Oral Bacteriotherapy in Patients With COVID-19: A Retrospective Cohort Study
et al., Frontiers in Medicine, doi:10.3389/fnut.2020.613928, Jan 2021
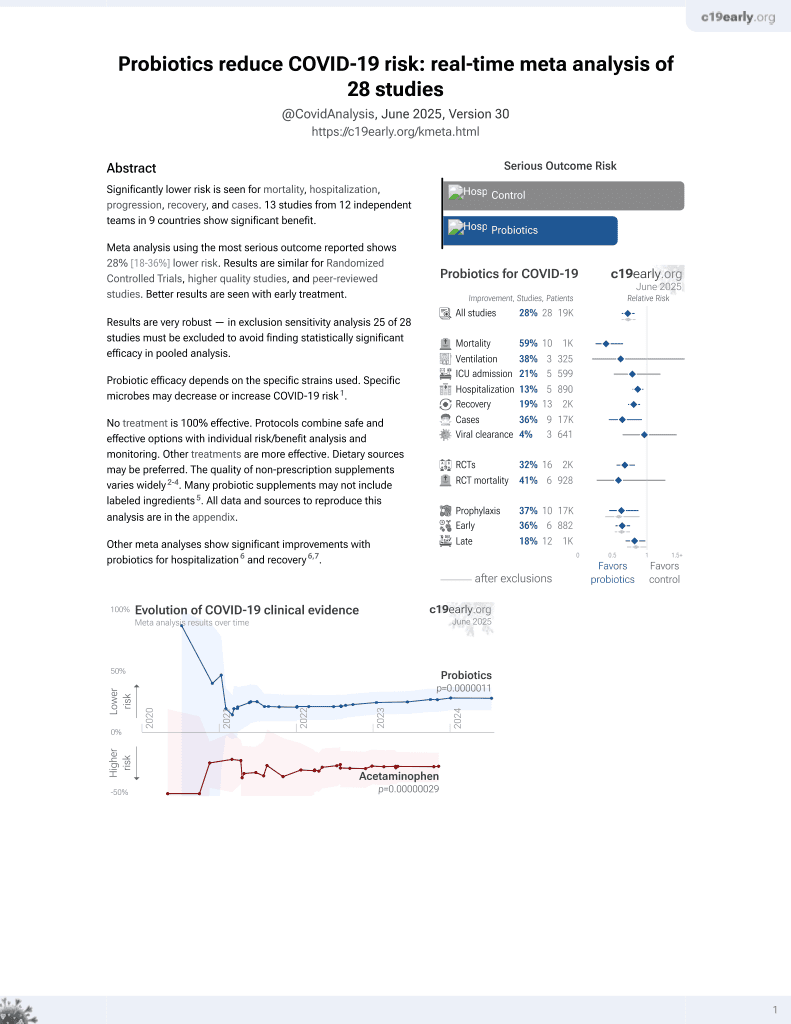
Probiotics for COVID-19
20th treatment shown to reduce risk in
March 2021, now with p = 0.00000044 from 29 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 200 severe condition hospitalized patients in Italy, 88 treated with probiotic Sivomixx, showing lower mortality with treatment.
Probiotic efficacy depends on the specific strains used. Specific microbes may decrease or increase COVID-19 risk1.
|
risk of death, 64.2% lower, RR 0.36, p = 0.003, treatment 10 of 88 (11.4%), control 34 of 112 (30.4%), NNT 5.3, adjusted per study, odds ratio converted to relative risk.
|
|
risk of ICU admission, 15.2% lower, RR 0.85, p = 0.60, treatment 16 of 88 (18.2%), control 24 of 112 (21.4%), NNT 31.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ceccarelli et al., 11 Jan 2021, retrospective, Italy, peer-reviewed, 14 authors.
Oral Bacteriotherapy in Patients With COVID-19: A Retrospective Cohort Study
Frontiers in Nutrition, doi:10.3389/fnut.2020.613928
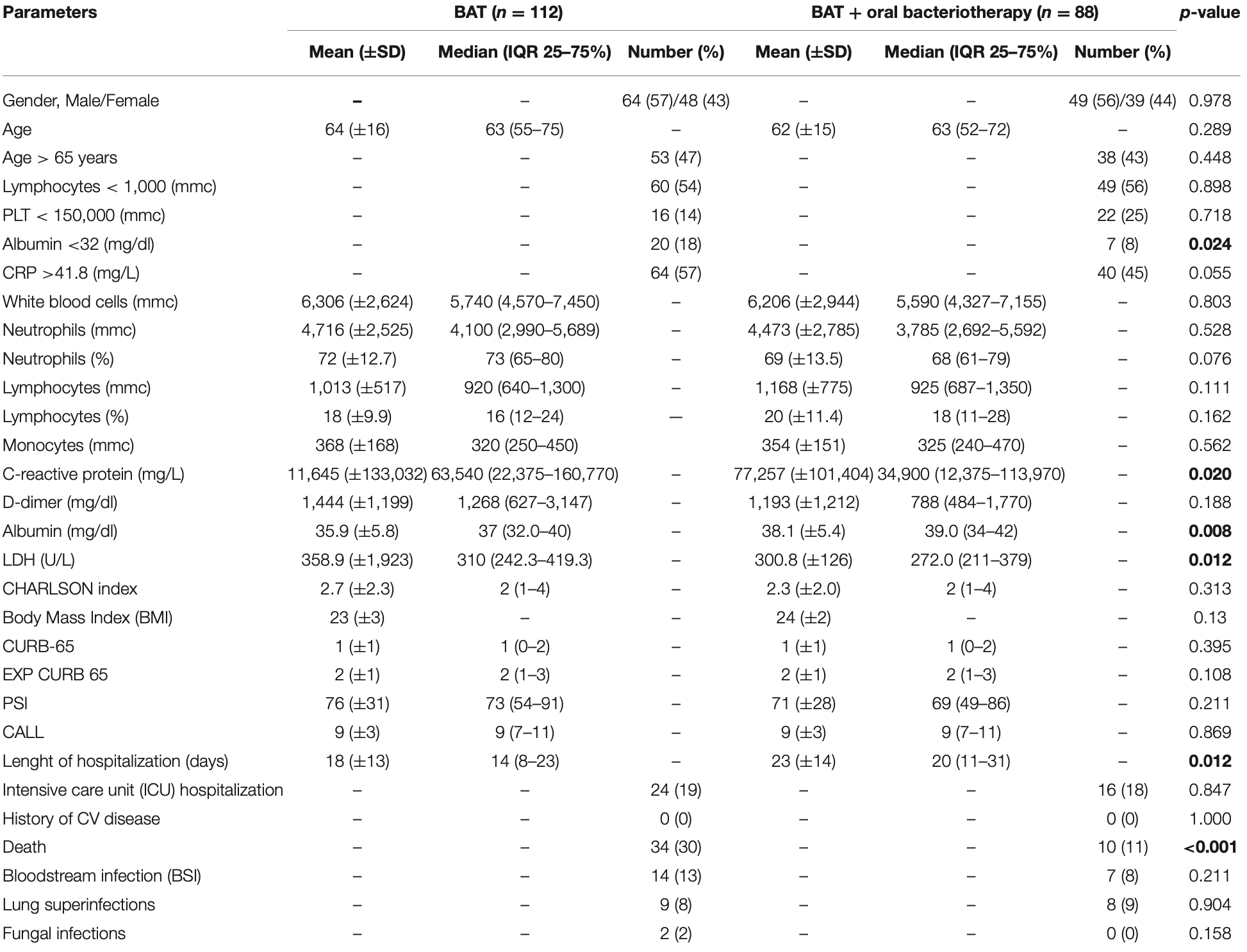
Background: Mounting evidence suggests SARS-CoV-2 may impact on host microbiota and gut inflammation, infecting intestinal epithelial cells. This possible link and its implications can be investigated by observing the effects of modulation of the microbial flora in patients with COVID-19. The aim of this study was to compare the rate of mortality, the need of ICU hospitalization and the length of hospitalization in patients with severe COVID-19 pneumonia who received the best available therapy (BAT) vs. patients treated with BAT and supplemented with oral bacteriotherapy. Methods: This retrospective, observational cohort study included 200 adults with severe COVID-19 pneumonia. All patients received therapeutic regimens including low molecular weight heparin plus one or more between hydroxychloroquine, azithromycin, antivirals, and Tocilizumab. Oral bacteriotherapy was used as complementary treatment. Results: Out of the 200 patients, 112 received BAT without oral bacteriotherapy, and 88 BAT with oral bacteriotherapy. Crude mortality was 22%. Eleven percent died in the group of patients treated with BAT plus oral bacteriotherapy vs. 30% subjects in the group of patients managed only with BAT (p < 0.001). By multivariate analysis, the age >65 years, CRP >41.8 mg/L, Platelets <150.000 mmc, and cardiovascular events were associated with the increased risk of mortality. Oral bacteriotherapy was an independent variable associated with a reduced risk for death. Despite large prospective trials are needed, this study highlights a possible role for oral bacteriotherapy in the management of patients hospitalized for COVID-19 pneumonia.
Hydroxycloroquine, Lopinavir/r, Azithromycin 9 ( 8 ) Hydroxycloroquine, Tocilizumab, Azithromycin 8 (7) 2.5 (0-5) Combination of the 4 drugs 8 ( 7 ) BAT plus oral bacteriotherapy (n = 88) Bacteriotherapy and 1 drug 13 ( 15 ) Bacteriotherapy and the 4 drugs The values in bold highlight statistically significant differences. transferable to different bacterial preparations (24) (25) (26) . The two groups of patients enrolled were substantially comparable for clinical characteristics, but not for CRP, LDH, and albumin levels; anyway, the increased levels of the CRP and LDH (observed in the group treated with BAT and bacteriotherapy) suggest a more severe disease-connected with lung injury-and a worse prognosis but are not considered a main prognostic factor (27) . Finally, the albumin levels were lower in the subjects treated only with BAT than in the other group, anyway, according to previous studies, only when albumin is below a specific range-i.e., <35g/L-the risks of venous and arterial thrombosis increase (28) (29) (30) (31) (32) .
CONCLUSION Mounting evidence suggests SARS-CoV-2 may impact on host microbial flora and gut inflammation in patients
CONSENT FOR PUBLICATION The participants provided their written consent for publication.
DATA AVAILABILITY STATEMENT The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.
ETHICS STATEMENT The studies..
References
Castelli, Angelo, Lombardi, Alfonsetti, Antonosante et al., Effects of the probiotic formulation SLAB51 in in vitro and in vivo Parkinson's disease models, Aging, doi:10.18632/aging.102927
Ceccarelli, Scagnolari, Pugliese, Mastroianni, Ettorre, Probiotics and COVID-19, Lancet Gastroenterol Hepatol, doi:10.1016/S2468-1253(20)30196-5
Ceccarelli, Statzu, Santinelli, Pinacchio, Bitossi et al., Challenges in the management of HIV infection: update on the role of probiotic supplementation as a possible complementary therapeutic strategy for cART treated people living with HIV/AIDS, Expert Opin Biol Ther, doi:10.1080/14712598.2019.1638907
Charlson, Pompei, Ales, Mackenzie, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis, doi:10.1016/0021-9681(87)90171-8
Chen, Lei, Wu, Liu, Zhou, Liver impairment associated with disease progression in COVID-19 patients, Liver Int, doi:10.1111/liv.14481
Conte, Toraldo, Targeting the gut-lung microbiota axis by means of a high-fibre diet and probiotics may have antiinflammatory effects in COVID-19 infection, Ther Adv Respir Dis, doi:10.1177/1753466620937170
D'ettorre, Ceccarelli, Marazzato, Campagna, Pinacchio et al., Challenges in the management of SARS-CoV2 infection: the role of oral bacteriotherapy as complementary therapeutic strategy to avoid the progression of COVID-19, Front. Med, doi:10.3389/fmed.2020.00389
Espinoza, León, Céspedes, Gómez, Canedo-Marroquín et al., Heme oxygenase-1 modulates human respiratory syncytial virus replication and lung pathogenesis during infection, J Immunol, doi:10.4049/jimmunol.1601414
Fine, Auble, Yealy, Hanusa, Weissfeld et al., A prediction rule to identify low-risk patients with community-acquired pneumonia, N Engl J Med, doi:10.1056/NEJM199701233360402
Gao, Jiang, Shi, Yang, Xia, Risk factors influencing the prognosis of elderly patients infected with COVID-19: a clinical retrospective study in Wuhan, China, Aging, doi:10.18632/aging.103631
Han, Zhang, Mu, Wei, Jin et al., Lactate dehydrogenase, an independent risk factor of severe COVID-19 patients: a retrospective and observational study, Aging, doi:10.18632/aging.103372
Hashiba, Suzuki, Nagashima, Suzuki, Inoue et al., Adenovirus-mediated transfer of heme oxygenase-1 cDNA attenuates severe lung injury induced by the influenza virus in mice, Gene Ther, doi:10.1038/sj.gt.3301540
Hill-Batorski, Halfmann, Neumann, Kawaoka, The cytoprotective enzyme heme oxygenase-1 suppresses Ebola virus replication, J Virol, doi:10.1128/JVI.02422-13
Howell, Donnino, Talmor, Clardy, Ngo et al., Performance of severity of illness scoring systems in emergency department patients with infection, Acad Emerg Med, doi:10.1197/j.aem.2007.02.036
Infusino, Marazzato, Mancone, Fedele, Mastroianni et al., Diet supplementation, probiotics, and nutraceuticals in SARS-CoV-2 infection: a scoping review, Nutrients, doi:10.3390/nu12061718
Ji, Zhang, Xu, Chen, Yang et al., Prediction for progression risk in patients with COVID-19 pneumonia: the CALL score
Kalantar-Zadeh, Ward, Kalantar-Zadeh, El-Omar, Considering the effects of microbiome and diet on SARS-CoV-2 infection: Nanotechnology roles, ACS Nano, doi:10.1021/acsnano.0c03402
Li, Ma, Pang, Fan, Hua, The commensal microbiota and viral infection: a comprehensive review, Front Immunol, doi:10.3389/fimmu.2019.01551
Lim, Van Der Eerden, Laing, Boersma, Karalus et al., Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study, Thorax, doi:10.1136/thorax.58.5.377
Liu, Xu, Zhou, Wu, -J et al., Expanded CURB-65: a new score system predicts severity of community-acquired pneumonia with superior efficiency, Sci Rep
Nobel, Phipps, Zucker, Lebwohl, Wang et al., Gastrointestinal symptoms and COVID-19: a casecontrol study from the United States, Gastroenterology, doi:10.1053/j.gastro.2020.04.017
Pouya, Saber, Kerachian, Molecular aspects of co-morbidities in COVID-19 infection, Arch Bone Jt Surg, doi:10.22038/abjs.2020.47828.2361
Ramachandran, Onukogu, Ghanta, Gajendran, Perisetti et al., Gastrointestinal symptoms and outcomes in hospitalized COVID-19 patients, Dig Dis, doi:10.1159/000509774
Toumazi, Constantinou, A fragile balance: the important role of the intestinal microbiota in the prevention and management of colorectal cancer, Oncology, doi:10.1159/000507959
Tseng, Lin, Wu, Chen, Chen et al., Human heme oxygenase 1 is a potential host cell factor against dengue virus replication, Sci Rep, doi:10.1038/srep32176
Tulic, Piche, Verhasselt, Lung-gut cross-talk: evidence, mechanisms and implications for the mucosal inflammatory diseases, Clin Exp Allergy, doi:10.1111/cea.12723
Viana, Nunes, Reis, ACE2 imbalance as a key player for the poor outcomes in COVID-19 patients with agerelated comorbidities -Role of gut microbiota dysbiosis, Ageing Res Rev, doi:10.1016/j.arr.2020.101123
Violi, Cangemi, Romiti, Ceccarelli, Oliva et al., Is albumin predictor of mortality in COVID-19?, Antioxid Redox Signal, doi:10.1089/ars.2020.8142
Violi, Ceccarelli, Cangemi, Alessandri, 'ettorre et al., Hypoalbuminemia, coagulopathy, and vascular disease in COVID-19, Circ Res, doi:10.1161/CIRCRESAHA.120.317173
Zhang, Yu, Tong, Liu, Tang, Predictive factors for disease progression in hospitalized patients with coronavirus disease 2019 in Wuhan, China, J Clin Virol, doi:10.1016/j.jcv.2020.104392
DOI record:
{
"DOI": "10.3389/fnut.2020.613928",
"ISSN": [
"2296-861X"
],
"URL": "http://dx.doi.org/10.3389/fnut.2020.613928",
"abstract": "<jats:p><jats:bold>Background:</jats:bold> Mounting evidence suggests SARS-CoV-2 may impact on host microbiota and gut inflammation, infecting intestinal epithelial cells. This possible link and its implications can be investigated by observing the effects of modulation of the microbial flora in patients with COVID-19. The aim of this study was to compare the rate of mortality, the need of ICU hospitalization and the length of hospitalization in patients with severe COVID-19 pneumonia who received the best available therapy (BAT) vs. patients treated with BAT and supplemented with oral bacteriotherapy.</jats:p><jats:p><jats:bold>Methods:</jats:bold> This retrospective, observational cohort study included 200 adults with severe COVID-19 pneumonia. All patients received therapeutic regimens including low molecular weight heparin plus one or more between hydroxychloroquine, azithromycin, antivirals, and Tocilizumab. Oral bacteriotherapy was used as complementary treatment.</jats:p><jats:p><jats:bold>Results:</jats:bold> Out of the 200 patients, 112 received BAT without oral bacteriotherapy, and 88 BAT with oral bacteriotherapy. Crude mortality was 22%. Eleven percent died in the group of patients treated with BAT plus oral bacteriotherapy vs. 30% subjects in the group of patients managed only with BAT (<jats:italic>p</jats:italic> &lt; 0.001). By multivariate analysis, the age &gt;65 years, CRP &gt;41.8 mg/L, Platelets &lt;150.000 mmc, and cardiovascular events were associated with the increased risk of mortality. Oral bacteriotherapy was an independent variable associated with a reduced risk for death. Despite large prospective trials are needed, this study highlights a possible role for oral bacteriotherapy in the management of patients hospitalized for COVID-19 pneumonia.</jats:p>",
"alternative-id": [
"10.3389/fnut.2020.613928"
],
"author": [
{
"affiliation": [],
"family": "Ceccarelli",
"given": "Giancarlo",
"sequence": "first"
},
{
"affiliation": [],
"family": "Borrazzo",
"given": "Cristian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pinacchio",
"given": "Claudia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Santinelli",
"given": "Letizia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Innocenti",
"given": "Giuseppe Pietro",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cavallari",
"given": "Eugenio Nelson",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Celani",
"given": "Luigi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Marazzato",
"given": "Massimiliano",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alessandri",
"given": "Francesco",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ruberto",
"given": "Franco",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Pugliese",
"given": "Francesco",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Venditti",
"given": "Mario",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mastroianni",
"given": "Claudio M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "d'Ettorre",
"given": "Gabriella",
"sequence": "additional"
}
],
"container-title": "Frontiers in Nutrition",
"container-title-short": "Front. Nutr.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2021,
1,
11
]
],
"date-time": "2021-01-11T13:44:07Z",
"timestamp": 1610372647000
},
"deposited": {
"date-parts": [
[
2021,
1,
13
]
],
"date-time": "2021-01-13T09:38:27Z",
"timestamp": 1610530707000
},
"indexed": {
"date-parts": [
[
2024,
4,
8
]
],
"date-time": "2024-04-08T09:17:39Z",
"timestamp": 1712567859607
},
"is-referenced-by-count": 54,
"issued": {
"date-parts": [
[
2021,
1,
11
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
11
]
],
"date-time": "2021-01-11T00:00:00Z",
"timestamp": 1610323200000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fnut.2020.613928/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2021,
1,
11
]
]
},
"published-online": {
"date-parts": [
[
2021,
1,
11
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1159/000509774",
"article-title": "Gastrointestinal symptoms and outcomes in hospitalized COVID-19 patients",
"author": "Ramachandran",
"doi-asserted-by": "publisher",
"first-page": "373",
"journal-title": "Dig Dis.",
"key": "B1",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.1053/j.gastro.2020.04.017",
"article-title": "Gastrointestinal symptoms and COVID-19: a case-control study from the United States",
"author": "Nobel",
"doi-asserted-by": "publisher",
"first-page": "373",
"journal-title": "Gastroenterology",
"key": "B2",
"volume": "159",
"year": "2020"
},
{
"DOI": "10.1016/j.jcv.2020.104392",
"article-title": "Predictive factors for disease progression in hospitalized patients with coronavirus disease 2019 in Wuhan, China",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "104392",
"journal-title": "J Clin Virol.",
"key": "B3",
"volume": "127",
"year": "2020"
},
{
"DOI": "10.22038/abjs.2020.47828.2361",
"article-title": "Molecular aspects of co-morbidities in COVID-19 infection",
"author": "Pouya",
"doi-asserted-by": "publisher",
"journal-title": "Arch Bone Jt Surg",
"key": "B4",
"year": "2020"
},
{
"DOI": "10.1016/j.arr.2020.101123",
"article-title": "ACE2 imbalance as a key player for the poor outcomes in COVID-19 patients with age-related comorbidities - Role of gut microbiota dysbiosis",
"author": "Viana",
"doi-asserted-by": "publisher",
"first-page": "101123",
"journal-title": "Ageing Res Rev.",
"key": "B5",
"volume": "62",
"year": "2020"
},
{
"DOI": "10.1111/liv.14481",
"article-title": "Liver impairment associated with disease progression in COVID-19 patients",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "2308",
"journal-title": "Liver Int.",
"key": "B6",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.3389/fmed.2020.00389",
"article-title": "Challenges in the management of SARS-CoV2 infection: the role of oral bacteriotherapy as complementary therapeutic strategy to avoid the progression of COVID-19",
"author": "d'Ettorre",
"doi-asserted-by": "publisher",
"first-page": "389",
"journal-title": "Front. Med.",
"key": "B7",
"volume": "7",
"year": "2020"
},
{
"key": "B8",
"unstructured": "Laboratory Testing for 2019 Novel Coronavirus (2019-nCoV) in Suspected Human Cases2020"
},
{
"key": "B9",
"unstructured": "Handbook for the Care of People With COVID-19 Disease, Version 2.02020"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"article-title": "A new method of classifying prognostic comorbidity in longitudinal studies: development and validation",
"author": "Charlson",
"doi-asserted-by": "publisher",
"first-page": "373",
"journal-title": "J Chronic Dis.",
"key": "B10",
"volume": "40",
"year": "1987"
},
{
"DOI": "10.1136/thorax.58.5.377",
"article-title": "Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study",
"author": "Lim",
"doi-asserted-by": "publisher",
"first-page": "377",
"journal-title": "Thorax.",
"key": "B11",
"volume": "58",
"year": "2003"
},
{
"DOI": "10.1197/j.aem.2007.02.036",
"article-title": "Performance of severity of illness scoring systems in emergency department patients with infection",
"author": "Howell",
"doi-asserted-by": "publisher",
"first-page": "709",
"journal-title": "Acad Emerg Med.",
"key": "B12",
"volume": "14",
"year": "2007"
},
{
"DOI": "10.1038/srep22911",
"article-title": "Expanded CURB-65: a new score system predicts severity of community-acquired pneumonia with superior efficiency [published correction appears in Sci Rep",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "22911",
"journal-title": "Sci Rep",
"key": "B13",
"volume": "6",
"year": "2016"
},
{
"DOI": "10.1056/NEJM199701233360402",
"article-title": "A prediction rule to identify low-risk patients with community-acquired pneumonia",
"author": "Fine",
"doi-asserted-by": "publisher",
"first-page": "243",
"journal-title": "N Engl J Med.",
"key": "B14",
"volume": "336",
"year": "1997"
},
{
"DOI": "10.1093/cid/ciaa414",
"article-title": "Prediction for progression risk in patients with COVID-19 pneumonia: the CALL score [published online ahead of print, 2020]",
"author": "Ji",
"doi-asserted-by": "publisher",
"first-page": "1393",
"journal-title": "Clin Infect Dis.",
"key": "B15",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.18632/aging.103631",
"article-title": "Risk factors influencing the prognosis of elderly patients infected with COVID-19: a clinical retrospective study in Wuhan, China",
"author": "Gao",
"doi-asserted-by": "publisher",
"first-page": "12504",
"journal-title": "Aging (Albany NY).",
"key": "B16",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1177/1753466620937170",
"article-title": "Targeting the gut-lung microbiota axis by means of a high-fibre diet and probiotics may have anti-inflammatory effects in COVID-19 infection",
"author": "Conte",
"doi-asserted-by": "publisher",
"first-page": "1753466620937170",
"journal-title": "Ther Adv Respir Dis.",
"key": "B17",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1111/cea.12723",
"article-title": "Lung-gut cross-talk: evidence, mechanisms and implications for the mucosal inflammatory diseases",
"author": "Tulic",
"doi-asserted-by": "publisher",
"first-page": "519",
"journal-title": "Clin Exp Allergy.",
"key": "B18",
"volume": "46",
"year": "2016"
},
{
"DOI": "10.1021/acsnano.0c03402",
"article-title": "Considering the effects of microbiome and diet on SARS-CoV-2 infection: Nanotechnology roles",
"author": "Kalantar-Zadeh",
"doi-asserted-by": "publisher",
"first-page": "5179",
"journal-title": "ACS Nano.",
"key": "B19",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.18632/aging.102927",
"article-title": "Effects of the probiotic formulation SLAB51 in in vitro and in vivo Parkinson's disease models",
"author": "Castelli",
"doi-asserted-by": "publisher",
"first-page": "4641",
"journal-title": "Aging (Albany NY).",
"key": "B20",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1038/sj.gt.3301540",
"article-title": "Adenovirus-mediated transfer of heme oxygenase-1 cDNA attenuates severe lung injury induced by the influenza virus in mice",
"author": "Hashiba",
"doi-asserted-by": "publisher",
"journal-title": "Gene Ther.",
"key": "B21",
"year": "2001"
},
{
"DOI": "10.4049/jimmunol.1601414",
"article-title": "Heme oxygenase-1 modulates human respiratory syncytial virus replication and lung pathogenesis during infection",
"author": "Espinoza",
"doi-asserted-by": "publisher",
"first-page": "212",
"journal-title": "J Immunol.",
"key": "B22",
"volume": "199",
"year": "2017"
},
{
"DOI": "10.1038/srep32176",
"article-title": "Human heme oxygenase 1 is a potential host cell factor against dengue virus replication",
"author": "Tseng",
"doi-asserted-by": "publisher",
"first-page": "32176",
"journal-title": "Sci Rep.",
"key": "B23",
"volume": "6",
"year": "2016"
},
{
"DOI": "10.1128/JVI.02422-13",
"article-title": "The cytoprotective enzyme heme oxygenase-1 suppresses Ebola virus replication",
"author": "Hill-Batorski",
"doi-asserted-by": "publisher",
"first-page": "13795",
"journal-title": "J Virol.",
"key": "B24",
"volume": "87",
"year": "2013"
},
{
"DOI": "10.1016/S2468-1253(20)30196-5",
"article-title": "Probiotics and COVID-19",
"author": "Ceccarelli",
"doi-asserted-by": "publisher",
"first-page": "721",
"journal-title": "Lancet Gastroenterol Hepatol.",
"key": "B25",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.3390/nu12061718",
"article-title": "Diet supplementation, probiotics, and nutraceuticals in SARS-CoV-2 infection: a scoping review",
"author": "Infusino",
"doi-asserted-by": "publisher",
"first-page": "1718",
"journal-title": "Nutrients.",
"key": "B26",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1080/14712598.2019.1638907",
"article-title": "Challenges in the management of HIV infection: update on the role of probiotic supplementation as a possible complementary therapeutic strategy for cART treated people living with HIV/AIDS",
"author": "Ceccarelli",
"doi-asserted-by": "publisher",
"first-page": "949",
"journal-title": "Expert Opin Biol Ther.",
"key": "B27",
"volume": "19",
"year": "2019"
},
{
"DOI": "10.18632/aging.103372",
"article-title": "Lactate dehydrogenase, an independent risk factor of severe COVID- 19 patients: a retrospective and observational study",
"author": "Han",
"doi-asserted-by": "publisher",
"first-page": "11245",
"journal-title": "Aging.",
"key": "B28",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1159/000507959",
"article-title": "Constantinou C. A fragile balance: the important role of the intestinal microbiota in the prevention and management of colorectal cancer",
"author": "Toumazi",
"doi-asserted-by": "publisher",
"first-page": "593",
"journal-title": "Oncology.",
"key": "B29",
"volume": "98",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2019.01551",
"article-title": "The commensal microbiota and viral infection: a comprehensive review",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "1551",
"journal-title": "Front Immunol",
"key": "B30",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1089/ars.2020.8142",
"article-title": "Is albumin predictor of mortality in COVID-19?",
"author": "Violi",
"doi-asserted-by": "publisher",
"journal-title": "Antioxid Redox Signal",
"key": "B31",
"year": "2020"
},
{
"DOI": "10.1161/CIRCRESAHA.120.317173",
"article-title": "Hypoalbuminemia, coagulopathy, and vascular disease in COVID-19",
"author": "Violi",
"doi-asserted-by": "publisher",
"first-page": "400",
"journal-title": "Circ Res.",
"key": "B32",
"volume": "127",
"year": "2020"
}
],
"reference-count": 32,
"references-count": 32,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fnut.2020.613928/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Nutrition and Dietetics",
"Endocrinology, Diabetes and Metabolism",
"Food Science"
],
"subtitle": [],
"title": "Oral Bacteriotherapy in Patients With COVID-19: A Retrospective Cohort Study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "7"
}