Medical Sciences, Beijing 100700, China"
}
],
"family": "Li",
"given": "Ning",
"sequence": "additional"
}
],
"container-title": "Cells",
"container-title-short": "Cells",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
8,
14
]
],
"date-time": "2024-08-14T10:23:05Z",
"timestamp": 1723630985000
},
"deposited": {
"date-parts": [
[
2024,
8,
14
]
],
"date-time": "2024-08-14T10:46:14Z",
"timestamp": 1723632374000
},
"funder": [
{
"DOI": "10.13039/501100001809",
"award": [
"82141220",
"82104672"
],
"doi-asserted-by": "publisher",
"id": [
{
"asserted-by": "publisher",
"id": "10.13039/501100001809",
"id-type": "DOI"
}
],
"name": "National Natural Science Foundation of China"
},
{
"award": [
"KYG-202405"
],
"name": "TCM Theory Inheritance and Innovation Project of CACMS Innovation Fund"
},
{
"award": [
"CI2021A00609",
"CI2021A00112"
],
"name": "Scientific and Technological Innovation Project, China Academy of Chinese Medical Sciences"
},
{
"award": [
"YPX-202301"
],
"name": "Fundamental Research Funds for the Central Public Welfare Research Institutes"
}
],
"indexed": {
"date-parts": [
[
2024,
8,
15
]
],
"date-time": "2024-08-15T00:24:23Z",
"timestamp": 1723681463452
},
"is-referenced-by-count": 0,
"issue": "16",
"issued": {
"date-parts": [
[
2024,
8,
14
]
]
},
"journal-issue": {
"issue": "16",
"published-online": {
"date-parts": [
[
2024,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
8,
14
]
],
"date-time": "2024-08-14T00:00:00Z",
"timestamp": 1723593600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2073-4409/13/16/1353/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1353",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
8,
14
]
]
},
"published-online": {
"date-parts": [
[
2024,
8,
14
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1172/JCI0215217",
"article-title": "Mucus clearance as a primary innate defense mechanism for mammalian airways",
"author": "Knowles",
"doi-asserted-by": "crossref",
"first-page": "571",
"journal-title": "J. Clin. Investig.",
"key": "ref_1",
"volume": "109",
"year": "2002"
},
{
"DOI": "10.1152/ajplung.00283.2020",
"article-title": "First contact: The role of respiratory cilia in host-pathogen interactions in the airways",
"author": "Kuek",
"doi-asserted-by": "crossref",
"first-page": "L603",
"journal-title": "Am. J. Physiol. Lung Cell. Mol. Physiol.",
"key": "ref_2",
"volume": "319",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(03)13412-5",
"article-title": "Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: A prospective study",
"author": "Peiris",
"doi-asserted-by": "crossref",
"first-page": "1767",
"journal-title": "Lancet",
"key": "ref_3",
"volume": "361",
"year": "2003"
},
{
"DOI": "10.1016/j.xcrm.2021.100421",
"article-title": "Determinants of SARS-CoV-2 entry and replication in airway mucosal tissue and susceptibility in smokers",
"author": "Nakayama",
"doi-asserted-by": "crossref",
"first-page": "100421",
"journal-title": "Cell Rep. Med.",
"key": "ref_4",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1038/s41467-021-24521-x",
"article-title": "SARS-CoV-2 infection induces the dedifferentiation of multiciliated cells and impairs mucociliary clearance",
"author": "Robinot",
"doi-asserted-by": "crossref",
"first-page": "4354",
"journal-title": "Nat. Commun.",
"key": "ref_5",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1007/s13238-020-00752-4",
"article-title": "Single-cell analysis reveals bronchoalveolar epithelial dysfunction in COVID-19 patients",
"author": "He",
"doi-asserted-by": "crossref",
"first-page": "680",
"journal-title": "Protein Cell",
"key": "ref_6",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1242/jcs.239871",
"article-title": "Ciliary proteins specify the cell inflammatory response by tuning NFκB signalling, independently of primary cilia",
"author": "Koneva",
"doi-asserted-by": "crossref",
"first-page": "jcs239871",
"journal-title": "J. Cell Sci.",
"key": "ref_7",
"volume": "133",
"year": "2020"
},
{
"DOI": "10.1038/s41392-023-01556-8",
"article-title": "SARS-CoV-2 spike protein receptor-binding domain perturbates intracellular calcium homeostasis and impairs pulmonary vascular endothelial cells",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "276",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_8",
"volume": "8",
"year": "2023"
},
{
"DOI": "10.3390/v13030503",
"doi-asserted-by": "crossref",
"key": "ref_9",
"unstructured": "Taha, M.A., Hall, C.A., Shortess, C.J., Rathbone, R.F., and Barham, H.P. (2021). Treatment Protocol for COVID-19 Based on T2R Phenotype. Viruses, 13."
},
{
"DOI": "10.1513/AnnalsATS.201802-128AW",
"article-title": "Airway Epithelial Differentiation and Mucociliary Clearance",
"author": "Whitsett",
"doi-asserted-by": "crossref",
"first-page": "S143",
"journal-title": "Ann. Am. Thorac. Soc.",
"key": "ref_10",
"volume": "15",
"year": "2018"
},
{
"DOI": "10.1111/1759-7714.13323",
"article-title": "Environmental pollutants damage airway epithelial cell cilia: Implications for the prevention of obstructive lung diseases",
"author": "Cao",
"doi-asserted-by": "crossref",
"first-page": "505",
"journal-title": "Thorac. Cancer",
"key": "ref_11",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1146/annurev-cellbio-120219-034238",
"article-title": "Structural Biology of Cilia and Intraflagellar Transport",
"author": "Klena",
"doi-asserted-by": "crossref",
"first-page": "103",
"journal-title": "Annu. Rev. Cell Dev. Biol.",
"key": "ref_12",
"volume": "38",
"year": "2022"
},
{
"DOI": "10.1016/j.jpeds.2020.11.040",
"article-title": "Understanding Primary Ciliary Dyskinesia and Other Ciliopathies",
"author": "Horani",
"doi-asserted-by": "crossref",
"first-page": "15",
"journal-title": "J. Pediatr.",
"key": "ref_13",
"volume": "230",
"year": "2021"
},
{
"DOI": "10.1038/s41392-022-01293-4",
"article-title": "DRC3 is an assembly adapter of the nexin-dynein regulatory complex functional components during spermatogenesis in humans and mice",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "26",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_14",
"volume": "8",
"year": "2023"
},
{
"DOI": "10.1038/ncb2939",
"article-title": "Structural mechanism of the dynein power stroke",
"author": "Lin",
"doi-asserted-by": "crossref",
"first-page": "479",
"journal-title": "Nat. Cell Biol.",
"key": "ref_15",
"volume": "16",
"year": "2014"
},
{
"DOI": "10.15252/embr.201949431",
"article-title": "The microRNA/TET3/REST axis is required for olfactory globose basal cell proliferation and male behavior",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "e49431",
"journal-title": "EMBO Rep.",
"key": "ref_16",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.3389/fcimb.2022.1035566",
"doi-asserted-by": "crossref",
"key": "ref_17",
"unstructured": "Clifton, C., Niemeyer, B.F., Novak, R., Can, U.I., Hainline, K., and Benam, K.H. (2022). BPIFA1 is a secreted biomarker of differentiating human airway epithelium. Front. Cell. Infect. Microbiol., 12."
},
{
"DOI": "10.1016/j.cell.2021.10.027",
"article-title": "Visualizing in deceased COVID-19 patients how SARS-CoV-2 attacks the respiratory and olfactory mucosae but spares the olfactory bulb",
"author": "Khan",
"doi-asserted-by": "crossref",
"first-page": "5932",
"journal-title": "Cell",
"key": "ref_18",
"volume": "184",
"year": "2021"
},
{
"DOI": "10.1007/s00418-005-0790-5",
"article-title": "Formation and maturation of olfactory cilia monitored by odorant receptor-specific antibodies",
"author": "Schwarzenbacher",
"doi-asserted-by": "crossref",
"first-page": "419",
"journal-title": "Histochem. Cell Biol.",
"key": "ref_19",
"volume": "123",
"year": "2005"
},
{
"DOI": "10.1186/1471-2164-10-493",
"doi-asserted-by": "crossref",
"key": "ref_20",
"unstructured": "Raman, T., O’Connor, T.P., Hackett, N.R., Wang, W., Harvey, B.G., Attiyeh, M.A., Dang, D.T., Teater, M., and Crystal, R.G. (2009). Quality control in microarray assessment of gene expression in human airway epithelium. BMC Genom., 10."
},
{
"DOI": "10.1289/ehp.84553",
"article-title": "Cellular structure, function and organization in the lower respiratory tract",
"author": "Breeze",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "Environ. Health Perspect.",
"key": "ref_21",
"volume": "55",
"year": "1984"
},
{
"DOI": "10.1186/s13630-017-0046-8",
"article-title": "CILIA: Before and after",
"author": "Satir",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Cilia",
"key": "ref_22",
"volume": "6",
"year": "2017"
},
{
"DOI": "10.1083/jcb.200504008",
"article-title": "Proteomic analysis of a eukaryotic cilium",
"author": "Pazour",
"doi-asserted-by": "crossref",
"first-page": "103",
"journal-title": "J. Cell Biol.",
"key": "ref_23",
"volume": "170",
"year": "2005"
},
{
"DOI": "10.1074/mcp.M200037-MCP200",
"article-title": "A proteomic analysis of human cilia: Identification of novel components",
"author": "Ostrowski",
"doi-asserted-by": "crossref",
"first-page": "451",
"journal-title": "Mol. Cell. Proteom.",
"key": "ref_24",
"volume": "1",
"year": "2002"
},
{
"DOI": "10.1371/journal.pone.0052166",
"doi-asserted-by": "crossref",
"key": "ref_25",
"unstructured": "Hoh, R.A., Stowe, T.R., Turk, E., and Stearns, T. (2012). Transcriptional program of ciliated epithelial cells reveals new cilium and centrosome components and links to human disease. PLoS ONE, 7."
},
{
"DOI": "10.1152/ajplung.00001.2009",
"article-title": "Initiation and maturation of cilia-generated flow in newborn and postnatal mouse airway",
"author": "Francis",
"doi-asserted-by": "crossref",
"first-page": "L1067",
"journal-title": "Am. J. Physiol. Lung Cell. Mol. Physiol.",
"key": "ref_26",
"volume": "296",
"year": "2009"
},
{
"DOI": "10.1016/S0344-0338(88)80086-4",
"article-title": "The morphology of ciliogenesis in the developing fetal human respiratory epithelium",
"author": "Moscoso",
"doi-asserted-by": "crossref",
"first-page": "403",
"journal-title": "Pathol. Res. Pract.",
"key": "ref_27",
"volume": "183",
"year": "1988"
},
{
"DOI": "10.1586/ers.12.60",
"article-title": "Primary ciliary dyskinesia: Recent advances in epidemiology, diagnosis, management and relationship with the expanding spectrum of ciliopathy",
"author": "Bush",
"doi-asserted-by": "crossref",
"first-page": "663",
"journal-title": "Expert. Rev. Respir. Med.",
"key": "ref_28",
"volume": "6",
"year": "2012"
},
{
"DOI": "10.1146/annurev-physiol-021014-071931",
"article-title": "Cilia dysfunction in lung disease",
"author": "Tilley",
"doi-asserted-by": "crossref",
"first-page": "379",
"journal-title": "Annu. Rev. Physiol.",
"key": "ref_29",
"volume": "77",
"year": "2015"
},
{
"DOI": "10.1083/jcb.202307150",
"doi-asserted-by": "crossref",
"key": "ref_30",
"unstructured": "Lyu, Q., Li, Q., Zhou, J., and Zhao, H. (2024). Formation and function of multiciliated cells. J. Cell Biol., 223."
},
{
"DOI": "10.3390/children8020153",
"doi-asserted-by": "crossref",
"key": "ref_31",
"unstructured": "Machogu, E., and Gaston, B. (2021). Respiratory Distress in the Newborn with Primary Ciliary Dyskinesia. Children, 8."
},
{
"DOI": "10.3390/ijms23095124",
"doi-asserted-by": "crossref",
"key": "ref_32",
"unstructured": "Schreiner, T., Allnoch, L., Beythien, G., Marek, K., Becker, K., Schaudien, D., Stanelle-Bertram, S., Schaumburg, B., Mounogou Kouassi, N., and Beck, S. (2022). SARS-CoV-2 Infection Dysregulates Cilia and Basal Cell Homeostasis in the Respiratory Epithelium of Hamsters. Int. J. Mol. Sci., 23."
},
{
"DOI": "10.1016/S2213-2600(21)00079-5",
"article-title": "Airway mucin MUC5AC and MUC5B concentrations and the initiation and progression of chronic obstructive pulmonary disease: An analysis of the SPIROMICS cohort",
"author": "Radicioni",
"doi-asserted-by": "crossref",
"first-page": "1241",
"journal-title": "Lancet Respir. Med.",
"key": "ref_33",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1113/jphysiol.2007.149310",
"article-title": "Munc13-2−/− baseline secretion defect reveals source of oligomeric mucins in mouse airways",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "1977",
"journal-title": "J. Physiol.",
"key": "ref_34",
"volume": "586",
"year": "2008"
},
{
"DOI": "10.1164/ajrccm/137.3.726",
"article-title": "The propulsion of mucus by cilia",
"author": "Sleigh",
"doi-asserted-by": "crossref",
"first-page": "726",
"journal-title": "Am. Rev. Respir. Dis.",
"key": "ref_35",
"volume": "137",
"year": "1988"
},
{
"DOI": "10.1083/jcb.201304099",
"article-title": "Big steps toward understanding dynein",
"author": "Kikkawa",
"doi-asserted-by": "crossref",
"first-page": "15",
"journal-title": "J. Cell Biol.",
"key": "ref_36",
"volume": "202",
"year": "2013"
},
{
"DOI": "10.1016/j.cub.2014.08.047",
"article-title": "Multiciliated cells",
"author": "Brooks",
"doi-asserted-by": "crossref",
"first-page": "R973",
"journal-title": "Curr. Biol.",
"key": "ref_37",
"volume": "24",
"year": "2014"
},
{
"DOI": "10.1089/jamp.2007.0659",
"article-title": "Role of cilia, mucus, and airway surface liquid in mucociliary dysfunction: Lessons from mouse models",
"author": "Mall",
"doi-asserted-by": "crossref",
"first-page": "13",
"journal-title": "J. Aerosol Med. Pulm. Drug Deliv.",
"key": "ref_38",
"volume": "21",
"year": "2008"
},
{
"DOI": "10.1513/pats.200611-183HT",
"article-title": "Advancing outcome measures for the new era of drug development in cystic fibrosis",
"author": "Ramsey",
"doi-asserted-by": "crossref",
"first-page": "370",
"journal-title": "Proc. Am. Thorac. Soc.",
"key": "ref_39",
"volume": "4",
"year": "2007"
},
{
"DOI": "10.1126/science.1173869",
"article-title": "Motile cilia of human airway epithelia are chemosensory",
"author": "Shah",
"doi-asserted-by": "crossref",
"first-page": "1131",
"journal-title": "Science",
"key": "ref_40",
"volume": "325",
"year": "2009"
},
{
"DOI": "10.1016/S1569-1993(17)30457-5",
"article-title": "93 Determining the impact of the T2R38 bitter taste receptor on P. aeruginosa infection in the cystic fibrosis airway",
"author": "Turnbull",
"doi-asserted-by": "crossref",
"first-page": "S88",
"journal-title": "J. Cyst. Fibros.",
"key": "ref_41",
"volume": "16",
"year": "2017"
},
{
"DOI": "10.1201/9781420005844",
"doi-asserted-by": "crossref",
"key": "ref_42",
"unstructured": "Liedtke, W.B., and Heller, S. (2007). Frontiers in Neuroscience the TRPV4 Channel in Ciliated Epithelia. TRP Ion Channel Function in Sensory Transduction and Cellular Signaling Cascades, CRC Press/Taylor & Francis Group, LLC."
},
{
"DOI": "10.1016/j.cell.2022.11.030",
"article-title": "SARS-CoV-2 replication in airway epithelia requires motile cilia and microvillar reprogramming",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "112",
"journal-title": "Cell",
"key": "ref_43",
"volume": "186",
"year": "2023"
},
{
"DOI": "10.1128/JVI.00384-06",
"article-title": "Infection of human airway epithelium by human and avian strains of influenza a virus",
"author": "Thompson",
"doi-asserted-by": "crossref",
"first-page": "8060",
"journal-title": "J. Virol.",
"key": "ref_44",
"volume": "80",
"year": "2006"
},
{
"DOI": "10.1128/JVI.79.2.1113-1124.2005",
"article-title": "Infection of ciliated cells by human parainfluenza virus type 3 in an in vitro model of human airway epithelium",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "1113",
"journal-title": "J. Virol.",
"key": "ref_45",
"volume": "79",
"year": "2005"
},
{
"DOI": "10.1093/infdis/jix640",
"article-title": "In Vitro Model of Fully Differentiated Human Nasal Epithelial Cells Infected with Rhinovirus Reveals Epithelium-Initiated Immune Responses",
"author": "Tan",
"doi-asserted-by": "crossref",
"first-page": "906",
"journal-title": "J. Infect. Dis.",
"key": "ref_46",
"volume": "217",
"year": "2018"
},
{
"DOI": "10.1128/JVI.76.11.5654-5666.2002",
"article-title": "Respiratory syncytial virus infection of human airway epithelial cells is polarized, specific to ciliated cells, and without obvious cytopathology",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "5654",
"journal-title": "J. Virol.",
"key": "ref_47",
"volume": "76",
"year": "2002"
},
{
"article-title": "Comparative anatomy, physiology, and function of the upper respiratory tract",
"author": "Reznik",
"first-page": "171",
"journal-title": "Environ. Health Perspect.",
"key": "ref_48",
"volume": "85",
"year": "1990"
},
{
"DOI": "10.1113/jphysiol.2004.079228",
"article-title": "Ionic conductances in sustentacular cells of the mouse olfactory epithelium",
"author": "Vogalis",
"doi-asserted-by": "crossref",
"first-page": "785",
"journal-title": "J. Physiol.",
"key": "ref_49",
"volume": "562",
"year": "2005"
},
{
"DOI": "10.1038/s41591-020-0868-6",
"article-title": "SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes",
"author": "Sungnak",
"doi-asserted-by": "crossref",
"first-page": "681",
"journal-title": "Nat. Med.",
"key": "ref_50",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1126/science.abd2985",
"article-title": "Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity",
"author": "Ojha",
"doi-asserted-by": "crossref",
"first-page": "856",
"journal-title": "Science",
"key": "ref_51",
"volume": "370",
"year": "2020"
},
{
"DOI": "10.1074/jbc.M117.783845",
"article-title": "Neuropilin-1 promotes Hedgehog signaling through a novel cytoplasmic motif",
"author": "Pinskey",
"doi-asserted-by": "crossref",
"first-page": "15192",
"journal-title": "J. Biol. Chem.",
"key": "ref_52",
"volume": "292",
"year": "2017"
},
{
"DOI": "10.1016/j.jaci.2017.07.018",
"article-title": "Propagation of respiratory viruses in human airway epithelia reveals persistent virus-specific signatures",
"author": "Brito",
"doi-asserted-by": "crossref",
"first-page": "2074",
"journal-title": "J. Allergy Clin. Immunol.",
"key": "ref_53",
"volume": "141",
"year": "2018"
},
{
"DOI": "10.1183/09031936.01.00093001",
"article-title": "The effects of coronavirus on human nasal ciliated respiratory epithelium",
"author": "Chilvers",
"doi-asserted-by": "crossref",
"first-page": "965",
"journal-title": "Eur. Respir. J.",
"key": "ref_54",
"volume": "18",
"year": "2001"
},
{
"DOI": "10.1177/0194599820929278",
"article-title": "Aggregate Prevalence of Chemosensory and Sinonasal Dysfunction in SARS-CoV-2 and Related Coronaviruses",
"author": "Lehrich",
"doi-asserted-by": "crossref",
"first-page": "156",
"journal-title": "Otolaryngol. Head Neck Surg.",
"key": "ref_55",
"volume": "163",
"year": "2020"
},
{
"DOI": "10.1093/chemse/bjaa081",
"article-title": "Recent Smell Loss Is the Best Predictor of COVID-19 among Individuals with Recent Respiratory Symptoms",
"author": "Gerkin",
"doi-asserted-by": "crossref",
"first-page": "bjaa081",
"journal-title": "Chem. Senses",
"key": "ref_56",
"volume": "46",
"year": "2021"
},
{
"DOI": "10.1038/s41591-020-0916-2",
"article-title": "Real-time tracking of self-reported symptoms to predict potential COVID-19",
"author": "Menni",
"doi-asserted-by": "crossref",
"first-page": "1037",
"journal-title": "Nat. Med.",
"key": "ref_57",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1126/sciadv.abc5801",
"article-title": "Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia",
"author": "Brann",
"doi-asserted-by": "crossref",
"first-page": "eabc5801",
"journal-title": "Sci. Adv.",
"key": "ref_58",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1016/j.isci.2020.101839",
"article-title": "SARS-CoV-2 Receptors and Entry Genes Are Expressed in the Human Olfactory Neuroepithelium and Brain",
"author": "Fodoulian",
"doi-asserted-by": "crossref",
"first-page": "101839",
"journal-title": "iScience",
"key": "ref_59",
"volume": "23",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.12603",
"article-title": "Persistent Symptoms in Patients After Acute COVID-19",
"author": "Bernabei",
"doi-asserted-by": "crossref",
"first-page": "603",
"journal-title": "JAMA",
"key": "ref_60",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1002/lary.29286",
"article-title": "Prevalence of Olfactory Dysfunction in Coronavirus Disease 2019 (COVID-19): A Meta-analysis of 27,492 Patients",
"author": "Saniasiaya",
"doi-asserted-by": "crossref",
"first-page": "865",
"journal-title": "Laryngoscope",
"key": "ref_61",
"volume": "131",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2022.01.024",
"article-title": "Non-cell-autonomous disruption of nuclear architecture as a potential cause of COVID-19-induced anosmia",
"author": "Zazhytska",
"doi-asserted-by": "crossref",
"first-page": "1052",
"journal-title": "Cell",
"key": "ref_62",
"volume": "185",
"year": "2022"
},
{
"DOI": "10.1136/bmj.m1091",
"article-title": "Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "m1091",
"journal-title": "BMJ",
"key": "ref_63",
"volume": "368",
"year": "2020"
},
{
"DOI": "10.1002/alr.22053",
"article-title": "Olfactory loss in chronic rhinosinusitis is associated with neuronal activation of c-Jun N-terminal kinase",
"author": "Victores",
"doi-asserted-by": "crossref",
"first-page": "415",
"journal-title": "Int. Forum Allergy Rhinol.",
"key": "ref_64",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.1093/cid/ciaa995",
"article-title": "Severe Acute Respiratory Syndrome Coronavirus 2 Infects and Damages the Mature and Immature Olfactory Sensory Neurons of Hamsters",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "e503",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_65",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.1126/scitranslmed.add0484",
"article-title": "Persistent post-COVID-19 smell loss is associated with immune cell infiltration and altered gene expression in olfactory epithelium",
"author": "Finlay",
"doi-asserted-by": "crossref",
"first-page": "eadd0484",
"journal-title": "Sci. Transl. Med.",
"key": "ref_66",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1038/s41588-021-00986-w",
"article-title": "The UGT2A1/UGT2A2 locus is associated with COVID-19-related loss of smell or taste",
"author": "Shelton",
"doi-asserted-by": "crossref",
"first-page": "121",
"journal-title": "Nat. Genet.",
"key": "ref_67",
"volume": "54",
"year": "2022"
},
{
"DOI": "10.1016/j.nic.2022.07.022",
"article-title": "Anatomy of the Pharynx and Cervical Esophagus",
"author": "Ozgen",
"doi-asserted-by": "crossref",
"first-page": "791",
"journal-title": "Neuroimaging Clin. N. Am.",
"key": "ref_68",
"volume": "32",
"year": "2022"
},
{
"DOI": "10.21873/invivo.12712",
"article-title": "Epipharyngeal Abrasive Therapy Down-regulates the Expression of SARS-CoV-2 Entry Factors ACE2 and TMPRSS2",
"author": "Nishi",
"doi-asserted-by": "crossref",
"first-page": "371",
"journal-title": "In Vivo",
"key": "ref_69",
"volume": "36",
"year": "2022"
},
{
"DOI": "10.21873/invivo.12967",
"article-title": "Epipharyngeal Abrasive Therapy Down-regulates the Expression of Cav1.2: A Key Molecule in Influenza Virus Entry",
"author": "Nishi",
"doi-asserted-by": "crossref",
"first-page": "2357",
"journal-title": "In Vivo",
"key": "ref_70",
"volume": "36",
"year": "2022"
},
{
"DOI": "10.1016/j.yexcr.2020.112204",
"article-title": "Network perturbation analysis in human bronchial epithelial cells following SARS-CoV2 infection",
"author": "Nunnari",
"doi-asserted-by": "crossref",
"first-page": "112204",
"journal-title": "Exp. Cell Res.",
"key": "ref_71",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1080/07391102.2020.1818626",
"article-title": "Exploring structural dynamics of the MERS-CoV receptor DPP4 and mutant DPP4 receptors",
"author": "Alaofi",
"doi-asserted-by": "crossref",
"first-page": "752",
"journal-title": "J. Biomol. Struct. Dyn.",
"key": "ref_72",
"volume": "40",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2001017",
"article-title": "A Novel Coronavirus from Patients with Pneumonia in China, 2019",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "727",
"journal-title": "N. Engl. J. Med.",
"key": "ref_73",
"volume": "382",
"year": "2020"
},
{
"article-title": "Severe acute respiratory syndrome (SARS)--new, unknown disease?",
"author": "Zajkowska",
"first-page": "183",
"journal-title": "Pol. Merkur. Lek.",
"key": "ref_74",
"volume": "16",
"year": "2004"
},
{
"article-title": "Airway Clearance Techniques for Primary Ciliary Dyskinesia; is the Cystic Fibrosis literature portable?",
"author": "Schofield",
"first-page": "73",
"journal-title": "Paediatr. Respir. Rev.",
"key": "ref_75",
"volume": "25",
"year": "2018"
},
{
"DOI": "10.2139/ssrn.3582819",
"doi-asserted-by": "crossref",
"key": "ref_76",
"unstructured": "Grant, M.C., Geoghegan, L., Arbyn, M., Mohammed, Z., McGuinness, L., Clarke, E.L., and Wade, R.G. (2020). The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): A systematic review and meta-analysis of 148 studies from 9 countries. PLoS ONE, 15."
},
{
"DOI": "10.1016/S2213-2600(21)00125-9",
"article-title": "Confronting COVID-19-associated cough and the post-COVID syndrome: Role of viral neurotropism, neuroinflammation, and neuroimmune responses",
"author": "Song",
"doi-asserted-by": "crossref",
"first-page": "533",
"journal-title": "Lancet Respir. Med.",
"key": "ref_77",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1080/02770903.2020.1804576",
"article-title": "The causes of acute cough: A tertiary-care hospital study in Japan",
"author": "Tajiri",
"doi-asserted-by": "crossref",
"first-page": "1495",
"journal-title": "J. Asthma",
"key": "ref_78",
"volume": "58",
"year": "2021"
},
{
"DOI": "10.1164/rccm.201709-1813OC",
"article-title": "IFN-γ Enhances the Cough Reflex Sensitivity via Calcium Influx in Vagal Sensory Neurons",
"author": "Deng",
"doi-asserted-by": "crossref",
"first-page": "868",
"journal-title": "Am. J. Respir. Crit. Care Med.",
"key": "ref_79",
"volume": "198",
"year": "2018"
},
{
"DOI": "10.1016/j.rmed.2023.107372",
"article-title": "Dysfunctional mucociliary clearance in asthma and airway remodeling—New insights into an old topic",
"author": "Jesenak",
"doi-asserted-by": "crossref",
"first-page": "107372",
"journal-title": "Respir. Med.",
"key": "ref_80",
"volume": "218",
"year": "2023"
},
{
"DOI": "10.1089/jamp.2009.0775",
"article-title": "Acute lung injury: Epidemiology, pathogenesis, and treatment",
"author": "Johnson",
"doi-asserted-by": "crossref",
"first-page": "243",
"journal-title": "J. Aerosol Med. Pulm. Drug Deliv.",
"key": "ref_81",
"volume": "23",
"year": "2010"
},
{
"DOI": "10.3390/idr14030041",
"article-title": "Bacterial and Fungal Co-Infections and Superinfections in a Cohort of COVID-19 Patients: Real-Life Data from an Italian Third Level Hospital",
"author": "Ceccarelli",
"doi-asserted-by": "crossref",
"first-page": "372",
"journal-title": "Infect. Dis. Rep.",
"key": "ref_82",
"volume": "14",
"year": "2022"
},
{
"article-title": "Bronchiectasis as a Long-Term Consequence of SARS-COVID-19 Pneumonia: Future Studies are Needed",
"author": "Aksamit",
"first-page": "739",
"journal-title": "Arch. Bronconeumol.",
"key": "ref_83",
"volume": "57",
"year": "2021"
},
{
"DOI": "10.3390/microorganisms12040665",
"doi-asserted-by": "crossref",
"key": "ref_84",
"unstructured": "Retuerto-Guerrero, M., López-Medrano, R., de Freitas-González, E., and Rivero-Lezcano, O.M. (2024). Nontuberculous Mycobacteria, Mucociliary Clearance, and Bronchiectasis. Microorganisms, 12."
},
{
"DOI": "10.1038/nrm.2017.60",
"article-title": "Genes and molecular pathways underpinning ciliopathies",
"author": "Reiter",
"doi-asserted-by": "crossref",
"first-page": "533",
"journal-title": "Nat. Rev. Mol. Cell Biol.",
"key": "ref_85",
"volume": "18",
"year": "2017"
},
{
"DOI": "10.1083/jcb.202108015",
"doi-asserted-by": "crossref",
"key": "ref_86",
"unstructured": "Wang, L., Liu, C., Yang, B., Zhang, H., Jiao, J., Zhang, R., Liu, S., Xiao, S., Chen, Y., and Liu, B. (2022). SARS-CoV-2 ORF10 impairs cilia by enhancing CUL2ZYG11B activity. J. Cell Biol., 221."
},
{
"DOI": "10.1128/mBio.02374-20",
"article-title": "Defensive Properties of Mucin Glycoproteins during Respiratory Infections-Relevance for SARS-CoV-2",
"author": "Chatterjee",
"doi-asserted-by": "crossref",
"first-page": "e02374-20",
"journal-title": "mBio",
"key": "ref_87",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1183/13993003.04548-2020",
"article-title": "SARS-CoV-2 infections in people with primary ciliary dyskinesia: Neither frequent, nor particularly severe",
"author": "Pedersen",
"doi-asserted-by": "crossref",
"first-page": "2004548",
"journal-title": "Eur. Respir. J.",
"key": "ref_88",
"volume": "58",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2020.06.034",
"article-title": "The Global Phosphorylation Landscape of SARS-CoV-2 Infection",
"author": "Bouhaddou",
"doi-asserted-by": "crossref",
"first-page": "685",
"journal-title": "Cell",
"key": "ref_89",
"volume": "182",
"year": "2020"
},
{
"DOI": "10.1038/s41586-022-04826-7",
"doi-asserted-by": "crossref",
"key": "ref_90",
"unstructured": "COVID-19 Host Genetics Initiative (2022). A first update on mapping the human genetic architecture of COVID-19. Nature, 608, E1–E10."
},
{
"DOI": "10.1038/s41586-023-06355-3",
"doi-asserted-by": "crossref",
"key": "ref_91",
"unstructured": "COVID-19 Host Genetics Initiative (2023). A second update on mapping the human genetic architecture of COVID-19. Nature, 621, E7–E26."
},
{
"DOI": "10.1038/s41467-020-19145-6",
"article-title": "ACE2 localizes to the respiratory cilia and is not increased by ACE inhibitors or ARBs",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "5453",
"journal-title": "Nat. Commun.",
"key": "ref_92",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1172/JCI148517",
"article-title": "Nasal ciliated cells are primary targets for SARS-CoV-2 replication in the early stage of COVID-19",
"author": "Ahn",
"doi-asserted-by": "crossref",
"first-page": "e148517",
"journal-title": "J. Clin. Investig.",
"key": "ref_93",
"volume": "131",
"year": "2021"
},
{
"DOI": "10.1038/s41421-022-00488-x",
"article-title": "Structures of ACE2-SIT1 recognized by Omicron variants of SARS-CoV-2",
"author": "Shen",
"doi-asserted-by": "crossref",
"first-page": "123",
"journal-title": "Cell Discov.",
"key": "ref_94",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1016/S0955-0674(97)80026-9",
"article-title": "SNAREs and NSF in targeted membrane fusion",
"author": "Hay",
"doi-asserted-by": "crossref",
"first-page": "505",
"journal-title": "Curr. Opin. Cell Biol.",
"key": "ref_95",
"volume": "9",
"year": "1997"
},
{
"DOI": "10.1016/j.jgg.2015.11.006",
"article-title": "Depletion of BBS Protein LZTFL1 Affects Growth and Causes Retinal Degeneration in Mice",
"author": "Jiang",
"doi-asserted-by": "crossref",
"first-page": "381",
"journal-title": "J. Genet. Genom.",
"key": "ref_96",
"volume": "43",
"year": "2016"
},
{
"DOI": "10.1016/j.ebiom.2021.103806",
"doi-asserted-by": "crossref",
"key": "ref_97",
"unstructured": "Fink-Baldauf, I.M., Stuart, W.D., Brewington, J.J., Guo, M., and Maeda, Y. (2022). CRISPRi links COVID-19 GWAS loci to LZTFL1 and RAVER1. eBioMedicine, 75."
},
{
"DOI": "10.1371/journal.pgen.1007635",
"doi-asserted-by": "crossref",
"key": "ref_98",
"unstructured": "Pacentine, I.V., and Nicolson, T. (2019). Subunits of the mechano-electrical transduction channel, Tmc1/2b, require Tmie to localize in zebrafish sensory hair cells. PLoS Genet., 15."
},
{
"DOI": "10.1038/s41598-017-15027-y",
"doi-asserted-by": "crossref",
"key": "ref_99",
"unstructured": "Cockx, M., Gouwy, M., Ruytinx, P., Lodewijckx, I., Van Hout, A., Knoops, S., Pörtner, N., Ronsse, I., Vanbrabant, L., and Godding, V. (2017). Monocytes from patients with Primary Ciliary Dyskinesia show enhanced inflammatory properties and produce higher levels of pro-inflammatory cytokines. Sci. Rep., 7."
},
{
"DOI": "10.15252/embj.201798615",
"article-title": "Cilia-localized LKB1 regulates chemokine signaling, macrophage recruitment, and tissue homeostasis in the kidney",
"author": "Viau",
"doi-asserted-by": "crossref",
"first-page": "e98615",
"journal-title": "Embo J.",
"key": "ref_100",
"volume": "37",
"year": "2018"
},
{
"DOI": "10.1152/ajpgi.00381.2017",
"article-title": "Primary cilia disruption differentially affects the infiltrating and resident macrophage compartment in the liver",
"author": "Zimmerman",
"doi-asserted-by": "crossref",
"first-page": "G677",
"journal-title": "Am. J. Physiol. Gastrointest. Liver Physiol.",
"key": "ref_101",
"volume": "314",
"year": "2018"
},
{
"DOI": "10.3389/fphar.2021.814953",
"doi-asserted-by": "crossref",
"key": "ref_102",
"unstructured": "Zhu, Z., Wang, W., Zha, Y., Wang, X., Wang, L., Han, J., Zhang, J., and Lv, W. (2021). Transcriptomic and Lipidomic Profiles in Nasal Polyps of Glucocorticoid Responders and Non-Responders: Before and After Treatment. Front. Pharmacol., 12."
},
{
"DOI": "10.1371/journal.pone.0169161",
"doi-asserted-by": "crossref",
"key": "ref_103",
"unstructured": "Chinnapaiyan, S., Parira, T., Dutta, R., Agudelo, M., Morris, A., Nair, M., and Unwalla, H.J. (2017). HIV Infects Bronchial Epithelium and Suppresses Components of the Mucociliary Clearance Apparatus. PLoS ONE, 12."
},
{
"DOI": "10.1016/j.advms.2019.10.003",
"article-title": "Unveiling the genetic etiology of primary ciliary dyskinesia: When standard genetic approach is not enough",
"author": "Pereira",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Adv. Med. Sci.",
"key": "ref_104",
"volume": "65",
"year": "2020"
},
{
"DOI": "10.1007/978-1-4939-2438-7_1",
"article-title": "Coronaviruses: An overview of their replication and pathogenesis",
"author": "Fehr",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Methods Mol. Biol.",
"key": "ref_105",
"volume": "1282",
"year": "2015"
},
{
"DOI": "10.1007/s00018-004-4242-5",
"article-title": "Angiotensin-converting enzyme 2: A functional receptor for SARS coronavirus",
"author": "Kuhn",
"doi-asserted-by": "crossref",
"first-page": "2738",
"journal-title": "Cell. Mol. Life Sci.",
"key": "ref_106",
"volume": "61",
"year": "2004"
},
{
"DOI": "10.1128/JVI.02744-05",
"article-title": "Conformational states of the severe acute respiratory syndrome coronavirus spike protein ectodomain",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "6794",
"journal-title": "J. Virol.",
"key": "ref_107",
"volume": "80",
"year": "2006"
},
{
"DOI": "10.1016/S0140-6736(15)60454-8",
"article-title": "Middle East respiratory syndrome",
"author": "Zumla",
"doi-asserted-by": "crossref",
"first-page": "995",
"journal-title": "Lancet",
"key": "ref_108",
"volume": "386",
"year": "2015"
},
{
"DOI": "10.1016/S0955-0674(02)00012-1",
"article-title": "The vertebrate primary cilium is a sensory organelle",
"author": "Pazour",
"doi-asserted-by": "crossref",
"first-page": "105",
"journal-title": "Curr. Opin. Cell Biol.",
"key": "ref_109",
"volume": "15",
"year": "2003"
},
{
"DOI": "10.1183/13993003.00688-2020",
"article-title": "ACE-2 expression in the small airway epithelia of smokers and COPD patients: Implications for COVID-19",
"author": "Leung",
"doi-asserted-by": "crossref",
"first-page": "2000688",
"journal-title": "Eur. Respir. J.",
"key": "ref_110",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1038/s41598-018-28109-2",
"doi-asserted-by": "crossref",
"key": "ref_111",
"unstructured": "Haverkamp, A.K., Lehmbecker, A., Spitzbarth, I., Widagdo, W., Haagmans, B.L., Segalés, J., Vergara-Alert, J., Bensaid, A., van den Brand, J.M.A., and Osterhaus, A. (2018). Experimental infection of dromedaries with Middle East respiratory syndrome-Coronavirus is accompanied by massive ciliary loss and depletion of the cell surface receptor dipeptidyl peptidase 4. Sci. Rep., 8."
},
{
"DOI": "10.1016/S0140-6736(03)13413-7",
"article-title": "Lung pathology of fatal severe acute respiratory syndrome",
"author": "Nicholls",
"doi-asserted-by": "crossref",
"first-page": "1773",
"journal-title": "Lancet",
"key": "ref_112",
"volume": "361",
"year": "2003"
},
{
"DOI": "10.1146/annurev.immunol.25.022106.141706",
"article-title": "The Immunobiology of SARS",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "443",
"journal-title": "Annu. Rev. Immunol.",
"key": "ref_113",
"volume": "25",
"year": "2007"
},
{
"DOI": "10.1172/jci.insight.160277",
"article-title": "SARS-CoV-2 infection of sustentacular cells disrupts olfactory signaling pathways",
"author": "Verma",
"doi-asserted-by": "crossref",
"first-page": "e160277",
"journal-title": "JCI Insight",
"key": "ref_114",
"volume": "7",
"year": "2022"
},
{
"DOI": "10.1371/journal.ppat.1004502",
"doi-asserted-by": "crossref",
"key": "ref_115",
"unstructured": "Burkard, C., Verheije, M.H., Wicht, O., van Kasteren, S.I., van Kuppeveld, F.J., Haagmans, B.L., Pelkmans, L., Rottier, P.J., Bosch, B.J., and de Haan, C.A. (2014). Coronavirus cell entry occurs through the endo-/lysosomal pathway in a proteolysis-dependent manner. PLoS Pathog., 10."
},
{
"DOI": "10.1099/0022-1317-83-7-1535",
"article-title": "Dissecting virus entry via endocytosis",
"author": "Sieczkarski",
"doi-asserted-by": "crossref",
"first-page": "1535",
"journal-title": "J. Gen. Virol.",
"key": "ref_116",
"volume": "83",
"year": "2002"
},
{
"DOI": "10.1038/cr.2008.15",
"article-title": "SARS coronavirus entry into host cells through a novel clathrin- and caveolae-independent endocytic pathway",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "290",
"journal-title": "Cell Res.",
"key": "ref_117",
"volume": "18",
"year": "2008"
},
{
"DOI": "10.1242/jcs.059519",
"article-title": "The ciliary pocket: An endocytic membrane domain at the base of primary and motile cilia",
"author": "Ghossoub",
"doi-asserted-by": "crossref",
"first-page": "1785",
"journal-title": "J. Cell Sci.",
"key": "ref_118",
"volume": "123",
"year": "2010"
},
{
"DOI": "10.15252/embj.2022110727",
"article-title": "Autophagy-linked plasma and lysosomal membrane protein PLAC8 is a key host factor for SARS-CoV-2 entry into human cells",
"author": "Ugalde",
"doi-asserted-by": "crossref",
"first-page": "e110727",
"journal-title": "Embo J.",
"key": "ref_119",
"volume": "41",
"year": "2022"
},
{
"DOI": "10.7150/ijbs.45498",
"article-title": "Targeting the Endocytic Pathway and Autophagy Process as a Novel Therapeutic Strategy in COVID-19",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "1724",
"journal-title": "Int. J. Biol. Sci.",
"key": "ref_120",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1038/s41586-024-07575-x",
"article-title": "Human SARS-CoV-2 challenge uncovers local and systemic response dynamics",
"author": "Lindeboom",
"doi-asserted-by": "crossref",
"first-page": "189",
"journal-title": "Nature",
"key": "ref_121",
"volume": "631",
"year": "2024"
},
{
"DOI": "10.1002/cm.21351",
"article-title": "WDPCP regulates the ciliogenesis of human sinonasal epithelial cells in chronic rhinosinusitis",
"author": "Ma",
"doi-asserted-by": "crossref",
"first-page": "82",
"journal-title": "Cytoskeleton",
"key": "ref_122",
"volume": "74",
"year": "2017"
},
{
"DOI": "10.1097/CCM.0000000000004724",
"article-title": "Inflammatory Response and Phenotyping in Severe Acute Respiratory Infection From the Middle East Respiratory Syndrome Coronavirus and Other Etiologies",
"author": "Arabi",
"doi-asserted-by": "crossref",
"first-page": "228",
"journal-title": "Crit. Care Med.",
"key": "ref_123",
"volume": "49",
"year": "2021"
},
{
"DOI": "10.1093/cid/ciaa199",
"article-title": "Clinical Characteristics of Imported Cases of Coronavirus Disease 2019 (COVID-19) in Jiangsu Province: A Multicenter Descriptive Study",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "706",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_124",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.1128/mBio.00165-13",
"article-title": "Cell host response to infection with novel human coronavirus EMC predicts potential antivirals and important differences with SARS coronavirus",
"author": "Josset",
"doi-asserted-by": "crossref",
"first-page": "e00165-13",
"journal-title": "mBio",
"key": "ref_125",
"volume": "4",
"year": "2013"
},
{
"DOI": "10.1371/journal.pone.0088716",
"doi-asserted-by": "crossref",
"key": "ref_126",
"unstructured": "Faure, E., Poissy, J., Goffard, A., Fournier, C., Kipnis, E., Titecat, M., Bortolotti, P., Martinez, L., Dubucquoi, S., and Dessein, R. (2014). Distinct immune response in two MERS-CoV-infected patients: Can we go from bench to bedside?. PLoS ONE, 9."
},
{
"DOI": "10.1093/cid/ciaa248",
"article-title": "Dysregulation of Immune Response in Patients with Coronavirus 2019 (COVID-19) in Wuhan, China",
"author": "Qin",
"doi-asserted-by": "crossref",
"first-page": "762",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_127",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.14814/phy2.12116",
"article-title": "The exocyst and regulatory GTPases in urinary exosomes",
"author": "Choi",
"doi-asserted-by": "crossref",
"first-page": "e12116",
"journal-title": "Physiol. Rep.",
"key": "ref_128",
"volume": "2",
"year": "2014"
},
{
"DOI": "10.1016/j.scib.2023.09.027",
"article-title": "Ciliary ectosomes: Critical microvesicle packets transmitted from the cell tower",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "2674",
"journal-title": "Sci. Bull.",
"key": "ref_129",
"volume": "68",
"year": "2023"
},
{
"DOI": "10.1093/jb/mvaa112",
"article-title": "Current understandings of the relationship between extracellular vesicles and cilia",
"author": "Ikegami",
"doi-asserted-by": "crossref",
"first-page": "139",
"journal-title": "J. Biochem.",
"key": "ref_130",
"volume": "169",
"year": "2021"
},
{
"DOI": "10.1016/S2213-2600(20)30418-5",
"article-title": "Human recombinant soluble ACE2 in severe COVID-19",
"author": "Zoufaly",
"doi-asserted-by": "crossref",
"first-page": "1154",
"journal-title": "Lancet Respir. Med.",
"key": "ref_131",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor",
"author": "Hoffmann",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Cell",
"key": "ref_132",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1073/pnas.2221809120",
"article-title": "Proxalutamide reduces SARS-CoV-2 infection and associated inflammatory response",
"author": "Qiao",
"doi-asserted-by": "crossref",
"first-page": "e2221809120",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_133",
"volume": "120",
"year": "2023"
},
{
"DOI": "10.1021/acschemneuro.0c00619",
"article-title": "Novel Compounds Targeting Neuropilin Receptor 1 with Potential To Interfere with SARS-CoV-2 Virus Entry",
"author": "Patek",
"doi-asserted-by": "crossref",
"first-page": "1299",
"journal-title": "ACS Chem. Neurosci.",
"key": "ref_134",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/j.isci.2020.101160",
"article-title": "The MERS-CoV Receptor DPP4 as a Candidate Binding Target of the SARS-CoV-2 Spike",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "101160",
"journal-title": "iScience",
"key": "ref_135",
"volume": "23",
"year": "2020"
},
{
"DOI": "10.1038/s41467-020-15562-9",
"article-title": "Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV",
"author": "Ou",
"doi-asserted-by": "crossref",
"first-page": "1620",
"journal-title": "Nat. Commun.",
"key": "ref_136",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.12839",
"article-title": "Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review",
"author": "Wiersinga",
"doi-asserted-by": "crossref",
"first-page": "782",
"journal-title": "JAMA",
"key": "ref_137",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1016/j.ejmech.2020.112527",
"article-title": "A promising antiviral candidate drug for the COVID-19 pandemic: A mini-review of remdesivir",
"author": "Liang",
"doi-asserted-by": "crossref",
"first-page": "112527",
"journal-title": "Eur. J. Med. Chem.",
"key": "ref_138",
"volume": "201",
"year": "2020"
},
{
"DOI": "10.1038/s41598-020-66440-9",
"doi-asserted-by": "crossref",
"key": "ref_139",
"unstructured": "Jácome, R., Campillo-Balderas, J.A., Ponce de León, S., Becerra, A., and Lazcano, A. (2020). Sofosbuvir as a potential alternative to treat the SARS-CoV-2 epidemic. Sci. Rep., 10."
},
{
"article-title": "The first Chinese oral anti-COVID-19 drug Azvudine launched",
"author": "Yu",
"first-page": "100321",
"journal-title": "Innovation",
"key": "ref_140",
"volume": "3",
"year": "2022"
},
{
"DOI": "10.1016/j.jinf.2022.09.027",
"article-title": "Efficacy and safety of Paxlovid for COVID-19: A meta-analysis",
"author": "Zheng",
"doi-asserted-by": "crossref",
"first-page": "66",
"journal-title": "J. Infect.",
"key": "ref_141",
"volume": "86",
"year": "2023"
},
{
"DOI": "10.1093/cid/ciac443",
"article-title": "Effectiveness of Paxlovid in Reducing Severe Coronavirus Disease 2019 and Mortality in High-Risk Patients",
"author": "Gronich",
"doi-asserted-by": "crossref",
"first-page": "e342",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_142",
"volume": "76",
"year": "2023"
},
{
"DOI": "10.1080/13543776.2021.1884224",
"article-title": "Coronavirus helicases: Attractive and unique targets of antiviral drug-development and therapeutic patents",
"author": "Spratt",
"doi-asserted-by": "crossref",
"first-page": "339",
"journal-title": "Expert. Opin. Ther. Pat.",
"key": "ref_143",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.1002/pro.4075",
"article-title": "Characterization of the SARS-CoV-2 E Protein: Sequence, Structure, Viroporin, and Inhibitors",
"author": "Cao",
"doi-asserted-by": "crossref",
"first-page": "1114",
"journal-title": "Protein Sci.",
"key": "ref_144",
"volume": "30",
"year": "2021"
},
{
"DOI": "10.15252/embj.2020105938",
"article-title": "Structures of the SARS-CoV-2 nucleocapsid and their perspectives for drug design",
"author": "Peng",
"doi-asserted-by": "crossref",
"first-page": "e105938",
"journal-title": "Embo J.",
"key": "ref_145",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.1038/s41421-022-00381-7",
"article-title": "Broad ultra-potent neutralization of SARS-CoV-2 variants by monoclonal antibodies specific to the tip of RBD",
"author": "Ma",
"doi-asserted-by": "crossref",
"first-page": "16",
"journal-title": "Cell Discov.",
"key": "ref_146",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1016/j.addr.2018.04.003",
"article-title": "Repurposing excipients as active inhalation agents: The mannitol story",
"author": "Anderson",
"doi-asserted-by": "crossref",
"first-page": "45",
"journal-title": "Adv. Drug Deliv. Rev.",
"key": "ref_147",
"volume": "133",
"year": "2018"
},
{
"DOI": "10.1067/mai.2002.129704",
"article-title": "Effect of beta-adrenergic agonists on mucociliary clearance",
"author": "Bennett",
"doi-asserted-by": "crossref",
"first-page": "S291",
"journal-title": "J. Allergy Clin. Immunol.",
"key": "ref_148",
"volume": "110",
"year": "2002"
},
{
"DOI": "10.1159/000193645",
"article-title": "[Effects of drugs and environmental factors on ciliary movement (author’s transl)]",
"author": "Iravani",
"doi-asserted-by": "crossref",
"first-page": "157",
"journal-title": "Respiration",
"key": "ref_149",
"volume": "32",
"year": "1975"
},
{
"article-title": "Effect of terbutaline on movement of Cl− and Na+ across the trachea of the dog in vitro",
"author": "Davis",
"first-page": "547",
"journal-title": "Am. Rev. Respir. Dis.",
"key": "ref_150",
"volume": "120",
"year": "1979"
},
{
"DOI": "10.1056/NEJM199004263221704",
"article-title": "A pilot study of aerosolized amiloride for the treatment of lung disease in cystic fibrosis",
"author": "Knowles",
"doi-asserted-by": "crossref",
"first-page": "1189",
"journal-title": "N. Engl. J. Med.",
"key": "ref_151",
"volume": "322",
"year": "1990"
},
{
"DOI": "10.1016/0952-0600(92)90068-R",
"article-title": "The effects of salmeterol and salbutamol on ciliary beat frequency of cultured human bronchial epithelial cells, in vitro",
"author": "Devalia",
"doi-asserted-by": "crossref",
"first-page": "257",
"journal-title": "Pulm. Pharmacol.",
"key": "ref_152",
"volume": "5",
"year": "1992"
},
{
"DOI": "10.1038/s41584-020-0371-y",
"article-title": "Therapeutic glucocorticoids: Mechanisms of actions in rheumatic diseases",
"author": "Hardy",
"doi-asserted-by": "crossref",
"first-page": "133",
"journal-title": "Nat. Rev. Rheumatol.",
"key": "ref_153",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.1126/sciadv.abe4724",
"article-title": "JAK inhibition reduces SARS-CoV-2 liver infectivity and modulates inflammatory responses to reduce morbidity and mortality",
"author": "Stebbing",
"doi-asserted-by": "crossref",
"first-page": "eabe4724",
"journal-title": "Sci. Adv.",
"key": "ref_154",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1038/s41577-020-0311-8",
"article-title": "The trinity of COVID-19: Immunity, inflammation and intervention",
"author": "Tay",
"doi-asserted-by": "crossref",
"first-page": "363",
"journal-title": "Nat. Rev. Immunol.",
"key": "ref_155",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2209760",
"article-title": "Early Treatment with Pegylated Interferon Lambda for COVID-19",
"author": "Reis",
"doi-asserted-by": "crossref",
"first-page": "518",
"journal-title": "N. Engl. J. Med.",
"key": "ref_156",
"volume": "388",
"year": "2023"
},
{
"DOI": "10.1016/S1473-3099(22)00433-9",
"article-title": "Home as the new frontier for the treatment of COVID-19: The case for anti-inflammatory agents",
"author": "Perico",
"doi-asserted-by": "crossref",
"first-page": "e22",
"journal-title": "Lancet Infect. Dis.",
"key": "ref_157",
"volume": "23",
"year": "2023"
}
],
"reference-count": 157,
"references-count": 157,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2073-4409/13/16/1353"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "The Interplay between Airway Cilia and Coronavirus Infection, Implications for Prevention and Control of Airway Viral Infections",
"type": "journal-article",
"volume": "13"
}